Abstract
Crohn’s disease (CD) and ulcerative colitis (UC) are two chronic relapsing inflammatory bowel diseases (IBD). Although there are several treatment options available to improve the symptoms of IBD patients, there is no effective treatment that provides a definitive solution. In the present study, we aim to investigate the antioxidative/anti-inflammatory effects of oral administration of boric acid and Bacillus clausii in a rat trinitrobenzenesulfonic acid (TNBS)-induced colitis model. The effects of boric acid and B. clausii were examined in serum and colon tissues with the help of some biochemical and histological analyses. Elevated inflammation and oxidative damage were found in the blood and colon tissue samples in the TNBS-induced group according to the complete blood count (CBC), tumor necrosis factor (TNF) alpha, interleukin-35 (IL-35), malondialdehyde (MDA), glutathione peroxidase (GPx), myeloperoxidase (MPO), nitric oxide (NO), and histological findings. Particularly, the highest IL-35 level (70.09 ± 12.62 ng/mL) in the combined treatment group, highest catalase activity (5322 ± 668.1 U/mg protein) in the TNBS-induced group, and lower relative expression of inducible nitric oxide synthase in the TNBS-induced group than the control group were striking findings. According to our results, it can be concluded that boric acid showed more curative effects, even if B. clausii probiotics was partially ameliorative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a group of chronic and idiopathic diseases of the small and large intestinal mucosa. Although its etiology is not yet known, it is characterized by two clinical phenotypes: ulcerative colitis (UC) and Crohn’s disease (CD) [1]. Ulcerative colitis is an intestinal disease that primarily affects the mucosal layer of the colon and rectum, resulting with inflammation and ulcers that continue on normal tissues without forming segments [2]. In Crohn’s disease, inflammation is typically segmental, asymmetric, and transmural. As disease severity increases, complications (strictures, fistulas, and abscesses) increase and with nearly half of patients requiring surgical intervention [3].
Currently, there are a variety of treatment options to improve the symptoms of IBD patients, although there is no effective treatment that provides a definitive solution. In addition, the development of negative side effects such as excessive suppression of the immune system, high risk of infection, osteoporosis, osteonecrosis, and myopathy due to the mandatory long-term use of steroid medications in IBD is a major concern [4].
Despite many comprehensive studies, no clear model has been found for the initiation, development, and spread of IBD. A disturbance in the balance between beneficial and harmful bacteria in the microflora, genetic predisposition, and environmental factors lead to a dysregulation of immune mechanisms. This situation, which leads to intense infiltration of immune cells into the mucosa, produces an irreversible immune response [5]. Infiltration of neutrophils and monocytes is the result of both types of IBD. Myeloperoxidase (MPO) is one of the major inflammatory markers secreted by intracellular granules of activated neutrophils and to a lesser extent monocytes [6]. Nitric oxide is synthesized by various cell types through a reaction catalyzed by nitric oxide synthase [7,8,9]. The increase in the levels of nitric oxide (NO) and inducible nitric oxide synthase (iNOS) expressions is associated with inflammation [10].
Studies have shown that cytokines play an important role in IBD. In particular, anti-tumor necrosis factor-alpha (TNF-α) antibody therapy, which is now widely used in IBD treatment, has shown that TNF-α plays a key role in the pathogenesis of UC and CD [11]. The potential therapeutic efficacy of interleukin-35 (IL-35), which has emerged as an intriguing cytokine in recent years, particularly in autoimmune diseases, has been investigated in several animal models [12]. It is also known that IL-35 reduces and controls active colitis by suppressing the cytokine response on T cells [13].
Oxidative stress plays an important role in the pathophysiology of IBD, although the specific pathways that cause cellular damage are not fully understood [5]. Endogenous antioxidant mechanisms such as reduced glutathione (GSH), glutathione peroxidase (GPx), catalase, and superoxide dismutase (SOD) are impaired in inflammatory bowel diseases, and oxidative stress results with increase in lipid peroxidation [14,15,16,17]. On the other hand, high concentrations of NO can react with the superoxide radical and converted to peroxynitrite radicals, which leads to increase in oxidative stress [18].
Boron, the fifth element of the periodic table, reacts with oxygen and transforms into inorganic forms such as boric acid (BA) and borax. Boric acid cannot be metabolized by humans and animals because it requires high energy to break the oxygen bond with boron [19]. Although the biochemical mechanisms of BA are not fully understood, studies have shown that BA has antioxidant, anti-inflammatory, and anti-apoptotic properties [20,21,22,23]. According to Kar et al. (2019), BA exhibits antioxidant properties by breaking down protons on oxidant molecules or taking free radicals to its structure. The fact that there has not been much recent research in the field of health has made BA a remarkable molecule for researchers.
Probiotics, according to the World Health Organization, are living microorganisms, when supplied in sufficient quantities provide significant benefits to the host [24]. Probiotics are particularly involved in mucosal protection and gut barrier integrity and have a reciprocal relationship with the host by secreting a range of secondary metabolites. B. clausii as a probiotic is approved in the literature as an over-the-counter medical supplement under the name Enterogermina® and contains only spores of the species B. clausii [25]. In one study, the probiotic B. clausii was reported to suppress oxidative stress [26], and in another study, it was found that affect genes involved in mechanisms such as apoptosis, inflammation, and the immune system [27].
The aim of our study is to improve the quality of life of people with IBD by developing new treatment strategies. In this context, to investigate the antioxidant and/or anti-inflammatory effects on the 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced IBD rat model, BA and B. clausii were administered orally, individually, or in combination. In the current study, we present the first data on the effects of BA in the IBD rat model.
Material and Methods
Chemicals
The chemicals which were used in the study are as follows: cadmium granules were from Fluka (Germany). Potassium chloride (KCl) was purchased from Merck (Germany). Enterogermina (Sanofi, Italy) (for B. clausii spores) was purchased from local pharmacy. Ditiotreitol (DTT), boric acid, and Tris were from AppliChem (Spain). Sulphuric acid and acetic acid were purchased from Riedel-de Haën (Germany). Inducible nitric oxide synthase 2 (NOS2) primer and seconder antibodies were from Santa Cruz (USA). Actin primer and seconder antibodies were from ABclonal (USA). All other chemicals were purchased from Sigma-Aldrich (USA). Standard commercial rat pellets was purchased from DSA Agrifood Products Inc. (Kırıkkale, Turkey).
Animals
Forty-five male Sprague Dawley rats, 8 weeks old, weighing 250–300 g, were housed at a constant temperature of 22 ± 3 °C and humidity of 50 ± 10%, the day/night cycle was adjusted for 12 h/12 h, and were ad libitum access to chow. All animal research protocols in this study were approved by the Institutional Ethics Committee (HADYEK, Protocol # 778/2019). The experimental animals were fed with standard commercial rat pellets: 23.5% crude protein, 5.97% crude cellulose, 2.4% crude fat, 1–2% vitamins, and minerals; 3% trace elements, manganese, selenium, iron, zinc, cobalt, and iodide (270 kcal 100 g−1). The care and surgical interventions of the rats were carried out at Eskişehir Osmangazi University (ESOGU) Medical and Surgical Experimental Research and Application Centre (TICAM), biochemical analyses were carried out at ESOGU Medical Biochemistry Department, and histological examinations were performed at ESOGU Histology and Embryology Department.
Induction of Colitis
Colitis was induced according to the method as previously described by Kankuri et al. (1999). Briefly, in this model, TNBS was prepared at a dose of 120 mg/kg in 50% ethanol and injected to the rats under anesthesia by entering 8 cm into the rectum using a plastic cannula. The rats were held upside down for 30 s to ensure that TNBS reached the descending colon. At the end of the 30 s, the excess TNBS remaining in the rectum and colon was discarded and the rats were placed in the cages.
