Abstract
Zinc is an essential microelement that plays many important functions in the body. It is crucial for the regulation of cell growth, hormone release, immunological response, and reproduction. Thus, this trial aimed to evaluate the effects of zinc supplementation in comparison with placebo on the improvement of premenstrual symptoms in female university students. This triple-masked, randomized, placebo-controlled, parallel trial was conducted among 69 female students aged 18–35 with premenstrual syndrome that living in dormitories of Hamadan University of Medical Sciences, in west of Iran. Participants were randomly assigned to two groups of equal number; one group received 220 mg of elemental zinc (n = 33) and the other group received placebo (n = 36) on a regular daily for 24 weeks. The premenstrual syndrome was assessed by Premenstrual Symptoms Screening Tool-Adolescent (PSST-A) questionnaire for all participants. Chi-square and t-student tests were used to compare the percentage or mean of parameters between two groups. All statistical analysis conducted by SPSS version 16. The mean age in the intervention group was 25.64 \(\pm\) 0.53 years, and in the control group was 24.38 \(\pm\) 0.51 years (P = 0.087). After 24 weeks of intervention, PMS physical and psychological symptoms such as anger, anxiety, depressed mood, overeating, breast tenderness, headaches, muscle pain, bloating, and weight gain significantly decreased in zinc group compared to placebo group (P < 0.001). We observed a significant increase in relationship with friends, classmates, and coworkers (p = 0.003) after 24 weeks of intervention with zinc compared to placebo. In conclusion, zinc, as a simple and inexpensive treatment, was associated with improvement of PMS symptoms. Given that this is among the first studies to evaluate the effect of zinc supplementation on PMS, additional studies are warranted to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Premenstrual syndrome (PMS) involves a set of clinically significant physical and psychological manifestations during the luteal phase of the menstrual cycle. This syndrome causes significant distress and impaired functional capacity in individuals. Usually, the symptoms following PMS disappear shortly after the onset of menstruation [1]. Evidence indicates that the prevalence of PMS is close to 50% in women at reproductive age worldwide [2]. Most patients experience mild to moderate symptoms of the syndrome, and only about 2.5–3% experience severe symptoms that can interfere with their daily functioning. Female university students are among women with the higher rate of PMS [1, 3].
There are about 200 different symptoms associated with PMS, the three most important of which are mood swings, stress, and anxiety. Common emotional and non-specific symptoms following PMS include stress, anxiety, insomnia, headache, fatigue, mood swings, increased emotional sensitivity, and changes in libido [4]. Formal definitions absolutely require the presence of emotional symptoms as the main complaint of PMS; The presence of physical symptoms associated with the menstrual cycle include changes in appetite, nausea, constipation, swelling or tenderness of the breast, menstrual cycle acne, fatigue, and joint or muscle pain [4, 5].
The etiology of PMS is unknown [1]. It is believed that this syndrome is not a single disorder but is a set of symptoms of biological origin that also includes psychological and social aspects. Therefore, efforts have been made for pharmacological and non-pharmacological treatment [6]. Treatment is usually based on symptom relief and reduces the effects of PMS on the patient daily routine activities. For example, combinations of pharmacotherapies including diuretics, painkillers, antihistamines, antidepressants, and anti-anxiety are used to treat the same symptom [1].
Recently, more attention has been paid to other treatments that are mostly based on clinical experience and reduce the prevalence and severity of annoying PMS by unknown mechanisms. These treatments include mineral deficiency replacement including calcium, magnesium, vitamin B6, and vitamin E supplements, as well as various diets such as primrose oil or a high-carbohydrate diet, which have recently received much attention [7].
Serum zinc concentrations fluctuate throughout the menstrual cycle. In PMS women, serum zinc level is significantly lower than the normal women. Zinc supplements may reduce the negative effects of PMS in women. This mineral is able to regulate the secretion of progesterone as a hormone that increases the risk of premenstrual syndrome. Zinc supplements in women prevent painful menstruation. It also plays a vital role in the physical development of the gastrointestinal tract and immune system [8, 9]. So far, very few studies have examined the beneficial effects of zinc supplementation on biochemical and genetic factors associated with PMS. Also, due to the fact that zinc participates in some metabolic and signaling pathways, therefore, the administration of this drug may further improve the symptoms in patients with PMS. Given the antioxidant role, antidepressant activity, and anti-inflammatory action of zinc supplement, so it seems to alleviate PMS symptoms [10,11,12]. There is little information about the effect of zinc supplement on PMS complications; therefore, this study was conducted to investigate the effect of zinc supplement on the symptoms of women with premenstrual syndrome.
