Abstract
Idiopathic male infertility (IMI) remains challenging as the etiology of semen abnormalities is still unidentified. Sperm DNA fragmentation (SDF) has been suggested as a potential mechanism. Oral antioxidants including selenium have been tried for IMI with variable results. This study was undertaken to explore the effect of selenium therapy on semen parameters, antioxidant capacity, and SDF in infertile patients with idiopathic oligoasthenoteratospermia (OAT). Sixty-five infertile men with idiopathic OAT and fifty fertile controls were included in this prospective clinical study. Patients received selenium (200 μg/day) orally for 6 months. Seminal fluid parameters (WHO 5th criteria), total antioxidant capacity (TAC), catalase (CAT), and seminal SDF levels were assessed for all participants at the start of the study and after 6 months. Sperm concentration (P < 0.001), progressive motility (P < 0.001), and total motility (P < 0.01) significantly increased in patients after selenium therapy. Seminal TAC and CAT increased in patients post-therapy as compared to baseline values (P < 0.01). SDF levels significantly decreased (P < 0.001) in patients following selenium treatment in comparison to baseline values. SDF levels also correlated negatively with sperm progressive motility (r = − 0.44, P = 0.003) and total motility (r = − 0.48, P = 0.001). In conclusion, selenium therapy (200 μg/day) for 6 months increases sperm concentration, motility, seminal antioxidant capacity, and reduces SDF in patients with idiopathic OAT. Thus, selenium could be a promising therapy for men with IMI and may boost their fertility and fertility treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infertility is a worldwide medical condition with medical, psychological, and social implications. The prevalence of infertility is increasing and affecting approximately 12% of couples [1]. Male factor accounts for 40–50% of infertility cases [2]. The combination of sperm concentration, motility, and normal morphology below the reference values is referred to as oligoasthenoteratospermia (OAT). The exact mechanisms of male infertility remain unidentified. Several anatomical, endocrine, microbiological, genetic, systemic, and environmental contributing factors have been identified [3]. However, in approximately 20–25% of cases, the etiology of semen abnormalities is unknown and is termed idiopathic male infertility (IMI) [4]. Growing evidence indicates that genetic, epigenetic, posttranslational modifications, oxidative stress (OS), and sperm DNA fragmentation (SDF) could be implicated in the development of IMI [5].
SDF is a key contributor to male infertility and is associated with IMI, recurrent pregnancy loss as well as the outcomes of pregnancy and assisted reproductive techniques (ART) [6]. SDF could be attributed to abortive apoptosis, defective spermatogenesis, and OS [7]. OS is an imbalance between prooxidants production and endogenous antioxidant defense system. Excessive reactive oxygen species (ROS) levels adversely affect sperm function and fertilization [8]. While conventional semen analysis remains the primary test for male infertility assessment, it has many limitations including the inability to separate fertile from infertile men, the lack of assessment of sperm functions, and poor prediction of ART outcomes [9]. These limitations have motivated the search for new and complementary diagnostic tools for the assessment of infertile men including sperm function tests, OS markers, and SDF [10]. Different direct and indirect tests have been established for the detection of SDF and the most widely used tests encompass Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL), single-cell gel electrophoresis (comet), and sperm chromatin dispersion (SCD) tests [11].
