Abstract
Purpose of Review
Although external ventricular drains (EVDs) are widely used, there is a lot of variability in how they are managed. This review will provide an update on the management of EVDs, based on the current evidence.
Recent Findings
Bundles of care focused on aseptic techniques for EVD insertion, maintenance, and care are likely to prevent EVD-associated infections. EVD management in subarachnoid hemorrhage (SAH) found no clinical advantage to gradual weaning over rapid weaning with an intermittent drainage strategy versus a continuous strategy. Rapid weaning was associated with a shorter length of stay, lower incidence of ventriculostomy-associated infections, and EVD blockages. EVD placements done by mid-level practitioners found no significant differences in accuracy or infection rates when compared to placement by neurosurgeons which could be of value in low resource centers. Intraventricular fibrinolytics for treatment of intraventricular hemorrhage may not affect functional outcomes but hasten ventricular blood clearance and may lower mortality compared to no treatment.
Summary
EVDs are indicated when CSF diversion and intracranial pressure monitoring are needed. There is variability in insertion, management, and removal of EVDs, as well as administration of intraventricular medications. More research is required to standardize EVD-related processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An external ventricular drain (EVD) insertion or ventriculostomy is one of the most common procedures performed by neurosurgeons with an estimated over 20,000 EVD placements per year in the USA alone [1, 2]. After being first attempted in the eighteenth century, EVD insertion techniques, indications, and materials used have undergone several changes to date particularly with the advancements of technology, knowledge of infection control, and safety [3]. However, there remains significant variability surrounding EVD practices from insertion, infection control measures, and administration of intraventricular medications to strategies for drainage and removal [4••, 5]. This review will provide an overview of the management of EVDs and treatment of some common related complications.
Disease states
There are two primary indications for EVD insertion: drainage of cerebrospinal fluid (CSF) and measurement of intracranial pressure (ICP). The commonly encountered conditions where EVDs are inserted include:
-
1.
Subarachnoid Hemorrhage (SAH)
This is probably the most common indication for EVD placement [6]. Intraventricular hemorrhage (IVH) secondary to high grade SAH can lead to acute obstructive hydrocephalus requiring EVD insertion. Hydrocephalus occurs secondary to obstruction of the arachnoid villi (the natural CSF absorbent system) and the obstruction of the ventricular and cisternal drainage systems [7]. The incidence of hydrocephalus in aneurysmal SAH is around 20–30%, mostly occurring acutely within 48 h after bleed onset, but also can be delayed by weeks or even months after hemorrhage [8]. EVD insertion in patients presenting with SAH-related hydrocephalus is recommended as it provides a temporary diversion of the CSF outside the brain as well as ICP monitoring [9]. Aneurysmal rebleeding is a theoretical risk after inserting an EVD. This may occur because of rapid CSF drainage and fluctuating ICP immediately after EVD insertion in SAH patients with an unsecured aneurysm. One retrospective study found that the volume of CSF drainage was highly correlated with the probability of in-hospital aneurysmal rebleeding [10]. However, other studies found no increased risk [11, 12]. It is prudent to carefully control the amount of CSF drainage and avoid over-drainage prior to aneurysm obliteration.
-
2.
Traumatic Brain Injury (TBI)
EVDs are one of the commonly used types of ICP monitors in TBI patients along with intraparenchymal devices. As per the 2016 Brain Trauma Foundation (BTF) guidelines, ICP monitoring is indicated in all salvageable TBI patients with abnormal CT scans [13]. It is also indicated with a normal CT scan, if two of the following three risk factors are present: age > 40 years, motor posturing, and SBP < 90 mmHg. An EVD can serve in these conditions both as a diagnostic tool for ICP monitoring as well as for immediate therapy to drain CSF in cases of high ICP with increased ventricular size. An intraparenchymal fiberoptic probe is preferred if the goal is only to measure ICP in the presence of collapsed ventricles secondary to diffuse cerebral edema. One prospective observational study compared EVDs to intraparenchymal fiberoptic probes in TBI patients and found a better 6-month Glasgow Outcome Scale score in the EVD group [14]. It also found less refractory high ICP episodes and better 1-month and 6-month survival rates in the EVD group with similar rates of device-related complications.
-
3.
Intraventricular Hemorrhage (IVH)
Extension of the hemorrhage into the ventricular system, i.e., IVH, is an independent risk factor for poor prognosis [15, 16]. IVH following ICH or SAH can be limited to a small layer of blood in the lateral ventricles, or a large extension casting the entire ventricular system. An IVH amount of more than 20 mL has been demonstrated as a strong predictor of poor outcome [17]. Elevated ICP and obstructive hydrocephalus are commonly associated with ICH and IVH which would require emergent EVD insertion to prevent worse outcomes [16]. The outcomes remain poor in many patients with high-grade hemorrhages despite EVD insertion. This may be due to the primary etiology of the bleed, its location, and the toxic effects of IVH on the adjacent brain structures and vasculature leading to cell ischemia and fibrosis [18, 19]. CSF drainage may not clear the blood from the ventricles. Therefore, injection of fibrinolytic agents such as alteplase through the EVD, intraventricular fibrinolysis, has been studied with the expectation that faster clearance of intraventricular blood will lead to improved outcomes. Despite the promising safety profile and results from the CLEAR II trial (Thrombolytic Removal of Intraventricular Hemorrhage in Treatment of Severe Stroke), the larger randomized, placebo-controlled phase 3 trial (CLEAR III) showed that routine irrigation with alteplase did not substantially improve functional outcomes at the modified Ranking Scale (mRS) score of 3 cutoff compared with irrigation with saline alone [20]. Numerous systematic reviews and meta-analyses have been conducted reviewing the role of intraventricular fibrinolysis in patients with IVH. The most recent one by van Solinge et al. showed a lower risk of EVD obstruction, faster clearance of blood from the 3rd and 4th ventricles, and reduction in mortality rates in patients receiving intraventricular fibrinolytics compared to EVD alone. There was no significant difference in functional outcomes and rates of ventriculitis [21••].
-
4.
Acute Ischemic Stroke
EVDs can also be used for ICP monitoring and CSF drainage in severe ischemic strokes associated with cerebral edema, mass effect, and midline shift. Insertion can be either prior to or after decompressive craniectomy, if ICP elevation remains a concern. EVD use in this situation remains controversial secondary to a lack of randomized controlled studies. A small prospective study suggested that ICP monitoring of large hemispheric ischemic strokes can predict clinical deterioration and final outcomes [22]. However, a later study showed that severe brainstem herniation and pupillary changes can occur despite normal ICP readings [23]. Thus, ICP monitoring should not be a substitute to frequent bedside clinical exam and radiographic monitoring. EVDs can also be used for temporary relief of obstructive hydrocephalus secondary to posterior fossa large cerebellar ischemic strokes. Cautious CSF drainage should be applied to prevent upward brainstem herniation which is frequently encountered on imaging prior to EVD insertion due to posterior fossa space occupying lesion; however, this remains safe upon EVD insertion in one study by Braksick et al. [24]. It should be considered as a temporizing measure until definitive surgical treatment is achieved. The American Stroke Association recommends surgical management with posterior fossa decompression in favor of EVD placement alone [25].
