Abstract
Intracerebral hemorrhage (ICH) is bleeding in brain caused by the rupture of brain blood vessel, which may lead to patient unconsciousness or death. In this study, we measured the expression of matrix metalloproteinase-9 (MMP-9) and its relevant inflammatory factors in the brain of rat with ICH. The effect of propofol on the expression of MMP-9 and inflammatory factors was investigated. We found the water content in the brain of ICH rats was significantly higher when compared with normal brain. Expression of MMP-9 and inflammatory factors IL-1β and TNF-α were up-regulated in ICH rats. Medium or high concentration of propofol can alleviate ICH in rats by inhibition of the inflammatory factor release and up-regulation of MMP-9 in brain. Our study suggests the inflammatory response after reduction of ICH through promotion of MMP-9 expression and neurite regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracerebral hemorrhage (ICH) is a common clinical cerebrovascular disease [1]. Edema is a significant histological change after ICH injury and initiates sequelae such as neurological deficits, increased intracranial pressure and encephalopathy, which are the key factors that lead to disability and fatality of patients. So far, there is no efficient treatment for ICH [2]. Therefore, an important topic of clinical research is to study the mechanism of cerebral edema for alleviation or prevention of the injury after ICH.
MMP-2 and MMP-9 are the members of MMPs family, which is the most important proteinase family involved in degrading various extracellular matrix (ECM). MMP-2 and MMP-9 are mainly expressed in cerebral vessels [2], which can be activated by free radicals through NF-κB pathway, resulting in increased vascular permeability and cerebral edema. Studies have also shown that MMP-9 aggregates in the activated microglia in surrounding tissues and exacerbates inflammatory response of brain tissue. Therefore, it is thought to be an important therapeutic target for alleviating inflammatory reactions after brain hemorrhage [3–6].
Propofol is an intravenous anesthetic widely used clinically. The anti-inflammatory property of propofol has been proved in some studies. It possesses neuroprotective effect on a variety of neurological injuries [7–9]. Studies indicated that the neuroprotective effect of propofol is extremely complicated, which is the result of multi-channel and multi-locus interactions. Therefore, neuroprotective mechanism of propofol has not been fully elucidated yet [10–12].
In this study, the conditions of early cerebral edema, MMP-9 expression, and inflammatory factor release after ICH are assessed. We explored the effect of propofol on alleviating early cerebral edema after ICH, as well as whether this effect correlates with MMP-9 expression and inflammatory factor release in brain.
Materials and Methods
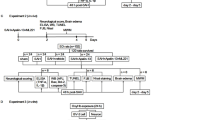
Animal Treatment
Rats were randomly divided into five groups, including the sham group, the ICH group, the low-dose propofol group (P1, treated with 15 mg/kg propofol), the medium-dose propofol group (P2, treated with 30 mg/kg propofol), and the high-dose propofol group (P3, treated with 60 mg/kg propofol). 15, 30, and 60 mg/kg of propofol were intraperitoneally injected into the rats in the P1, P2, and P3 groups, respectively, after the ICH model was established. The total volume of propofol for each rat was below 3 mL and was injected within 30 min. The rats in the ICH and the sham group were injected with the same dosage of saline solution.
Animal Model of ICH
Collagenase-induced ICH rat model was described by Rosenberg et al. Rats were fixed on a stereotaxic apparatus in prone position, making their plane of upper incisors ditch 2.4 mm lower than the plane of biauricular line so that the anterior fontanelle and posterior fontanelle was in the same plane. 75 % alcohol was used for local disinfection. Longitudinal incision was implemented in the middle of the cephalic region, separating layer by layer to expose anterior fontanelle. A stoma was drilled using pinhead on skull at 3 mm left to the central line and 0.24 mm in front of fontanelle, taking the center of anterior fontanelle as origin. The microsyringe fixed on the stereotaxic apparatus was inserted along the stoma with the depth of 5.8 mm (the position of the left caudate nucleus). 0.5 U of type VII collagenase (made in saline solution at 1 U/μL) was tardily injected within 3 min. The needle was kept at the position for 5 min after the injection and then slowly pulled out. After that, the rat was sutured and placed back to the cage for breeding. The same amount of saline solution was injected into the sham group with the same procedure described above.
