Abstract
The most common type of urinary bladder cancer is called as transitional cell carcinoma. The major risk factors for bladder cancer are environmental, tobacco smoking, exposure to toxic industrial chemicals and gases, bladder inflammation due to microbial and parasitic infections, as well as some adverse side-effects of medications. The genetic mutations in some chromosomal genes, such as FGFR3, RB1, HRAS, TP53, TSC1, and others, occur which form tumors in the urinary bladder. These genes play an important role in the regulation of cell division which prevents cells from dividing too quickly. The changes in the genes of human chromosome 9 are usually responsible for tumor in bladder cancer, but the genetic mutation of chromosome 22 can also result in bladder cancer. The identification of p53 gene mutation has been studied at NIH, Washington, DC, USA, in urine samples of bladder cancer patients. The invasive bladder cancers were determined for the presence of gene mutations on p53 suppressor gene. The 18 different bladder tumors were evaluated, and 11 (61 %) had genetic mutations of p53 gene. The bladder cancer studies have suggested that 70 % of bladder cancers involve a specific mutation in a particular gene, namely telomerase reverse transcriptase (TERT) gene. The TERT gene is involved in DNA protection, cellular aging processes, and cancer. The Urothelial carcinomas of the bladder have been described in Atlas of genetics and cytogenetics in oncology and hematology. HRAS is a proto-oncogene and has potential to cause cancer in several organs including the bladder. The TSC1 c. 1907 1908 del (E636fs) mutation in bladder cancer suggests that the location of the mutation is Exon 15 with frequency of TSC1 mutation of 11.7 %. The recent findings of BAP1 mutations have shown that it contributes to BRCA pathway alterations in bladder cancer. The discoveries of more gene mutations and new biomarkers and polymerase chain reaction bioassays for gene mutations in bladder cancer need further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The urinary bladder is a hollow, soft muscular organ situated in the lower abdomen of the body that stores urine until it is ready for excretion. Bladder cancer is a disease in which certain cells of the bladder become abnormal and cells start to multiply without any control or order [1]. The bladder cancer can cause blood in urine, painful urination, frequent urination, and feeling to urinate without any result in small quantities. Such signs and symptoms are not specific to bladder cancer, but bladder infections of non-cancerous type may also occur. Bladder cancer is the fourth common type of cancer in men and ninth most common in women, and about 45,000 men and 17,000 women are diagnosed with bladder cancer in USA each year and more in the world. The exact cause of bladder cancer is not yet known; however, several risk factors are associated with this cancer. The major risk factors for bladder cancer are environmental, smoking, exposure to toxic industrial chemicals and gases, bladder inflammation due to microbial and parasitic infections of Schistosomiasis, and some adverse effects of medications used for the treatment of bladder cancer, genetic mutations, and other risk factors.
Several genetic factors play a significant role in determining the bladder cancer risk. The genetic mutations in some chromosomal genes, such as FGFR3, RB1, HRAS, TP53, TSC1, and others, occur which form tumors in the urinary bladder. These genes play an important role in the regulation of cell division which prevent cells from dividing too fast and in an uncontrolled way. The changes in the genes structure may explain why some bladder cancer cells grow faster and spread more rapidly than others. The changes in the genes of human chromosome 9 are usually responsible for the tumor in bladder cancer, but the genetic mutation of chromosome 22 can also develop bladder cancer. The most genetic changes develop in bladder tissues during lifetime of a person rather than being inherited from parents. The bladder cancer is not inherited, and the tumors are formed by genetic mutations that occur in bladder cells; such genetic changes are called somatic mutations. The identification of p53 gene mutations has been studied at NIH, Washington, USA, in urine samples of bladder cancers [2]. The invasive bladder cancers were determined by the presence of gene mutations in the p53 suppressor gene. The 18 bladder tumors were evaluated, and 11 (61 %) had genetic mutations of p53. The genetic changes included 10 point mutations resulting in single amino acid substitutions and 1, 24-base pair deletion. In all these cases except one case, the genetic mutations were associated with chromosome 17p allelic deletions, leaving the cells with only mutant forms of p53 gene products. Using polymerase chain reaction (PCR) and