Abstract
Osteoporosis is a general bone-related ailment characterized by reduced bone density and quality, elevated bone fragility, and fractures. It was reported that both aged men and women has an increased risks of osteoporosis. The current research work focused to unveil the beneficial roles of ponicidin treatment in the proliferation and calcium deposition on the osteoblast-like MG-63 cells. The effect of 5 and 10 µg/ml of ponicidin on the cell proliferation was assessed. The viability of ponicidin-supplemented MG-63 cells was inspected by MTT test. The contents of osteocalcin, collagen, and ALP activity in the ponicidin administered cells were assessed by kits. The level of calcium mineralization was examined by ARS staining technique. The ponicidin treatment remarkably improved the proliferation of MG-63 cells. The ponicidin did not affect the MG-63 cells viability but promoted its viability 24- and 48-h treatment. The contents of osteocalcin, collagen, and ALP activity in the 5 and 10 µg/ml of ponicidin-supplemented MG-63 cells were found increased than the control cells. The ponicidin also increased the level of calcium deposition in MG-63 cells, which is assessed by ARS staining. In conclusion, it was clear that ponicidin improved the proliferation and calcium mineralization in a MG-63 cells. Therefore, it was clear that ponicidin has helpful roles on the new bone development as a hopeful therapeutic candidate to treat the bone-related disease like osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a common metabolic bone disease characterized by weakened bone tissues and depleted bone density, which leads to the elevated risks of bone fracture [1, 2]. It is common among the aged peoples, especially a woman, with the higher global prevalence [3]. The osteoporosis is primarily caused by the inequality of osteoblast-regulated bone development and osteoclast-regulated bone resorption that is necessary for regular bone metabolism due to the aging process and inadequate estrogen generation [4]. The bone fractures usually take place at the regions of the distal forearm and hip [5]. The problems of the osteoporosis like hip fractures result in four times increased rate of mortality in aged peoples around the world. Generally, one in three women at the age of 50 years or older may suffer from osteoporotic fractures worldwide [6].
Osteoblasts are developed from the pre-osteoblasts from the mesenchymal cells and perform an imperative function in the mineralization and development of bone matrix. During the early phases of osteoblast differentiation, several genes like osteocalcin, type I collagen, and ALP play an essential role on the development of matrix. Osteocalcin is believed as a useful biomarker of late bone generation. It is generated and developed by osteoblasts and then combined in bone matrix [7]. During the later phases of osteoblast differentiation, the produced matrix is mineralized by the calcium deposition [8]. The differentiation of osteoblasts is controlled by the expression of several proteins like osteocalcin and collagen. Runx-2 is a most imperative factor that controls other differentiation biomarkers like ALP. After that, the middle osteoblast differentiation factors like osteopontin and collagen are stimulated during the pre-osteoblast formation into matured osteoblasts. During the matured stage of osteoblasts, the osteocalcin is expressed [9].
Osteoporosis is primarily treated with the aim of decreasing the risks of bone fractures via triggering new bone generation or hindering bone resorption. However, present therapies for the osteoporosis are highly restricted to drugs, which act primarily to prevent the bone resorption. In spite of the highlighted therapeutic benefits, the anti-resorptive drugs were mentioned to possess several deleterious effects like gastrointestinal problems, thromboembolic diseases, and breast cancer [10, 11]. Additionally, bisphosphonates can provoke kidney failure, esophageal cancer, and jaw necrosis. The parathyroid hormones are an only FDA-approved drug that triggers new bone development, but it also connected with risks of osteosarcoma [12]. Contrastingly, bone anabolic therapy triggering new bone development through the osteoblasts signifies a perfect therapeutic option for osteoporosis [13]. As substitutes to synthetic drugs, there was a growing interest by researchers focusing on the phytomedicines [14].
Ponicidin is a diterpenoid compound extensively found on the Isodon adenolomus, a traditional Chinese herb [15]. It was already highlighted that the ponicidin demonstrated several biological activities like antibacterial [16], antitumor activities against leukemia, lung, and hepatocellular cancers [17,18,19]. Ponicidin treatment can effectively decrease the growth and trigger the apoptosis in several cancer cells, for instance, blood cancer [20], breast [21], gastric [22], and colorectal [23] cancers. However, the beneficial properties of ponicidin against the bone regeneration were not scientifically studied yet. As a result, the current research work focused to unveil the beneficial roles of ponicidin treatment on the proliferation and calcium deposition on the osteoblast-like MG-63 cells to discover the bone regenerative properties of the ponicidin.