Experimental Design
The rats were randomly divided into five groups, each consisting of 9 animals. Groups are organized as follows: control, IBD, IBD + boric acid (IBD + BA), IBD + Bacillus clausii (IBD + BC), and IBD + boric acid + Bacillus clausii (IBD + BA + BC). On the first day of the study, physiological saline (0.9% NaCl solution) was performed by intracolonic injection to the control group and the TNBS (120 mg/kg dissolved in 50% ethanol) was applied by intracolonic injection to the IBD, IBD + BA, IBD + BC, and IBD + BA + BC groups. From the second day to the fifth day of the study, 2 mL saline solution was orally administrated to the control and IBD groups; BA (100 mg/kg) [23, 29,30,31], Bacillus clausii (1 × 109 CFU/mL/100 g) [26], and the combination of the BA and B. clausii were applied by gavage to the IBD + BA, IBD + BC, and IBD + BA + BC groups, respectively. Twenty-four hours after the last dose of the treatments, rats were sacrificed and colon tissues were collected.
Analysis of Blood Biochemical Profile and Complete Blood Count
To evaluate possible liver and kidney function changes, serum enzyme activities (alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP)) and also creatinine and blood urea nitrogen (BUN) levels were analyzed by using the Auto Analyzer System (Roche Cobas 702 modular, Mannheim, Germany) on the same day. ALT, AST, and ALP activities were expressed as U/L, and creatinine and BUN levels were as mg/dL. Hemoglobin (Hb), RBC, WBC, neutrophil, lymphocyte, and monocyte counts were analyzed by Automated Hematology Analyzer (Sysmex NX1000, USA) and expressed g/dL or × 103/μL.
Analysis of TNF-α and IL-35 Levels of Serum Samples
To investigate the possible effects of treatments on IBD, TNF-α (a pro-inflammatory cytokine) and IL-35 (an anti-inflammatory cytokine) levels were analyzed by using commercial ELISA kits (Cat. No. E0764Ra, Bioassay Technology Laboratory, China, for TNF-α; Cat. No. E2118Ra, Bioassay Technology Laboratory, China, for IL-35) and expressed as ng/mL.
The Measurement of Colon Tissue MPO Activities
Myeloperoxidase activity, one of the indicators of neutrophil infiltration and inflammation, was analyzed in intestinal tissue as previously described [32]. The method is based on measuring the oxidation of 3,3′,5,5′-tetramethylbenzidine (TMB), a synthetic substrate, by a reaction catalyzed by myeloperoxidase. Briefly, the colon tissue samples were homogenized in ice-cold 50 mM phosphate buffer (pH 7.4), in the ratio of 1 g wet tissue to 9 mL buffer, and homogenates were centrifuged at 5500 × g for 5 min at 4 °C. After the supernatants were discarded, pellets were suspended with 50 mM phosphate buffer (pH 6.0) (contains hexadecyltrimethylammonium (HETAB)) and re-homogenized immediately. A mixture was prepared by adding 0.5 mL of 160 mM potassium phosphate buffer (pH 5.4), 0.33 mL of distilled water, 0.02 mL of homogenate, and 0.1 mL of 16 mM TMB and incubated at 37 °C for 2 min. After the incubation, 0.05 mL of H2O2 was added to the mixture and the reaction was started. Absorbance change was recorded at 655 nm for 5 min and results were expressed as U/mg protein.
The Measurement of Colon Tissue NO Levels
Nitric oxide levels were analyzed according to the method determined by Cortas and Wakid [33]. The method is based on the principle of converting nitrate (NO3−) to nitrite (NO2−) with copper-coated cadmium granules and measuring nitrite levels. Tissue samples were homogenized in ice-cold 50 mM phosphate buffer (pH 7.4), in the ratio of 1 g wet tissue to 9 mL buffer, and centrifuged at 4000 × g for 20 min at 4 °C. To prepare the mixture, 0.25 mL of supernatant, 1.25 mL of 55 mM sodium hydroxide (NaOH), and 1 mL of 75 mM zinc sulfate (ZnSO4) were added into the tubes. Ten minutes following the incubation, mixtures were centrifuged at 3500 × g for 10 min and the second supernatant was used for the next step. One milliliter of glycine–NaOH buffer, 1 mL of the second supernatant, 2 mL of distilled water, and cadmium granules were added into the mixtures. After 90 min of incubation, 2 mL of the third supernatant, 0.5 mL of distilled water, 1 mL of sulphanilamide, and 1 mL N-naphthyl ethylene diamine were added into the tubes and kept under the room temperature for 60-min incubation. Following the incubation, samples were spectrophotometrically measured at 545 nm and expressed as µmol/mg protein by using a standard curve generated with NaNO2.
The Measurement of Colon Tissue MDA Levels
As one of the important last products of lipid peroxidation, malondialdehyde (MDA) levels were determined as previously described [34]. The method is based on the color reaction of MDA with incubation of thiobarbituric acid (TBA) at pH 3.5 and 95 °C. Tissue samples were homogenized in ice-cold 1.15% KCl solution, in ratio 1 g wet tissue and 9 mL KCl, and homogenates were centrifuged at 1500 × g for 15 min at 4 °C. A mixture was prepared by adding 0.2 mL of supernatant, 0.1 mL of 8.1% sodium dodecyl sulfate (SDS), 0.75 mL of 20% acetic acid, 0.75 mL of 0.8% of TBA, and 0.2 mL of distilled water to adjust the volume 2 mL. The mixture was incubated in the boiling water for 1 h and centrifuged at 1000 × g for 10 min. The absorbance of the mixture (purple colored product) was spectrophotometrically analyzed at 532 nm and results were expressed as nmol/mg protein by using the standard curve generated with 1,1,3,3-tetraethoxypropane.
The Measurement of Colon Tissue Catalase Activities
The measurement of catalase activity is based on the principle of following the rate of catalysis of hydrogen peroxide by catalase to water and oxygen [35]. Tissue samples were homogenized with ice-cold 50 mM phosphate buffer (pH 7.0) and centrifuged at 700 × g for 10 min at 4 °C. To prepare the mixture, ethanol (0.17 M for the final concentration) was added to the supernatant and incubated in cold water for 30 min. Following 30 min, 10% Triton X-100 was added (1% for final concentration) into the supernatants. The supernatants were diluted in the ratio of 1/100 and used in the measurement. In order to analyze catalase activities, 0.3 mL of H2O2 was added to 0.6 mL of diluted supernatants and decreasing of absorbance was recorded at 240 nm. The activities of catalase were expressed as a U/mg protein.
The Measurement of Colon Tissue GPx Activities
A commercial kit (Cayman Chemical, Cat. No. 703102) was used for the measurement of GPx activity. The principle of the measurement is depended on the consumption of NADPH during the interconversion of reduced glutathione and oxidized glutathione by the enzymes GPx and glutathione reductase (GR). The decreased levels of NADPH are directly proportional to the GPx activity. The GPx activities were expressed as U/mg protein.
Western Blot Analysis of Colon Tissue Samples
Colon tissue specimens were homogenized in the Eppendorf tubes for each group and protein levels were adjusted to 50 µg/µL. Proteins were separated by SDS-PAGE, transferred to the membranes, and blocked with bovine serum albumin (BSA) contained blocking solution. The membranes were then incubated in iBind™ Flex for 2.5 h with anti-iNOS and anti-actin antibodies. Luminol-Enhancer solution and peroxide solution were used for the monitoring of the protein bands on both membranes and the bands were photographed by an imaging system. Western blot analysis was repeated for three times. ImageJ program was used to convert the intensities of the formed bands into numerical data. Results are given as the relative expression of iNOS proteins.