Brain Water Content Measurement
Under deep anesthesia, rat head was incised and the brain was taken out 24 h after ICH surgery. The front olfactory bulb as well as the pia mater and the blood stains on the cortical surface were removed. About 500 mg of perihematoma was isolated on ice. The perihematoma was wet weighed immediately and then kept in a thermostatic oven for 48 h at 80 °C. The dry weight was measured consequently. The brain water content (BWC) was calculated as BWC = (wet weight − dry weight)/wet weight × 100 %.
Brain Pathological Morphology
Coronal incision was implemented 0.24 mm in front of anterior fontanelle, with the incision line exactly passed the original needle stoma. The brain tissue slices were immediately fixed in 4 % paraformaldehyde solution, and then dehydrated and embedded. Pathological changes in the caudate nucleus and the adjacent brain tissue were observed after hematoxylin and eosin (HE) staining under a microscope.
Western Blot
Protein was extracted from left side of brain at 4 °C and the protein concentration was measured with BCA protein assay kit. 10 μg of protein in each sample was subjected to SDS–polyacrylamide gel electrophoresis and transferred onto PVDF membrane. The membrane was blocked with 5 % skim milk at room temperature for 1 h and then probed with anti-MMP-9 monoclonal antibody (diluted at 1:3,000) at 4 °C on a shaker overnight. The membrane was then probed with horseradish peroxidase-conjugated goat anti-mouse antibody (diluted at 1:5,000) at room temperature for 1 h, incubated with chemiluminescence horseradish peroxidase substrate, and exposed to X-ray film.
RT-PCR
The samples were collected 24 h after ICH model was established. Total RNA in the right basal ganglia tissue of rats was extracted and reverse transcribed into cDNA. PCR amplification was implemented according to the following parameters: pre-degeneration at 94 °C for 3 min, followed by 30 cycles of degeneration at 94 °C for 30 s, renaturation at 60 °C for 45 s, extension at 72 °C for 45 s. The reactions were then incubated at 72 °C for 7 min. β-actin was used as internal reference, and its primers were added into PCR reactions after 5 cycles. The PCR primer sequences are as follows: IL-1β forward, 5′-GAAGGCAGTGTCACTCATT-3′. IL-1β reverse, 5′-TCTTTGGGTATTGTTTGG-3′. The product size is 443 bp. TNF-α forward, 5′-GCCTCTTCTCATTCCTGCTCGT-3′. TNF-α reverse, 5′-GCTGACGGTGTGGGTGAGGA-3′. The product size is 377 bp. β-actin forward, 5′-AGCCATGTACGTAGCCATCC-3′. β-actin reverse, 5′-CTCTCAGCTGTGGTGGTGAA-3′. The product size is 228 bp.
ELISA
The samples were collected 24 h after ICH model was established. 250–400 μL of cerebrospinal fluid was taken by gentle puncturing of the cisterna magna to avoid puncture of blood vessels and blood contamination. The collected cerebrospinal fluid was centrifuged at 2,000×g at 4 °C for 20 min. The supernatant was stored at −80 °C. ELISA was performed with rat IL-1β and TNF-α immunoassay kit according to the manufacturer’s instruction. The sample OD value was read at 450 nm within 30 min. Standard curve was drawn using OD value as y-axis and the standard sample concentration as x-axis. The concentration of the samples (pg/mL) was calculated based on the standard curve.
Statistical analysis
All the measurement data were represented as mean ± SD. SPSS 16.0 software was used for statistical analysis. One-way ANOVA and independent-sample test were used for comparison between groups. p < 0.05 was considered as statistically significant.
Results
Water Content in Brain Tissue
We measured water content in rat brain and found it significantly increased 24 h after ICH surgery when compared with the sham group, indicating that cerebral edema was generated after ICH. The water content in the ICH group was significantly higher than that in the sham group (p < 0.05). In the P1, P2, and P3 groups, it was significantly lower when compared with the ICH group (p < 0.05). The results are summarized in Table 1.
