Abstract
Purpose of the review
Psychosis is broadly defined as a disengagement from reality. It describes syndromes that impair both thought content and thought process. Psychosis negatively impacts an individual’s quality of life, in addition to the families caring for them. Psychosis with different types of hallucinations and delusions occurs in the context of delirium. Neuropsychiatric symptoms (NPS) are almost universal in the course of common neurodegenerative disorders (NDD) like Alzheimer’s disease (AD) or Parkinson’s disease (PD).
In this paper, the authors took an effort to characterize AD and PD psychosis with a special focus on the most diagnostically reliable features. Effectiveness and limitations of pharmacological interventions are discussed.
Recent findings
Consensus diagnostic criteria have evolved for psychosis secondary to AD as well as psychosis in PD. Psychotropic medications can be effective in the treatment of NPS in NDD; however, clinicians must be mindful of the side effects. There is a consensus on benefit of initiating any acetylcholinesterase inhibitor (ACHI: donepezil, rivastigmine, and galantamine) as a first line of treatment for psychosis in AD, as it may reduce and/or avoid the need for the use antipsychotics. Pimavanserin, a selective-serotonin inverse agonist that preferentially targets 5-HT2A receptors, while avoiding activity at dopamine and other receptors commonly targeted by antipsychotics had recently been approved by FDA to treat hallucinations and delusions in PD. Quetiapine is widely prescribed for the treatment of psychosis in different NDD, but the data remains equivocal.
Summary
Psychosis with different types of hallucinations and delusions may occur in the context of delirium and is almost universal as a neuropsychiatric symptom in the course of PD and AD. Currently, pimavanserin remains the only pharmacologic agent approved for treatment of psychosis in PD. In cases of other NPS in other than Parkinson’s diseases, atypical antipsychotics are commonly used off-label. More research is greatly needed to advance this field and address NPS especially psychosis in geriatric population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extent of the problem and overall impact
Psychosis is broadly defined as a loss of contact with reality. It defines syndromes that impair both thought content and thought process which can result from any number of diseases and disorders. Disturbances in thought content include perceptions that are not based in reality, whereas disturbances in thought process reflect thoughts that are disorganized and illogical in form. Psychosis may present as acute or chronic, primary psychiatric, or secondary in the course of other medical conditions [1, 2]. Term psychosis envelopes two phenomena: delusions and hallucinations. Delusions are persistent beliefs that are not accepted in the context of a person’s cultural and religious background, whereas hallucinations are false sensory perceptions. A slightly broader definition of psychosis can include disorganized speech or behavior. Considering psychiatric illnesses, psychosis is most commonly associated with schizophrenia, but it can also co-occur with mood disorders such as severe forms of depression and mania and can occur transiently in personality disorders. It can also manifest itself secondary to medication and/or drug use. Symptoms of psychosis are typically episodic and these episodes are generally precipitated or exacerbated by psychosocial stressors [1, 2].
There are only a few studies and limited data available about the prevalence, risk factors, and course of psychosis in geriatric population even though it is a general consensus that episode of psychosis may occur late in life. Its prevalence, irrespective of underlying cause, is estimated at 10% or even higher among those residing in institutional settings [3,4,5]. Psychosis commonly accompanies delirium or exposure to substances in geriatric population. Therefore, clinicians may have more difficulties trying to determine the etiology of psychotic symptoms and should evaluate a patient thoroughly, ruling out other medical conditions, reviewing patient’s medications [2, 6, 7].
Dementia remains, however, the most common underlying causes of late onset psychosis. Javadpour [3] analyzed a group of 201 elderly patients with first episode of psychosis and his study gives an interesting overview of its character and causes. Most of the patient (almost 90%) presented with delusions. Persecutory delusions seemed to dominate (64.7%) followed by delusions of reference (15.9%); incarnation syndrome (14.9%); misidentification syndrome (13.9%); and partition delusion (11.9%). Visual hallucinations were the most common type of hallucination (56.7%) followed by auditory hallucinations (37.8%) and tactile hallucinations (5%). In almost 70% combination of delusion and hallucination was reported. Dementia was the most common underlying cause of psychosis in the examined group and was an underlying cause of 34.8% of cases. It was followed by psychosis due to mood disorders (30.3%), primary psychosis (19.9%), delirium (8%), psychosis due to general medical conditions (5%), and finally psychosis due to drugs and substances (1%) [3].