Materials and Methods
Chemicals
Ponicidin was bought from the Fisher Scientific, Hampton, USA. The 3-(4,5-dimethylthiazoyl-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and additional reagents were obtained from Sigma-Aldrich, USA. The respective kits for experiments were attained from Thermo Fisher, MA, USA.
Maintenance of MG-63 Cells
The osteoblast-like MG-63 cells were grown on a DMEM medium enriched with 10% of FBS and 1% of antimycotic mixture at 37 °C with 5% of CO2 supplementation. The grown MG-63 cells were trypsinized, cleansed with buffer, and then sub-cultured for the further experimentations.
Cell Proliferation Assay
The influence of ponicidin treatment on a proliferation of the MG-63 cells was assessed. Shortly, cells were cultured on a 6-well plate at 1 × 106 cells/well and maintained at 37 °C for a day. Then media was replenished with fresh media and administered with the 5 and 10 µg/ml of ponicidin. The control cells were added only with growth medium and maintained for 24 and 48 h at 37 °C. Followed by the incubation, the levels of cell proliferation were monitored beneath the light microscope [27].
MTT Assay
The influence of ponicidin treatment on the MG-63 cells’ viability was scrutinized by MTT calorimetric test. For this, cells were cultured on the 96-well plate and incubated for 24 h at 37 °C. Then medium was reloaded with fresh media and administered with the 5 and 10 µg/ml of ponicidin for 24 and 48 h at 37 °C. After that, 10 μl of MTT reagent was mixed to every well, and then plate was sustained at 37 °C for 4 h to develop insoluble formazan crystals. Then, 100 μl of DMSO was administered to wells to liquefy the formazan sediments. After that, cell viability was scrutinized by taking absorbance at 570 nm.
Measurement of Osteocalcin, Collagen, and ALP Contents
The contents of osteocalcin and collagen, and ALP activity in the ponicidin-supplemented MG-63 cells were assessed using kits as per the instructions provided by manufacturer (Thermo Fisher, USA). Shortly, the osteoblast-like MG-cells were supplemented with the 5 and 10 µg/ml of ponicidin for 24 and 48 h. Then the cell supernatant was prepared and utilized for the assessment of ALP activity and the contents of collagen and osteocalcin using kits [28].
Assay of Calcium Mineralization
The influence of ponicidin treatment on the level of calcium deposition in the MG-63 cells was scrutinized by ARS staining technique. Shortly, MG-63 cells were grown on 12-well plate at 3 × 104 cells per well population and then administered with the 5 and 10 µg/ml of ponicidin for 7 days. After that, the MG-63 cells were cleansed with chilled buffer solution and sustained with 70% ethanol for 1 h for the cell fixation. Then mM ARS stain was utilized to stain the cells at 37 °C for 10 min. After that, treated cells were de-stained for 10 min using 10% of cetylpyridinium chloride and lastly the cells were monitored using microscope to assess the level of calcium deposition [28].
Statistical Analysis
The data were scrutinized with the help of SPSS software, and final outcome was represented as mean ± SD of triplicate examinations. All the results were assessed using one-way ANOVA and Tukey’s post hoc assay, and p < 0.05 were fixed as significant.
Results
Effect of Ponicidin on the Proliferation of Osteoblast-Like MG-63 Cells
The impact of ponicidin treatment on the proliferation level of human osteoblast-like MG-63 cells was assessed, and data was represented in Fig. 1. The ponicidin treatment remarkably improved the MG-63 cell proliferation than control. The MG-63 cells supplemented with the 5 and 10 µg/ml of ponicidin were demonstrated the appreciable increase in the proliferative level at 24 and 48 h time period than the untreated control cells (Fig. 1). These findings suggested that the ponicidin treatment appreciably improved the proliferation of MG-63 cells.