Studies have reported increased SDF among men with infertility in comparison to fertile men [5, 12, 13]. SDF levels of more than 30% correlated negatively with male fertility potential [14]. A recent meta-analysis compared in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) success rates in men with variable SDF levels and demonstrated higher pregnancy rates in men with low SDF levels [15], but the influence of SDF on ICSI outcome remains controversial [16]. Therapies suggested reducing SDF levels encompass oral antioxidants, varicocelectomy, recurrent ejaculations with or without sperm selection techniques, and the use of retrieved sperm for ICSI [3, 17]. Treatment with individual or combined oral antioxidants has resulted in lower SDF levels in infertile men post-therapy [5, 10, 18]
Selenium is an essential dietary micronutrient and involved in several metabolic and reproductive functions including testosterone formation and is also an integral component of sperm selenoproteins [19]. Selenoproteins have antioxidant and anti-inflammatory activities which protect against OS and SDF [20]. The main effect of selenium on the male reproductive system is mediated via selenoprotein P and phospholipid hydroperoxide glutathione peroxidase (PHGPx) [21]. The recommended dietary allowance in adult is 55 μg/day [22]. Selenium deficiency has been detected in 20–40% of men with infertility [23]. Previous studies have reported improvement in sperm concentration, motility, and morphology in infertile men following selenium administration [24]. Another study has also demonstrated that selenium therapy protects sperm during cryopreservation and incubation in animal studies [25]. Therefore, this study was undertaken to investigate the influence of selenium therapy on semen measures, antioxidant capacity and SDF in infertile men with idiopathic OAT and fertile controls. To the best of our knowledge, this study is the first to assess the influence of selenium therapy on SDF in patients with idiopathic OAT.
Materials and Methods
Patients
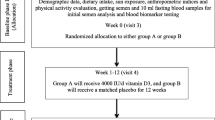
In this prospective controlled clinical study, sixty-five infertile men with idiopathic OAT and fifty fertile healthy control subjects were included in the study (7 patients dropped out). The patients were recruited from Fertility Clinic, Hilla, Iraq, from August 2018 to January 2019. A dedicated questionnaire was used to collect data. Medical history, physical examination, and investigations were undertaken by a fertility specialist to exclude existing causes of OAT. Patients received selenium 200 μg/day (America Medic & Science, Washington USA) orally as a single dose for six months. For all participants, seminal fluid analysis (WHO 2010 5th criteria) and SDF were assessed at baseline and after 6 months. We have used the selenium dose used in previous studies [26]. The calculation of sample size encompassed 80% power and 5% significance level and was estimated to be 42 for each group to achieve the desired statistical power. Ethical acceptance was issued by the University of Babylon, Iraq, and consent was received before recruitment (EC/9926).
Eligibility Criteria
Patients enrolled in the study had infertility of at least 12 months. OAT was diagnosed when abnormal sperm concentration, motility, and morphology according to WHO 2010 5th criteria were identified in semen analysis [27]. Patients with varicocele, infection, scrotal injury or surgery, cryptorchidism, azoospermia, systemic illness, endocrine disease, smoking, alcohol, female pathology, and recent administration of antioxidants in the last 6 months were excluded. The control group should have fathered a child in the last 24 months with a normal semen analysis.
Semen Analysis
All the participants were instructed to follow the standard protocol for abstinence, semen sample collection, and delivery to the laboratory to minimize sample collection and handling errors. Collection of semen samples was achieved by masturbation with sexual abstinence for 2 to 3 days, held at 37 °C for liquefaction, and then analyzed according to WHO guidelines 5th criteria [27]. All semen analyses were undertaken by the same researcher, and the average of two semen samples were collected at the start of the study and after 6 months was presented in the current study. OAT was defined as sperm concentration, motility, and morphology below 15 million/ml, 40%, and 4% respectively according to WHO guidelines. Samples that were delivered to the laboratory after more than 1 h of collection and incomplete samples, and samples with long abstinence were excluded from the study. All semen samples were processed and assessed within 1 h of delivery to the laboratory, and assessment conditions were standardized for all semen analyses.
Total Antioxidant Capacity and Catalase Activity
Seminal plasma was obtained by centrifugation of semen sample at 3000 rpm for 5 min and stored at − 20 °C. A colorimetric method was applied to assess TAC using the total antioxidant capacity assay kit (#E-BC-K136; Elabscience, Houston, TX, USA). Seminal plasma CAT activity was assessed using a CAT assay kit (#E-BC-K031, Elabscience). The tests were performed following the recommended protocol of the manufacturer.
Sperm Chromatin Dispersion Test
Sperm chromatin dispersion (SCD) was tested using the Halosperm kit (Halotech DNA, Madrid, Spain). Following acid denaturation and removal of nuclear proteins, sperm with fragmented DNA demonstrated a halo in contrast to sperm without DNA fragmentation which showed no halo. Bright-field microscopy with Diff-Quik staining was used to assess sperm with SDF. SDF level, defined as the percentage ratio of sperm with SDF to the total spermatozoa, was calculated using previously published methods [10, 28].