-
5.
Central Nervous System Infections
In the neurological critical care unit (NCCU), ventriculostomy-associated infection is a well-known complication after EVD placement [26]. The mainstay of treatment for such infections is intravenous antibiotics. However, in certain cases, refractory to standard intravenous treatment, intraventricular or intrathecal antibiotics can be considered. This is discussed in more detail in a subsequent section. Another indication for intraventricular antibiotics is a severe nosocomial meningitis with obstructive hydrocephalus refractory to intravenous antibiotics. EVD placement and intrathecal antibiotics would be next best therapeutic step in such cases [27].
Placement of EVD
The technique of placing EVDs is beyond the scope of this review. Due to the urgent nature of this procedure, EVDs are often placed at the bedside in the intensive care unit (ICU) or in the emergency departments. Timely ventriculostomy placement is critical to avoid secondary brain tissue damage from prolonged elevations of ICP. Alert protocols including team members across the patient’s pathway within the hospital have been demonstrated to reduce delays [28••]. EVDs are typically placed by neurosurgeons or neurosurgery residents. There is no significant difference in EVD placement accuracy based on operator experience or the location of EVD insertion (operating room or bedside) [29••]. More recently, neurointensivists and even advanced practice providers (APPs) such as nurse practitioners (NPs) and physicians assistants (PAs) have taken up this role after undergoing appropriate training [30]. Simulation using virtual reality and smartphone devices is aimed to reduce learning curves and improve placement in emergency situations [31••, 32]. In one retrospective analysis, EVDs placed by NPs and PAs were compared with EVDs placed by neurosurgeons at the same center [33••]. The rates of hemorrhage, infection, and placement accuracy were similar between the two groups. Having non-neurosurgeons be able to place EVDs has many advantages. It may allow for more prompt intervention as intensivists and APPs are often situated on-site and can place the EVDs at the bedside without any delay.
The use of prophylactic systemic antibiotics peri-procedurally during EVD placement is a common practice in many institutions. The results of studies that looked at the effect of prophylactic antibiotic use have been inconclusive. Older studies suggested that prophylactic antibiotics resulted in a reduction of ventriculostomy-related infections (VRI), recently termed ventriculostomy-associated infections (VAI), at the expense of selecting for resistant bacteria [34]. However, subsequent studies did not find any reduction in VAI rates among patients who received antibiotics throughout the duration of EVD treatment compared to those who did not, with increased rates of nosocomial infections and cost in the group receiving antibiotics [35]. According to a recent systematic review by Lord et al. those who received a prolonged duration of intravenous antibiotics throughout the EVD use were at an increased risk of developing resistant organisms, C. difficile colitis, and increased healthcare cost with mixed results in reduction of VAI [36••]. The Neurocritical Care Society suggests one dose of prophylactic antibiotics prior to insertion of EVDs [37]. An additional step that has now become standard is tunneling of EVD catheters as a means of reducing infection risk. A recent meta-analysis showed that tunnel lengths of 5 to 10 cm were associated with the lowest rate of VAI [38••]. An important consideration before placing an EVD is whether to place a standard silicone catheter or an antimicrobial-impregnated one [40]. Antibiotic-impregnated EVDs were first introduced about two decades ago, followed soon after by silver-impregnated catheters. Both have shown a decreased rate of catheter-related infections compared to standard EVDs alone in multiple studies and meta-analyses [39–41]. In an RCT where 288 patients were randomized to get antibiotic-impregnated catheters versus standard silicone catheters, the VAI rate was significantly reduced in patients with antibiotic-impregnated catheters compared to the control group (1.3% compared with 9.4%, respectively, p = 0.002) [42]. Another study showed that the combination of antibiotic-impregnated catheters and an evidence-based EVD insertion and management bundle decreased VAI rates from 8.2 to 1% (p = 0.0005) [40]. The mean duration to onset of infection has also been found to be significantly prolonged with antibiotic-impregnated catheter use compared to standard catheters (8.8 days and 4.6 days, respectively, p = 0.002) [43]. In a large meta-analysis pooling 4399 patients from 4 randomized clinical trials and 7 observational studies, there was a 62% relative reduction in infection rates when using antibiotic-impregnated devices [39]. The Neurocritical Society in their evidence-based consensus statement recommends usage of antimicrobial-impregnated catheters as part of a bundle to minimize infection risk associated with EVDs [37]. Finally, chlorhexidine-impregnated dressings, which are widely utilized to reduce central line colonization and catheter-related bloodstream infection, have also been used with EVDs to reduce rates of VAI. A recent meta-analysis that included 5 studies found a significant reduction of EVD-associated infections with chlorhexidine use (7.9% vs 1.7%, p = 0.04) [44••]. However, the authors reported a significant risk of bias in all the included studies.
Table 1 offers a practical suggestion on how to minimize ventricular-associated infections.