The Measurement of Colon Tissue Protein Levels
The total protein level in tissue homogenates was determined according to the Biuret method reported by [36]. The principle of this method is based on the formation of a blue-violet complex of copper salts with compounds containing two or more peptide bonds under alkaline conditions. The absorbance of the formed colored complex was measured spectrophotometrically at a wavelength of 545 nm. Bovine serum albumin was used to generate the standard curve.
Histological Analysis
For histological analysis, the intestinal tissue samples were kept in 10% buffered formaldehyde solution in the dark until the analysis day. Specimens were exposed to ascending graded ethyl alcohol for dehydration. Following the dehydration, tissue samples were kept in xylol and then embedded in paraffin. The paraffin blocks were cut to 5 µm in thickness and stained by the hematoxylin–eosin technique in order to evaluate the histopathological changes. Tissue slices were examined under the light microscope (Olympus BH-2) and the photographs were taken by Olympus DP-70 digital camera. The severity of the damages of the colon tissue specimens were expressed as 0 (no damage), 1 (mild damage), 2 (moderate damage), and 3 (high damage) by scoring.
Statistical Analysis
GraphPad Prism 7 was used in the statistical analysis of the study. One-way ANOVA and Kruskal–Wallis tests were performed according to the results of the Shapiro–Wilk normality test. In the one-way ANOVA test, the differences between the groups were determined according to the Tukey test, while in the Kruskal–Wallis test, differences between the groups were determined according to the Dunn’s test. Results were given as mean (± standard deviation). p < 0.05 was considered to be significant, p < 0.01 was highly significant, and p < 0.001 was a very high significant difference.
Results
Serum AST, ALT, and ALP Activities
Serum AST activities were found to be lower in the IBD + BA, IBD + BC, and IBD + BA + BC groups compared to the control group (p < 0.05, p < 0.01, and p < 0.01, respectively). Also, in the IBD + BA + BC group, AST activities were significantly lower than in the IBD group (p < 0.05) (Table 1). According to the statistical analyses, ALT levels decreased significantly in the IBD + BA, IBD + BC, and IBD + BA + BC groups (p < 0.05, p < 0.01, and p < 0.05, respectively) (Table 1). The ALP activity values of the IBD group were found to be higher and significantly different from the control group (p < 0.01). On the other hand, a decrease was detected in the ALP activity of the IBD + BC and IBD + BA + BC groups (p < 0.05).
Serum Creatinine and BUN Levels
According to statistical analyses, the mean values of creatinine levels were found to be higher in the IBD + BC (0.42 ± 0.07 mg/dL) and IBD + BA + BC (0.39 ± 0.07 mg/dL) groups compared to the control (0.29 ± 0.03 mg/dL) group, p < 0.001 (Table 1). Similarly, BUN levels were higher in the IBD + BC (31 ± 8 mg/dL) and IBD + BA + BC (33 ± 10 mg/dL) groups than the control (22 ± 3 mg/dL) group, p < 0.01 (Table1).
Complete Blood Count Results
According to the statistical analysis, Hb levels of the IBD (15 ± 0.6 g/dL), IBD + BA (14 ± 1 g/dL), and IBD + BA + BC (15 ± 0.6 g/dL) groups were found to be lower compared to the control group (17 ± 1.2 g/dL), p < 0.01 (Table 2). Statistical findings showed that RBC levels of the IBD + BC group (10 ± 0.5 × 103/µL) were significantly higher than the IBD, IBD + BA, and IBD + BA + BC groups, p < 0.05 (Table 2). Although WBC levels were significantly increased in the IBD group (9 ± 3 × 103/µL, p < 0.01), the highest WBC levels were found in the IBD + BC group (10 ± 1.7 × 103/µL, p < 0.001) (Table 2). The neutrophil levels of the IBD (2.25 ± 0.8 × 103/µL) and IBD + BC (2.55 ± 1.8 × 103/µL) groups were found to be approximately threefold higher than the control group (0.79 ± 0.1 × 103/µL). Even though the neutrophil levels of the IBD + BA and IBD + BA + BC groups were found to be roughly twofold higher than the control group, no significant differences were detected between the groups (Table 2). In accordance with the statistical analyses, the lymphocyte levels of the IBD + BC group were found to be significantly higher than the control group (p < 0.05) (Table 2). On the other hand, lymphocyte levels of the combined treatment group were detected to be significantly lower compared to the IBD + BC group (p < 0.001) (Table 2). The monocyte levels were found to be significantly higher in the IBD (1.31 ± 1.27 × 103/µL), IBD + BC (1.69 ± 0.6 × 103/µL), and IBD + BA + BC (1 ± 0.79 × 103/µL) groups than the control group (0.03 ± 0.01 × 103/µL), while there were no significant differences found between the control and BA-treated groups (Table 2). TNBS administration significantly increased the N/L ratio compared to the control group (0.47 ± 0.2 vs 0.18 ± 0.05, p < 0.05) (Table 2).
Serum TNF-α and IL-35 Levels
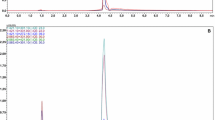
According to the statistical analysis, the mean value of serum TNF-α levels of the IBD group was 45.29 ± 4.57 ng/mL and it was significantly higher than the control group (35.50 ± 2.70 ng/mL, p < 0.001). Administration of BA and B. clausii probiotics led to a reduction in TNF-α levels of the IBD + BA (35.51 ± 4.20 ng/mL), IBD + BC (36.38 ± 4.12 ng/mL), and IBD + BA + BC (39.9 ± 2.06 ng/mL) groups compared to the IBD group, p < 0.05 (Fig. 1a). TNBS administration significantly decreased the serum IL-35 levels in the IBD group (39.27 ± 13.78 ng/mL, p < 0.01) compared to the control group (59.80 ± 8.36 ng/mL). The highest IL-35 levels were detected in the combined treated group (70.09 ± 12.62 ng/mL) and the levels were significantly higher than the IBD (39.27 ± 13.78 ng/mL), IBD + BA (52.99 ± 9.59 ng/mL, p < 0.05), and IBD + BC (51.11 ± 12.82 ng/mL, p < 0.05) groups, p < 0.05 (Fig. 1b).
Pro-inflammatory and anti-inflammatory cytokine levels in serum. a Serum TNF-α levels of the rats; b serum IL-35 levels of the rats. a*, a**Significant difference vs control (*p < 0.01; **p < 0.001); b, b**significant difference vs IBD (p < 0.05; **p < 0.001); csignificant difference vs IBD + BA (p < 0.05); dsignificant difference vs IBD + BC (p < 0.05). TNF-α, tumor necrosis factor-alpha; IL-35, interleukin-35; IBD, inflammatory bowel disease; IBD + BA, inflammatory bowel disease + boric acid; IBD + BC, inflammatory bowel disease + Bacillus clausii; IBD + BA + BC, inflammatory bowel disease + boric acid + Bacillus clausii
MDA Levels, Catalase, and GPx Activities of Colon Tissues
Highest MDA levels were observed in the IBD group yet the difference was not significant compared to the control group. Conversely, the MDA levels were found significantly lower in the IBD + BA (13.37 ± 5.20 nmol/mg protein), IBD + BC (14.02 ± 2.89 nmol/mg protein), and IBD + BA + BC (13.68 ± 4.07 nmol/mg protein) groups than in the IBD (21.51 ± 7.65 nmol/mg protein) group, p < 0.05 (Fig. 2a). According to the statistical analysis, in spite of the catalase activities were found to be higher in all groups compared to the control group (1774 ± 733 U/mg protein), the significant differences were detected in the IBD (5322 ± 668 U/mg protein, p < 0.001), IBD + BA (4911 ± 1392 U/mg protein, p < 0.001), and IBD + BA + BC (3958 ± 1387 U/mg protein, p < 0.01) groups. Probiotic administration significantly decreased the catalase activities in the BC group (p < 0.001) (Fig. 2b). GPx activities of the colon tissues were observed to be approximately twofold lower in the IBD (6.1 ± 0.94 U/mg protein, p < 0.05), IBD + BC (5.18 ± 1.21 U/mg protein, p < 0.001), and IBD + BA + BC (6.19 ± 2.56 U/mg protein, p < 0.05) groups than the control group. Also, the decreased GPx activities were detected in the IBD + BA group compared to the control group but the decrease was not significant (Fig. 2c).