Effect of Ponicidin on the Viability of Osteoblast-Like MG-63 Cells
The influence of ponicidin treatment on the cell viability of MG-63 cells is depicted in Fig. 2. The findings exhibited that the ponicidin treatment did not affected the cell viability, instead improved the MG-63 cells’ viability. When related with control cells, the 5 and 10 µg/ml of ponicidin-supplemented cells displayed the increased cell viability, which proves the non-toxic nature of ponicidin against the MG-63 cells (Fig. 2). This finding witnessed that the ponicidin treatment appreciably improved the MG-63 cell viability.
Effect of ponicidin on the cell viability of osteoblast-like MG-63 cells. The ponicidin treatment at the dose of 5 and 10 µg/ml did not affect the cell viability; instead, it improved the viability of the osteoblast-like MG-63 cells. Each bar demonstrates the mean ± SD of triplicates assessed by one-way ANOVA and Tukey’s post hoc assay. The values do not share common superscript and statistically differ from control
Effect of Ponicidin on the Level of Osteocalcin, Collagen, and ALP Activity in the Osteoblast-Like MG-63 Cells
The contents of osteocalcin, collagen, and ALP activity in the ponicidin-administered MG-63 cells are depicted in Fig. 3. The ponicidin appreciably improved the contents of osteocalcin, collagen, and ALP activity. The administration of 5 and 10 µg/ml of ponicidin to the MG-63 cells and 24 and 48 h demonstrated the appreciable elevation in the contents of osteocalcin, collagen, and ALP activity, when compared with control cells (Fig. 3
Effect of ponicidin on the level of osteocalcin, collagen, and ALP activity in the osteoblast-like MG-63 cells. The contents of osteocalcin, collagen, and ALP activity were found augmented in the 5 and 10 µg/ml of ponicidin-treated osteoblast-like MG-63 cells. Each bar demonstrates the mean ± SD of triplicates assessed by one-way ANOVA and Tukey’s post hoc assay. “*” represents the p < 0.05, and “#” represents the p < 0.01, which statistically differ from control
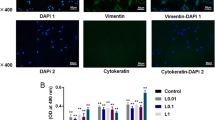
Effect of Ponicidin on the Calcium Deposition in the Osteoblast-Like MG-63 Cells
The level of calcium deposition in the ponicidin-supplemented MG-63 cells was assessed by ARS staining, and data were depicted in Fig. 4. Our findings witnessed that the ponicidin treatment appreciably improved the calcium deposition in the MG-63 cells. The 5 and 10 µg/ml of ponicidin-administered MG-63 cells displayed the remarkable improvement in the level of calcium mineralization than in the untreated control cells (Fig. 4). Hence, it was suggested that the ponicidin treatment can improve the mineralization in the MG-63 cells.
Effect of ponicidin on the calcium deposition in the osteoblast-like MG-63 cells. The 5 and 10 µg/ml of ponicidin treatment appreciably improved the calcium deposition in the MG-63 cells, which is assessed by the ARS staining technique. Each bar demonstrates the mean ± SD of triplicates assessed by one-way ANOVA and Tukey’s post hoc assay. “*” represents the p < 0.05, and “#” represents the p < 0.01, which statistically differ from control
Discussion
Osteoporosis is a common bone disease characterized by decreased bone density and quality, elevated bone fragility, and fractures [24, 25]. It was already reported both women (33%) and men (20%) have a risk of osteoporosis, especially in the forearm, hip, and spine [26, 27]. Osteoporosis signifies the accumulative disproportion in bone remodeling, due to the re-absorptive osteoclasts of the bone and excessive generation of osteoblasts to rebuild the resorptive regions [28]. The irregular remodeling can distress both cortical and trabecular bone. The loss of cortical bones results in the fractures of long bones and loss of trabecular bones results in the fractures of hip and spinal bones [29]. A previous report highlighted that nearly 5 to 10% of bone fracture cases not healed properly [30].
