Abstract
Purpose of review
This article highlights recent progress in research on treatment and neurorehabilitation of cognitive impairment in multiple sclerosis (MS) including pharmacological interventions, physical exercise, and neuropsychological rehabilitation, both in conventional and technology-assisted settings.
Recent findings
The most consistent evidence in terms of improvement or preservation of circumscribed cognitive scores in MS patients comes from moderately sampled randomized clinical trials on multimodal approaches that combine conventional or computerized neuropsychological training with psychoeducation or cognitive behavioral therapy. Disease-modifying treatments also appear to have beneficial effects in preventing or attenuating cognitive decline, whereas there is little evidence for agents such as donepezil or stimulants. Finally, physical exercise may yield some cognitive improvement in MS patients.
Summary
Despite substantial and often promising research efforts, there is a lack of validated and widely accepted clinical procedures for cognitive neurorehabilitation in MS. Development of such approaches will require collaborative efforts towards the design of interventions that are fundamentally inspired by cognitive neuroscience, potentially guided by neuroimaging, and composed of conventional neuropsychological training and cognitive behavioral therapy as well as physical exercise and therapeutic video games. Subsequently, large-scale validation will be needed with meaningful outcome measures reflecting transfer to everyday cognitive function and maintenance of training effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the advent of high-efficacy pharmacological disease-modifying treatments (DMTs), patients with relapsing remitting multiple sclerosis (RRMS) can be treated in a more efficacious and often more convenient way [1]. The higher efficacy DMTs have been shown to dramatically reduce the rate of relapses and associated impairment, particularly in the motor domain. Ocrelizumab, the first DMT approved for primary progressive multiple sclerosis (PPMS), may yield similar beneficial effects on long-term disease evolution in this patient group [2]. Clinical care and research can therefore begin to focus on prevention and management of problems other than relapse frequency or impairments in motor and ambulatory function.
Cognitive impairment represents one such problem encountered by MS patients. Up to two thirds of people with MS experience altered cognitive function, and this represents a significant burden in everyday life [3]. Cognitive impairment is related to disease progression and higher age [4•]. Efficient approaches to treating cognitive deficits are still lacking, although numerous promising research efforts have been undertaken over the past few years in this direction.
In this article, we review recent research on interventions for cognitive deficits in MS, first highlighting the primarily affected cognitive domains and commonly used neuropsychological assessment tools, followed by pharmacological studies, before turning to physical exercise and neuropsychological rehabilitation, both in conventional and technology-assisted settings.
Cognitive impairment and outcome measures in MS patients
Processing speed, attention, and working and episodic memory are the major cognitive domains affected by MS [3]. These functions rely on interplay between distributed cortical areas in the fronto-parietal networks, mediated by white-matter pathways connecting these regions. MS predominantly affects these white-matter connections. Despite recent criticism [5], diffusion magnetic resonance imaging (MRI) may provide some insights on white matter integrity. Indeed, diffusion MRI shows reduced fiber tract fractional anisotropy in white-matter networks considered relevant for sustained attention, working memory, and processing speed—that is specifically related to cognitive deficits in these domains [6]. Importantly, these abnormalities were also found in normal appearing white matter of MS patients, underlining contribution of pathophysiological mechanisms beyond clinically manifest demyelination. For instance, microstructural measures in normal appearing white matter provided by advanced MRI may predict cognitive fatigue, attention deficits, and overall disability [7]. Apart from this subcortical disconnection syndrome, gray matter abnormalities are increasingly detected in imaging of MS patients and are likely to contribute to cognitive dysfunction [8]. Cortical lesions in early RRMS as revealed by Magnetization-Prepared 2 Rapid Acquisition Gradient Echoes (MP2RAGE) MRI were found to predict long-term memory deficits [9]. Whole-brain, cortical, and putaminal atrophy was associated to Expanded Disability Status Scale (EDSS) progression over 10 years [10].
Older age and male gender appear to be related to greater cognitive impairment [3, 4•]. Cognitive deficits are also found nearly twice as often in patients with progressive forms of MS (PPMS and secondary progressive MS, SPMS) than in RRMS [4•, 11]. A meta-analysis indicated not only quantitative but also qualitative differences in cognitive profile, with a higher proportion and magnitude of executive deficits in progressive MS but more frequent memory dysfunction in RRMS due to altered retrieval [11]. As there is only one, recently approved and partially effective therapy for progressive MS, ocrelizumab [2], the patients with progressive MS are in particular need for effective cognitive interventions.