oligomer-specific hybridization, the p53 gene mutations were identified in 1–7 % of the cells in the urine sediment of each of three patients tested. The p53 gene mutations are the first genetic alterations for invasive bladder cancers. The detection of such genetic mutations ex vivo has important clinical implications for monitoring bladder cancer in people whose tumor cells are shed extracorporeally as indicated. The p53 mutations in bladder cancer have also been studied which are called as TCC, transitional cell carcinoma [3]. The pattern of p53 mutations on bladder cancer and its sensitivity and specificity to detect genetic mutations using clinical material were studied using following assays: immunohistochemistry, restriction-fragment-length polymorphism, single-strand conformation polymorphism, and sequencing [4]. The morphological correlation with genotypic characteristics of the tissue analyzed was determined. The 42 patients with bladder cancer or tumors were used for this study. The nuclear immunoreactivities were observed in 26 out of 42 bladder tumors analyzed. The abnormal shifts were noted in mobility in 14 out of 42 cases in distinct exons, with one tumor revealing 3 mutations. A strong association was found between p53 nuclear over-expression and 17p LOH, and p53 nuclear over-expression and detection of mutations by SSCP and sequencing. The receiver-operating-curve statistical analysis showed that the accuracy of detecting p53 mutations by IHC was 90.3 %. It was a highly sensitive and specific method with a simple application using clinical material for bladder cancer.
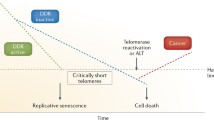
The bladder cancer study at Barcelona, Spain, CNIO, 2013, suggests that the 70 % of bladder cancers involve a specific mutation in a particular gene, namely TERT, telomerase reverse transcriptase gene [5]. The TERT gene is involved in DNA protection, cellular ageing processes, and cancer. The study of bladder cancer showed that TERT gene mutations occur during carcinogenesis and that such mutations may be present at any stage of the urothelial tumor process. This suggests that these mutations occur early on during carcinogenesis. The TERT gene produces a protein, the reverse transcriptase of the telomerase complex, which increases the length of telomeres, structures that are located at the end of the chromosomes, and protect genetic material and are also associated with cellular ageing process. The new bladder cancer biomarkers were studied using TERT to detect genetic mutations in urine samples of bladder cancer patients. The tumors were detected and monitored for their inhibiting drugs for bladder cancers. The bladder cancer molecular biology suggested many genetic mutations for the people with bladder cancer [6]. A range of different chromosomal abnormalities has been found in bladder cancer cells. The frequently detected genetic abnormality in transitional cell carcinoma (TCC) of the bladder was LOH on chromosome 9. The abnormalities in genes regulating cell cycle control were seen in advanced bladder cancers, particularly gene mutations in TP53 and proteins of the G1 checkpoint, especially RB1, CDKN2A (p16), and cyclin D1 (CCND1). The over-expression of gene p73 was also common in bladder cancers, and some studies have shown that this was associated with disease progression. The differential mucin expression was also reported in bladder cancers. However, reports of such results need more confirmation about the expression-specific mucins: MUC1, MUC2, and MUC7. The Uroplakins, membrane proteins, were expressed in both normal and cancerous urothelium which could act as a marker for the detection of metastases and circulating TCC cells. The gene–environment interaction studies have investigated genes that might modulate the susceptibility to bladder cancer associated with cigarette smoking. These genes include NAT1, NAT2, and GSTM1.
The HRAS is a proto-oncogene which has potential to cause normal cells to become cancerous cells in several organs including the bladder [7]. The somatic mutations occur and are not inherited from parents. The somatic mutations in the HRAS gene in bladder cells have been associated with bladder cancer. When one specific mutation occurs, it substitutes one protein building block, amino acid, for another amino acid in the HRAS protein. The genetic mutation replaces the amino acid glycine with the amino acid valine at position 12 (written as Gly12 Val or G12 V). The altered HRAS protein is activated within the cell, and this overactive protein directs the cell to grow and divide in the absence of outside signals, which leads to uncontrolled cell division and the formation of a tumor in bladder. The gene mutations in the HRAS gene have also been associated with the progression of bladder cancer which increases the risk of tumor recurrence after the cancer treatment.