Oxidative stress and antioxidant system related parameters in colon tissue samples of rats. a MDA levels in colon tissue; b catalase activities in colon tissues; c GPx activities in colon tissues. a, a*, a**Significant difference vs control (p < 0.05; *p < 0.01; **p < 0.001); b, b*significant difference vs IBD (p < 0.05; *p < 0.01). MDA, malondialdehyde; GPx, glutathione peroxidase; IBD, inflammatory bowel disease; IBD + BA, inflammatory bowel disease + boric acid; IBD + BC, inflammatory bowel disease + Bacillus clausii; IBD + BA + BC, inflammatory bowel disease + boric acid + Bacillus clausii
MPO and NO Levels and Relative Expression of iNOS of Colon Tissues
The mean values of MPO activities of the IBD (0.026 ± 0.016 U/mg protein, p < 0.001) and BC (0.024 ± 0.016 U/mg protein, p < 0.001) groups were found to be significantly higher compared to the control group. On the other hand, the BA and combined treatments led to a decrease in MPO activities against TNBS-induced colitis, but there was no significantly differences detected between the groups (Fig. 3a). Administration of TNBS led to increase in NO levels of the IBD (9.13 ± 3.84 µmol/mg protein, p < 0.001) and IBD + BA (6.99 ± 0.75 µmol/mg protein, p < 0.01) groups compared to the control group (5.05 ± 0.77 µmol/mg protein). The colon tissue NO levels were found to be significantly lower in the IBD + BC group than in the IBD group (5.86 ± 0.57 µmol/mg protein, p < 0.05) (Fig. 3b). Statistical analyses of relative iNOS protein expressions of colon tissues showed that there were no significant differences between the groups. Interestingly, relative iNOS expression in all the groups was detected lower compared to the control group (Fig. 3c).
Inflammatory process associated parameters in colon tissue samples of the rats. a MPO activities in colon tissues; b NO levels in colon tissues; c relative protein expression of iNOS in colon tissues. a*, a**Significant difference vs control (*p < 0.01; **p < 0.001); bsignificant difference vs IBD (p < 0.05). MPO, myeloperoxidase; NO, nitric oxide; iNOS, inducible nitric oxide synthase; IBD, inflammatory bowel disease; IBD + BA, inflammatory bowel disease + boric acid; IBD + BC, inflammatory bowel disease + Bacillus clausii; IBD + BA + BC, inflammatory bowel disease + boric acid + Bacillus clausii
Histological Evaluation
According to the histological examinations of the colon tissue sections, the control group exhibited to be normal histological architecture with the lamina epithelialis, lamina propria, lamina mucosa, and lamina muscularis layers, in addition to rich goblet and epithelial cells (Fig. 4a). On the contrary, severe inflammation, epithelial damage, edema, vascular dilatation, and congestion were observed from the colon tissues of the IBD group (Fig. 4b; Table 3). Colonic architecture deformation, inflammation, loss of goblet and epithelial cells, vascular dilatation, and congestion were decreased by BA administration compared to the IBD group (Fig. 4c; Table 3). Less colonic tissue renewal was observed in the B. clausii-treated group compared to the IBD + BA group. Also, intense inflammation, edema, cellular loss, and dilatation were noted of the colon tissue sections of the BC group (Fig. 4d; Table 3). Histopathological examinations of the combined treatment group showed similarity with the IBD + BC group by immense infiltration, epithelial damage, edema, and cellular loss (Fig. 4e; Table 3).
Histological examination in colon tissue sections of the rats (HE, scale bar: 200 µm, 100 µm, 50.0 µm). a Control group had normal histological appearance with rich goblet cells (), lamina epithelia (le), lamina propria (lp), and lamina muscularis mucosa (lmm); b IBD group had intense damage in mucosa (►), loss of goblet cells, intense damage in lamina propria, edema (), congestion (c), intense edema in submucosa (
 ), intensive inflammation (inf), dilatation (d); c IBD + BA group had improved goblet cells, partial damage (O), partial edema in tunica submucosa (
), intensive inflammation (inf), dilatation (d); c IBD + BA group had improved goblet cells, partial damage (O), partial edema in tunica submucosa (
 ), and decreased inflammation (inf); d IBD + BC group had intensive damage (►), cellular loss, edema (), intense damage in lamina propria, edema in submucosa (
), and decreased inflammation (inf); d IBD + BC group had intensive damage (►), cellular loss, edema (), intense damage in lamina propria, edema in submucosa (
 ), inflammation (inf), and dilatation (d); e IBD + BA + BC group had intensive damage in epithelia (►) and cellular loss, intensive damage and edema in lamina propria (), edema in submucosa (
), inflammation (inf), and dilatation (d); e IBD + BA + BC group had intensive damage in epithelia (►) and cellular loss, intensive damage and edema in lamina propria (), edema in submucosa (
 ), inflammation (inf), and dilatation (d). TM, tunica mucosa; TSM, tunica submucosa; TMS, tunica muscularis; TA, tunica adventitia
), inflammation (inf), and dilatation (d). TM, tunica mucosa; TSM, tunica submucosa; TMS, tunica muscularis; TA, tunica adventitia
Discussion
Inflammatory bowel diseases are chronic and idiopathic diseases of the distal and mucosa of the intestine and are characterized by two clinical phenotypes, ulcerative colitis and Crohn’s disease [1]. Depending on the long-term usage of drugs in the treatment of IBD, the occurrence of some side effects such as suppression of the immune system and high risk of infection are significant problems [4]. Additional treatments may be required to eliminate the side effects of the drugs. In this respect, it is critical to determine an ideal agent with minimal side effects for the treatment of IBD.
In the present study, TNBS was administered to generate a colitis model. Blood and tissue samples were taken from rats at the last day of the animal experiments. Biochemical analyses and histological examinations were carried out to evaluate the possible protective effects of treatments. Serum ALT, AST, and ALP activities and BUN and creatinine levels were analyzed as liver and kidney function tests. It is shown that TNBS administration led to abnormalities in liver function tests [37, 38]. Decreased expression of intestinal ALP (IAP) was found even in non-inflamed tissues of the IBD patients compared to the control group. Moreover, administration of exogenous IAP leads to reduction on inflammatory effects of IBD in IAP knock-out mice [39]. According to our findings, in contrary, TNBS did not affect the liver function tests apart from the ALP activities. We consider that a mechanism underlying the increased ALP levels might be associated with the intestinal damage that occurred following by TNBS administration. According to Malo et al. [40], intestinal ALP is released through the damaged tissue into the blood stream and the activities are increased in serum. One outcome that can be clearly understood according to our result is liver function tests did not affect from the BA and B. clausii treatments. One outcome from our findings is that the BA and B. clausii treatments did not lead to abnormalities in liver function tests. According to the results we obtained, neither TNBS nor BA administration did affect the kidney function tests. Remarkably, BUN and creatinine levels showed a tendency to increase in orally B. clausii applicated groups. This result may be related to the fact that TNBS impaired intestinal barrier integrity; thus, B. clausii spores or the vegetative forms may infiltrate the bloodstream, reach the kidney tissues, and lead to deflection in kidney function tests. According to a previously published study, oral administration of Bacillus subtilis spores was shown that spores could spread to the other organs in different hours [41].