Fatigue, which is highly debilitating in MS, may also confound results. While the impact of fatigue on cognitive function and outcome measures remains unclear [12], beneficial effects on fatigue have been shown for physical exercise [13, 14] and some computerized neuropsychological interventions [15, 16]. Conversely, cognitive training may also increase fatigue levels [17].
The clinical assessment of cognitive function relies on a standardized neuropsychological examination that is quite extensive, in order to pick up possibly isolated early deficits arising from inter-individual variability in network architecture and pathological changes. On the other hand, research on cognitive deficits and rehabilitation has relied on relatively short and easy-to-use tests and batteries. In what follows, we will briefly outline the most important cognitive outcome measures in MS to set the stage for discussing recent trials on cognitive neurorehabilitation.
The currently most widely accepted tool is the Symbol Digit Modalities Test (SDMT), where patients fill in the numbers associated to presented symbols, according to a symbol-digit key [18]. The SDMT mainly assesses processing speed but is also affected by working memory, attention, and thus learning, as well as hand function. Nonetheless, it is a sensitive cognitive test without floor or ceiling effects and is a recommended outcome measure for trials on cognition in MS [19•, 20]. The Paced Auditory Serial Attention Test (PASAT), where participants add numbers presented verbally, assesses auditory processing speed, working memory, and calculation abilities [21]. The PASAT was historically the standard cognitive outcome measure in MS trials and part of the Multiple Sclerosis Functional Composite (MSFC). However, due to its lower sensitivity and lower tolerance by patients and the higher occurrence of ceiling and practice effects, it is being replaced by the SDMT in the MSFC [20].
The Selective Reminding Test (SRT) provides a useful assessment of verbal long-term memory despite relative heterogeneity of the normative data. This test evaluates recall of unrelated words, with subsequent presentation of words that were not recalled on the current trial [22]. The California Verbal Learning Test-II (CVLT-II) [23], that evaluates encoding, recall, and recognition of an item list at immediate, short, and long delays and includes interference items, is exquisitely well normalized.
Screening, longitudinal assessment, and measuring trial outcomes for visuospatial memory can be reliably accomplished with the Brief Visuospatial Memory Test-Revised (BVMT-R). Here, the patient draws geometric shapes from memory at short and long delays after their presentation, and then has to recognize which geometric forms had been presented [24]. The BVMT-R outperforms the 10/36 Spatial Recall Test (10/36 SPART) [25] in terms of sensitivity, reliability, and availability of normative data [26]. Yet, the 10/36 SPART, where patients reproduce the spatial arrangement of ten pawns on a 6 × 6 checkerboard immediately after stimulus presentation, and after a delay, does not depend as heavily on preserved upper limb function [19•].
Broad assessment of executive deficits in MS patients is most often accomplished with the Delis–Kaplan Executive Function System (D-KEFS) [27], that provides encompassing measures of several verbal and spatial executive functions.
Finally, in an effort to propose an international consensus battery of tests sensitive for diagnosing cognitive deficits in MS while requiring short administration times by non-specialist staff and maintaining validity across different cultures and languages, an international board of specialists has proposed and validated the Brief International Cognitive Assessment for Multiple Sclerosis [28]. The BICAMS consists of the above-described SDMT, the CVLT-II, and the immediate recall version of the BVMT-R tests [29••], requires approximately 15 min to administer, and benefits from a growing effort to validate it in various populations around the globe (Langdon 2012 no. 1).
Pharmacological effects on cognition
One primary approach to preventing cognitive impairment in MS is through prevention of inflammatory activity. Data from several large-scale trials of DMTs including interferons, fingolimod, and natalizumab have demonstrated beneficial effects in terms of delaying and perhaps improving cognitive function.
To provide a few examples, in the case of interferons, in the BENEFIT trial that enrolled 464 patients with clinically isolated syndrome (CIS), PASAT-3 scores improved significantly more after 2 years of treatment with interferon beta-1b relative to placebo [30]. Furthermore, the 5-year active treatment follow-up [31], as well as the subsequent 3-year [32] and 6-year observational follow-ups [33] confirmed that the group initially receiving interferon beta-1b maintained higher PASAT scores throughout. A higher dose of interferon beta-1a was found to be associated to lower incidence of neuropsychological test performance at one standard deviation below normal in 201 RRMS patients in a 2-year extension study of the 3-year COGIMUS trial [34], yet a trend towards greater cognitive impairment in the lower dose group had already been seen at baseline of the COGIMUS trial [35].