Cancer genome study of bladder cancer, TSC1 c. 1907 1908del (E636 fs) mutation in bladder cancer [8], has suggested that the location of the mutation is Exon 15 with frequency of TSC1 mutation being 11.7 % in bladder cancer. The mTOR inhibitor targeted therapeutics for E636 fs mutation which resulted in a frame shift and the introduction of a premature stop codon into the TSC1 gene, and this mutation occurred within exon 15 in bladder cancer. The bladder cancer-related gene mutation was identified in New York, 2015, by Creative Biomart [9]. The STAG2 gene is the most mutation-inclined gene in bladder cancer especially for local carcinoma. The genetic test for the prevention of mutation was developed in bladder cancer patients. The STAG2 gene is a component of cohesion complex, which requires cohesion of sister chromatids after DNA replication. This cohesion complex forms a large ring of protein within which sister chromatids can be trapped. At anaphase of cell division, the complex is cleaved and dissociates from chromatin, which allows sister chromatids to segregate. This cohesion complex may also play a role in spindle pole assembly during mitosis.
The Urothelial carcinomas of the bladder have been described in the Atlas of genetics and cytogenetics in oncology and hematology [10]. In urinary bladder cancer, the bladder wall becomes massively infiltrated by an ulcerated and hemorrhagic tumor. These urothelial carcinomas of the bladder are classified as squamous cell carcinoma, adenocarcinoma (2 %), rare and poorly differentiated carcinoma as well as small-cell carcinoma. The urothelial carcinoma is the most frequent type of bladder cancer in the USA and Europe which represents 90–95 % cases, while squamous cell carcinoma represents only 5 %. About 70–80 % cases of squamous cell carcinoma are found in Middle East. The smoking of tobacco cigarettes and exposure to industrial chemicals such as aniline, benzidine, naphthylamine, and others cause bladder cancer with symptoms of blood in urine and irritation factor.
The treatment of bladder cancer includes resection, electrofulguration, cystectomy, chemotherapy, and radiotherapy. FGFR3 mutations seem to have lower recurrence rate compared to genetic mutations of TP53. The bladder tumors with elevated immunohistochemical expression of gene p53 and MIB-1 have the highest recurrence rate and bladder cancer mortality. For cytogenetics, urothelial carcinomas exhibit pseudo diploid karyotype with only a few anomalies in early stages which evolve toward pseudo-tetraploid complex karyotypes. The partial or complete monosomy 9 [9] was an early event which is found in 50 % of cases, and deletion (11p) or -11 was found in 20–25 % of cases as invasive tumors. The Del (13q) was found in 25 % of cases and correlated with high grades or stages of tumors with Rb alterations which were invasive. The Del (17p) was a late event found in 40 % of cases, but TP53 tumors had a worse prognosis for bladder cancer in patients. The gene FGFR3 was the most mutated oncogene for bladder cancer. The HRAS genetic mutations were found in about 15 % cases of bladder cancer.
Researchers in China have reported frequent mutations of chromatin remodeling genes in TCC of the bladder. This research provides a valuable genetic basis to understand TCC and aberration of chromatin regulation in bladder cancer patients. About 360,000 new cases of urinary bladder cancer are expected each year, and about 150,000 patients may suffer and die of bladder cancer worldwide.
