Abstract
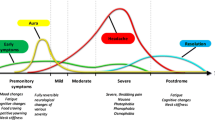
Migraine is a chronic paroxysmal neurological disorder characterized by multiphase attacks of head pain and a myriad of neurological symptoms. Chronic migraine causes a great personal and societal burden. Many patients are poorly responsive to, or non-compliant with, conventional migraine preventive therapies. For this reason, physicians are constantly looking for effective migraine prevention strategies. The recent introduction of an innovative pharmacological class useful for migraine prevention, namely monoclonal antibodies towards calcitonin gene-related peptide or its receptors, opens a new, immense therapeutic scenario. In this commentary, the development and efficacy of this novel class of preventive anti-migraine therapy have been discussed and compared with the conventional therapies of migraine prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Migraine is one of the most prevalent neurologic disorders worldwide and is one of the leading causes of years lived with disability [1]. Considering the substantial economic burden migraine poses, physicians are constantly looking for new migraine therapies. Depending on whether these medications are used as needed or daily, they may be categorized into abortive (acute) and preventive (prophylactic) medications, respectively. Use of preventive anti-migraine therapies (PAMT) is primarily reserved for more frequent headaches to reduce disability and prevent chronicity. However, historically prevention of migraine has been challenging. This may be attributed to the fact that most available migraine preventive therapies, such as beta-blockers, anti-epileptics, and tricyclic anti-depressants, were originally designed for other clinical indications, may have variable drug-drug interactions, and may cause adverse effects with prolonged use. Also, most of these drugs require daily dosing, resulting in lack of adherence and failure of therapy. In this commentary, we will describe some of the challenges faced in the development of migraine-specific treatments and highlight some of the emerging PAMTs.
For several years, migraine was primarily considered a vascular disorder and the associated pain was thought to be caused by dilation of cerebral and meningeal arteries. However, we now know that the pathophysiology of migraine is much more complex. Not understanding the exact mechanism behind migraine development has made it difficult to create migraine-specific preventive drug therapies. In recent years, the role of CGRP in the pathogenesis of migraine via the trigeminovascular pathway has been well established [2, 3]. Based on these findings, CGRP was made the focus of research for the development of new migraine preventive therapies.
Characterization of the CGRP receptor led to the development of small molecules that could potentially block the receptor-“CGRP receptor antagonists” (Gepants). Olcegepant (BIBN4096BS) was the first gepant to be tested in humans. It demonstrated positive results in clinical trials for the acute treatment of migraine. However, due to its large molecular weight and low bioavailability, it could only be administered intravenously. This made the drug non-practical and commercially not viable. Following the positive results that were seen with this drug, seven more gepants were developed for migraine treatment. Of these, BI 44370 TA, telcagepant, and MK-3207 were discontinued secondary to concerns about liver toxicity. Most of them were tested for the acute treatment of migraine; however, two gepants are in phase II trials for proof of concept in migraine prophylaxis. Both atogepant and rimegepant will be tested on the basis of efficacy, safety, and tolerability, and appropriate dose will be evaluated in these studies.
Based on the pharmacologic studies of the gepants, it was suggested that gepants might not have a primary central action. Considering this finding, peripherally acting anti-CGRP therapies were developed. Monoclonal antibodies (mAbs), large molecules that do not cross the blood brain barrier, were developed as a migraine-specific therapy. Monoclonal antibodies are eliminated via the reticuloendothelial system, and were not found to be hepatotoxic. Moreover, the long half-lives of the mAbs allow for infrequent dosing, making it much easier for people with migraine to comply with the treatment regimen. Currently, four mABs have been studied for the prevention of migraine: erenumab, fremanezumab, galcanezumab, and eptinezumab. Of these mAbs, erenumab targets the canonical CGRP receptor, whereas all the others target CGRP peptide (the ligand) itself. All of these drugs have shown success in phase II and phase III clinical trials. All have been genetically engineered to decrease affinity for the Fcγreceptors (FcγRs) which reduces immune activity by preventing the antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) pathways.