The bone-associated complications like fracture, bone defect, and osteoporosis lead to a great burden on individuals as well as society. The important task to maintain the healthy bones is to acquire the ideal bone mass during growth and decrease the bone loss rate during adulthood [31]. The components of the bones were entirely substituted within 3–10 years as a result of bone remodeling via bone development and resorption mechanisms. This defines the regenerative ability of the bones like healing of injury, fractures, and wounds. The bone development and resorption were controlled by two distinct cell types, i.e., osteoblasts and osteoclasts, respectively [32]. MG-63 cells are primary osteosarcoma cells, which is extensively utilized as a study model for bone regeneration researches [33,34,35].
Bone remodeling is an active mechanism coordinated by bone-developing osteoblasts and bone-resorbing osteoclast cells. The stimulation of several signaling pathways actively participates on the mechanism of bone development [36]. The disproportion on the activities of osteoclasts and osteoblasts may lead to the development of bone-related ailments. The maturation of osteoblast is a manifold process, comprising proliferation, differentiation, and calcium deposition that were regulated by the connections of the several signaling pathways [37]. During the bone remodeling, an osteoblast, which is differentiated from the osteoprogenitors, is the vital player on the new bone development via producing new extracellular matrix and promoting calcium mineralization [38]. Our findings from this study indicated that the ponicidin supplementation appreciably improved the calcium deposition in the MG-63 cells.
Osteoblasts are the most vital players of the development of bone matrix and controlling of bone resorption. The osteoblasts produce several mediators like osteopontin, osteocalcin, and ALP to modulate the activity of osteoclast [39]. The differentiation of osteoblasts is the foremost and complex biological mechanism, which is a hallmark of bone tissues [40]. Hence, the influence of sample drugs on the osteoblast differentiation and new bone development was examined by determining the mineralization by osteoblasts in vitro [41, 42]. The differentiation of osteoblasts is characterized by three distinct stages, comprising proliferation, maturation, and mineralization [43]. The capacity to support the MG-63 cell differentiation was usually examined by measuring the activity of ALP, a potential biomarker of osteogenesis [44]. ALP is an imperative enzyme highly stimulated during earlier maturation stage of osteoblasts, and the activity of ALP is regarded as a biomarker of osteoblast cell’s early differentiation [45]. ALP is highly essential to deliver the phosphate for bone mineralization [46]. In general, ALP is produced by the osteoblasts during early phase of differentiation and mediates the generation of collagen [47]. ALP is also participates in the re-organization of mineralization constituents in the extracellular matrix [47]. In this current exploration, we witnessed that the ALP activity was elevated remarkably on the ponicidin-supplemented osteoblast-like MG-63 cells in 24 and 48 h time period, which representing that the ponicidin treatment effectively triggered the early-stage osteoblast differentiation.
The bone development, metabolism, and regeneration are highly controlled by the osteocalcin and collagen that has the straight connections with availability of calcium. Osteocalcin is reported to conjugate with calcium, and hydroxyapatite is greatly activated in developing skeletal tissues assisting to mineralization and bone turnover mechanisms [48, 49]. After the completion of bone calcium mineralization, the level of deposition of calcium on the cells can be identified by numerous staining techniques. The mineralized bone matrix is primarily developed of collagen, osteopontin, osteocalcin, and inorganic hydroxyapatite. Hence, these bone-specific biomarkers are examined to assess the osteoblasts [50]. Collagen is an imperative ingredient of the extracellular matrix produced by the osteoblasts. It gives a structural background to the extracellular matrix maturation [51, 52]. In similar manner, collagen is actively participated in mineralization during differentiation of bone cells [53].
It was already reported that the osteoblasts produce several proteins to make a bone, comprising collagen, a foremost protein in the bone matrix [54]. The remarkable elevation in the content of collagen indicates the maturation of osteoblasts. The osteocalcin are the foremost Gla-containing proteins in the bone [55]. Osteocalcin is a most critical non-collagen component produced by the osteoblasts during calcium mineralization process. It is tightly connected with the hydroxyapatite in bone cells and contributes to the mediation of bone mineralization [56]. Osteocalcin is explicitly activated by bone developing osteoblasts and consists of three Gla residues that provide the capacity to osteocalcin for calcium binding to regulate the calcium metabolism via regulating its connection with hydroxyapatite. The bone resorption mechanism decreases osteocalcin’s affinity for hydroxyapatite, hence improving the discharge of osteocalcin into blood stream [57]. Additionally, a several previous research reports highlighted the functional roles of osteocalcin. Briefly, an osteocalcin knockout mouse demonstrates the remarkable depletion of bone strength, calcium deposition, and its associated metabolic mechanisms [58, 59]. In our exploration, we found that the ponicidin administration remarkably improved the content of collagen in MG-63 cells, which evidences that ponicidin treatment improves the maturation of osteoblasts.