Psychosis as neuropsychiatric symptoms (NPS) of neurodegenerative disorders seems to be even more prevalent than in general geriatric population. In this, especially, vulnerable group of patients its occurrence ranged from 3 to 54% for delusions and 1 to 39% for hallucinations [4, 5, 7].
Rationale for interventions and treatment
Only one agent—pimavanserin—is currently approved by the US Food and Drug Administration (FDA) for the treatment of a psychosis secondary to one of the NDD. This pharmacologic agent is approved for the treatment of hallucinations and delusions occurring in PD [8••]. Since there is either little or no data concerning the use of psychotropics in patients with NDD, clinicians are utilizing medication off-label [6, 9,10,11].
Very few clinical studies look specifically at psychosis in the elderly and cognitive impaired populations; thus, conclusions are extrapolated from clinical trials of psychotropic agents used in the treatment of idiopathic psychiatric disorders. Antipsychotics are used for the treatment of psychosis (hallucinations and delusions) as well as agitation in NDD; this approach is based on the approval of antipsychotics for schizophrenia or bipolar affective disorder [6, 9, 10]. This extrapolation is based on the phenomenological similarities of the neuropsychiatric syndromes occurring in NDD and non-NDD and the absence of alternatives. The challenge remains that patients with NDD are typically excluded from antipsychotic drug trials, as well as other groups of psychotropics (antidepressants, anxiolytics, stimulants, or hypnotics). The extension of these therapies from non-NDD to NDD patients is based on many untested assumptions that may result in treating patients with agents that are ineffective or have safety and tolerability issues. Most patients with NDD are elderly, and this may affect the pharmacokinetics and the pharmacodynamics of an agent [2, 6, 9,10,11, and]. The potential benefit of all antipsychotics must thus be weighed against the significant risks, such as cerebrovascular accidents or worse, mortality [11].
There are, however, studies suggesting potential benefit of the treatment with atypical antipsychotics. Decreased caregiver burden was linked to its use in cases of NDD psychosis [6, 9, 11]. It has also been shown as well that antipsychotics does not universally increase the risk of premature death or increased institutionalization as long as careful control for cardiovascular risk factors is implemented [12].
Psychosis of Alzheimer’s disease
Extent of the problem, pathogenesis, and overall impact
Psychosis may present in the prodromal phase of AD and increase in frequency through the course of the illness [4]. Estimates of the incidence of psychosis in AD range widely from 10 to 75% [13]. More severe cognitive impairment and faster rate of cognitive decline are associated with and predictive of hallucinations and delusions in patients with AD [14]. The presence of parkinsonism was linked to imminent psychotic symptoms in AD. Some studies found a significant association between psychosis and age, age at onset of AD, and illness duration [4,5,6, 10, 13].
As a result of more extensive meta-analysis Ropacki and Jeste [4] estimated that psychosis occurs in 41% of patients with Alzheimer’s disease with delusions in 36% and hallucinations in 18% of the patients. The incidence of psychosis increased progressively over the first 3 years of observation, after which the incidence seemed to plateau. Psychotic symptoms tended to last for several months but became less prominent after 1 year. African American ethnicity and severe cognitive impairment were associated with a higher rate of psychosis. Gender, education, and family history of dementia or psychiatric illness showed weak or inconsistent relationships with AD psychosis [4]. Interestingly, the presence of psychosis was, however, clearly associated with more rapid cognitive decline [4, 14].