In the SENTINEL trial in which 500 patients received natalizumab combined with interferon beta 1-a vs 245 patients who received placebo and interferon beta 1-a for 2 years [36], no difference was seen in evolution of PASAT performance [37]. However, in the AFFIRM trial [38], natalizumab alone reduced the rate of PASAT score decline in 574 patients when compared with 282 patients on placebo [37]. Natalizumab treatment has also been suggested to significantly diminish fatigue scores and cognitive impairment in observational studies that included cohorts of 153 [39] and 41 [40] patients, respectively. More recently, in a post-hoc pooled analysis of the fingolimod pivotal clinical trials (FREEDOMS [41] and FREEDOMS II [42]), which included 1556 patients overall, treatment with fingolimod for 6 months yielded improved sustained attention as reflected by the PASAT, whereas treatment with placebo did not [43].
It is likely that the beneficial effects of DMTs on cognition arise from the prevention of inflammatory activity and secondary neurodegeneration. Evaluation of cognitive effects beyond reduction of inflammatory activity would require differently designed trials specifically aimed at cognitive assessment, controlling for potential practice effects and adjusting for overall degree of alterations in structural and functional connectivity.
To date, assessment of substances known to improve cognition in other neurological or psychiatric domains has remained rather limited. No significant differences in verbal memory as assessed by the SRT were found in 61 patients with RRMS, SPMS, and PPMS on donepezil, a cholinesterase inhibitor used in Alzheimer’s disease, 10 mg daily over 24 weeks as compared to 59 patients on placebo [44]. Stimulating agents have also been tested: 30 mg of l-amphetamine daily over 4 weeks in 99 patients vs placebo in 37 patients significantly improved visuospatial memory assessed by BVMT-R and verbal memory assessed by the CVLT-II, but the latter only in patients with impaired memory at baseline [45]. No effects on learning or self-reported fatigue were found in a small (n = 16) crossover trial for 200 mg modafinil daily during 2 weeks [46].
On the other hand, a commonly prescribed potassium channel blocker, fampridine, has been shown to not only improve walking in MS patients, but also physical and cognitive fatigue [47, 48], as well as alertness, psychomotor speed, and verbal fluency [47].
Conventional neuropsychological rehabilitation
Several RCTs have evaluated the utility of conventional neuropsychological approaches for cognitive neurorehabilitation in MS, primarily in the domains of verbal learning and memory. Strong positive evidence comes from the MEMREHAB study, a double-blind RCT on the modified Story Memory Technique (mSMT) that employs imagery and context over 10 sessions to facilitate verbal learning [49••]. Eighty-six patients with MS and impaired learning as measured by the Open Trial SRT were included and randomly assigned to mSMT or a placebo intervention. The placebo condition featured the same number of sessions but lacked mSMT content. The CVLT learning slope was significantly higher in the mSMT than the placebo group, and everyday memory function evaluated by the Rivermead Behavioral Memory Test also showed a significant specific improvement for the mSMT group. Follow-up at 6 months demonstrated some CVLT performance decline in both groups. However, the mSMT group retained a higher CVLT learning slope. In a preliminary study using the same technique and including functional MRI as outcome measure, similar CVLT benefits were shown in 16 MS patients, with activation of the right medial frontal gyrus being associated with CVLT improvement [50]. Other studies have also indicated that mental visual imagery techniques may be efficient to alleviate autobiographic memory deficits [51, 52] and to promote episodic future thinking [52] in MS patients. In an elegant design including an active control condition, 11 patients undergoing textbook executive function exercises during half an hour four times weekly over 6 weeks exhibited significant improvement in verbal learning, whereas 14 patients assigned to computerized reaction capacity training and 15 patients without any intervention did not [53]. Crucially, the beneficial effects in the cognitive intervention group were still present at follow-up after 1 year.
Promising outcomes were found for an integrative cognitive rehabilitation approach, REHACOP, initially developed for schizophrenia. REHACOP represents a 3-month group program starting with remediation of low-level cognition, before addressing higher-order cognitive processes and, eventually, daily life functions that require integration across cognitive domains. The cognitive domains range from processing speed and attention over language to executive function and social cognition. Processing speed, working memory, verbal memory, and executive functioning outcomes of 21 MS patients after 3 months of REHACOP training were significantly better than in 21 patients on a waiting list [54]. However, between-group differences were already present at baseline in most cognitive scores.