Conclusion
In summary, our present results established that ponicidin increased the proliferation and calcium deposition in the osteoblast-like MG-63 cells. Ponicidin treatment effectively improved the contents of osteocalcin, collagen, and ALP activity in the MG-63 cells. It is recommended that ponicidin may have helpful roles on the new bone development as a hopeful therapeutic candidate for treating bone-related disease-like osteoporosis. Additional investigations on this background are needed in the future to clearly understand the underlying mechanism by which ponicidin triggers osteoblastic proliferation and differentiation.
Data Availability
Not applicable.
References
Curate, F. (2014). Osteoporosis and paleopathology: A review. Journal of Anthropological Sciences, 92, 119–146.
Zhao, X., Wu, Z. X., Zhang, Y., Gao, M. X., Yan, Y. B., Cao, P. C., Zang, Y., & Lei, W. (2012). Locally administrated perindopril improves healing in an ovariectomized rat tibial osteotomy model. PLoS One, 7, e33228.
Kling, J. M., Clarke, B. L., & Sandhu, N. P. (2014). Osteoporosis prevention, screening, and treatment: A review. Journal of Women’s Health, 23, 563–572.
Zhang, S., Wu, W., Jiao, G., Li, C., & Liu, H. (2018). MiR-455-3p activates Nrf2/ARE signaling via HDAC2 and protects osteoblasts from oxidative stress. International Journal of Biological Macromolecules, 107, 2094–2101.
Cauley, J. A., Chalhoub, D., Kassem, A. M., & Fuleihan, G. E. H. (2014). Geographic and ethnic disparities in osteoporotic fractures. Nature Reviews. Endocrinology, 10, 338.
Rao, L., & Rao, A. (2015). Oxidative stress and antioxidants in the risk of osteoporosis — Role of phytochemical antioxidants lycopene and polyphenol-containing nutritional supplements. In A. V. Rao & L. G. Rao (Eds.), Phytochemicals - Isolation, characterisation and role in human health [Internet]. IntechOpen [cited 2022 May 11]. Available from: https://www.intechopen.com/chapters/49068, https://doi.org/10.5772/60446.
Tsao, Y. T., Huang, Y. J., Wu, H. H., Liu, Y. A., Liu, Y. S., & Lee, O. K. (2017). Osteocalcin mediates biomineralization during osteogenic maturation in human mesenchymal stromal Cells. International Journal of Molecular Sciences, 18, 159.
Klumpers, D. D., Zhao, X., Mooney, D. J., & Smit, T. H. (2013). Cell mediated contraction in 3D cell-matrix constructs leads to spatially regulated osteogenic differentiation. Integr Biol (Camb), 5, 1174–1183.
Liu, T. M., & Lee, E. H. (2013). Transcriptional regulatory cascades in Runx2-dependent bone development. Tissue Engineering. Part B, Reviews, 19(3), 254–263.
Cheung, A. S., Pattison, D., Bretherton, I., Hoermann, R., Lim, J. D., Ho, E., … Grossmann, M. (2013). Cardiovascular risk and bone loss in men undergoing androgen deprivation therapy for non-metastatic prostate cancer: Implementation of standardized management guidelines. Andrology, 1, 583-589.
Gambacciani, M., & Levancini, M. (2014). Management of postmenopausal osteoporosis and the prevention of fractures. Panminerva Medica, 56, 115–131.
Park, H. S., Kim, C. G., Hong, N., Lee, S. J., Seo, D. H., & Rhee, Y. (2017). Osteosarcoma in a patient with pseudo-hypoparathyroidism type 1b due to paternal uniparental disomy of chromosome 20q. Journal of Bone and Mineral Research, 32, 770–775.
Bhutani, G., & Gupta, M. C. (2013). Emerging therapies for the treatment of osteoporosis. J Midlife Health, 4, 147–152.