Specific diagnostic consensus criteria have been developed for psychosis in AD as published by Jeste and Finkel [15]. This seminal paper and other studies report AD psychosis commonly taking a form of delusions followed by hallucinations and misidentifications [5, 10, 15]. Delusions tend to cluster with hallucinations, agitation/aggression, depressed mood, apathy, irritability, aberrant motor activity, sleep disturbances, and eating disorders [6, 10]. Delusions in the course of AD are typically characterized as paranoid, nonbizarre, and simple. Delusions tend to recur or persist for several years in AD patients but active and vivid perception and delusions have a tendency to diminish in intensity in the course of cognitive decline, shallow insight, and decreasing ability for verbal expression [15]. AD patients with delusions tend to be significantly older, with higher age at onset of cognitive impairment, more severe in stage of dementia, and with more depressive symptoms than AD patients without delusions. Delusional patients tend to show a higher grade of disability in basic and instrumental activities of daily living [16]. Hallucinations are predominantly visual. Auditory phenomena especially of a schizophrenic quality are rare in AD [15].
Regarding the neurobiological basis of psychosis associated with AD, it is believed to be the result of dysfunction of frontal lobe circuitry with contributions from neurofibrillary tangles in limbic structures, in addition to neurochemical abnormalities including cholinergic deficit as well as dopaminergic dysfunctions [6, 17, 18]. Neuropathologic studies provide evidence that presence of Lewy bodies contribute to the occurrence of visual hallucinations in NDD [19].
Rationale for interventions and treatment
Clinical approach to psychosis in AD is guided by general rules of geriatric medicine. Particularly, if the onset is acute, clinicians should consider a thorough work up in order to rule out secondary causes, such as delirium, infection, or toxic-metabolic etiologies. Clinicians should also consider concurrently reviewing the patient’s medication list and discontinue any non-essential medications that could contribute to psychosis. The list includes but is not limited to tricyclic antidepressants, anticholinergics, benzodiazepines, opioids, and steroids.
There is a consensus on benefit of initiating any acetylcholinesterase inhibitor (ACHI; donepezil, rivastigmine, and galantamine; see supplement) as a first line of treatment for psychosis in AD, as it may reduce and/or avoid the need for the use antipsychotics, given their problematic safety profile [6, 20,21,22,23].
Memantine (see supplement) appears to provide only modest benefit for the management of AD psychosis but has a favorable safety profile. In a pooled, retrospective analysis of data from three placebo-controlled trials in moderate to severe AD, memantine was linked to significant reduction in psychosis, agitation, and aggression [24].
AChEIs and memantine have been shown, however, to be insufficient remedy for severe psychotic symptoms [22]. Antipsychotics may need to be considered in those situations. Atypical antipsychotic in general appear to have some impact in reducing psychosis as well as agitation in AD with the best evidence base for risperidone [25]. Olanzapine (up to 10 mg daily) has shown benefit in managing delusions, hallucinations, as well as anxiety and agitation in AD patients [26]. Aripiprazole (5–10 mg/day) was efficacious and relatively safe for psychosis associated with AD, significantly improving psychotic symptoms and agitation as assessed by Neuropsychiatric Inventory (NPI), Brief Psychiatric Rating Scale (BPRS), and The Cohen-Mansfield Agitation Inventory (CMAI scores [27]. Risperidone (mean doses of 1.5 mg daily) treatment was proved efficacious for psychosis of AD in couple of studies [28]. Devanand et al. [25] documented that in AD patients with psychosis or agitation who had responded to risperidone therapy for 4–8 months, discontinuation of risperidone was associated with an increased risk of relapse [25]. Carefully monitored and relative brief courses of antipsychotics are recommended despite well-documented risk for symptoms re-occurrence [22, 25].
Risperidone, olanzapine, and aripiprazole may be effective for severe agitation, aggression, and psychosis associated with AD where there is risk of harm to the patient and/or others [6]. There is than some support for use of olanzapine [26, 29] or aripiprazole [27] for the management of psychosis as well agitation in AD.