Materials and Methods
Study Design and Setting
This study was a double-blind randomized clinical trial that was conducted on female students aged 18–35 with PMS living in dormitories of Hamadan University of Medical Sciences, Hamadan (west of Iran), from February to April 2021.
Eligibility Criteria
Inclusion criteria included patients with moderate to severe PMS in the age range of 18–35 years who were studying at Hamadan University of Medical Sciences and were willing to participate in the study. Patients with symptoms of malnutrition (Marasmus, Kwashiorkor, Marasmus-Kwashiorkor) and need zinc replacement or any signs of severe malnutrition, symptoms of systemic disease (sepsis, acute meningitis, hemodynamic instability), diarrhea with 3 or more watery stools in the last 24 h, known intolerance or sensitivity to zinc or zinc-containing compounds, smoking, being in a stressful situation, and having a history of mental illness were considered as exclusion criteria.
Intervention
Patients randomly were divided into two groups. The control group received the placebo and the intervention group received 220 mg zinc sulfate capsules (containing 50 mg zinc) that were administered for 3 months. Patients were evaluated for symptoms at initiation, 1 month, 3 month, and 6 month after running the study.
Randomization and Blinding
Balanced block randomization (block size, 4) was used to allocate patients into two groups and 43 patients finally were assigned to each group. Moreover, because neither the participants nor the experimenters know who is receiving a particular treatment, therefore, the study was double-blind.
Measurement Tool
Prior to the study, patients were asked to complete and sign an informed consent form if they wished to participate in the study. After the patients entered the study, demographic information including age, education, marital status, and occupation were asked and recorded.
In this study, PSST questionnaire was used to assess the severity of PMS. The PSST questionnaire consists of 19 questions that have two parts: the first part which includes 14 questions related to mood, physical, and behavioral symptoms; and the second part which measures the effect of these symptoms on people’s lives and consists of 5 questions. This questionnaire was designed by McMaster University of Canada and standardized in Persian by Siahbazi et al. in the Iranian population [13]. The validity and reliability indices of the Persian version of this questionnaire in the above study were presented at an acceptable level so that Cronbach’s alpha index was higher than 0.7 that indicates the acceptable internal consistency. Moreover, its face and content validity in this study was approved by the panel of experts. This questionnaire completed by the patients at the beginning of the study, 1 month, 3, and 6 months after the beginning of the study.
Statistical Analysis
All quantitative data were presented as mean ± SD. Chi-square test was used to compare the percentage or frequency of parameters between two groups. Comparison of the continuous variables between two groups was done using independent Student sample-t test. Using ANCOVA, the mean score of PSST-A components (adjusting for baseline score), between two groups, was compared in the investigated time periods. Moreover, changes in the score of PSST-A components over time between the two groups were performed using repeated measures ANOVA test. In this study, p < 0.05 was considered statistically significant. The SPSS software (IBM, version 23) was applied for data analysis.
Ethical Considerations
Ethical approval for the study was obtained from the ethics committee of Hamadan University of Medical Sciences according to Helsinki declaration. This clinical trial was registered by the Iranian Registry of Clinical Trials (IRCT) on 2020–03-14 and the IRCT ID was IRCT20120215009014N347.
Results
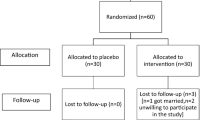
Figure 1 shows the process of patients selecting and follow-up in two groups. Of the 92 investigated patients, 21 of them were excluded due to not meeting the inclusion criteria or decline for participation. After equally allocation of patients (36 patients in each group), 3 patients discontinued the study in the intervention group.
Table 1 shows the distribution of individual characteristics of the participants in zinc sulfate and placebo groups. The majority of participants in the intervention group (n = 33) and placebo group (n = 36) were Ph.D. students. The mean age in the intervention group was 25.64 \(\pm\) 0.53 years, and in the control group was 24.38 \(\pm\) 0.51 years (P = 0.087). According to the results presented in the table, there was no statistically significant difference between the zinc sulfate supplementation and placebo groups regarding the individual features that might affect the treatment.
In Table 2, we compared the mean score of PSST-A components at the baseline between the intervention and control groups. As shown, there was not a significant difference between two groups in this regard (P > 0.05).