Pathological Morphology in Brain of Rats
We next examined the brain morphology. In the sham group, the brain structure was clear and intact without bleeding, edema, or significant pathological changes. Significant hemorrhage foci were observed in the caudate nucleus in the ICH group. The brain tissue around the hemorrhage foci was in a state of porosity and edema with a shape of net. Nerve cells scattered in the central region of hemorrhage foci and were highly swelling. Most of the region was stained light red without structure. The visible hemorrhage foci in the P2 and P3 groups were significantly smaller when compared with that in the ICH group. There are more nerve cells, with decreased porosity and edema. The alleviated pathological changes described above were observed in the P1 group, but the morphology of rats brain did not show obvious improvement when compared with the ICH group.
MMP-9 Expression in Brain
As shown in Fig. 1, MMP-9 expression level in brain was measured and was significantly higher in the P1, P2, P3, and ICH groups when compared with the sham group (p < 0.05). MMP-9 expression in the P1 group and the ICH group had no significant difference (p > 0.05). Its expression in the P2 and P3 groups was significantly higher than that in the ICH group (p < 0.05).
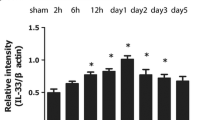
IL-1β and TNF-α Expression in Brain
As shown in Figs. 2 and 3, IL-1β and TNF-α mRNA levels and their protein concentration were significantly higher in the ICH group than the sham group (p < 0.05). Their mRNA and protein had no significant difference between the P1 group and the ICH group (p > 0.05). The mRNA and protein were significantly higher in the ICH group when compared with the P2 and P3 groups (p < 0.05). The results are summarized in Tables 2 and 3.
IL-1β mRNA level and the protein concentration in each group (\(\overline{\textit{x}}\) ± s, n = 5). The IL-1β mRNA was measured with semi-quantitative PCR (left panel). The IL-1β protein concentration was measured with ELISA (right panel). a p < 0.05, compared with the sham group. b p < 0.05, compared with the ICH group
TNF-α mRNA level and the protein concentration in each group (\(\overline{\textit{x}}\) ± s, n = 5). The TNF-α mRNA was measured with semi-quantitative PCR (left panel). The TNF-α protein concentration was measured with ELISA (right panel). a p < 0.05, compared with the sham group. b p < 0.05, compared with the ICH group
Discussion
MMP-9 has an important role in the degradation of ECM and is involved in multiple developmental and pathological processes. It is expressed at low level in normal cerebral tissue, while its expression can be stimulated by inflammatory factors, ischemia, and hypoxia, etc. MMP-9 high expression can be induced by cerebral hemorrhage. Since it undermines the integrity of blood–brain barrier by degrading the main component of the basement membrane surrounding blood vessels, it causes cerebral edema after cerebral hemorrhage and is toxic to nerve cells.
In our current study, we explored the effect of propofol on the inflammatory response of early cerebral edema and MMP-9 expression after ICH. Rat ICH model was established by injection of collagenase in the caudate nucleus. We discovered that the brain water content significantly increases 24 h after the establishment of rat ICH model. In addition, MMP-9 and proinflammatory cytokine are also up-regulated. Propofol treatment can alleviate early cerebral edema of ICH rats. Medium and high dose of propofol are able to promote MMP-9 expression and significantly decrease the release of inflammatory factors, while low dose of propofol has no obvious effect on inflammation inhibition. Therefore, it could be possible that propofol promotes MMP-9 expression, which in turn induces neurite regeneration. Neurite regeneration partially recovers neural circuits, which favors the survival of neurons, alleviates inflammatory response, and improves nerve functions.
The mechanisms of brain protection by propofol include reduction of neuronal apoptosis, inhibition of oxidative stress, and regulation of proteins in astrocytes [12, 13, 14]. These mechanisms have important implications on alleviating acute brain injury and providing brain protection in pathological processes of central nervous system diseases. Although the current study does not identify the mechanism for MMP-9 expression regulation by propofol, it provided a beneficial direction for reducing inflammatory response after ICH through promotion of MMP-9 expression and neurite regeneration.