In North America, Europe, and Asia, TCC is the most common type of bladder cancer diagnosed, accounting for 90 % of all bladder malignancies in those regions. The genetic aberrations of the chromatin remodeling genes occurred in 59 % of the 97 cases with TCC and the gene UTX could be altered more frequently in tumors with low stages and grades as suggested by Professor Jun Wang, Executive Director of BGI. The American Association for Cancer Research (AACR) reported that bladder cancer patients with rare genetic mutations showed exceptional response to Everolimus in Philadelphia [12]. A patient with advanced bladder cancer experienced a complete response for 14 months to the drug combination Everolimus and Pazopanib in a phase I trial, and genomic profiling of his tumor showed two alterations that may have caused this exceptional response, according to a study published in Cancer Discovery, a journal of the American Association for Cancer Research. “Studying exceptional responses can help us understand the specific reasons why some tumors are highly sensitive to certain anti-cancer agents,” said Nikhil Wagle, an instructor in medicine at Dana-Farber Cancer Institute and an associate member of the Broad Institute in Cambridge, MA, USA. “We can use that information to identify patients whose tumors have genetic alterations similar to those found in exceptional responders, and treat them with those same agents.” The phase I clinical trial was done for two anticancer agents, the mTOR inhibitor Everolimus, and Pazopanib, another drug used to treat kidney cancer, and one patient developed near complete remission of bladder cancer which lasted for 14 months. The whole-exome sequencing of the patient’s tumor was performed, and two mutations in the gene mTOR were found, which was the target of Everolimus. In the phase I trial, the investigators recruited nine patients with advanced solid tumors, including five with bladder cancer, whose disease had progressed despite treatment with standard therapies. Patients received one to 13 cycles of Everolimus and Pazopanib. One of the five patients with bladder cancer had a complete response, which lasted for 14 months. These investigators performed complete sequencing of the coding regions of the tumor genome, which included about 25,000 genes, and identified 2 mutations in mTOR. Two mutations, mTOR E2419K and mTOR E2014K, had never been identified in humans. This study was funded by the Next Generation Fund at the Broad Institute of MIT and Harvard University, Boston, MA, USA, the National Human Genome Research Institute, GlaxoSmithKline and Novartis. Dr. Wagle is an equity holder and a consultant to Foundation Medicine. Recently, the human urinary bladder cancer mutation PCR Array has been described by QIAGEN [13].
The Human Bladder Cancer qBiomarker Somatic Mutation PCR Array is a translational research tool that allows rapid, accurate, and comprehensive profiling of the somatic mutations in human bladder cancer samples on the following key genes: AKT1, CDKN2A, CTNNB1/beta-catenin, FGFR3, HRAS, KRAS, NRAS, PIK3CA, and P53. Further research of these mutations will enhance the understanding of carcinogenesis and identify potential drug targets. The research studies have demonstrated the function of individual and multiple somatic mutation statuses in identifying key signaling transduction disruptions. The mutation status of the EGFR and KRAS genes can predict the physiological response to certain drugs targeting these molecules. The human bladder cancer qBiomarker Somatic Mutation PCR Array, with its content coverage, was designed for studies of mutations in the bladder cancer and has the great potential for breakthrough and development of effective biomarkers for bladder cancers and other cancers in which these mutations were identified. This array includes 85 DNA sequence mutation assays designed to detect the most frequent, functionally verified, and biologically significant mutations in human bladder cancer. These mutations were taken from curated, somatic mutation databases and peer-reviewed scientific literature and represent the most frequently recurring somatic mutations compiled from over 3,200 bladder cancer patients. The simplicity of the products and operating procedure enables routine somatic mutations and profiling in research labs with access to real-time PCR instruments and assays.
The recent findings of BAP1 mutations indicated that it contributed to BRCA pathway alterations in bladder cancer [14]. The next-generation sequencing (NGS) of bladder tumors from over 100 Chinese patients showed alterations in additional genes those coding chromatin and remodeling enzymes, like lysine-specific histone demethylase 6A (KDM6A) and ARID1A, and spindle checkpoint proteins. The validated somatic variants occurred in 67 genes which mutated in bladder cancer. The frequently mutated genes which were altered in three or more tumors included KDM6A, ARID1A, and four other chromatin remodeling genes which were not recognized as mutated in bladder cancer, GCN1L1, CHD1, CHD1L, and BAP1 suggested an important role for these genes in bladder cancer. The BAP1 and other sequenced genes in additional 40 tumors were matched with normal tissue. About 15 % of 54 tumors showed BAP1 variants predicted to alter protein function. The novel bladder cancer genes show interactions with other pathways that might be targeted by therapeutics and show the importance of TERT, KDM6A, and BAP1 in bladder cancer [15].