Table 3 shows the mean score of each item in the PSST-A questionnaire on the 1st, 3th, and 6th months after the intervention. This table also shows the changes in the mean difference between the intervention and control group in each period of intervention. The mean score of anger and irritability 1 month after intervention in the zinc sulfate supplementation group was 3.65 \(\pm\) 0.59 and in the control group was 3.94 \(\pm\) 0.61, which was significantly different between the intervention and control groups (P = 0.001). This significant difference was also seen in the third and sixth months of the study. The mean score of anxiety and tension 1 month after intervention in the zinc sulfate group was 3.79 \(\pm\) 0.89 and in the placebo group was 3.80 \(\pm\) 0.89, which statistically different between intervention and control groups (the mean of anxiety in the group receiving zinc was 0.85 less than the control group). Also, the means of work efficiency, relationship with friends, classmates, and family members, social life activities, and responsibility in the home in the intervention group were higher than the control group. Results of the repeated measure ANOVA indicate no significant interaction between treatment and time for all components (P > 0.05).
Discussion
Premenstrual syndrome is one of the most common disorders of reproductive age [14]. This study showed that zinc supplementation compared to placebo was effective on all dimensions of the PSST-A questionnaire.
The control placebo group also had lower scores after intervention, but only in the first month of the study. The positive role of placebo has been reported by others [15], suggesting that the response to placebo in published trials on psychological aspects of disorders or treatment of pain is highly effective [16].
Zinc supplement has an anti-inflammatory effect [17]. This property reduces the production of prostaglandins and leukotriene by inhibiting the cyclooxygenase and lipoxygenase pathways and reduces the severity of the physical symptoms of PMS and improves physical function and physical pain [18].
Many of the symptoms of PMS, such as depression, sleep disorders, anxiety, aggression, and difficulty concentrating, are due to a decrease in the neurotransmitter serotonin [19]. Zinc supplementation affects the levels of neurotransmitters such as serotonin, which are responsible for behavioral and emotional symptoms [20]. Furthermore, zinc is also required for the production and modulation of melatonin and GABAs [21, 22], which helps regulate dopamine function, an important factor in PMS and its treatment [23].
In healthy people, the activity of oxidants and antioxidants is in balance. Loss of this balance causes oxidative stress. According to the results of some studies, the level of total antioxidant capacity (TAC) in patients with premenstrual syndrome decreases. A decrease in TAC is associated with an increase in the production of free radicals and a decrease in the level of defense antioxidants. Zinc supplement has antioxidant activity; As a result, the antioxidant activity of zinc is effective in improving all dimensions of the PSST-A questionnaire [24].
The study of Siahbazi et al. [9] as the effect of zinc sulfate supplementation on premenstrual syndrome and quality of life showed that the prevalence of this syndrome in the zinc sulfate group was significantly reduced during the study period. The mean scores of health-related quality of life in the physical and mental components in the intervention group improved significantly. Therefore, it was consistent with the results of the present study.
One of the strengths of this study was blinding and its limitations were individual, personality, and genetic differences of research units that could be controlled to some extent through random selection of samples. Also, some PMS confounders were not studied, such as relationship status, lifestyle, and physical activity. In addition, we did not measure blood zinc concentration to monitor alterations in zinc levels before and during treatment.
Conclusion
In conclusion, zinc, as a simple and inexpensive treatment, was associated with improvement of PMS symptoms. Given that this is among the first studies to evaluate the effect of zinc supplementation on PMS, additional studies are warranted to confirm these findings.
Data Availability
The data that support the findings of the study are available from the corresponding author in SPSS form upon reasonable request.
Code availability
Not applicable.
References
Gudipally PR, Sharma GK (2021) Premenstrual Syndrome. StatPearls. Treasure Island (FL): StatPearls Publishing
Nascimento AF, Gaab J, Kirsch I, Kossowsky J, Meyer A, Locher C (2020) Open-label placebo treatment of women with premenstrual syndrome: study protocol of a randomised controlled trial. BMJ Open 10(2):e032868
Direkvand-Moghadam A, Sayehmiri K, Delpisheh A, Kaikhavandi S (2014) Epidemiology of premenstrual syndrome (PMS)-a systematic review and meta-analysis study. J Clin Diagnos Res: JCDR 8(2):106