In summary, we found that medium and high concentration of propofol can alleviate the water content in ICH rat brain, promote the expression of MMP-9, and decrease the inflammatory response in brain. This study also suggests a mechanism for the neuroprotective effect of propofol. However, the pathways that are involved in this process are still unclear. Further study of the neuroprotective effect of propofol and possible regulatory mechanisms will help to understand the pharmacological effects of propofol.
References
van Muiswinkel, F. L., & Kuiperij, H. B. (2005). The Nrf2-ARE signalling pathway: Promising drug target to combat oxidative stress in neurodegenerative disorders. Current Drug Targets-CNS and Neurological Disorders, 4(3), 267–281.
Yang, Y. I., Estrada, E. Y., Thompson, J. F., et al. (2006). Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. Journal of Cerebral Blood Flow and Metabolism, 27(4), 697–709.
Carriel, V., Garzon, I., Campos, A., et al. (2014). Differential expression of MMP-9 and neurofilament during peripheral nerve regeneration through bio-artificial conduits. Journal of Tissue Engineering and Regenerative Medicine,. doi:10.1002/term.1949.
Mahajan, C., Chouhan, R. S., Rath, G. P., et al. (2014). Effect of intraoperative brain protection with propofol on postoperative cognition in patients undergoing temporary clipping during intracranial aneurysm surgery. Neurology India, 62(3), 262–268.
Chen, G., Feng, D., Zhang, L., et al. (2013). Expression of nemo-like kinase (NLK) in the brain in a rat experimental subarachnoid hemorrhage model. Cell Biochemistry and Biophysics, 66(3), 671–680.
Wu, J., Chen, J., Guo, H., et al. (2014). Effects of high-pressure oxygen therapy on brain tissue water content and AQP4 expression in rabbits with cerebral hemorrhage. Cell Biochemistry and Biophysics, 70, 1–6.
Sloan, T. B., Mongan, P., Lyda, C., et al. (2014). Lidocaine infusion adjunct to total intravenous anesthesia reduces the total dose of propofol during intraoperative neurophysiological monitoring. Journal of Clinical Monitoring and Computing, 28(2), 139–147.
Lee, K. R., Colon, G. P., Betz, A. L., et al. (1996). Edema from intracerebral hemorrhage: the role of thrombin. Journal of Neurosurgery, 84(1), 91–96.
Tanskanen, P. E., Kyttä, J. V., Randell, T. T., et al. (2006). Dexmedetomidine as an anaesthetic adjuvant in patients undergoing intracranial tumour surgery: A double-blind, randomized and placebo-controlled study. British Journal of Anaesthesia, 97(5), 658–665.
Broderick, J. P., Adams, H. P., Barsan, W., et al. (1999). Guidelines for the management of spontaneous intracerebral hemorrhage a statement for healthcare professionals from a special writing group of the Stroke council, American Heart Association. Stroke, 30(4), 905–915.
Pinaud, M., Lelausque, J. N., Chetanneau, A., et al. (1990). Effects of propofol on cerebral hemodynamics and metabolism in patients with brain trauma. Anesthesiology, 73(3), 404–409.
Karwacki, Z., Kowianski, P., Dziewiatowski, J., et al. (2006). The effect of propofol on astro- and microglial reactivity in the course of experimental intracerebral haemorrhage in rats. Folia Neuropathologica, 44(1), 50–58.
Qing, Y. U. (2013). Effect of propofol and sevoflurane anesthesia on postoperatively cognitive function of aged patients in orthopedics. Journal of Bengbu Medical College, 8, 024.
Wagner, K. R. (2014). White matter injury after experimental intracerebral hemorrhage. White matter injury in Stroke and CNS disease (pp. 219–256). New York: Springer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, D., Li, S., Xiong, Q. et al. Effect of Propofol on the Expression of MMP-9 and Its Relevant Inflammatory Factors in Brain of Rat with Intracerebral Hemorrhage. Cell Biochem Biophys 72, 675–679 (2015). https://doi.org/10.1007/s12013-015-0516-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0516-9