Elevated levels of WBCs, monocytes, lymphocytes, and neutrophils are associated with the inflammatory response in IBD [42,43,44]. In addition, the N/L ratio has been reported as a significant indicator of the total inflammatory status of the body that peaking particularly in active periods of colitis [45]. In our study, the increased levels of WBC, neutrophil and monocyte count, and the N/L ratio in the IBD group are consistent with the previous studies. Boric acid and ampicillin combination leads to a decrease in the WBC levels [46], while probiotic supplementation causes to increase in the WBC, lymphocyte, and neutrophil levels [47]. According to our findings, the WBC, neutrophil, monocyte levels, and the N/L ratio tended to decrease in the BA-treated group. On the other hand, these biomarkers were detected to be significantly elevated in the B. clausii-treated groups. These findings are in a harmony with histological examinations and scorings. We consider that BA meliorated the disrupted intestinal morphology and thus suppressed the inflammatory response. In contrast, B. clausii may have been infiltrated to the submucosa in the impaired barrier integrity and acted as an unfamiliar substance to the host, and thus increased the inflammatory response.
IBD is a significant disease that leads to an imbalance between the anti-inflammatory and pro-inflammatory cytokines in serum. TNF-α, as a pro-inflammatory cytokine, has been reported that increase in almost all types of IBD models [48, 49]. On the other hand, it was demonstrated that IL-35, an inhibitory cytokine, plays a significant role in the immunosuppressive activities of regulatory T cells (Treg cells). Treg cells, a subpopulation of CD4+ cells, are involved in prevention of chronic inflammatory diseases such as IBD [50]. It was shown that TNBS or DSS administration leads to depletion in IL-35 levels [51, 52]. It is understood from our findings that the TNBS associated colon tissue damage led to the immune response by causing an increase in serum TNF-α levels and a decrease in IL-35 levels. Cao et al. [53] showed that BA administration caused a decrease in TNF-a levels and expression. This result on the decrease in TNF-α level by BA administration is also similar to the results of our previous studies on different animal models [23, 30]. In the present study, serum TNF-α level was found significantly decreased by following BA administration. We considered that BA showed an anti-inflammatory effect on Thp-1 cells by suppressing the release and expression of TNF-α. Additionally, it has known that monocytes infiltrate into tissue in inflammatory conditions and transform into macrophages which releases TNF-α. Thus, according to our CBC findings, decreased monocyte count may have caused fewer macrophages transformation and resulted in slight TNF-α release in the BA administered group. Depending on the pathophysiology of the disease, probiotics keep the immune system under control by modulating cellular and humoral immune responses [54]. TNF-α levels were observed lower following the B. clausii administration in postmenopausal osteoporotic rats [55]. In our study, B. clausii administration led to a significant decrease in TNF-α levels compared to the IBD group. Following an extensive literature review, no study was found in which BA and B. clausii was applied, and IL-35 levels were analyzed. Thus, in our study, increased IL-35 levels of the treatment groups are striking findings. We consider that the administration of BA and B. clausii did not heal only the mucosal tissue but also improved the anti-inflammatory effects of Treg cells.
In our study, MPO activity, NO level, and relative expression of iNOS were investigated in relation to the inflammatory status of colon tissue. According to our analyses, which were performed on colon tissue, we found that MPO activity and NO level were significantly increased following intrarectal TNBS administration. Remarkably, however, iNOS expression was lower in the IBD group. In vivo, in vitro, and clinical studies have reported that NO is generated due to increased iNOS levels during the active phase of IBD [56, 57]. This discordance, particularly between the expression of iNOS and NO levels, was an unexpected result. According to our findings, BA and combined treatments led to decrease in MPO levels. This finding related to MPO level was in consistent with our histological analyses. We consider that BA reduces the number of neutrophils and monocytes and obstructs their migration into the intestinal tissue by lowering TNF-α levels. On the other hand, iNOS expression tended to increase while no significant differences were detected in terms of NO levels in BA administered group. In an in vitro study, it was proved that all strains of Bacillus clausii increase nitrite production in active peritoneal cells. Researchers, who attributed that nitrite production to iNOS induction, suggested that increased IFN-γ levels are responsible for the stimulation of iNOS [58]. On the other hand, no data was found in the literature associated with the measurement of MPO activity following B. clausii administration. In our study, a slight decrease in MPO activities and NO levels was obtained in the BC group, while there was an increase in iNOS expression. According to these results, inconsistent between the iNOS expression and NO levels might be explained with iNOS enzyme activity. So, BA and B. clausii treatments might have affected the iNOS expression but not iNOS activity.
TNBS-induced colitis studies and clinical researches were associated with high MDA levels [59,60,61,62]. In the present study, we demonstrated that MDA levels tended to increase in TNBS administered group. Research studies showed that BA administration leads to a decrease in oxidative stress. Cengiz [63] attributed the decrease in MDA levels to the free radical scavenging properties of BA, while Ince et al. (2011) attributed to the antioxidant system enhancer features of BA. In our previous experimental animal and in vitro studies, we showed that BA has a significant effect on the reduction of MDA levels [22, 23, 29, 31, 65]. In the present study, lower MDA levels of the colon tissues in the IBD + BA group may have been associated with the free radical scavenging features of BA. In addition, we found that B. clausii lowering the MDA levels in colon tissues. We attribute this to the exopolysaccharide productivity of B. clausii probiotics as it is indicated by Catinean et al. [66]. Likewise, the reduction in MDA levels also took place in the combined treatment group. However, statistically, BA administration appears to be more effective than B. clausii and combined treatment.
Catalase and GPx are crucial enzymes of the endogenous antioxidant system [67, 68]. Genetic studies show that the deficiency of the GPx enzyme is directly related to the pathogenesis of the IBD [69, 70]. We consider that the reason for the decline in GPx activities in the IBD group is taking part in the scavenging of the increased hydrogen peroxide and hydroperoxides in colitis. Catalase activities were observed as decreased in TNBS-induced colitis model studies [71, 72]. However, in our study, the catalase activity of the IBD group was found significantly higher than the control group. Colares et al. [73] demonstrated that catalase activity increased through a mechanism that is activated to compensate for changes in colitis. We previously reported the catalase activities were recovered by BA administration [22, 23, 29, 31]. Patel et al. [26] showed that B. clausii administration led to a decrease in MDA levels, also recovery in catalase, SOD activities, and GSH levels. In accordance with our findings, GPx activities of the BA and combined treatment groups showed a tendency to increase in contrast to the B. clausii treatment group. Although, on the other hand, catalase activities slightly decreased in all treatment groups, it is understood that B. clausii administration has more recovery effect on catalase activity. To summarize, the probiotic application was more effective on catalase activity, whereas BA was on GPx activity.