Setting up and managing an EVD
After placing the EVD, it is standard practice to raise the patient’s head of bed to an angle of 30°, keep the neck in a neutral position, and attach the EVD CSF collection system to a pole near the head end of the bed (Fig. 1). The EVD collection system is zeroed at the level of the foramen of Monroe. This corresponds to the external auditory meatus in the supine position and the midsagittal line in the lateral position [45••]. The height of the EVD collection system is determined by the indication for the procedure. If placed for treating SAH, the level is initially set high, often at 20 cm H2O, to prevent over-drainage and possible rebleeding of the unsecured aneurysm. In surgical cases, it is usually set at a lower level and then gradually increased. While it is common practice to have an open drainage system, this practice has been called into question by newer studies in aneurysmal SAH [46••, 47]. With an open drainage system, CSF is allowed to drain continuously and ICPs are checked periodically, typically once an hour. While this does facilitate ease of use, it does not allow for continuous ICP monitoring. In patients with SAH, a continuous drainage strategy has been associated with more complications compared to an intermittent drainage strategy, wherein CSF is only drained when ICP reaches a certain predetermined threshold. Single center studies have shown associations with decreased length of stay, lower ventriculo-peritoneal shunt (VPS) rates, and decreased risk of malfunctioning catheters with closed drainage systems [48–50]. A prospective study by Olson et al. reported a higher rate of nonpatent EVDs in the continuous group versus the intermittent group (44.1% vs 11.5%, respectively; OR 4.35, 95% CI 1.18–16.10) along with a higher rate of ventriculitis as well (17.6% vs 3.8%, respectively; OR 5.36, 95% CI 0.60–47.57) [49]. They also found a strong association (alpha = 0.01) between loss of patency and infection, regardless of group assignment (OR 7.96). They felt that the higher rate of infection was probably due to higher rates of EVD manipulation due to loss of patency. A retrospective study by Rao et al. observed higher rates of VP shunt placement (35% vs 13%, p = 0.001) and ICU length of stay (16.9 days vs 14.2 days, p = 0.001) and double the rates of non-functioning EVD in the continuous group versus the intermittent group (30% vs 15%, respectively; OR 0.29, CI 0.12–0.71, p = 0.006) [48]. A recent meta-analysis that included 1549 patients concluded that intermittent CSF drainage was associated with lower EVD infection rates (2% vs 12%; RR = 0.20, 95% CI 0.05–0.72, I-squared = 0%) and EVD blockages (15% vs 36%; RR = 0.45, 95% CI 0.27–0.74) compared to continuous strategies [46••]. Interestingly, they also observed that the amount of CSF drainage per day was similar in both groups (129.6 mL/day with continuous drainage versus 119.5 mL/day with intermittent drainage). Various explanations have been put forth to explain these findings. Rao et al. theorize that a closed EVD “…might involve early recruitment of CSF outflow pathways. A closed EVD and relatively higher CSF compartment pressures could facilitate CSF resorption through arachnoid granulations.” They also suggest that an open system might augment CSF production due to lower CSF pressures and increase the risk of blockage.
The data is less clear in non-SAH patients. In a matched cohort study of severe TBI patients treated with continuous versus intermittent EVD draining approaches, the mean ICP was lower in the continuous group, with better overall ICP control [51]. When evaluating for infection, EVD systems are frequently used to collect CSF samples. Care must be taken during these maneuvers as frequent CSF sampling has been associated with an increased risk of EVD-related infections [52, 53]. CSF sampling should only be done when infection is suspected or to gauge treatment response.
External ventricular drain complications and their management
Given the invasive nature of EVDs and despite appropriate care and maintenance, EVDs can be complicated by malfunction due to malposition, dislodgment, obstruction, hemorrhage, and infection, all of which can result in increasing ICU length of stay and contribute to significant morbidity and mortality as discussed in the following section.
Ventriculostomy-associated infection
Ventriculostomy-associated infection is a major concern after catheter placement. Infection rates have been reported in the range of 0 to 22%, but mostly around 10% or less [54–56]. In a large scale surveillance study in a neurological ICU of a major tertiary care center, the incidence rate (per 1000 device days) of VAI was 4.0 [26]. Coagulase negative Staphylococcus is usually the most common pathogen isolated. Other common organisms include Staphylococcus aureus, Klebsiella species, and Pseudomonas species [57••]. The diagnosis of VAI can be challenging due to the lack of a consistent definition in the literature. CSF inflammation and inflammatory ventriculitis can be seen with IVH and following neurosurgery and not only with infection. Many studies have used the definition of VAI set by the CDC which is based on a combination of a positive CSF culture, typical laboratory findings, and clinical symptoms. Risk factors associated with VAI include SAH, IVH, craniotomy, depressed skull fracture, and history of diabetes mellitus [55, 56, 58••]. In a subarachnoid hemorrhage study using Bayesian Model Averaging, only higher-grade Hunt and Hess, and diabetes mellitus were associated with the probability of developing VAI; craniotomy did not increase the probability [59]. VAI can result from inoculation of pathogens during EVD placement or due to contamination of EVD postoperatively by migration of organisms along the cutaneous tract. It may also be introduced secondary to frequent EVD manipulation [56]. Many studies have shown a direct correlation between the risk of VAI and the duration of EVD placement. Most studies have reported a lower VAI rate in the first 5 days of EVD drainage and that the infection rate increases significantly after 5 to 10 days of EVD placement [60–62]. Prophylactic or regular exchange of EVD catheters after 5 days of EVD placement has not been shown to decrease VAI risk. On the other hand, the number of EVD placements has been found to be a strong predictor of VAI [63]. Hence, it is recommended to remove the EVD as early as the clinical situation allows and to avoid routine changes of EVD [37]. As discussed earlier, antibiotic-impregnated catheters have been shown to potentially reduce VAI rates. VAI should be considered in the differential diagnosis of any patient with an EVD who has signs and symptoms suggestive of an infection. Initial VAI treatment involves removal or exchange of the catheter and administration of broad-spectrum intravenous antibiotics with activity against gram-positive as well as gram-negative pathogens. Subsequent targeted antibiotic therapy can be tailored to CSF culture and susceptibility results and continued for 10 to 14 days following last positive CSF culture [27]. Brain MRI with contrast-enhanced or DWI sequences can help guide the antimicrobial course particularly in cases poorly responsive to treatment by identifying loculated infections or abscess formation. Intraventricular antibiotic administration should be considered in patients who do not respond to intravenous antibiotics alone or in infections caused by multi-drug-resistant organisms. They have also been used to treat infections with organisms with high MIC to intravenous antibiotics that do not achieve adequate CSF concentrations. Most of the studies done in this area are small, retrospective in design, and not sufficiently powered to detect significant differences in meaningful clinical outcomes [57••, 64, 65]. However, many of them have demonstrated faster achievement of CSF sterility and improvement of CSF parameters with the use of intrathecal antibiotics. In a multicenter retrospective cohort study that included 105 patients who received intraventricular antibiotics, CSF sterilization occurred in 88% of patients with recurrence of positive cultures in about 10% [57••]. In another study of 34 post-neurosurgical patients with persistently positive CSF cultures despite appropriate intravenous antibiotics, the addition of intraventricular antibiotics resulted in CSF sterilization at an average of 2.9 days [65]. Interestingly, within 24 h of initiating intraventricular antibiotics, 50% of these patients had negative CSF cultures. It is to be noted that no specific antibiotic has been approved for intrathecal use by the FDA. The antibiotics most ordered are vancomycin and aminoglycosides [57••]. Intrathecal antifungal treatment can also be considered for special fungal infections such as coccidial meningitis and cryptococcal meningitis. It is prudent to involve infectious disease specialists in these situations and remain vigilant regarding possible increase in ICP with such treatment secondary to the introduction of exogenous therapy into the ventricular system.