Li, C., Li, Q., Liu, R., Niu, Y., Pan, Y., Zhai, Y., & Mei, Q. (2014). Medicinal herbs in the prevention and treatment of osteoporosis. American Journal of Chinese Medicine, 42, 1–22.
Zhao, W., Pu, J. X., Du, X., Su, J., Li, X. N., Yang, J. H., & Sun, H. D. (2011). Structure and cytotoxicity of diterpenoids from Isodon adenolomus. Journal of Natural Products, 74, 1213–1220.
Osawa, K., Yasuda, H., Maruyama, T., Morita, H., Takeya, K., & Itokawa, H. (1994). Antibacterial trichorabdal diterpenes from Rabdosia trichocarpa. Phytochemistry, 36, 1287–1291.
Zhang, J. F., Liu, P. Q., Chen, G. H., Lu, M. Q., Cai, C. J., Yang, Y., & Li, H. (2007). Ponicidin inhibits cell growth on hepatocellular carcinoma cells by induction of apoptosis. Digestive and Liver Disease, 39, 160–166.
Liu, J. J., Huang, R. W., Lin, D. J., Peng, J., Zhang, M., Pan, X., … Chen, F. (2006). Ponicidin, an ent-kaurane diterpenoid derived from a constituent of the herbal supplement PC-SPES, Rabdosia rubescens, induces apoptosis by activation of caspase-3 and mitochondrial events in lung cancer cells in vitro. Cancer Invest, 24, 136-148.
Bai, N., He, K., Zhou, Z., Tsai, M. L., Zhang, L., Quan, Z., … Ho, C. T. Ent-kaurane diterpenoids from Rabdosia rubescens and their cytotoxic effects on human cancer cell lines. Planta Med ,76, 140–145.
Liu, J. J., Zhang, Y., Guang, W. B., Yang, H. Z., Lin, D. J., & Xiao, R. Z. (2008). Ponicidin inhibits monocytic leukemia cell growth by induction of apoptosis. International Journal of Molecular Sciences, 9, 2265–2277.
Hsieh, T. C., Wijeratne, E. K., Liang, J. Y., Gunatilaka, A. L., & Wu, J. M. (2005). Differential control of growth, cell cycle progression, and expression of NF-kappaB in human breast cancer cells MCF-7, MCF-10A, and MDA-MB-231 by ponicidin and oridonin, diterpenoids from the Chinese herb Rabdosia rubescens. Biochemical and Biophysical Research Communications, 337, 224–231.
Liu, Y. F., Lu, Y. M., Qu, G. Q., Liu, Y., Chen, W. X., Liao, X. H., & Kong, W. M. (2015). Ponicidin induces apoptosis via JAK2 and STAT3 signaling pathways in gastric carcinoma. International Journal of Molecular Sciences, 16, 1576–1589.
Du, J., Chen, C., Sun, Y., Zheng, L., & Wang, W. (2015). Ponicidin suppresses HT29 cell growth via the induction of G1 cell cycle arrest and apoptosis. Molecular Medicine Reports, 12, 5816–5820.
Armas, L. A. (2012). Recker RR Pathophysiology of osteoporosis: New mechanistic insights. Endocrinology and Metabolism Clinics of North America, 41(3), 475–486.
Burge, R., Dawson-Hughes, B., Solomon, D. H., Wong, J. B., & King, A. (2007). Tosteson A Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. Journal of Bone and Mineral Research, 22(3), 465–475.
Reid, I. R. (2015). Short-term and long-term effects of osteoporosis therapies. Nature Reviews. Endocrinology, 11(7), 418–428.
Coughlan, T., & Dockery, F. (2014). Osteoporosis and fracture risk in older people. Clinical Medicine, 14(2), 187–191.
Brown, C. (2017). Osteoporosis: Staying strong. Nature, 550(7674), S15–S17.
Chen, H., Senda, T., & Kubo, K. Y. (2015). The osteocyte plays multiple roles in bone remodeling and mineral homeostasis. Medical Molecular Morphology, 48(2), 61–68.