Quetiapine (see supplement) is also commonly used in (off-label) for NPS in AD. It is believed to have a lower incidence of serious side effects such as extrapyramidal symptoms (EPS) and tardive dyskinesia (TD) when compared with other antipsychotics. Quetiapine can be used in a wide range of doses. Sedating properties are of some use in certain clinical situations in NDD, as it may calm the patient—promote sleep-wake cycle. Results may vary across studies but most show minimal only benefit for psychosis and agitation. Despite lack of data to support effectiveness of quetiapine in treating agitation or psychosis, this antipsychotic is not only prescribed for those symptoms but the treatment is commonly prolonged [30].
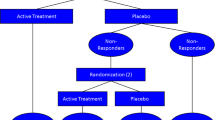
More extensive analysis of date The Clinical Antipsychotic Trials of Intervention Effectiveness-Alzheimer’s Disease (CATIE-AD) study included 421 outpatients with AD and NPS. Improvement was reported with olanzapine or risperidone on the NPI total score. Risperidone demonstrated greater improvement on the Clinical Global Impression of Changes (CGI-C), olanzapine and risperidone on the Brief Psychiatric Rating Scale (BPRS) hostile suspiciousness factor, and risperidone on the BPRS psychosis factor [6, 31]. Recent analysis of CATIE-AD data compared symptom trajectories between placebo and active drug responders to examine whether early placebo improvement would be associated with subsequent placebo response in the treatment of patients with behavioral and psychological symptoms of dementia. Interestingly, symptom trajectories of improvement of behavioral and psychological symptoms of AD follow the same pattern irrespective of the treatment [31].
Psychosis of Parkinson’s disease
Extent of the problem, pathogenesis, and impact
Psychosis is a debilitating symptom of PD; it is an independent risk factor for nursing home placement, increases caregiver distress, and patient mortality [32]. The lifetime prevalence of psychosis in PD had been estimated for 50%, with a range of 25–60% depending on diagnostic criteria used [33].
Consensus diagnostic criteria were established for psychosis in PD [34, 35]. National Institute of Neurological Disorders and Stroke and the National Institute of Mental Health (NINDS-NIMH) criteria require the presence of at least one of the following: hallucinations, delusions, illusions, or false sense of presence. Psychosis must occur within the setting of a clear sensorium and a chronic course (> 1 month), either recurrent or continuous. Other medical, neurologic, or psychiatric causes for the symptoms must be excluded [34]. Criteria for PD psychosis include then milder psychotic phenomena, such as visual illusions or sense of presence [35]. In one study of 116 PD patients, the cross-sectional prevalence of PD psychosis was 43% with the more traditional definition of psychosis, but with the more inclusive NINDS-NIMH criteria, increased to 60% [33].
Visual hallucinations are the most common psychotic manifestation in PD. These hallucinations may be nonthreatening, brief, and well formed; reports of small children or animals are common. Hallucinations occur more frequently during times of decreased environmental stimulation, such as in the evening, low ambient lighting, or decreased sound levels. A false sense of presence or passage, as well as visual illusions, are considered minor psychotic phenomena but can affect anywhere from 17 to 72% of PD patients [35, 36]. While auditory, olfactory, or tactile hallucinations are less common than their visual counterparts, they do occur; up to 20% of patients report auditory hallucinations. Nonvisual hallucinations or mixed hallucinations are more common in patients who develop psychotic symptoms at advanced ages [35, 37]. Minor hallucinations such as presence and passage hallucinations may precede the structured visual hallucinations [36].
Delusions occur in about 5% of PD patients. Dopaminergic medications, cognitive dysfunction, depression, sleep disturbances, and longer duration of PD are risk factors for the emergence of psychosis in PD [37].
The pathophysiology of psychosis in PD is most likely multifactorial, where disruption of serotonin, dopaminergic, and acetylcholine neurotransmissions may play a role [6, 38]. Overstimulation of dopaminergic receptors, particularly in the mesocorticolimbic region, may occur in the context of chronic dopaminergic therapy and enhanced sensitivity of native receptors [38]. Imbalances between dopamine and acetylcholine also play a role, with compensatory increase in cholinergic activity in response to dopamine deprivation. Additionally, the use of dopaminergic medications may result in decreasing intrinsic serotonin levels. This observation adds to already growing body of evidence suggesting serotoninergic circuitry involvement in the phenomenon of PD psychosis. In autopsies, study of the psychotic PD patients’ abnormalities was found in 5HT-2A receptors (increased serotonin binding) especially in inferior temporal cortex [39]. Neuropathological studies link the development of psychosis with progressive formation of Lewy bodies in cortex, amygdala, and hippocampus [40]. Altered cortical visual processing and rapid eye movement (REM) sleep anomalies had been proposed as contributors to the process [6, 32].