Hemorrhage
The incidence of ICH after EVD placement varies widely in the literature. While single center studies have reported hemorrhage rates as high as 56% [66••], three meta-analyses reported incidence rates between 5.7 and 8.4% [67–69]. The definition of EVD-related hemorrhages is important in this context—new catheter tract hemorrhage vs spontaneous new or enlargement of existing ICH/IVH—as most hemorrhages are asymptomatic. Clinically significant hemorrhage rates range from 0.6 to 0.8% with significantly increased risk if they have received anti-platelet agents within 96 h of EVD insertion [70]. Coagulopathy, therapeutic anticoagulation, and antiplatelet use are all known to be associated with increased risk of hemorrhage [71, 72]. The precise value of the coagulation parameters that make it safe to insert EVDs is not clear. One small retrospective study involving 71 patients with TBI compared bleeding risk in 3 groups of patients—those with an INR < 1.2, between 1.2 and 1.4, and between 1.4 and 1.6 [73]. They found no difference in hemorrhage rates between these groups and concluded that the insertion of an EVD was safe in this INR range. A good practice statement from the Neurocritical Care Society recommends correcting coagulopathy prior to EVD insertion, unless it is a dire emergency [37].
Catheter misplacement
EVD malposition rates can range from 4 to 20% [1, 74, 75]. EVD catheters are usually placed using free hand techniques by neurosurgeons in most centers worldwide. The accuracy of placement is graded by the Kakarla methodology, with optimal position (grade 1) being the catheter tip in the frontal horn of the ipsilateral lateral ventricle or third ventricle [1]. Based on these criteria, Kakarla et al. found that optimal catheter position was achieved in about 77% of the cases in their retrospective review of 346 cases. Newer techniques using image guidance are available but not yet popular in usage. A recent meta-analysis of studies including more than 3000 patients comparing free hand technique to image guidance methodology reported higher accuracy and reduced rates of drain failure with image guidance, despite similar number of attempts [76••]. The added time needed for set up and the bulkiness of the equipment make them less useful in emergency situations. Newer devices using holograms and smartphone applications show promise in overcoming some of these limitations [77, 78]. Ultrasound-guided insertion is also gaining popularity especially in certain countries like UK [79••]. Newer probes can transduce via burr holes making real-time image acquisition possible. However, more scalable research and evidence are needed.
Catheter malfunction
EVD catheter malfunction secondary to catheter obstruction results from misplacement or migration of the EVD catheter tip into the brain parenchyma. Occlusion of the EVD catheter lumen by blood clots and cellular debris will lead to under-drainage or cessation of CSF drainage and may result in a rapid rise in ICP [80, 81]. The incidence rate of EVD malposition is in the range of 4 to 20%, the majority of which do not result in significant clinical complications, but about 4% require EVD replacement [1, 74]. Measures to resolve obstruction include distal EVD tube flushing. If this fails, the proximal EVD tubing can be flushed with a small amount of sterile saline by experienced medical professionals under strict aseptic conditions. We sometimes use intraventricular alteplase if we suspect a blood clot occluding the EVD with no contraindication to its use. If this is not successful, then EVD replacement may be necessary. Removing and reintroducing an EVD carry its own risk of secondary hemorrhage and CSF infection.
Removal of EVD
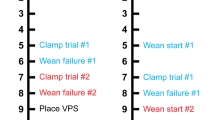
There are two well-described approaches to removing an EVD. The more popular one is the gradual weaning approach, which is done by raising the level of the EVD everyday by an average of 5 cm H20 at a time and then doing a clamp trial when the level has reached a predetermined target, usually 20–25 cm H20. The other approach is immediate clamping and monitoring for 24 h. During the weaning period and clamp trial, the patient is closely monitored for the development of any neurological or radiologic worsening. If this occurs, the EVD is opened, and patient stabilized. The options are then to either repeat a clamp trial or proceed with shunt placement. The superiority of one approach over the other has been a matter of great debate. The only prospective randomized controlled clinical trial (RCT) comparing gradual weaning versus rapid weaning found that a rapid wean with immediate clamping was safe and led to shorter duration of EVD use and shorter lengths of stay in the ICU and hospital [50]. There was no difference in ventriculo-peritoneal shunt placement rates in this study. In contrast, in a prospective multicenter observational study, a rapid wean protocol was associated with a lower rate of VPS, 2.1 fewer EVD days, and decrease ICU length of stay [82••]. A recent meta-analysis compared the two weaning methods and found no significant benefits with gradual weaning but a significant reduction in hospital length of stay in the rapid weaning group (30.2 days versus 26.7 days, respectively, 95% CI 0.22–0.47, I-squared = 0%) [46••]. Again, there was no significant difference in rates of shunt placement between the groups. While the decision to choose one approach over the other depends mainly on the individual situation of each patient, considering the length of EVD placement, the ability for meaningful clinical assessment during the weaning, and the amount of initial IVH and its clearance, the American Stroke Association recommends a rapid wean approach in patients with SAH [83]. So too does the Neurocritical Care Society, which advises to wean EVDs as quickly as clinically feasible, ostensibly to reduce the risk of VAI [37].
Conclusion
EVDs remain an important part of managing certain neurological emergencies in the NCCU, both for diagnostic and therapeutic purposes. Although there is an accumulating body of evidence favoring practices such as continuous ICP monitoring over continuous CSF drainage and rapid weaning versus gradual weaning, the neurosurgical community has not widely adopted these changes in its practice. New technical modalities that can help in improving accuracy of EVD placements are available, including holographic technology and smartphone apps. More research in several areas of EVD usage is needed, including larger multicenter RCTs on continuous versus intermittent CSF drainage, more data on effectiveness of intraventricular antibiotics, optimal methods of weaning/removal of EVDs, and further refinement of image guidance technology with RCTs comparing them to free hand techniques. With the expansion of the field of neurocritical care, more focused training programs on EVD insertion and management for neurointensivists and advanced practice providers (NPs/PAs) are mandated, as the available evidence seems to suggest that this is feasible.
Change history
15 September 2022
Adding ORCID of Dr Jamil R. Dibu.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kakarla UK, Kim LJ, Chang SW, Theodore N, Spetzler RF. Safety and accuracy of bedside external ventricular drain placement. Neurosurgery. 2008;63(1 Suppl 1):ONS162–6; discussion ONS6–7. https://doi.org/10.1227/01.neu.0000335031.23521.d0.
O'Neill BR, Velez DA, Braxton EE, Whiting D, Oh MY. A survey of ventriculostomy and intracranial pressure monitor placement practices. Surg Neurol. 2008;70(3):268–73; discussion 73. https://doi.org/10.1016/j.surneu.2007.05.007.
Srinivasan VM, O’Neill BR, Jho D, Whiting DM, Oh MY. The history of external ventricular drainage. J Neurosurg. 2014;120(1):228–36. https://doi.org/10.3171/2013.6.JNS121577.