Derman O, Kanbur NÖ, Tokur TE, Kutluk T (2004) Premenstrual syndrome and associated symptoms in adolescent girls. Eur J Obs Gynecol Reprod Biol 116(2):201–206
Ryu A, Kim T-H (2015) Premenstrual syndrome: a mini review. Maturitas 82(4):436–440
Frank RT (1931) The hormonal causes of premenstrual tension. Arch Neurol Psychiatry 26(5):1053–1057
Jang SH, Kim DI, Choi M-S (2014) Effects and treatment methods of acupuncture and herbal medicine for premenstrual syndrome/premenstrual dysphoric disorder: systematic review. BMC Complement Altern Med 14(1):1–13
Erickson KL, Medina EA, Hubbard NE (2000) Micronutrients and innate immunity. J Infect Dis 182(Supplement_1):S5–S10
Siahbazi S, Behboudi-Gandevani S, Moghaddam-Banaem L, Montazeri A (2017) Effect of zinc sulfate supplementation on premenstrual syndrome and health-related quality of life: clinical randomized controlled trial. J Obs Gynaecol Res 43(5):887–894
Fathizadeh S, Amani R, Haghighizadeh MH, Hormozi R (2016) Comparison of serum zinc concentrations and body antioxidant status between young women with premenstrual syndrome and normal controls: a case-control study. Int J Reprod BioMed 14(11):699
Prasad AS (2014) Zinc: an antioxidant and anti-inflammatory agent: role of zinc in degenerative disorders of aging. J Trace Elem Med Biol 28(4):364–371
Szewczyk B, Kubera M, Nowak G (2011) The role of zinc in neurodegenerative inflammatory pathways in depression. Prog Neuropsychopharmacol Biol Psychiatry 35(3):693–701
Siahbazi S, Hariri F, Montazeri A, Moghadam BL (2011) Standardization of premenstrual symptoms screening questionnairePSST: translation and psychometric Iranian species. J Payesh 10(4):421–427
Maskani S, Tafazoli M, Rakhshandeh H, Esmaily H (2020) The effect of Nigella sativa seeds capsules on the quality of life in students with premenstrual syndrome: a randomized clinical trial. J Sabzevar Univ Med Sci 26(6):779–787
Piantadosi S (2017) Clinical trials: a methodologic approach. New York, NY, USA: John Wiley & Sons
Muthukumaraswamy SD, Forsyth A, Lumley T (2021) Blinding and expectancy confounds in psychedelic randomized controlled trials. Expert Rev Clin Pharmacol 14(9):1133–1152
Chasapis CT, Ntoupa PSA, Spiliopoulou CA, Stefanidou ME (2020) Recent aspects of the effects of zinc on human health. Arch Toxicol 94(5):1443–60
Juergens LJ, Worth H, Juergens UR (2020) New perspectives for mucolytic, anti-inflammatory and adjunctive therapy with 1, 8-cineole in COPD and asthma: review on the new therapeutic approach. Adv Ther 37(5):1737–1753
Rapkin AJ, Korotkaya Y, Taylor KC (2019) Contraception counseling for women with premenstrual dysphoric disorder (PMDD): current perspectives. Open Access J Contracept 10:27
García-Colunga J, Reyes-Haro D, Godoy-García IU, Miledi R (2005) Zinc modulation of serotonin uptake in the adult rat corpus callosum. J Neurosci Res 80(1):145–149
Hershfinkel M (2018) The zinc sensing receptor, ZnR/GPR39, in health and disease. Int J Mol Sci 19(2):439
Groundwater PW, Hamid K, Ng I, Tallapragada VJ, Hibbs DE, Hanrahan J (2015) The differential effects of resveratrol and trans-ε-viniferin on the GABA-induced current in GABAA receptor subtypes expressed in xenopus laevis oocytes. J Pharm Pharm Sci 18(4):328–338
Moderie C, Boudreau P, Shechter A, Lespérance P, Boivin DB (2021) Effects of exogenous melatonin on sleep and circadian rhythms in women with premenstrual dysphoric disorder. Sleep 44(12):zsab171
Jafari F, Amani R, Tarrahi MJ (2020) Effect of zinc supplementation on physical and psychological symptoms, biomarkers of inflammation, oxidative stress, and brain-derived neurotrophic factor in young women with premenstrual syndrome: a randomized, double-blind, placebo-controlled trial. Biol Trace Elem Res 194(1):89–95
Acknowledgements
Deputy of Research and Technology of Hamadan University of Medical Sciences approved our study (Ethic code: IR.UMSHA.REC.1398.1080). We would like gratefully acknowledge the medical staff of the Fatemieh Hospital.
Funding
This study was funded by the Hamadan University of Medical Sciences, Iran.
Author information
Authors and Affiliations
Contributions
MA, SK, and HP developed the original idea and the protocol, abstracted, and prepared the manuscript. AP and AA participated in the study design and analyzed the data. MA and SK contributed to the study design and data gathering. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Institutional review board approval was obtained from the ethics committees of Hamadan University of Medical Sciences.
Consent for Publication
Written and informed consent was obtained from the patients.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmadi, M., Khansary, S., Parsapour, H. et al. The Effect of Zinc Supplementation on the Improvement of Premenstrual Symptoms in Female University Students: a Randomized Clinical Trial Study. Biol Trace Elem Res 201, 559–566 (2023). https://doi.org/10.1007/s12011-022-03175-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03175-w