Statistical Analysis
Statistical analysis was accomplished with SPSS (v.24). The results were described as mean ± standard deviation. The normality of data was assessed using Kolmogorov–Smirnov test. Unpaired and paired t tests were used to compare means for normally distributed data. Mann–Whitney and Wilcoxon signed-ranked tests were used to compare means for non-normally distributed data. Correlations between seminal parameters and SDF were estimated using Spearman’s correlation coefficient. P value below 0.05 was adopted as the level for statistical significance.
Results
In this study, sperm concentration significantly increased (P < 0.001) in patients with idiopathic OAT following 6 months of selenium therapy as compared to baseline (Table 1). Sperm progressive motility and total motility also increased significantly in patients post-therapy (P < 0.001, P < 0.01 respectively). Seminal TAC and CAT activity significantly increased in patient following selenium therapy as compared to baseline (P < 0.01, P < 0.01 respectively) (Table 2). SDF percentage was significantly higher in patients group as compared to fertile controls (P < 0.001). In addition, SDF levels, there was a significant decrement in SDF levels in patients following selenium treatment (P < 0.001). The levels of SDF correlated significantly and inversely with sperm progressive motility (r = − 0.44, P = 0.003) and total motility (r = − 0.48, P = 0.001) (Table 3).
Discussion
Infertility is a global health problem and the number of couples presenting to fertility clinics is increasing. In addition to its physical impact, infertility imposes negative influences on the psychological, social, and financial aspects of the affected couples. Infertility also increases the burden on the healthcare system due to costly and long-term investigations and interventions including ART. Male factor contributes to approximately half of infertility cases. While some contributing factors for male infertility have been identified such as genetic, anatomical and endocrine diseases, the exact underlying mechanisms for IMI remain to be elucidated. Genetic, OS, and SDF have been suggested as possible mechanisms that contribute to IMI [29]. OS imposes adverse effects on sperm function as sperm membranes are characterized by the abundance of polyunsaturated fatty acids which represent a target for ROS-induced damage. OS attacks not only the sperm membrane but also the sperm DNA leading to SDF and impaired fertilization ability of sperm [30]. Therefore, SDF has been proposed as a new marker for male fertility that facilitates the assessment of male infertility in the clinical setting, guides the management, and provides prognostic data on the treatment outcomes. Selenium is a key player in many biological processes including spermatogenesis. Further, IMI represents a challenge for scientists and clinicians as the exact underlying mechanisms for IMI are unknown, and different therapies including selenium have been tried with variable success [3].
In the current study, selenium therapy for 6 months increased sperm concentration, and motility in patients with idiopathic OAT. Studies on the impact of selenium therapy on semen parameters in patients with idiopathic OAT are limited. Our findings are consistent with a study on infertile patients with asthenoteratospermia (AT) who received selenium (83 μg/day) for 6 months and demonstrated higher sperm concentration, motility, and normal morphology in comparison to baseline [1]. Similarly, increased sperm concentration, motility, normal morphology, and vitality following selenium therapy (59 μg/day) in infertile men for 3 months [31]. In a study on infertile patients with idiopathic AT, the administration of selenium (200 μg/day) and vitamin E (400 U/day) for 100 days resulted in an increment in sperm motility or morphology or both [19]. Recently, a controlled study on 60 patients with AT demonstrated a decrement in sperm apoptosis and increased sperm motility and viability following the administration of a similar combination of selenium and vitamin E [23].