Valiya Kambrath, A., Williams, J. N., & Sankar, U. (2020). An improved methodology to evaluate cell and molecular signals in the reparative callus during fracture healing. Journal of Histochemistry and Cytochemistry, 2020(68), 199–208.
Bonjour, J. P., Chevalley, T., Ferrari, S., & Rizzoli, R. (2009). The importance and relevance of peak bone mass in the prevalence of osteoporosis. Salud Publica de Mexico, 51(Suppl 1), S5–S17.
DiMasi, J. A., Hansen, R. W., & Grabowski, H. G. (2003). The price of innovation: New estimates of drug development costs. Journal of Health Economics, 22, 151–185.
Wegler, C., Wikvall, K., & Norlin, M. (2016). Effects of osteoporosis-inducing drugs on vitamin d-related gene transcription and mineralization in MG-63 and Saos-2 Cells. Basic & Clinical Pharmacology & Toxicology, 119(5), 436–442.
Zofkova, I., Davis, M., & Blahos, J. (2017). Trace elements have beneficial, as well as detrimental effects on bone homeostasis. Physiological Research, 66(3), 391–402.
Plikerd, W. D., Trivedi, M. K., Branton, A., Trivedi, D., Nayak, G., Gangwar, M., & Jana, S. (2018). Impact of biofield energy healing treated Vitamin D3 on human osteoblast cell line (MG-63) for bone health. American Journal of Clinical and Experimental Medicine, 6(1), 1–9.
Raggatt, L. J., & Partridge, N. C. (2010). Cellular and molecular mechanisms of bone remodeling. Journal of Biological Chemistry, 285, 25103–25108.
Zaidi, M. (2007). Skeletal remodeling in health and disease. Nature Medicine, 13, 791–801.
Twine, N. A., Chen, L., Pang, C. N., Wilkins, M. R., & Kassem, M. (2014). Identification of differentiation-stage specific markers that define the ex vivo osteoblastic phenotype. Bone, 67, 23–32.
Sudo, H., Kodama, H. A., Amagai, Y., Yamamoto, S., & Kasai, S. (1983). In vitro differentiation and calcification in a new clonal osteogenic cell line derived from newborn mouse calvaria. Journal of Cell Biology, 96, 191–198.
Ducy, P., Schinke, T., & Karsenty, G. (2001). The osteoblast: A sophisticated fibroblast under central surveillance. Science, 289, 1501–1504.
Kostenuik, P. J., Halloran, B. P., Morey-Holton, E. R., & Bikle, D. D. (1997). Skeletal unloading inhibits the in vitro proliferation and differentiation of rat osteoprogenitor cells. American Journal of Physiology, 273, E1133–E1139.
Kostenuik, P. J., Harris, J., Halloran, B. P., Turner, R. T., Morey-Holton, E. R., & Bikle, D. D. (1999). Skeletal unloading causes resistance of osteoprogenitor cells to parathyroid hormone and to insulin-like growth factor-I. J Bone Min Res, 14, 21–31.
Kalajzic, I., Staal, A., Yang, W. P., Wu, Y., Johnson, S. E., Feyen, J. H., … Rowe, D. W. (2005). Expression profile of osteoblast lineage at defined stages of differentiation. J Biol Chem, 280, 24618-24626.
Kotliarova, M. S., Zhuikov, V. A., Chudinova, Y. V., Khaidapova, D. D., Moisenovich, A. M., & Kon’kov, A. S., … Shaitan, K. V. (2016). Induction of osteogenic differentiation of osteoblast-like cells MG-63 during cultivation on fibroin microcarriers. Moscow University Biological Science Bulletin, 71(4), 212–217.
Chaturvedi, R., Singha, P. K., & Dey, S. (2013). Water soluble bioactives of nacre mediate antioxidant activity and osteoblast differentiation. PLoS One, 8, e84584.
Wei, J., & Karsenty, G. (2015). An overview of the metabolic functions of osteocalcin. Reviews in Endocrine & Metabolic Disorders, 16, 93.
Marie, P. J. (2002). Role of N-cadherin in bone formation. Journal of Cellular Physiology, 190, 297–305.