Intrarectal TNBS (dissolved in 50% ethanol) administration mimics ulcerative colitis through leading the ulcerations and inducing the immune response in colon tissues. In the present study, according to the histologic examination and scoring findings, the intensive immigration of the immune response-related cells was observed in the colon tissue specimens of the TNBS-induced group. These histological analyses also strongly supported our complete blood count, increased TNF-α, IL-35 and NO levels, and MPO activities. In our study, loss of goblet cells and massive damage in mucosa and lamina propria were other significant histologic findings of the TNBS administration. One of the results of this colonic damage was alteration in oxidant/antioxidant system towards the oxidant side. Indeed, these changes in oxidant/antioxidant system were proved by decreased GPx activities and increased MDA levels and catalase activities in colon tissue homogenates. According to our histological examinations and scorings, BA led to an increase in mucosal healing, lowering the goblet and epithelial cell losses and inflammation. These effects of BA on the colon histology could be implicated with decreased oxidative stress and suppressed of immune response in the IBD + BA group. In addition, similarly to the IBD + BA group, oxidative stress and immune response were found to be suppressed in the IBD + BA + BC group. However, no significant changes were detected in the histological and biochemical findings of the group in which B. clausii was administered alone. Particularly the high histological scores of the IBD + BC group, colon tissue specimens suggested that boric acid had more curative effect than B. clausii.
Conclusion
This study is the first to investigate the effects of BA and combination of BA and B. clausii in the animal colitis model. Our findings showed that TNBS-induced colitis caused to significant changes in oxidant/antioxidant system, immune response, and structure of colon tissue. It has been observed that BA both alone and together with B. clausii alleviates the effects of IBD. On the other hand, most ameliorative effect in catalase activity among the treatment groups was B. claussi-treated group. However, the increases in WBC, monocytes, lymphocyte, and neutrophil levels were striking findings following to B. clausii treatment. One of the inferences to be obtained from this study, in which we investigated the acute inflammation process of ulcerative colitis, is that BA and combined treatments are more prominent than probiotic treatment alone in reducing both inflammatory processes and oxidative damage. However, it is clear that the probiotic administrated group also have a curative effect. The findings of the present study were supported by both biochemical and histological analyses. For further studies, it may be recommended to design pre- and post-treatment studies using BA and B. calusii. On the other hand, to elucidate both the effects of BA and B. calusii probiotic on IBD and the molecular mechanisms of IBD directly, co-culture studies can be carried out that can mimic the inflammatory response.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Abad C, Martinez C, Juarranz MG, Arranz A, Leceta J, Delgado M, Gomariz RP (2003) Therapeutic effects of vasoactive intestinal peptide in the trinitrobenzene sulfonic acid mice model of Crohn’s disease. Gastroenterology 124(4):961–971. https://doi.org/10.1053/gast.2003.50141
Head KA, Jurenka JS (2003) Inflammatory bowel disease part I: ulcerative colitis—pathophysiology and conventional and alternative treatment options. Altern Med Rev 8(3):247–283
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L (2017) Crohn’s disease. Lancet 389:1741–1755. https://doi.org/10.1016/S0140-6736(16)31711-1
de Mattos BRR, Garcia MPG, Nogueira JB, Paiatto LN, Albuguerque CG, Souza C L, Fernandes LGR, Tamashiro WM, Simioni PU (2015) Inflammatory bowel disease: an overview immun mechanisms and biological treatments. Mediators of Inflamm 1-11.https://doi.org/10.1155/2015/493012
Rezaie A, Parker RD, Abdollahi M (2007) Oxidative stress and pathogenesis of inflammatory bowel disease: an epiphenomenon or the cause? Dig Dis Sci 52(9):2015–2021. https://doi.org/10.1007/s10620-006-9622-2
Davies MJ (2011) Myeloperoxidase-derived oxidation: mechanisms of biological damage and its prevention. J Clin Biochem Nutr 48(1):8–19. https://doi.org/10.3164/jcbn.11-006FR
Knowles RG, Moncada S (1994) Nitric oxide synthases in mammals. Biochem J 298:249–258. https://doi.org/10.1042/bj2980249
Nathan C, Xie QW (1994) Nitric oxide synthase: roles, tolls, and controls. Cell 78(6):915–918. https://doi.org/10.1016/0092-8674(94)90266-6
Bruckdorfer R (2005) The basics about nitric oxide. Mol Aspects Med 26:3–31. https://doi.org/10.1016/j.mam.2004.09.002
Cross RK, Wilson KT (2003) Nitric oxide in ınflammatory bowel disease. Inflamm Bowel Dis 9(3):179–189. https://doi.org/10.1097/00054725-200305000-00006
Neurath MF (2014) (2014) Cytokines in inflammatory bowel disease. Immunol 14(5):329–342. https://doi.org/10.1038/nri3661]
Catalan-Diebne J, Mclntyre LL, Zlotnik A (2018) Interleukin 30 to interleukin 40. J Interferon Cytokine Res 38(10):423–439. https://doi.org/10.1089/jir.2018.0089
Wirtz S, Billmeier U, Mchedlidze T, Blumberg RS, Neurath MF (2011) Interleukin-35 mediates mucosal immune responses that protect against T-cell–dependent colitis. Gastroentergology 141(5):1875–1886. https://doi.org/10.1053/j.gastro.2011.07.040
Ardite E, Sans M, Panes J, Romero FJ, Pique JM, Fernandez-Checa JC (2000) Replenishment of glutathione levels improves mucosal function in experimental acute colitis. Lab Invest 80(5):735–744. https://doi.org/10.1038/labinvest.3780077
Tham DM, Whitin JC, Cohen HJ (2002) Increased expression of extracellular glutathione peroxidase in mice with dextran sodium sulfate-ınduced experimental colitis. Pediatr Res 51(5):641–646. https://doi.org/10.1203/00006450-200205000-00016
Nieto N, Torres MI, Fernandez MI, Giron MD, Rios A, Suarez MD, Gil A (2000) Experimental ulcerative colitis ımpairs antioxidant defense system in rat intestine. Dig Dis Sci 45(9):1820–1827. https://doi.org/10.1023/a:1005565708038
Ghafar H, Yasa N, Mohammadirad A, Dehghan G, Zamani MJ, Nikfar S, Khorasani R, Minaie B, Abdollahi M (2006) Protection by Ziziphora clinopoides of acetic acid-induced toxic bowel inflammation through reduction of cellular lipid peroxidation and myeloperoxidase activity. Hum Exp Toxicol 25(6):325–332. https://doi.org/10.1191/0960327105ht626oa
Kolias G, Valatas V, Ward SG (2004) Nitric oxide in inflammatory bowel disease: a universal messenger in an unsolved puzzle. Immunology 113(4):427–437. https://doi.org/10.1111/j.1365-2567.2004.01984.x