Serum and semen selenium deficiency has been demonstrated in men with IMI [32]. Studies have also investigated the influence of selenium in combination with other oral antioxidants and reported an increment in one or more semen measures [3, 33,34,35,36,37]. However, there is a lack of consensus on the type of oral antioxidant, dose, duration of therapy, and the use of single or antioxidants combination in men with IMI. Our findings are congruent with previous studies which have reported an increased OS and reduced seminal antioxidant markers including TAC and CAT in men with IMI as compared to fertile controls [5, 12]. Previous studies have also illustrated increased seminal antioxidant capacity following antioxidant therapy [8, 10, 12, 18, 38]. In a study that has explored the impact of in vitro selenium treatment on semen quality in men with AT, sperm motility, and viability were increased and malondialdehyde levels were reduced [25]. In a recent study, the impact of selenium therapy (200 μg) and vitamin E (400 units) daily for 3 months resulted in a decrement in sperm apoptosis and superoxide level [23]. The increment in TAC and CAT activity demonstrated in the current study could be attributed to reduced ROS, OS, the antioxidant characteristics of selenium, and its influence on PHGPx and selenoprotein P.
In this study, the SDF level was higher in patients as compared to fertile controls and was reduced following selenium therapy for 6 months. In addition, there were significant and inverse correlations between SDF levels and sperm progressive and total motility. Studies on the impact of selenium on SDF in patients with idiopathic OAT are scarce. Recently, a study investigated the effect of selenium treatment for 6 months on semen parameters and SDF in men with autouimmune thyroiditis and illustrated an increment in all semen measures and a reduction in SDF levels as compared to pre-treatment values [1]. Another study investigated the influence of in vitro selenium treatment on semen measures, SDF, and mitochondrial membrane potential using different incubation times [25]. The study demonstrated higher sperm motility and mitochondrial membrane potential as well as lower SDF levels post-treatment.
The effectiveness of other oral antioxidants such as coenzyme Q10, vitamin C, E, B12, zinc, and l-carnitine on SDF in infertile men has also been reported in other studies. In previous papers, we have reported a decrement in SDF levels following coenzyme Q10 treatment (200 mg/day) for three months in patients with idiopathic OA and OAT in comparison to fertile controls [10, 39]. The levels of SDF also correlated with semen parameters, OS markers, and predicted pregnancy outcomes in men with IMI [40]. Other studies have reported similar effects for coenzyme Q10 on SDF values [41,42,43]. Combined antioxidants containing selenium, vitamin C, E, B12, zinc, and l-carnitine have been also used to reduce SDF levels in infertile men but the results were inconsistent [33, 44,45,46]. In a study on 20 infertile men with idiopathic AT who received a combination of oral antioxidants for 3 months, there were a reduction in SDF level as well as an improvement in sperm concentration and motility post-therapy [44]. In contrast, treatment with combined oral antioxidants resulted in an unexpected increment in SDF in infertile men who had at least two previous failures of IVF or ICSI [47]. High SDF levels are associated with male infertility, recurrent pregnancy loss, reduced pregnancy rate, and poor ART outcomes [30].
Previous studies have demonstrated a link between SDF level, ROS, and OS. In addition, selenium plays a role in the synthesis of RNA [48]. Therefore, the reduction of SDF levels observed in this study could be due to reduced OS, enhanced antioxidant enzyme activity, and the antioxidant and anti-inflammatory properties of selenium. The routine use of SDF test in the assessment of male infertility has not been recommended yet. However, some studies have recommended the use of SDF test in selected patients groups. Further, several clinical indications for SDF test in patients with infertility have been published [30]. High SDF levels are not only associated with reduced fertility and impaired sperm function but also with recurrent abortions and poor outcomes of infertility treatment including ART. In addition, increased SDF could be associated with increased rates of tumors and inherited diseases in the newborns [7]. Therefore, the reduction of SDF levels observed in our study could have beneficial effects for infertile men and their offspring.
Our study has some limitations. Dietary assessment of selenium and serum level of selenium were not explored although dietary studies are limited by the complex nature of food and recall bias. The pregnancy rate was also not included in this study due to time constraints of the follow-up but the primary endpoint for the study was the improvement in semen parameters and SDF level. Finally, the participants were selected from a single geographical area and therefore, the findings of the current study cannot be generalized to all areas worldwide. Additional large, multi-center studies are warranted to augment the evidence presented in this paper.