Feng, H., Cheng, T., Pavlos, N. J., Yip, K. H., Carrello, A., Seeber, R., Eidne, K., Zheng, M. H., & Xu, J. (2008). Cytoplasmic terminus of vacuolar type proton pump accessory subunit Ac45 is required for proper interaction with V(0) domain subunits and efficient osteoclastic bone resorption. Journal of Biological Chemistry, 283(19), 13194–13204.
Feng, J., Shi, Z., & Ye, Z. (2008). Effects of metabolites of the lignans enterolactone and enterodiol on osteoblastic differentiation of MG-63 cells. Biological &/and Pharmaceutical Bulletin, 31(6), 1067–1070.
Kasperk, C., Wergedal, J., Strong, D., Farley, J., Wangerin, K., Gropp, H., Ziegler, R., & Baylink, D. J. (1995). Human bone cell phenotypes differ depending on their skeletal site of origin. Journal of Clinical Endocrinology and Metabolism, 80, 2511–2517.
Pochampally, R. R., Horwitz, E. M., DiGirolamo, C. M., Stokes, D. S., & Prockop, D. J. (2005). Correction of a mineralization defect by overexpression of a wild-type cDNA for COL1A1 in marrow stromal cells (MSCs) from a patient with osteogenesis imperfecta: A strategy for rescuing mutations that produce dominant-negative protein defects. Gene Therapy, 12(14), 1119–1125.
Sakkers, R., Kok, D., Engelbert, R., van Dongen, A., Jansen, M., Pruijs, H., … Uiterwaal, C. (2004). Skeletal effects and functional outcome with olpadronate in children with osteogenesis imperfecta: A 2-year randomised placebo-controlled study. Lancet, 363(9419), 1427–1431.
Mathews, S., Gupta, P. K., Bhonde, R., & Totey, S. (2011). Chitosan enhances mineralization during osteoblast differentiation of human bone marrow-derived mesenchymal stem cells, by upregulating the associated genes. Cell Proliferation, 44(6), 537–549.
Reffitt, D. M., Ogston, N., Jugdaohsingh, R., Cheung, H. F., Evans, B. A., Thompson, R. P., Powell, J. J., & Hampson, G. N. (2003). Orthosilicic acid stimulates collagen type 1 synthesis and osteoblastic differentiation in human osteoblast-like cells in vitro. Bone, 32, 127–135.
Wen, L. P., Chen, J. P., Duan, L. L., & Li, S. Z. (2018). Vitamin K-dependent proteins involved in bone and cardiovascular health. Molecular Medicine Reports, 18, 3–15.
Cosman, F., Shen, V., Morgan, D., Gordon, S., Parisien, M., Nieves, J., & Lindsay, R. (2000). Biochemical responses of bone metabolism to 1,25-dihydroxyvitamin D administration in black and white women. Osteoporosis International, 11(3), 271–277.
Mizokami, A., Kawakubo-Yasukochi, T., & Hirata, M. (2017). Osteocalcin and its endocrine functions. Biochemical Pharmacology, 132, 1–8.
Diegel, C. R., Hann, S., Ayturk, U. M., Hu, J. C. W., Lim, K. E., Droscha, C. J., … Williams, B. O. (2020). An osteocalcin-deficient mouse strain without endocrine abnormalities. PLoS Genet, 16, 1008361.
Moriishi, T., Ozasa, R., Ishimoto, T., Nakano T., Hasegawa T., Miyazaki T., … Komori, T. (2020). Osteocalcin is necessary for the alignment of apatite crystallites, but not glucose metabolism, testosterone synthesis, or muscle mass. PLoS Genet, 16, e1008586.
Author information
Authors and Affiliations
Contributions
All authors contributed equally.
Corresponding author
Ethics declarations
Ethics Approval
All works have been done under the guidelines of Institutional Ethics Committee.
Consent to Participate
All authors have their consent to participate.
Consent for Publication
All authors have their consent to publish their work.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Hao, P., Li, H. et al. Ponicidin Treatment Improved the Cell Proliferation, Differentiation, and Calcium Mineralization on the Osteoblast-Like MG-63 Cells. Appl Biochem Biotechnol 194, 3860–3870 (2022). https://doi.org/10.1007/s12010-022-03927-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-022-03927-3