•• Thamjamrassri T, Yuwapattanawong K, Chanthima P, Vavilala MS, Lele AV, Collaborators EVS. A narrative review of the published literature, hospital practices, and policies related to external ventricular drains in the United States: the External Ventricular Drain Publications, Practices, and Policies (EVDPoP) study. J Neurosurg Anesthesiol. 2022;34(1):21–8. https://doi.org/10.1097/ANA.0000000000000694. This narrative review is based on surveys conducted to evaluate EVD management practices in the USA with the main focus on practices to reduce EVD-associated infections. It found modest adherence to guidelines recommendations.
Baum GR, Hooten KG, Lockney DT, Fargen KM, Turan N, Pradilla G, et al. External ventricular drain practice variations: results from a nationwide survey. J Neurosurg. 2017;127(5):1190–7. https://doi.org/10.3171/2016.9.JNS16367.
Gigante P, Hwang BY, Appelboom G, Kellner CP, Kellner MA, Connolly ES. External ventricular drainage following aneurysmal subarachnoid haemorrhage. Br J Neurosurg. 2010;24(6):625–32. https://doi.org/10.3109/02688697.2010.505989.
Ellington E, Margolis G. Block of arachnoid villus by subarachnoid hemorrhage. J Neurosurg. 1969;30(6):651–7. https://doi.org/10.3171/jns.1969.30.6.0651.
Germanwala AV, Huang J, Tamargo RJ. Hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010;21(2):263–70. https://doi.org/10.1016/j.nec.2009.10.013.
Ransom ER, Mocco J, Komotar RJ, Sahni D, Chang J, Hahn DK, et al. External ventricular drainage response in poor grade aneurysmal subarachnoid hemorrhage: effect on preoperative grading and prognosis. Neurocrit Care. 2007;6(3):174–80. https://doi.org/10.1007/s12028-007-0019-7.
van Lieshout JH, Pumplun I, Fischer I, Kamp MA, Cornelius JF, Steiger HJ, et al. Volume of cerebrospinal fluid drainage as a predictor for pretreatment aneurysmal rebleeding. J Neurosurg. 2018;128(6):1778–84. https://doi.org/10.3171/2017.2.JNS162748.
McIver JI, Friedman JA, Wijdicks EF, Piepgras DG, Pichelmann MA, Toussaint LG 3rd, et al. Preoperative ventriculostomy and rebleeding after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2002;97(5):1042–4. https://doi.org/10.3171/jns.2002.97.5.1042.
Hellingman CA, van den Bergh WM, Beijer IS, van Dijk GW, Algra A, van Gijn J, et al. Risk of rebleeding after treatment of acute hydrocephalus in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2007;38(1):96–9. https://doi.org/10.1161/01.STR.0000251841.51332.1d.
Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6–15. https://doi.org/10.1227/NEU.0000000000001432.
Liu H, Wang W, Cheng F, Yuan Q, Yang J, Hu J, et al. External ventricular drains versus intraparenchymal intracranial pressure monitors in traumatic brain injury: a prospective observational study. World Neurosurg. 2015;83(5):794–800. https://doi.org/10.1016/j.wneu.2014.12.040.
Atzema C, Mower WR, Hoffman JR, Holmes JF, Killian AJ, Wolfson AB, et al. Prevalence and prognosis of traumatic intraventricular hemorrhage in patients with blunt head trauma. J Trauma. 2006;60(5):1010–7; discussion 7. https://doi.org/10.1097/01.ta.0000218038.28064.9d.
Nieuwkamp DJ, Rinkel GJ, Silva R, Greebe P, Schokking DA, Ferro JM. Subarachnoid haemorrhage in patients > or = 75 years: clinical course, treatment and outcome. J Neurol Neurosurg Psychiatry. 2006;77(8):933–7. https://doi.org/10.1136/jnnp.2005.084350.
Roos YB, Hasan D, Vermeulen M. Outcome in patients with large intraventricular haemorrhages: a volumetric study. J Neurol Neurosurg Psychiatry. 1995;58(5):622–4. https://doi.org/10.1136/jnnp.58.5.622.
Mayfrank L, Kissler J, Raoofi R, Delsing P, Weis J, Kuker W, et al. Ventricular dilatation in experimental intraventricular hemorrhage in pigs. Characterization of cerebrospinal fluid dynamics and the effects of fibrinolytic treatment. Stroke. 1997;28(1):141–8. https://doi.org/10.1161/01.str.28.1.141.
Xi G, Keep RF, Hoff JT. Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol. 2006;5(1):53–63. https://doi.org/10.1016/S1474-4422(05)70283-0.
Hanley DF, Lane K, McBee N, Ziai W, Tuhrim S, Lees KR, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet. 2017;389(10069):603–11. https://doi.org/10.1016/S0140-6736(16)32410-2.
•• van Solinge TS, Muskens IS, Kavouridis VK, Gormley WB, Mekary RA, Broekman MLD, et al. Fibrinolytics and intraventricular hemorrhage: a systematic review and meta-analysis. Neurocrit Care. 2020;32(1):262–71. https://doi.org/10.1007/s12028-019-00786-5. This systematic review of intraventricular fibrinolytic use for intraventricular hemorrhage reviews many studies with over 1000 patients finding lower mortality and lower EVD obstruction with shorter time to clearance with use of intrathecal fibrinolytic, however no difference in good functional outcome.
Schwab S, Aschoff A, Spranger M, Albert F, Hacke W. The value of intracranial pressure monitoring in acute hemispheric stroke. Neurology. 1996;47(2):393–8. https://doi.org/10.1212/wnl.47.2.393.
Poca MA, Benejam B, Sahuquillo J, Riveiro M, Frascheri L, Merino MA, et al. Monitoring intracranial pressure in patients with malignant middle cerebral artery infarction: is it useful? J Neurosurg. 2010;112(3):648–57. https://doi.org/10.3171/2009.7.JNS081677.
Braksick SA, Himes BT, Snyder K, Van Gompel JJ, Fugate JE, Rabinstein AA. Ventriculostomy and risk of upward herniation in patients with obstructive hydrocephalus from posterior fossa mass lesions. Neurocrit Care. 2018;28(3):338–43. https://doi.org/10.1007/s12028-017-0487-3.
Warner JJ, Harrington RA, Sacco RL, Elkind MSV. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. Stroke. 2019;50(12):3331–2. https://doi.org/10.1161/STROKEAHA.119.027708.
Abulhasan YB, Rachel SP, Chatillon-Angle MO, Alabdulraheem N, Schiller I, Dendukuri N, et al. Healthcare-associated infections in the neurological intensive care unit: results of a 6-year surveillance study at a major tertiary care center. Am J Infect Control. 2018;46(6):656–62. https://doi.org/10.1016/j.ajic.2017.12.001.
Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Scheld WM, et al. 2017 infectious diseases society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017;64(6):e34–65. https://doi.org/10.1093/cid/ciw861.
•• Chang H, Silva MA, Giner A, Ancheta S, Romano JG, Komotar R, et al. Effects of an external ventricular drain alert protocol on venticulostomy placement time in the emergency department. Neurosurg Focus. 2021;51(5):E4. https://doi.org/10.3171/2021.8.FOCUS21378. This study evaluates factors that result in delays in EVD placement in the ED. It then describes implementation of an automated EVD alert system that showed significant reduction in EVD placement time.
•• Dawod G, Henkel N, Karim N, Caras A, Qaqish H, Mugge L, et al. Does the setting of external ventricular drain placement affect morbidity? A systematic literature review comparing intensive care unit versus operating room procedures. World Neurosurg. 2020;140:131–41. https://doi.org/10.1016/j.wneu.2020.04.215. A systematic review of the literature studying the difference in placing EVDs in the ICU vs operating rooms with overall inconclusive results while comparing efficacy and morbidity between both locations.
Ehtisham A, Taylor S, Bayless L, Klein MW, Janzen JM. Placement of external ventricular drains and intracranial pressure monitors by neurointensivists. Neurocrit Care. 2009;10(2):241–7. https://doi.org/10.1007/s12028-008-9097-4.
•• Eisenring CV, Burn F, Baumann M, Stieglitz LH, Kockro RA, Beck J, et al. sEVD-smartphone-navigated placement of external ventricular drains. Acta Neurochir (Wien). 2020;162(3):513–21. https://doi.org/10.1007/s00701-019-04131-9. The purpose of this study is to provide data on possible increase in EVD placement safety by using a novel guide for EVD positioning using multimodal simulation on cadavers and 3D advanced technologies showing safer and effective EVD placement. Requiers further validation in clinical studies.
Umana GE, Scalia G, Yagmurlu K, Mineo R, Di Bella S, Giunta M, et al. Multimodal simulation of a novel device for a safe and effective external ventricular drain placement. Front Neurosci. 2021;15: 690705. https://doi.org/10.3389/fnins.2021.690705.
•• Ellens NR, Fischer DL, Meldau JE, Schroeder BA, Patra SE. External ventricular drain placement accuracy and safety when done by midlevel practitioners. Neurosurgery. 2019;84(1):235–41. https://doi.org/10.1093/neuros/nyy090. This is a retrospective study of EVD placement accuracy and complications in a level 1 trauma center by midlevel practioners compared to neurosurgeons. It showed no significant difference in accuracy of placement or complication rate which may allow earlier management of high ICP when prompt access to neurosurgeons is limited.
Poon WS, Ng S, Wai S. CSF antibiotic prophylaxis for neurosurgical patients with ventriculostomy: a randomised study. Acta Neurochir Suppl. 1998;71:146–8. https://doi.org/10.1007/978-3-7091-6475-4_43.
Murphy RK, Liu B, Srinath A, Reynolds MR, Liu J, Craighead MC, et al. No additional protection against ventriculitis with prolonged systemic antibiotic prophylaxis for patients treated with antibiotic-coated external ventricular drains. J Neurosurg. 2015;122(5):1120–6. https://doi.org/10.3171/2014.9.JNS132882.
•• Lord AS, Nicholson J, Lewis A. Infection prevention in the neurointensive care unit: a systematic review. Neurocrit Care. 2019;31(1):196–210. https://doi.org/10.1007/s12028-018-0568-y. This systematic review looked into studies in patients admitted to neurointensive care units with interventions designed to prevent ICU-acquired infections. It highlighted the need for further collaborative multi-disciplinary approaches to reduce infections including VRI, SSI, VAP, CAUTI, and CLABSI.
Fried HI, Nathan BR, Rowe AS, Zabramski JM, Andaluz N, Bhimraj A, et al. The insertion and management of external ventricular drains: an evidence-based consensus statement : a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care. 2016;24(1):61–81. https://doi.org/10.1007/s12028-015-0224-8.
•• Garg K, Verma SK, Singh PK, Singh M, Chandra PS, Kale SS. Effect of external ventricular drain tunnel length on cerebrospinal fluid infection rates-a Bayesian network meta-analysis. World Neurosurg. 2021. https://doi.org/10.1016/j.wneu.2021.11.009. A meta-analysis that looked into rates of EVD-associated CSF infection with various EVD tunneling lengths showing that a tunnel length of 5–10 cm was associated with lowest risk of infections.
Cui Z, Wang B, Zhong Z, Sun Y, Sun Q, Yang G, et al. Impact of antibiotic- and silver-impregnated external ventricular drains on the risk of infections: a systematic review and meta-analysis. Am J Infect Control. 2015;43(7):e23-32. https://doi.org/10.1016/j.ajic.2015.03.015.
Harrop JS, Sharan AD, Ratliff J, Prasad S, Jabbour P, Evans JJ, et al. Impact of a standardized protocol and antibiotic-impregnated catheters on ventriculostomy infection rates in cerebrovascular patients. Neurosurgery. 2010;67(1):187–91; discussion 91. https://doi.org/10.1227/01.NEU.0000370247.11479.B6.
Sonabend AM, Korenfeld Y, Crisman C, Badjatia N, Mayer SA, Connolly ES Jr. Prevention of ventriculostomy-related infections with prophylactic antibiotics and antibiotic-coated external ventricular drains: a systematic review. Neurosurgery. 2011;68(4):996–1005. https://doi.org/10.1227/NEU.0b013e3182096d84.
Zabramski JM, Whiting D, Darouiche RO, Horner TG, Olson J, Robertson C, et al. Efficacy of antimicrobial-impregnated external ventricular drain catheters: a prospective, randomized, controlled trial. J Neurosurg. 2003;98(4):725–30. https://doi.org/10.3171/jns.2003.98.4.0725.
Pople I, Poon W, Assaker R, Mathieu D, Iantosca M, Wang E, et al. Comparison of infection rate with the use of antibiotic-impregnated vs standard extraventricular drainage devices: a prospective, randomized controlled trial. Neurosurgery. 2012;71(1):6–13. https://doi.org/10.1227/NEU.0b013e3182544e31.
•• Waqar M, Chari A, Islim AI, Davies BM, Fountain DM, Larkin S, et al. Chlorhexidine dressings could reduce external ventricular drain infections: results from a systematic review and meta-analysis. J Hosp Infect. 2021;117:37–43. https://doi.org/10.1016/j.jhin.2021.06.006. The aim of this systematic review and meta-analysis is to evaluate efficacy of chlorhexidine dressings in reducing EVD-associated CSF infection. It found a significantly lower incidence of infection in the chlorhexidine dressing group.