Conclusion
Treatment of infertile men with idiopathic OAT with selenium (200 μg/day) for 6 months improves sperm concentration, motility, seminal TAC, CAT, and reduces SDF level. Therefore, selenium therapy could be a promising therapy for infertile men with IMI and may enhance their fertility potential.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Cannarella R, Condorelli RA, Calogero AE et al (2021) Effects of selenium supplementation on sperm parameters and DNA-fragmentation rate in patients with chronic autoimmune thyroiditis. J Clin Med 10:3755. https://doi.org/10.3390/jcm10163755
Kumar N, Singh A (2015) Trends of male factor infertility, an important cause of infertility: a review of literature. J Hum Reprod Sci 8:191–196
Alahmar AT (2018) The effects of oral antioxidants on the semen of men with idiopathic oligoasthenoteratozoospermia. Clin Exp Reprod Med 45:57–66
Helli B, Kavianpour M, Ghaedi E et al (2020) Probiotic effects on sperm parameters, oxidative stress index, inflammatory factors and sex hormones in infertile men. Hum Fertil (Camb) 25:499–507. https://doi.org/10.1080/14647273.2020.1824080
Alahmar AT (2019) The impact of two doses of coenzyme Q10 on semen parameters and antioxidant status in men with idiopathic oligoasthenoteratozoospermia. Clin Exp Reprod Med 46:112–118. https://doi.org/10.5653/cerm.2019.00136
Negri L, Benaglia R, Monti E et al (2017) Effect of superoxide dismutase supplementation on sperm DNA fragmentation. Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol 89:212–218. https://doi.org/10.4081/aiua.2017.3.212
Agarwal A, Majzoub A, Baskaran S et al (2020) Sperm DNA fragmentation: a new guideline for clinicians. World J Mens Health 38:412. https://doi.org/10.5534/WJMH.200128
Alahmar A (2019) Role of oxidative stress in male infertility: an updated review. J Hum Reprod Sci 12:4–18. https://doi.org/10.4103/jhrs.JHRS_150_18
Esteves SC (2014) Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int Braz J Urol Off J Brazilian Soc Urol 40:443–453. https://doi.org/10.1590/S1677-5538.IBJU.2014.04.02
Alahmar A, Calogero AE, Sengupta P, Dutta S (2021) Coenzyme Q10 improves sperm parameters, oxidative stress markers and sperm DNA fragmentation in infertile patients with idiopathic oligoasthenozoospermia. World J Mens Health 39:346
Majzoub A, Esteves SC, Gosalvez J, Agarwal A (2016) Specialized sperm function tests in varicocele and the future of andrology laboratory. Asian J Androl 18:205–212. https://doi.org/10.4103/1008-682x.172642
Nadjarzadeh A, Shidfar F, Amirjannati N et al (2014) Effect of coenzyme Q10 supplementation on antioxidant enzymes activity and oxidative stress of seminal plasma: a double-blind randomised clinical trial. Andrologia 46:177–183. https://doi.org/10.1111/and.12062
Nadjarzadeh A, Sadeghi MR, Amirjannati N et al (2011) Coenzyme Q10 improves seminal oxidative defense but does not affect on semen parameters in idiopathic oligoasthenoteratozoospermia: a randomized double-blind, placebo controlled trial. J Endocrinol Invest 34:e224–e228. https://doi.org/10.3275/7572
Cho C-L, Agarwal A (2018) Role of sperm DNA fragmentation in male factor infertility: a systematic review. Arab J Urol 16:21. https://doi.org/10.1016/J.AJU.2017.11.002
Simon L, Zini A, Dyachenko A et al (2017) A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J Androl 19:80–90. https://doi.org/10.4103/1008-682X.182822
Ambar RF, Parekh N, Agarwal A (2020) Recent advances and controversies in diagnosing and treating male infertility. Fac Rev 9:22. https://doi.org/10.12703/R/22
Qiu Y, Yang H, Li C, Xu C (2020) Progress in research on sperm DNA fragmentation. Med Sci Monit Int Med J Exp Clin Res 26:e918746. https://doi.org/10.12659/MSM.918746