Murray FJ (1998) A comparative review of the pharrnacokinetics of boric acid in rodents and humans. Biol Trace Elem Res 66:331–341. https://doi.org/10.1007/BF02783146
Ince S, Kucukkurt I, Cigerci IH, Fidan F, Eryavuz A (2010) The effects of dietary boric acid and borax supplementation on lipid peroxidation, antioxidant activity, and DNA damage in rats. J Trace Elem Med Biol 24(3):161–164. https://doi.org/10.1016/j.jtemb.2010.01.003
Türkez H, Geyikoğlu F, Tatar A, Keleş S, Özkan A (2007) Effects of some boron compounds on peripheral human blood. Z Naturforsch C J Biosci 62:889–896. https://doi.org/10.1515/znc-2007-11-1218
Kar F, Hacıoğlu C, Özkoç M, Üstünışık N, Bütün A, Uslu S, Kanbak G (2018) The new perspective neuroprotective effect of boric acid against ethanol-induced oxidative damage on synaptosome. J Appl Biol Sci 12(2):28–33
Kar F, Hacioglu C, Senturk H, Donmez Burukoglu D, Kanbak G (2020) The role of oxidative stress, renal inflammation, and apoptosis in post ischemic reperfusion injury of kidney tissue: the protective effect of dose-dependent boric acid administration. Biol Trace Elem Res 195(1):150–158. https://doi.org/10.1007/s12011-019-01824-1
Mack DR (2005) Probiotics. Can Fam Physician 51(11):1455–1457
Cutting SM (2011) Bacillus probiotics. Food Microbiol 28(2):214–220. https://doi.org/10.1016/j.fm.2010.03.007
Patel C, Patel P, Acharya S (2020) Therapeutic prospective of a spore-forming probiotic—Bacillus clausii UBBC07 against acetaminophen-induced uremia in rats. Probiotics Antimicrob Proteins 12(1):253–258. https://doi.org/10.1007/s12602-019-09540-x]
Di Caro S, Tao H, Grillo A, Franceschi F, Elia C, Zocco MA, Gasbarrini G, Sepulveda AR, Gasbarrini A (2005) Bacillus clausii effect on gene expression pattern in small bowel mucosa using DNA microarray analysis. Eur J Gastroenterol Hepatol 17(9):951–960. https://doi.org/10.1097/00042737-200509000-00011
Kankuri E, Asmawi MZ, Korpela R, Vapaatalo H, Moilanen E (1991) Induction of iNOS ın a rat model of acute colitis. Inflammation 23(2):141–152. https://doi.org/10.1023/a:1020241028723
Ataizi Z, Ozkoc M, Kanbak G, Karimkhani H, Burukoglu Donmez D, Ustunisik N, Ozturk B (2019) Evaluation of the neuroprotective role of boric acid in preventing traumatic brain injury-mediated oxidative stress. Turk Neurosur 1-7.https://doi.org/10.5137/1019-5149.JTN.25692-18.5
Karimkhani H, Özkoç M, Shojaolsadati P, Uzuner K, Burukoglu Donmez D, Kanbak G (2021) Protective effect of boric acid and omega-3 on myocardial infarction in an experimental rat model. Biol Trace Elem Res 199:2612–2620. https://doi.org/10.1007/s12011-020-02360-z
Can B, Kar F, Kar E, Özkoç M, Şentürk H, Dönmez Burukoğlu D, Kanbak G, Alataş İÖ (2021) Conivaptan and boric acid treatments in acute kidney ınjury: ıs this combination effective and safe? Biol Trace Elem Res 1-15.https://doi.org/10.1007/s12011-021-02977-8
Suzuki K, Ota H, Sasagawa S, Sakatani T, Fujikura T (1983) Assay meethod for myeloperoxidase in human polymorphonuclear leukocytes. Anal Biochem 132(2):345–352. https://doi.org/10.1016/0003-2697(83)90019-2
Cortas NK, Wakid NW (1990) Determination of inorganic nitrate in serum and urine by a kinetic cadmium-reduction method. Clin Chem 36:1440–1443
Ohkawa H, Ohisi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. https://doi.org/10.1016/s0076-6879(84)05016-3
Gornall AG, Bardawill CJ, David MM (1949) Determination of serum proteins by means of the biuret reaction. J Biol Chem 177(2):751–766
Cengiz M, Altuner Y, Sahinturk V, Ozden H, Senturk H, Bayramoglu G, Burukoglu Donmez D, Sahin I, Ayhanci A (2012) Lycopene protects liver against ulcerative colitis. Current Drug Therapy 7(1):24–29. https://doi.org/10.2174/157488512800389227
Mateus V, Rocha J, Mota-Filipe H, Sepodes B, Pinto R (2018) Hemin reduces inflammation associated with TNBS-induced colitis. Clin Exp Gastroenterol 11:325–334. https://doi.org/10.2147/CEG.S166197
Fawley J, Gourlay D (2016) Intestinal alkaline phosphatase: a summary of its role in clinical disease. J Sur Res 202(1):225–234. https://doi.org/10.1016/j.jss.2015.12.008
Malo MS, Alam SN, Mostafa G, Zeller SJ, Johnson PV, Mohammad N, Chen KT, Moss AK, Ramasamy S, Faruqui A, Hodin S, Malo PS, Ebrahimi F, Narisawa S, Millan JL, Warren HS, Kaplan JB, Kitts CL, Hohmann EL, Hodin RA (2010) Intestinal alkaline phosphatase preserves the normal homeostasis of gut microbiota. Gut 59(11):1476–1484. https://doi.org/10.1136/gut.2010.211706
Hoa TH, Duc LH, Isticato R, Baccigalupi L, Ricca E, Van PH, Cutting SM (2011) Fate and sissemination of Bacillus subtilis spores in a murine model. Appl Environ Microbiol 67(9):3819–3823. https://doi.org/10.1128/AEM.67.9.3819-3823.2001
Togawa JI, Nagase H, Tanaka K, Inamori M, Nakajima A, Ueno N, Saito T, Sekihara H (2002) Oral administration of lactoferrin reduces colitis in rats via modulation of the immune system and correction of cytokine imbalance. J Gastroenterol Hepatol 17(12):1291–1298. https://doi.org/10.1046/j.1440-1746.2002.02868.x
Liu L, Yuan S, Sun Y, Long Y, Li Y, Niu Y, Li C, Gan H, Cao S, Mei Q (2009) The possible mechanisms of Fructus Mume pill in the treatment of colitis induced by 2,4,6-trinitrobenzene sulfonic acid in rats. J Ethnopharmacol 126(2):557–564. https://doi.org/10.1016/j.jep.2009.08.013
Larrosa M, Yanez-Gascon M, Selma M, Gonzalez-Sarrisa A, Toti S, Ceron J, Tomas-Barberan F, Dolara P, Espin JC (2009) Effect of a low dose of dietary resveratrol on colon microbiota, inflammation and tissue damage in a DSS-induced colitis rat model. J Agric Food Chem 57(6):2211–2220. https://doi.org/10.1021/jf803638d
Celikbilek M, Dogan S, Ozbakır O, Zararsız G, Kücük H, Gürsoy S, Yurci A, Güven K, Yücesoy M (2013) Neutrophil–lymphocyte ratio as a predictor of disease severity in ulcerative colitis. J Clin Lab Anal 27(1):72–76. https://doi.org/10.1002/jcla.21564
Idiz UO, Aysan E, Firat D, Ercan C, Demirci S, Sahin F (2019) Effects of boric acid-linked ampicillin on the rat intra-abdominal sepsis model. Pak J Pharm Sci 32(2):477–481
Herias MV, Koninkx J, Vos J, Huis in’t Veld J, van Dijk J, (2005) Probiotic effects of Lactobacillus casei on DSS-induced ulcerative colitis in mice. Int J Food Microbiol 103(2):143–155. https://doi.org/10.1016/j.ijfoodmicro.2004.11.032
Garside P (1991) Cytokines in experimental colitis. Clin Exp Immunol 118(3):337–339. https://doi.org/10.1046/j.1365-2249.1999.01088.x
Xu C-L, Guo Y, Qiao L, Ma L, Cheng Y-Y (2018) Recombinant expressed vasoactive intestinal peptide analogue ameliorates TNBS-induced colitis in rats. World J Gastroenterol 24(6):706–715. https://doi.org/10.3748/wjg.v24.i6.706
Collison LW, Workman CJ, Kuo TT, Boyd K, Wang Y, Vignali KM, Cross R, Sehy D, Blumberg RS, Vignali DAA (2007) The inhibitory cytokine IL-35 contributes to regulatory T-cell function. Nature 450:566–569. https://doi.org/10.1038/nature06306