Erenumab was the first drug of its class to receive FDA approval in May of 2018. Erenumab is a fully human IgG2 mAb that targets the CGRP receptor. It has peer-reviewed published studies (two phase III trials for episodic migraine [4, 5] and one phase II/III trial for chronic migraine [6]) demonstrating safety and effectiveness. The drug is currently co-marketed by Novartis and Amgen under the trade name “Aimovig.” It is available in two doses (70 mg and 140 mg) subcutaneously. Even though prescribing information recommends starting at the lower dose, studies have demonstrated that 140 mg dose has superior efficacy with a similar side effect profile. This has led some clinicians to recommend starting the patient on a higher dose of erenumab and not suffer a therapeutic penalty [7].
Fremanezumab is an IgG2 humanized mAb that targets CGRP and is administered subcutaneously. Two pivotal phase III trials were conducted (one for episodic migraine [8] and one for chronic migraine [9]) demonstrating efficacy and safety as a preventive anti-migraine therapy. It received FDA approval in September of 2018, and is currently marketed under the trade name “Ajovy” by Teva Pharmaceuticals. The current dosing regimen for fremanezumab is 225 mg monthly or 675 mg quarterly, and is available as a self-administered, subcutaneous injection.
Galcanezumab is another humanized mAb targeting CGRP. It has demonstrated success in the prevention of episodic migraine in two phase III trials (EVOLVE 1 [10] & EVOLVE 2 [11]). It has also successfully completed one phase III trial showing safety and efficacy in chronic migraine prevention (the REGAIN study) [12]. It received FDA approval in September of 2018 and is currently marketed by Eli Lilly and Company under the trade name “Emgality.” It is available in once monthly, self-administered, subcutaneous 120 mg or 240 mg doses.
Eptinezumab is the last drug of its class and is the only anti-CGRP antibody without the N-linked carbohydrate, to reduce binding to the Fc receptor. IV administration ensures reliable therapeutic bioavailability and consistency [13]. Eptinezumab was effective in migraine preventive therapy in phase III trials for both episodic [14] and chronic migraine [15]. At the time of this writing, it is awaiting FDA approval, and will be the only mAb to be available as an intravenous infusion. Two doses under consideration are 100 mg and 300 mg, administered quarterly.
Initiation of a PAMT should be considered in patients with recurring migraine attacks, four or more migraine attacks or eight or more headache days per month, presence of certain migraine conditions including hemiplegic migraine, migraine with brainstem aura, frequent and prolonged aura symptoms, and with patient’s preference to have as few attacks as possible. Previously among the PAMTs- anti-epileptics (sodium valproate, topiramate, divalproex sodium) and beta-blockers (propranolol, metoprolol, timolol) were the only drugs with level 1 evidence for migraine prophylaxis [16]. An efficacy-cost comparison has been shown between the major PAMTs commonly used in clinical practice and the FDA approved CGRP receptor mAbs (Table 1). CGRP mAbs may be three to ten times costlier than conventional PAMTs. Even though CGRP mAbs are not significantly superior in terms of efficacy, they have a side effect profile similar to placebo with minimal/none drug-drug interactions and CGRP mAbs work when prior preventive medications fail. Clinicians must individualize treatment when deciding which PAMT to consider for initiation of therapy. However, insurance companies typically require failure of prior PAMTs before they allow CGRP mAbs for migraine prophylaxis. Discontinuation of migraine prophylaxis may be considered if the patient develops intolerable side effects to any PAMT or if the drug fails to demonstrate even partial efficacy after 2 months of treatment. Migraine prophylaxis is often recommended for 3–6 months and may be tapered when headaches are well controlled for at least 6 months.
With no head-to-head comparative studies between the mAbs, clinicians may be faced with a dilemma on what drug to use as an initial therapy. Fremanezumab and eptinezumab may be considered in patients who prefer quarterly treatments. Eptinezumab being administered intravenously has a faster onset of action and can decrease the likelihood of developing a migraine attack within 1 day of infusion. This may be beneficial in patients with severe debilitating chronic migraine. With their specificity and variety of therapeutic targets (episodic migraine, chronic migraine, and medication overuse headaches), the mAbs expand our therapy.