Bisnaire D, Robinson L. Accuracy of levelling intraventricular collection drainage systems. J Neurosci Nurs. 1997;29(4):261–8. https://doi.org/10.1097/01376517-199708000-00008.
•• Palasz J, D'Antona L, Farrell S, Elborady MA, Watkins LD, Toma AK. External ventricular drain management in subarachnoid haemorrhage: a systematic review and meta-analysis. Neurosurg Rev. 2022;45(1):365–73. https://doi.org/10.1007/s10143-021-01627-w. This systematic review and meta-analysis of EVD management in SAH found a lower incidence of EVD-related infections and blockages with intermittent CSF drainage versus continuous, with shorter hospital length of stay with rapid weaning.
Chung DY, Mayer SA, Rordorf GA. External ventricular drains after subarachnoid hemorrhage: is less more? Neurocrit Care. 2018;28(2):157–61. https://doi.org/10.1007/s12028-017-0443-2.
•• Rao SS, Chung DY, Wolcott Z, Sheriff F, Khawaja AM, Lee H, et al. Intermittent CSF drainage and rapid EVD weaning approach after subarachnoid hemorrhage: association with fewer VP shunts and shorter length of stay. J Neurosurg. 2019;132(5):1583–8. https://doi.org/10.3171/2019.1.JNS182702. This was a retrospective study of 200 aneurysmal subarachnoid hemorrhages patients requiring EVDs at a single institution comparing intermittent drainage and rapid EVD weaning approach versus continuous drainage and gradual wean. They found a lower incidence of VP shunt placements with intermittent CSF drainage and rapid wean with fewer complications and shorter length of stay compared to continuous CSF drainage and gradual wean.
Olson DM, Zomorodi M, Britz GW, Zomorodi AR, Amato A, Graffagnino C. Continuous cerebral spinal fluid drainage associated with complications in patients admitted with subarachnoid hemorrhage. J Neurosurg. 2013;119(4):974–80. https://doi.org/10.3171/2013.6.JNS122403.
Klopfenstein JD, Kim LJ, Feiz-Erfan I, Hott JS, Goslar P, Zabramski JM, et al. Comparison of rapid and gradual weaning from external ventricular drainage in patients with aneurysmal subarachnoid hemorrhage: a prospective randomized trial. J Neurosurg. 2004;100(2):225–9. https://doi.org/10.3171/jns.2004.100.2.0225.
Nwachuku EL, Puccio AM, Fetzick A, Scruggs B, Chang YF, Shutter LA, et al. Intermittent versus continuous cerebrospinal fluid drainage management in adult severe traumatic brain injury: assessment of intracranial pressure burden. Neurocrit Care. 2014;20(1):49–53. https://doi.org/10.1007/s12028-013-9885-3.
Williamson RA, Phillips-Bute BG, McDonagh DL, Gray MC, Zomorodi AR, Olson DM, et al. Predictors of extraventricular drain-associated bacterial ventriculitis. J Crit Care. 2014;29(1):77–82. https://doi.org/10.1016/j.jcrc.2013.08.012.
Williams TA, Leslie GD, Dobb GJ, Roberts B, van Heerden PV. Decrease in proven ventriculitis by reducing the frequency of cerebrospinal fluid sampling from extraventricular drains. J Neurosurg. 2011;115(5):1040–6. https://doi.org/10.3171/2011.6.JNS11167.
Park P, Garton HJ, Kocan MJ, Thompson BG. Risk of infection with prolonged ventricular catheterization. Neurosurgery. 2004;55(3):594–9; discussion 9–601. https://doi.org/10.1227/01.neu.0000134289.04500.ee.
Bota DP, Lefranc F, Vilallobos HR, Brimioulle S, Vincent JL. Ventriculostomy-related infections in critically ill patients: a 6-year experience. J Neurosurg. 2005;103(3):468–72. https://doi.org/10.3171/jns.2005.103.3.0468.
Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES Jr. Ventriculostomy-related infections: a critical review of the literature. Neurosurgery. 2008;62(Suppl 2):688–700. https://doi.org/10.1227/01.neu.0000316273.35833.7c.
•• Lewin JJ 3rd, Cook AM, Gonzales C, Merola D, Neyens R, Peppard WJ, et al. Current practices of intraventricular antibiotic therapy in the treatment of meningitis and ventriculitis: results from a multicenter retrospective cohort study. Neurocrit Care. 2019;30(3):609–16. https://doi.org/10.1007/s12028-018-0647-0. Lewin et al. conducted a multicenter retrospective cohort study to study outcomes of patients receiving intraventricular antibiotic treatment for CNS infection. They reported a higher CSF sterilization rate with reduction in overall treatment duration with intraventricular antibiotic use.
•• Hussein K, Rabino G, Feder O, Eghbaryeh H, Zayyad H, Sviri G, et al. Risk factors for meningitis in neurosurgical patients with cerebrospinal fluid drains: prospective observational cohort study. Acta Neurochir (Wien). 2019;161(3):517–24. https://doi.org/10.1007/s00701-019-03801-y. This is a single center prospective observational study that examined risk factors for infections related to EVD insertions and assessed the effect of infection control interventions. They concluded that strict adherence to infection control measures, minimizing drain duration, and avoiding unnecessary EVD manipulation are necessary to prevent drain-related infections.
Abulhasan YB, Alabdulraheem N, Schiller I, Rachel SP, Dendukuri N, Angle MR, et al. Health care-associated infections after subarachnoid hemorrhage. World Neurosurg. 2018;115:e393–403. https://doi.org/10.1016/j.wneu.2018.04.061.
Mayhall CG, Archer NH, Lamb VA, Spadora AC, Baggett JW, Ward JD, et al. Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med. 1984;310(9):553–9. https://doi.org/10.1056/NEJM198403013100903.
Arabi Y, Memish ZA, Balkhy HH, Francis C, Ferayan A, Al Shimemeri A, et al. Ventriculostomy-associated infections: incidence and risk factors. Am J Infect Control. 2005;33(3):137–43. https://doi.org/10.1016/j.ajic.2004.11.008.
Holloway KL, Barnes T, Choi S, Bullock R, Marshall LF, Eisenberg HM, et al. Ventriculostomy infections: the effect of monitoring duration and catheter exchange in 584 patients. J Neurosurg. 1996;85(3):419–24. https://doi.org/10.3171/jns.1996.85.3.0419.
Lo CH, Spelman D, Bailey M, Cooper DJ, Rosenfeld JV, Brecknell JE. External ventricular drain infections are independent of drain duration: an argument against elective revision. J Neurosurg. 2007;106(3):378–83. https://doi.org/10.3171/jns.2007.106.3.378.