Zhang B, Liu Y, Lan X, Zhang X, Li X, Zhao Y, Li G, Du C, Lu S, Wang H (2018) Oral Escherichia coli expressing IL-35 meliorates experimental colitis in mice. J Transl Med 16(1):1–10. https://doi.org/10.1186/s12967-018-1441-7
Nan Z, Fan H, Tang Q, Zhang M, Xu M, Chen Q, Liu Y, Dong Y, Wu H, Deng S (2018) Dual expression of CXCR4 and IL-35 enhances the therapeutic effects of BMSCs on TNBS-induced colitis in rats through expansion of Tregs and suppression of Th17 cells. Biochem Biophys Res Commun 499(4):727–734. https://doi.org/10.1016/j.bbrc.2018.03.043
Cao J, Jiang L, Zhang X, Yao X, Geng C, Xue X, Zhong L (2008) Boric acid inhibits LPS-induced TNF-a formation through a thiol-dependent mechanism in THP-1 cells. J Trace Elem Med Biol 22(3):189–195. https://doi.org/10.1016/j.jtemb.2008.03.005
Dargahi N, Johnson J, Donkor O, Vasiljevic T, Apostolopoulos V (2019) Immunomodulatory effects of probiotics: can they be used to treat allergiesand autoimmune diseases? Maturitas 119:25–38. https://doi.org/10.1016/j.maturitas.2018.11.002
Dar HY, Pal S, Shukla P, Mishra PK, Tomar GB, Chattopadhyay N, Srivastava RK (2018) Bacillus clausii inhibits bone loss by skewing Treg-Th17 cell equilibrium in postmenopausal osteoporotic mice model. Nutrition 54:118–128. https://doi.org/10.1016/j.nut.2018.02.013
Ancha HR, Kurella RR, McKimmey CC, Lightfoot S, Harty RF (2009) Effects of n-acetylcysteine plus mesalamine on prostaglandin synthesis and nitric oxide generation in TNBS-induced colitis in rats. Dig Dis Sci 54(Suppl 4):758–766. https://doi.org/10.1007/s10620-008-0438-0
Avdagić N, Zaćiragić A, Babić N, Hukić M, Šeremet M, Lepara O, Nakaš-Ićindić E (2013) Nitric oxide as a potential biomarker in inflammatory bowel disease. Bosn J Basic Med Sci 13(1):5–9. https://doi.org/10.17305/bjbms.2013.2402
Urdaci MC, Bressollier P, Pinchuk I (2004) Bacillus clausii probiotic strains: antimicrobial and immunomodulatory activities. J Clin Gastroenterol 38(3):86–90. https://doi.org/10.1097/01.mcg.0000128925.06662.69
Li XL, Cai YQ, Qin H, Wu YJ (2008) Therapeutic effect and mechanism of proanthocyanidins from grape seeds in rats with TNBS-induced ulcerative colitis. Can J Physiol Pharmacol 86(12):841–849. https://doi.org/10.1139/Y08-089
Liu X, Wang J (2011) Anti-inflammatory effects of iridoid glycosides fraction of Folium syringae leaves on TNBS-induced colitis in rats. J Ethnopharmacol 133(2):780–787. https://doi.org/10.1016/j.jep.2010.11.010
Tabari MV, Moein S, Qujeq D, Kashifard M, Shirvani JS, Tilaki KH, Farshidfar G (2017) Evaluation of the potential antioxidant role of high-density lipoprotein-cholesterol (HDL-c) in patients with ulcerative colitis. Ann Colorectal Res 1-6.https://doi.org/10.5812/acr.13699
Xu M, Tao J, Yang Y, Tan S, Liu H, Jiang J, Zheng F, Wu B (2020) Ferroptosis involves in intestinal epithelial cell death in ulcerative colitis. Cell Death Dis 11:1–13. https://doi.org/10.1038/s41419-020-2299-1
Cengiz M (2018) Boric acid protects against cyclophosphamide-induced oxidative stress and renal damage in rats. Cell Mol Biol 64(12):11–14
Ince S, Keles H, Erdogan M, Hazman O, Kucukkurt I (2012) Protective effect of boric acid against carbon tetrachloride–induced hepatotoxicity in mice. Drug Chem Toxicol 35(3):285–292. https://doi.org/10.3109/01480545.2011.607825
Sogut I, Oglakci A, Kartkaya K, Kusat Ol K, Savasan Sogut M, Kanbak G, Erden Inal M (2015) Effect of boric acid on oxidative stress in rats with fetal alcohol syndrome. Exp Ther Med 9(3):1023–1027. https://doi.org/10.3892/etm.2014.2164
Catinean A, Neag MA, Krishnan K, Muntean DM, Bocsan CI, Pop RM, Mitre AO, Melincovici CS, Buzoianu AD (2020) Probiotic Bacillus spores together with amino acids and immunoglobulins exert protective effects on a rat model of ulcerative colitis. Nutrients 12(12):1–18. https://doi.org/10.3390/nu12123607
Izawa S, Inoue Y, Kimura A (1996) Importance of catalase in the adaptive response to hydrogen peroxide: analysis of acatalasaemic Saccharomyces cerevisiae. Biochem J 320:61–67. https://doi.org/10.1042/bj3200061
Tehrani SH, Moosavi-Movahedi AA (2018) Catalase and its mysteries. Prog Biophys Mol Biol 140:5–12. https://doi.org/10.1016/j.pbiomolbio.2018.03.001
Esworthy RS, Binder SW, Doroshow JH, Chu FF (2003) Microflora trigger colitis in mice deficient in selenium gene expression. Biol Chem 384(4):597–607. https://doi.org/10.1515/BC.2003.067
Häuser F, Rossmann H, Laubert-Reh D, Wild PS, Zeller T, Müller C, Neuwirth S, Blankenberg S, Lackner KJ (2015) Inflammatory bowel disease (IBD) locus 12: is glutathione peroxidase-1 (GPX1) the relevant gene? Genes Immun 16(8):571–575. https://doi.org/10.1038/gene.2015.35
Lee IA, Hyun YJ, Kim DH (2010) Berberine ameliorates TNBS-induced colitis by inhibiting lipid peroxidation, enterobacterial growth and NF-κB activation. Eur J Pharmacol 648:162–170. https://doi.org/10.1016/j.ejphar.2010.08.046
Yildiz G, Yildiz Y, Ulutas PA, Yaylali A, Ural M (2015) Resveratrol pretreatment ameliorates TNBS colitis in rats. Recent Pat Endocr Metab Immune Drug Discov 9(2):134–140. https://doi.org/10.2174/1872214809666150806105737
Colares JR, Schemitt EG, Hartmann RM, Moura RM, Morgan-Martins MI, Fillmann HS, Fillmann L, Marroni NP (2016) Effect of lecithin on oxidative stress in an experimental model of colitis rats induced by acetic acid. J Coloproctol 36(2):97–103. https://doi.org/10.1016/j.jcol.2016.03.002
Acknowledgements
The authors are thankful to the Director and workers of the Medical and Surgical Experimental Research Centre of the University for their kind cooperation throughout the animal care.
Funding
This project was financially supported by the Scientific Research Projects Commission of the Eskisehir Osmangazi University (Eskişehir, Turkey) (Project #202011D03).
Author information
Authors and Affiliations
Contributions
Özkoç M. and Kanbak G. designed the study; Özkoç M., Can B., and Şentürk H. performed surgical operations; Özkoç M. and Can B. performed the biochemical experiments, acquired and analyzed data; Özkoç M. and Kanbak G. interpreted the biochemical data; Dönmez Burukoğlu D. carried out the histological experiments and interpreted the histologic data; Özkoç M. wrote the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All animal research protocols in this study were approved by the Institutional Ethics Committee (HADYEK, Protocol # 778/2019).
Consent for Publication
All authors have given consent for the manuscript to be published by the corresponding author.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Özkoç, M., Can, B., Şentürk, H. et al. Possible Curative Effects of Boric Acid and Bacillus clausii Treatments on TNBS-Induced Ulcerative Colitis in Rats. Biol Trace Elem Res 201, 1237–1251 (2023). https://doi.org/10.1007/s12011-022-03215-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03215-5