Rationale for interventions and treatment
As noted earlier, the only pharmacological agent with FDA approval for treatment of PD psychosis is pimavanserin, a selective-serotonin inverse agonist that preferentially targets 5-HT2A receptors, while avoiding activity at dopamine and other receptors commonly targeted by antipsychotics. The FDA’s decision to approve pimavanserin was based on the results of a trial in which adults with PDP were randomly assigned to take 40 mg of pimavanserin or placebo daily for 6 weeks. Patients taking pimavanserin experienced fewer and less severe hallucinations and delusions without motor side effects, which is commonly seen in other antipsychotics that function through dopamine blockade. The most common adverse effects reported by patients taking pimavanserin included peripheral edema, nausea, and confusion [6, 8].
Efforts to treat psychosis of PD with antipsychotics commonly used for primary psychotic disorders to date have been challenging and associated with significant deterioration of the motor symptoms [41]. Typical antipsychotics, particularly potent blockers of dopaminergic receptors, are usually contraindicated in PD.
Observational studies which targeted PD with dementia (PDD) found beneficial effects of olanzapine in addressing psychosis especially delusions [42]. Worsening of motor function and overall psychiatric symptoms, however, has been reported in up to 80% of individuals with PDD following olanzapine treatment [33]. Risperidone was beneficial in managing psychotic symptoms of PDD as assessed by the BPRS and the CMAI scores. In the same group, treatment with risperidone improved levels of social, occupational, and psychological functioning [43]. In practice, an unfavorable safety profile limits risperidone use.
Clozapine (see supplement) is efficacious in the treatment of PD psychosis as shown by randomized controlled trials even in relatively low dosing ranges (6.25–50 mg daily) [41, 44]. Clozapine is a selective D1 mesolimbic receptors blocker without significant binding to striatal dopamine D2 receptors. This selectivity together with its greater serotoninergic 5HT-2A/2C affinity, results in clozapine’s favorable profile in managing PD psychosis. It is the antipsychotic medication that has consistently been found to be efficacious [41, 44]. The risk of agranulocytosis and the necessity of blood monitoring with clozapine had led many experts to recommend a trial of other antipsychotics, mainly quetiapine (12.5–150 mg) before implementing use of clozapine [6, 32, 41].
Quetiapine is the most frequently prescribed antipsychotic to target psychotic symptoms in PD. In its chemical structure (dibenzothiazepine), quetiapine is similar to clozapine. Findings are, however, inconsistent and firm conclusions about quetiapine efficacy cannot be drawn. One open label trial found a significant improvement in psychotic symptoms (as assessed by BPRS) in patients treated with quetiapine for 12 weeks. In this study, the benefit of quetiapine (mean dose 91.5 mg/daily) was comparable with a benefit of clozapine (mean dose 26 mg/daily) [45]. A meta-analysis of data from different trials including a total of 241 participants randomized to either quetiapine or a comparator (placebo or clozapine) [46] failed to show efficacy. Several studies report improvement in the level of global clinical functioning of the PD patients with psychosis treated with quetiapine (as assessed by clinical global impression scales) [45, 46]. Most studies indicate that patients taking quetiapine experienced fewer side effects compared to other antipsychotics; however, quetiapine has yet to be proven to be more effective than placebo in the treatment or psychosis in this population.
In severe cases of PD psychosis, hospitalization should be considered in order to stabilize the patient. Somatic therapies may be an option in certain clinical situations. In PD, ECT was proved to be effective for depression and motor symptoms as well as for psychosis. It may be than considered to treat psychosis that has not responded to other interventions [6, 47].