Netto (2012) described the molecular biomarkers in urothelial carcinoma of the bladder [16]. Recent advances in cancer genetics and genomics are affecting the clinical management of solid tumors. The molecular diagnostics are now a routine clinical practice for lung, colon, and breast cancer, and molecular biomarkers are now used for the treatment of bladder cancer. There is a need for new treatment options that can improve the modern outcomes that are currently associated with muscle-invasive bladder cancer. The validated prognostic molecular biomarkers that can help cancer clinicians to identify patients early on are lacking. Therefore, accurate predictive biomarkers are needed to be developed which can forecast and show response to emerging targeted bladder cancer therapies.
Conclusions
In conclusion, there are predictions of many genes which can be mutated in bladder cancer patients. More genetic research is needed for the genomic studies of human bladder cancer. Further research is warranted to develop more new drugs for the control of genetic mutations in the bladder cancer patients. The new biomarkers and methods of genetic experiments for bladder cancer are required which can be applied clinically.
References
www.GeneticsHomeReference (2015). Bladder cancer. Washington, USA: NIH.
Science www.sciencemag.org. Sidransky, D., von Eschenbach, A., Tsai, Y. C., Jones, P., Summerhayes, I. Marshall, F., Paul, M., Green, P, Hamilton, S. R., Frost, P. et al. (1991). Identification of p53 gene mutations in bladder cancers and urine samples. Science, 252(5006): 706–709.
www.Bladdercancer Website. (2015). p53 Mutations in bladder cancer.
Cordon-Cardo, C., Dalbagni, G., Saez, G. T., Oliva, M. R., Zhang, Z. F., Rosai, J., et al. (2013). Human cancer. p53 mutations in human bladder cancer: Genotypic versus phenotypic patterns. International Journal of Cancer, 56(3), 347–353.
Real, F. X. (2013). 70 % of bladder cancers involve a specific mutation in a particular gene. Pompeu Fabra University, Barcelona, Spain, Sept, 19, 2013. (Eur.Urol. 9/2013).
Cancer Genetics. Web www.cancergenetics.org. (2015). Bladder cancer. Molecular biology.
Wikipedia. www.wikipedia.freeencyclopedia. Html. HRAS, 2015.
Solit, D. TSC1 c.1907_1908del (E636fs) (2013). Mutation in bladder cancer. My cancer genome http://www.mycancergenome.org/content/disease/bladder-cancer/tsc1/237/. Updated 12 Feb 2013.
www.CreativeBiomart.(2015). Bladder cancer-related gene mutation was identified. html, NY.
www.Bladder: Urothelial carcinomas. (2015). Atlas of genetics and cytogenetics in oncology and haematology.
www.BGI. Stay Connected. Html. (2011). Chinese scientists report research discovers frequent mutations of chromatin remodeling genes in TCC of the bladder, BGI. Shenzhen, China: Peking University.
www.AACR. (2014). American Association for Cancer Research. Bladder cancer patient with rare genetic mutations shows exceptional response to everolimus.
www.QIAGEN. (2015). Bladder cancer mutation PCR array. Human: qBiomaker somatic mutation PCR array: Human blood cancer.
www.NationalCancerInstitute, Washington, DC, USA. (2014, 2015). Investigating genetic alterations in bladder cancer. 2014, 2015.
Nickerson, M. L., Dancik, G. M., Im, K. M., Edwards, M. G., Turan, S., Brown, J. et al. (2014). Concurrent alterations in TERT, KDM6A, and the BRCA pathway in bladder cancer (Pub Med Link). Clinical Cancer Research; (Sept):15.
Netto, G. J. (2012). Molecular biomarkers in urothelial carcinoma of the bladder: Are we there yet? Review. Nature Reviews Urology, 9, 41–51. Published online 13 Dec 2011.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, X., Zhang, Y. Bladder Cancer and Genetic Mutations. Cell Biochem Biophys 73, 65–69 (2015). https://doi.org/10.1007/s12013-015-0574-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0574-z