Beygi Z, Forouhari S, Mahmoudi E et al (2021) Role of oxidative stress and antioxidant supplementation in male fertility. Curr Mol Med 21:265–282. https://doi.org/10.2174/1566524020999200831123553
Moslemi MK, Tavanbakhsh S (2011) Selenium-vitamin E supplementation in infertile men: effects on semen parameters and pregnancy rate. Int J Gen Med 4:99–104. https://doi.org/10.2147/IJGM.S16275
Skoracka K, Eder P, Łykowska-Szuber L et al (2020) Diet and nutritional factors in male (In)fertility—underestimated factors. J Clin Med 9:1400. https://doi.org/10.3390/jcm9051400
Foresta C, Flohé L, Garolla A et al (2002) Male fertility is linked to the selenoprotein phospholipid hydroperoxide glutathione peroxidase. Biol Reprod 67:967–971. https://doi.org/10.1095/BIOLREPROD.102.003822
Stoffaneller R, Morse NL (2015) A review of dietary selenium intake and selenium status in Europe and the Middle East. Nutrients 7:1494–1537. https://doi.org/10.3390/NU7031494
Sabeti P, Pourmasumi S, Fagheirelahee N (2021) Effect of selenium and vitamin E on the level of sperm HSPA2+, intracellular superoxide anion and chromatin integrity in idiopathic asthenoteratozoospermia: a double-blind, randomized, placebo- controlled trial. Urol J 18:549–555. https://doi.org/10.22037/uj.v18i.6325
Agarwal A, Majzoub A (2017) Role of antioxidants in assisted reproductive techniques. World J Mens Health 35:77. https://doi.org/10.5534/wjmh.2017.35.2.77
Ghafarizadeh AA, Vaezi G, Shariatzadeh MA, Malekirad AA (2018) Effect of in vitro selenium supplementation on sperm quality in asthenoteratozoospermic men. Andrologia 50:e12869. https://doi.org/10.1111/and.12869
Safarinejad MR, Safarinejad S (2009) Efficacy of selenium and/or N-acetyl-cysteine for improving semen parameters in infertile men: a double-blind, placebo controlled, randomized study. J Urol 181:741–751. https://doi.org/10.1016/j.juro.2008.10.015
World Health Organization (2010) WHO laboratory manual for the examination and processing of human semen, 5th ed. WHO Press, Geneva, Switzerland:13–36
Zaazaa A, Adel A, Fahmy Y et al (2018) Effect of varicocelectomy and/or mast cells stabilizer on sperm DNA fragmentation in infertile patients with varicocele. Andrology 6:146–150
Nazari L, Salehpour S, Hosseini S et al (2021) Effect of antioxidant supplementation containing L-carnitine on semen parameters: a prospective interventional study. JBRA Assist Reprod 25:76–80. https://doi.org/10.5935/1518-0557.20200043
Alahmar A, Singh R, Palani A (2022) Sperm DNA fragmentation in reproductive medicine: a review. J Hum Reprod Sci 15:206–218
Morbat M, Hadi A, Hadri D (2018) Effect of selenium in treatment of male infertility. Exp Tech Urol Nephrol 1:1–4
Eroglu M, Sahin S, Durukan B et al (2014) Blood serum and seminal plasma selenium, total antioxidant capacity and coenzyme Q10 levels in relation to semen parameters in men with idiopathic infertility. Biol Trace Elem Res 159:46–51. https://doi.org/10.1007/s12011-014-9978-7
Alahmar A, Calogero AE, Singh R et al (2021) Coenzyme Q10, oxidative stress, and male infertility: a review. Clin Exp Reprod Med 48:97–104. https://doi.org/10.5653/cerm.2020.04175
Majzoub A, Agarwal A (2017) Antioxidant therapy in idiopathic oligoasthenoteratozoospermia. Indian J Urol 33:207–214
Ahmadi S, Bashiri R, Ghadiri-Anarip A, Nadjarzadehp A (2016) Antioxidant supplements and semen parameters: an evidence based review. Int J Reprod Biomed 14:729–736. https://doi.org/10.29252/ijrm.14.12.729