Conclusions
Psychosis with different types of hallucinations and delusions may occur in the context of delirium and is almost universal as a neuropsychiatric symptom in the course of PD and AD. Consensus clinical criteria have emerged for psychosis as well as other neuropsychiatric symptoms in AD and PD. A review of studies shows that antipsychotics benefit psychosis and agitation in AD. For psychosis of PD, pimavanserin is approved by the FDA and clozapine has consistently shown clinical benefit. Quetiapine is widely prescribed for the treatment of psychosis in NDD, but the data remains equivocal and does not support its use. Clinical trials with the goal of addressing psychotic symptoms without worsening other aspects of NDD are currently limited.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: APA; 2013.
Gautam S, Jain A, Gautam M, Gautam A. Clinical practice guideline for management of psychoses in elderly. Indian J Psychiatry. 2018;60(3):363–70.
Javadpou A, Sehatpour M, Mani A, Sahraian A. Assessing diagnosis and symptoms profile of late life psychosis among an elderly population. Am J Geriatr Psychiatr. 2013;21(3):159–60.
Ropacki SA, Jeste DV. Epidemiology of and risk factors for psychosis of Alzheimer’s disease: a review of 55 studies published from 1990 to 2003. Am J Psychiatr. 2005;162(11):2022–30.
Zuidema S, Koopmans R, Verhey F. Prevalence and predictors of neuropsychiatric symptoms in cognitively impaired nursing home patients. J Geriatr Psychiatry Neurol. 2007 Mar;20(1):41–9.
Rothenberg KG. Assessment and Management of Psychiatric Symptoms in Neurodegenerative Disorders (Chapter 23) In: Neuro-Geriatrics (Ed.) Tousi Babak and Cummings Jeffrey 2017, Springer International Publishing AG. * (Comprehensive review of treatment of NPS in NDD).
APA Practice Guideline Writing Group’s “Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients With Dementia. https://doi.org/10.1176/appi.books.9780890426807.
•• Cummings J, Isaacson S, Mills R, Williams H, Chi-Burris K, Corbett A, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2014;383(9916):533–40 This Paper summarizes pharmacological properties of pimavanserin and results which led to its approval by FDA.
Brodaty H, Arasaratnam C. Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. Am J Psychiatry. 2012;169(9):946–53.
Burns A, Jacoby R, Levy R. Psychiatric phenomena in Alzheimer’s disease. Parts I-IV. Br J Psychiatry. 1990;157:72–94.
Rothenberg KG, Wiechers IR. Antipsychotics for neuropsychiatric symptoms of dementia—safety and efficacy in the context of informed consent. Psychiatr Ann. 2015;45(7):348–53.
Lopez OL, Becker JT, Chang YF, Sweet RA, Aizenstein H, Snitz B, et al. The long-term effects of conventional and atypical antipsychotics in patients with probable Alzheimer’s disease. Am J Psychiatry. 2013;170(9):1051–8.
Paulsen JS, Salmon DP, Thal LJ, Romero R, Weisstein-Jenkins C, Galasko D, et al. Incidence of and risk factors for psychosis of Alzheimer’s disease. Neurology. 2000;54(10):1965–71.
Wilkosz PA, Seltman HJ, Devlin B, Weamer EA, Lopez OL, DeKosky ST, et al. Trajectories of cognitive decline in Alzheimer’s disease. Int Psychogeriatr. 2010;22(2):281–90.
Jeste D, Finkel S. Psychosis of Alzheimer’s disease and related dementias: diagnostic criteria for a distinct syndrome. Am J Geriatr Psychiatr. 2000;8(1):29–34.
D'Onofrio G, Panza F, Sancarlo D, Paris FF, Cascavilla L, Mangiacotti A, et al. Delusions in patients with Alzheimer’s disease: a multidimensional approach. J Alzheimers Dis. 2016;51(2):427–37.
Kuhl DE, Minoshima S, Fessler JA, Ficaro EP, Wieland DM, Koeppe RA, et al. In vivo mapping of cholinergic terminals in normal aging, Alzheimer’s disease, and Parkinson’s disease. Ann Neurol. 1996;40(3):399–410.