Wilkie MD, Hanson MF, Statham PF, Brennan PM. Infections of cerebrospinal fluid diversion devices in adults: the role of intraventricular antimicrobial therapy. J Infect. 2013;66(3):239–46. https://doi.org/10.1016/j.jinf.2012.11.006.
Remes F, Tomas R, Jindrak V, Vanis V, Setlik M. Intraventricular and lumbar intrathecal administration of antibiotics in postneurosurgical patients with meningitis and/or ventriculitis in a serious clinical state. J Neurosurg. 2013;119(6):1596–602. https://doi.org/10.3171/2013.6.JNS122126.
•• Abulhasan YB, Ortiz Jimenez J, Teitelbaum J, Simoneau G, Angle MR. Milrinone for refractory cerebral vasospasm with delayed cerebral ischemia. J Neurosurg. 2020;134(3):971–82. https://doi.org/10.3171/2020.1.JNS193107. This was a single center retrospective study looking at predictors of refractory vasposasm/DCI despite therapy with IV milrione and the effect of rescue therapy with intraarterial milrinone. They found the aggressive use of milrinone to be safe and and effective in vasospasm treatment.They also reported a rate of 56% for EVD tract hemorrhage.
Dey M, Stadnik A, Riad F, Zhang L, McBee N, Kase C, et al. Bleeding and infection with external ventricular drainage: a systematic review in comparison with adjudicated adverse events in the ongoing Clot Lysis Evaluating Accelerated Resolution of Intraventricular Hemorrhage Phase III (CLEAR-III IHV) trial. Neurosurgery. 2015;76(3):291–300; discussion 1. https://doi.org/10.1227/NEU.0000000000000624.
Binz DD, Toussaint LG 3rd, Friedman JA. Hemorrhagic complications of ventriculostomy placement: a meta-analysis. Neurocrit Care. 2009;10(2):253–6. https://doi.org/10.1007/s12028-009-9193-0.
Bauer DF, Razdan SN, Bartolucci AA, Markert JM. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011;69(2):255–60. https://doi.org/10.1227/NEU.0b013e31821a45ba.
Rowe AS, Rinehart DR, Lezatte S, Langdon JR. Intracerebral hemorrhage after external ventricular drain placement: an evaluation of risk factors for post-procedural hemorrhagic complications. BMC Neurol. 2018;18(1):22. https://doi.org/10.1186/s12883-018-1030-7.
Ross IB, Dhillon GS. Ventriculostomy-related cerebral hemorrhages after endovascular aneurysm treatment. AJNR Am J Neuroradiol. 2003;24(8):1528–31.
Davis JW, Davis IC, Bennink LD, Hysell SE, Curtis BV, Kaups KL, et al. Placement of intracranial pressure monitors: are “normal” coagulation parameters necessary? J Trauma. 2004;57(6):1173–7. https://doi.org/10.1097/01.ta.0000151257.79108.fb.
Bauer DF, McGwin G Jr, Melton SM, George RL, Markert JM. The relationship between INR and development of hemorrhage with placement of ventriculostomy. J Trauma. 2011;70(5):1112–7. https://doi.org/10.1097/TA.0b013e3181e7c2ae.
Khan SH, Kureshi IU, Mulgrew T, Ho SY, Onyiuke HC. Comparison of percutaneous ventriculostomies and intraparenchymal monitor: a retrospective evaluation of 156 patients. Acta Neurochir Suppl. 1998;71:50–2. https://doi.org/10.1007/978-3-7091-6475-4_16.
Paramore CG, Turner DA. Relative risks of ventriculostomy infection and morbidity. Acta Neurochir (Wien). 1994;127(1–2):79–84. https://doi.org/10.1007/BF01808552.
•• Aljoghaiman M, Bergen B, Takroni R, Wang B, Eangles P, Farrokhyar F, et al. Image-guided versus freehand ventricular drain insertion: systematic review and meta-analysis. World Neurosurg. 2022. https://doi.org/10.1016/j.wneu.2022.01.036. This systematic review and meta-analysis of studies looking at image-guided versus free hand ventricular drain insertion techniques found higher accuracy in EVD placement under image guidance with reduction in drain failure. However, image guidance did not decrease number of drain insertion attempts.
Eftekhar B. App-assisted external ventricular drain insertion. J Neurosurg. 2016;125(3):754–8. https://doi.org/10.3171/2015.6.JNS1588.
Li Y, Chen X, Wang N, Zhang W, Li D, Zhang L, et al. A wearable mixed-reality holographic computer for guiding external ventricular drain insertion at the bedside. J Neurosurg. 2018:1–8. https://doi.org/10.3171/2018.4.JNS18124.
•• Ofoma H, Cheaney B, 2nd, Brown NJ, Lien BV, Himstead AS, Choi EH, et al. Updates on techniques and technology to optimize external ventricular drain placement: a review of the literature. Clin Neurol Neurosurg. 2022;213:107126. https://doi.org/10.1016/j.clineuro.2022.107126. Ofoma et al. reviewed the literature on techniques and technology to optimize EVD placement to improve accuracy, precision, and efficacy of EVD placement.
Kawoos U, McCarron RM, Auker CR, Chavko M. Advances in intracranial pressure monitoring and its significance in managing traumatic brain injury. Int J Mol Sci. 2015;16(12):28979–97. https://doi.org/10.3390/ijms161226146.
Czosnyka M, Hutchinson PJ, Balestreri M, Hiler M, Smielewski P, Pickard JD. Monitoring and interpretation of intracranial pressure after head injury. Acta Neurochir Suppl. 2006;96:114–8. https://doi.org/10.1007/3-211-30714-1_26.
•• Chung DY, Thompson BB, Kumar MA, Mahta A, Rao SS, Lai JH, et al. Association of external ventricular drain wean strategy with shunt placement and length of stay in subarachnoid hemorrhage: a prospective multicenter study. Neurocrit Care. 2021. https://doi.org/10.1007/s12028-021-01343-9. Chung et al. conducted a prospective multicenter observational study in 6 neurocritical units in the USA to determine effect of EVD discontinuation strategy on shunt placement. They found that a rapid EVD wean was associated with reduced rates of VPS placement and shorter ICU length of stay.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43(6):1711–37. https://doi.org/10.1161/STR.0b013e3182587839.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Haamid H. Siddique declares no conflict of interest. Hussam Elkambergy declares no conflict of interest. Ahmad Bayrlee declares no conflict of interest. Yasser B. Abulhasan declares no conflict of interest. Florian Roser declares no conflict of interest. Jamil Dibu declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Critical Care Neurology
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siddique, H.H., Elkambergy, H., Bayrlee, A. et al. Management of External Ventricular Drains and Related Complications: a Narrative Review. Curr Treat Options Neurol 24, 347–363 (2022). https://doi.org/10.1007/s11940-022-00725-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-022-00725-4