Li KP, Yang XS, Wu T (2022) The effect of antioxidants on sperm quality parameters and pregnancy rates for idiopathic male infertility: a network meta-analysis of randomized controlled trials. Front Endocrinol (Lausanne) 13:151. https://doi.org/10.3389/FENDO.2022.810242/BIBTEX
Bahmyari R, Ariafar A, Sayadi M (2021) The effect of daily intake of selenium, vitamin E and folic acid on sperm parameters in males with idiopathic infertility: a single-blind randomized controlled clinical trial. Int J Fertil Steril 15:8–14
Salvio G, Cutini M, Ciarloni A et al (2021) Coenzyme Q10 and male infertility: a systematic review. Antioxidants (Basel, Switzerland) 10:874. https://doi.org/10.3390/ANTIOX10060874
Alahmar AT, Sengupta P, Dutta S, Calogero AE (2021) Coenzyme Q10, oxidative stress markers, and sperm DNA damage in men with idiopathic oligoasthenoteratospermia. Clin Exp Reprod Med 48:150–155. https://doi.org/10.5653/CERM.2020.04084
Alahmar AT, Naemi R (2022) Predictors of pregnancy and time to pregnancy in infertile men with idiopathic oligoasthenospermia pre- and post-coenzyme Q10 therapy. Andrologia 54:e14385. https://doi.org/10.1111/AND.14385
Safarinejad MR (2012) The effect of coenzyme Q 10 supplementation on partner pregnancy rate in infertile men with idiopathic oligoasthenoteratozoospermia: an open-label prospective study. Int Urol Nephrol 44:689–700. https://doi.org/10.1007/s11255-011-0081-0
Huang C, Cao X, Pang D et al (2018) Is male infertility associated with increased oxidative stress in seminal plasma? A-meta analysis. Oncotarget 9:24494–24513. https://doi.org/10.18632/oncotarget.25075
Kobori Y, Ota S, Sato R et al (2014) Antioxidant cosupplementation therapy with vitamin C, vitamin E, and coenzyme Q10 in patients with oligoasthenozoospermia. Arch Ital Urol Androl 86:1. https://doi.org/10.4081/aiua.2014.1.1
Abad C, Amengual MJ, Gosálvez J et al (2013) Effects of oral antioxidant treatment upon the dynamics of human sperm DNA fragmentation and subpopulations of sperm with highly degraded DNA. Andrologia 45:211–216. https://doi.org/10.1111/and.12003
Gual-frau J, Abad C, Amengual MARÍAJ et al (2015) Oral antioxidant treatment partly improves integrity of human sperm DNA in infertile grade I varicocele patients. Hum Fertil (Camb) 1–5. https://doi.org/10.3109/14647273.2015.1050462
Majzoub A, Agarwal A, Esteves SC (2017) Antioxidants for elevated sperm DNA fragmentation: a mini review. Transl Androl Urol 6:S649-S653. https://doi.org/10.21037/tau.2017.07.09
Ménézo YJR, Hazout A, Panteix G et al (2007) Antioxidants to reduce sperm DNA fragmentation: an unexpected adverse effect. Reprod Biomed Online 14:418–421. https://doi.org/10.1016/S1472-6483(10)60887-5
Oguntibeju O, Esterhuyse J, Truter E (2009) Selenium: its potential role in male infertility. Pakistan J Med Sci 25:332–337
Acknowledgements
The author is very grateful to all the patients included in the current study for their invaluable participation and cooperation to complete this study. The author is thankful to the colleagues at the University of Babylon for their help and support during this study. The author is also grateful to the anonymous reviewers for their great help, comments, and review of the manuscript before submission.
Author information
Authors and Affiliations
Contributions
ATA has undertaken conceptualization, study design, data collection and analysis, wrote, and revised the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alahmar, A.T. The Effect of Selenium Therapy on Semen Parameters, Antioxidant Capacity, and Sperm DNA Fragmentation in Men with Idiopathic Oligoasthenoteratospermia. Biol Trace Elem Res 201, 5671–5676 (2023). https://doi.org/10.1007/s12011-023-03638-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03638-8