Koppel J, Acker C, Davies P, Lopez OL, Jimenez H, Azose M, et al. Psychotic Alzheimer’s disease is associated with gender-specific tau phosphorylation abnormalities. Neurobiol Aging. 2014 Sep;35(9):2021–8.
Jacobson SA, Morshed T, Dugger BN, Beach TG, Hentz JG, Adler CH, et al. Plaques and tangles as well as Lewy-type alpha synucleinopathy are associated with formed visual hallucinations. Parkinsonism Relat Disord. 2014 Sep;20(9):1009–14.
Cummings JL, McRae T, Zhang R, The Donepezil-Sertraline Study Group. Effects of donepezil on neuropsychiatric symptoms in patients with dementia and severe behavioral disorders. Am J Geriatr Psychiatry. 2006;14:605–11.
Cummings J, Lai TJ, Hemrungrojn S, Mohandas E, Yun Kim S, Nair G, et al. Role of donepezil in the management of neuropsychiatric symptoms in Alzheimer’s disease and dementia with Lewy bodies. CNS Neurosci Ther. 2016 Mar;22(3):159–66.
Herrmann N, Lanctôt KL, Hogan DB. Pharmacological recommendations for the symptomatic treatment of dementia: the Canadian Consensus Conference on the Diagnosis and Treatment of Dementia 2012. Alzheimers Res Ther. 2013;5(Suppl1):1–12.
Holmes C, Wilkinson D, Dean C, Vethanayagam S, Olivieri S, Langley A, et al. The efficacy of donepezil in the treatment of neuropsychiatric symptoms in Alzheimer disease. Neurology. 2004;63:214–9.
Wilcock GK, Ballard CG, Cooper JA, Loft H. Memantine for agitation/aggression and psychosis in moderately severe to severe Alzheimer’s disease: a pooled analysis of 3 studies. J Clin Psychiatry. 2008;69(3):341–8.
Devanand DP, Mintzer J, Schultz SK. Relapse risk after discontinuation of risperidone in Alzheimer’s disease. N Engl J Med. 2012;367:1497–507.
Moretti R, Torre P, Antonello RM, Cazzato G, Griggio S, Bava A. Olanzapine as a treatment of neuropsychiatric disorders of Alzheimer’s disease and other dementias: a 24-month follow-up of 68 patients. Am J Alzheimers Dis Other Demen. 2003;18:205–14.
Mintzer JE, Tune LE, Breder CD, Swanink R, Marcus RN, McQuade RD, et al. Aripiprazole for the treatment of psychoses in institutionalized patients with Alzheimer dementia: a multicenter, randomized, double-blind, placebo-controlled assessment of three fixed doses. Am J Geriatr Psychiatry. 2007 Nov;15(11):918–31.
Katz I, de Deyn PP, Mintzer J, Greenspan A, Zhu Y, Brodaty H. The efficacy and safety of risperidone in the treatment of psychosis of Alzheimer’s disease and mixed dementia: a meta-analysis of 4 placebo-controlled clinical trials. Int J Geriatr Psychiatry. 2007 May;22(5):475–84.
Street JS, Clark WS, Gannon KS, Cummings JL, Bymaster FP, Tamura RN, et al. Olanzapine treatment of psychotic and behavioral symptoms in patients with Alzheimer disease in nursing care facilities: a double-blind, randomized, placebo-controlled trial. Arch Gen Psychiatry. 2000;57(10):968–76.
El-Saifi N, Moyle W, Jones C, Tuffaha H. Quetiapine safety in older adults: a systematic literature review. J Clin Pharm Ther. 2016 Feb;41(1):7–18.
Ozawa C, Roberts R, Yoshida K, Suzuki T, Lebowitz B, Reeves S, et al. Placebo effects in the treatment of noncognitive symptoms of Alzheimer’s disease: analysis of the CATIE-AD data. J Clin Psychiatry. 2017;78(9):1204–10.