Gepants are still in the final regulatory stages before pharmaceutical companies seek FDA approval for migraine prevention. While safety had been a concern with previous gepants (especially liver toxicity), none of the new gepants show signs of liver toxicity. When approved, they would be the first migraine-specific oral preventive medications. Some patients do not want injectable medications, and may prefer gepants over mAbs. Monoclonal antibodies have long half-lives and their effects on pregnancy are still not determined. Therefore, it may be prudent to use gepants (once approved) as a migraine preventive therapy over mAbs for females in their reproductive age group and not using contraceptives. Even though the initial studies with CGRP inhibitors have shown good tolerability, the long-term side effects of these therapies are still not clear and are hard to predict. There is a need for retrospective analysis with a larger cohort of patients in the future to truly assess their tolerability. This is an exciting era in the field of headache medicine and we have seen some significant and promising improvements made in the therapies available for migraine prevention. The biggest challenge for patients now would be the cost of and access to these medications.
References and Recommended Reading
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of Disease study 2016. Lancet. 2017;390(10100):1211–59.
Durham PL. Calcitonin gene-related peptide (CGRP) and migraine. Headache. 2006;46(Suppl 1):S3–8.
Edvinsson L. The trigeminovascular pathway: role of CGRP and CGRP receptors in migraine. Headache. 2017;57(Suppl 2):47–55.
Goadsby PJ, Reuter U, Hallstrom Y, Broessner G, Bonner JH, Zhang F, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377(22):2123–32.
Dodick DW, Ashina M, Brandes JL, Kudrow D, Lanteri-Minet M, Osipova V, et al. ARISE: a phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia. 2018;38(6):1026–37 333102418759786.
Tepper S, Ashina M, Reuter U, Brandes JL, Dolezil D, Silberstein S, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16(6):425–34.
Jain S, Yuan H, Spare N, Silberstein SD. Erenumab in the treatment of migraine. Pain Manag. 2018;8(6):415–26.
Dodick DW, Silberstein SD, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, et al. Effect of fremanezumab compared with placebo for prevention of episodic migraine: a randomized clinical trial. JAMA. 2018;319(19):1999–2008.
Silberstein SD, Dodick DW, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med. 2017;377(22):2113–22.
Stauffer VL, Dodick DW, Zhang Q, Carter JN, Ailani J, Conley RR. Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75(9):1080–8.
Skljarevski V, Matharu M, Millen BA, Ossipov MH, Kim BK, Yang JY. Efficacy and safety of galcanezumab for the prevention of episodic migraine: results of the EVOLVE-2 phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38(8):1442–54.
Detke HC, Goadsby PJ, Wang S, Friedman DI, Selzler KJ, Aurora SK. Galcanezumab in chronic migraine: the randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018;91(24):e2211–e21.
Ju MS, Jung ST. Aglycosylated full-length IgG antibodies: steps toward next-generation immunotherapeutics. Curr Opin Biotechnol. 2014;30:128–39.
Silberstein S, McAllister P, Berman G, et al. Eptinezumab reduced migraine frequency, duration, and pain intensity through week 24: results from the phase 3 PROMISE-1 trial. Neurology. 2018;90(15):P4.091.
Lipton R, Saper J, Ashina M. A phase 3, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of eptinezumab for the preventive treatment of chronic migraine: results of the PROMISE-2 (prevention of migraine via intravenous eptinezumab safety and efficacy–2) trial InPlenary Presentation. Am Acad Neurol Conf 2018. 2018.
Estemalik E, Tepper S. Preventive treatment in migraine and the new US guidelines. Neuropsychiatr Dis Treat. 2013;9:709–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Stephen D. Silberstein reports personal fees from Alder Biopharmaceuticals, Allergan, Inc., Amgen, Avanir Pharmaceuticals, Inc., Curelator, Inc., Dr. Reddy’s Laboratories, eNeura Inc., electroCore Medical, LLC, Lilly USA, LLC, Supernus Pharmaceuticals, Inc., Teva Pharmaceuticals, Theranica, Trigemina, Inc., Medscape, LLC, Abide Therapeutics, Biohaven Pharmaceuticals, Cefaly, Egalet, and GlaxoSmithKline, outside the submitted work. Sameer Jain reports no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Headache
Rights and permissions
About this article
Cite this article
Jain, S., Silberstein, S.D. Invited Commentary on Preventive Anti-Migraine Therapy (PAMT). Curr Treat Options Neurol 21, 14 (2019). https://doi.org/10.1007/s11940-019-0555-4
Published:
DOI: https://doi.org/10.1007/s11940-019-0555-4