Marsh L, Williams JR, Rocco M, Grill S, Munro C, Dawson TM. Psychiatric comorbidities in patients with Parkinson disease and psychosis. Neurology. 2004;293-300(32):63.
Fenelon G, Alves G. Epidemiology of psychosis in Parkinson’s disease. J Neurol Sci. 2010;289:12–7.
Fenelon G, Soulas T, Zenasni F, de Langavant LC. The changing face of Parkinson’s disease-associated psychosis: a cross-sectional study based on the new NINDS-NIMH criteria. Mov Disord. 2010;25:755–9.
Ravina B, Marder K, Fernandez HH, Friedman JH, McDonald W, Murphy D, et al. Diagnostic criteria for psychosis in Parkinson’s disease: report of an NINDS, NIMH work group. Mov Disord. 2007;22:1061–8.
Fenelon G, Mahieux F, Huon R, Ziegler M. Hallucinations in Parkinson’s disease: prevalence, phenomenology and risk factors. Brain. 2000;123(Pt 4):733–45.
Goetz CG, Fan W, Leurgans S. Antipsychotic medication treatment for mild hallucinations in Parkinson’s disease: positive impact on long-term worsening. Mov Disord. 2008;23(11):1541–5.
Murai T, Muller U, Werheid K, et al. In vivo evidence for differential association of striatal dopamine and midbrainserotonin systems with neuropsychiatric symptoms in Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 2001;13:222–8.
Huot P, Johnston TH, Darr T, Hazrati LN, Visanji NP, Pires D, et al. Increased 5-HT2A receptors in the temporal cortex of parkinsonian patients with visual hallucinations. Mov Disord. 2010;25:1399–408.
Harding AJ, Broe GA, Halliday GM. Visual hallucinations in Lewy body disease relate to Lewy bodies in the temporal lobe. Brain. 2002;125(pt 2):391–403.
Goldman JG, Holden S. Treatment of psychosis and dementia in Parkinson’s disease. Curr Treat Options Neurol. 2014;16(3):281–99.
Moretti R, Torre P, Antonello RM, Cazzato G, Griggio S, Bava A. Olanzapine as a treatment of neuropsychiatric disorders of Alzheimer’s disease and other dementias: a 24-month follow-up of 68 patients. Am J Alzheimers Dis Other Demen. 2003;18:205–14.
Workman RH Jr, Orengo CA, Bakey AA, et al. The use of risperidonefor psychosis and agitation in demented patients with Parkinson disease. J Neuropsychiatry Clin Neurosci. 1997;9:594–7.
Pollak P, Tison F, Rascol O, Destée A, Péré JJ, Senard JM, et al. Clozapine in drug induced psychosis in Parkinson’s disease: a randomised, placebo controlled study with open follow up. J Neurol Neurosurg Psychiatry. 2004;75(5):689–95.
Morgante L, Epifanio A, Spina E, Zappia M, Di Rosa AE, Marconi R, et al. Quetiapine and clozapine in parkinsonian patients with dopaminergic psychosis. Clin Neuropharmacol. 2004;27(4):153–6.
Desmarais P, Massoud F, Filion J, Nguyen QD, Bajsarowicz P. Quetiapine for psychosis in Parkinson disease and neurodegenerative parkinsonian disorders: a systematic review. J Geriatr Psychiatry Neurol. 2016;29(4):227–36 Systematic review of effectiveness of quetiapine in PD psychosis.
Hausner L, Damian M, Sartorius A, Frolich L. Efficacy and cognitive side effects of ECT in depressed elderly inpatients with co-existing mild cognitive impairment or dementia. J Clin Psychiatry. 2011;72:91–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Dementia
Electronic supplementary material
ESM 1
(DOCX 24 kb)
s
Rights and permissions
About this article
Cite this article
Rothenberg, K.G., Rajaram, R. Advances in Management of Psychosis in Neurodegenerative Diseases. Curr Treat Options Neurol 21, 3 (2019). https://doi.org/10.1007/s11940-019-0545-6
Published:
DOI: https://doi.org/10.1007/s11940-019-0545-6