Multidisciplinary and cognitive-behavioral interventions
Interdisciplinary approaches inspired by models from cognitive neuroscience and including psychoeducation or cognitive-behavioral therapy are also increasingly considered. Comprehensive group cognitive rehabilitation combining psychoeducation with memory, self-regulation, and compensatory training in 17 female MS patients yielded substantial improvement of memory and executive function but not attention [55]. This trial included a placebo group of 17 female patients undergoing the same number of sessions without therapeutic content. When compared to standard 4-week inpatient rehabilitation, a multidisciplinary intervention of the same duration that targeted coping with cognitive deficits resulted in better scores for quality of life, anxiety, and depression in 60 patients with subjective executive deficits [56]. In both groups, similar improvements were seen in self-reported executive function. The intervention consisted of comprehensive neuropsychological assessment with feedback and diverse information on cognitive deficits in MS. A 5-week program on self-awareness and cognitive monitoring increased knowledge of the cognitive profile associated with MS and efficacy when managing cognitive problems in 35 patients [57]. In 11 patients with MS, similar approaches combined with training of compensatory strategies and home-based computer-assisted cognitive training improved phasic and selective alertness as assessed by the Test Battery of Attentional Performance (TAP), with a trend for SDMT improvement [58].
Neurotechnology for cognitive neurorehabilitation
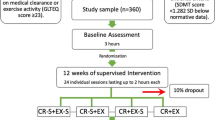
Over the past decade, technological approaches, in particular computerized neuropsychological training and serious video games, have been evaluated as complementary or optimized procedures for cognitive neurorehabilitation (Table 1). To cite some examples that have reported improvements primarily in the verbal learning and memory domain, 12 weeks of the home-based computerized CogniFit Personal Coach intervention improved general memory as well as visual and verbal working memory in 59 MS patients as compared to 48 patients without intervention [17]. In the Memory, Attention, and Problem Solving Skills for Persons with Multiple Sclerosis (MAPSS-MS) RCT, an intervention with eight weekly group sessions to learn compensatory strategies and home-based computerized training, both 34 patients on treatment and 27 patients on a waiting list significantly improved between baseline and follow-up. However, the intervention group outperformed the control group on verbal memory as measured by the CVLT-II and self-reported compensatory strategies [71]. Benefits in verbal and visual episodic memory, and in verbal fluency were found in ten MS patients with mild to moderate cognitive impairment after 13 bimonthly sessions of the ProCogSEP rehabilitation as compared to ten patients enrolled in a discussion program [61]. Weekly sessions of computerized training during 3 months significantly improved verbal memory, visuo-spatial delayed recall, working memory, processing speed, and phonetic fluency in 30 patients compared to 32 patients on a waiting list [70]. An RCT on the computer-based Sclerosi Multipla Intensive Cognitive Training (SMICT) during 15 weeks indicated significant SRT delayed recall and SPART 10/36 memory test improvements at 1-year follow-up in 22 MS patients specifically trained in their impaired cognitive domains vs 19 patients trained in unimpaired domains [16]. Of note, a between-group SRT delayed recall difference was present at baseline.
In the domains of processing speed and executive function, 13 weekly sessions of attention and working memory rehabilitation including computer-based exercise, psychoeducation, and strategy learning did not significantly change SDMT scores but improved subjective cognitive deficits immediately and 6 months after training in the intervention group consisting of 58 patients as compared to 40 patients in the control group [68]. Twice weekly Attention Processing Training on a computer at home over 3 months significantly improved PASAT scores in the treatment group of 55 patients, although self-reports of cognitive function were similar to 33 patients on non-specific computerized training [59]. Home-based computerized attention training, psychological counseling, and weekly group therapy over 5 weeks yielded significant improvement in alertness and divided attention assessed by the TAP in 20 MS patients compared to 20 patients on a waiting list [15]. A pilot study targeting attention and working memory with the PositScience InSight® and Brain Twister showed a trend towards better PASAT outcomes in 15 MS patients training 6 days per week during 6 weeks as compared to 15 patients on sham training [66]. A study aimed at problem-solving and attention using the videogame Space Fortress developed by cognitive psychophysiologists reported specific game skills improvement in 14 patients with MS, but without transfer to the targeted cognitive domains [67]. Five days a week of Nintendo DS®-based Dr. Kawashima’s Brain Training during 8 weeks improved SDMT and Stroop performance in 18 patients as compared to 17 patients on a waiting list [65]. The Hasomed RehaCom® is a commercially available home-based approach targeting attention, concentration, multi-tasking, planning, and logical thinking. As compared to 14 cognitively impaired RRMS patients in a newspaper reading control group, twice weekly home-based RehaCom® sessions over 8 weeks significantly improved SDMT, PASAT, SRT delayed recall, and SPART 10/36 scores in 18 patients. Furthermore, RehaCom® training specifically increased resting-state functional MRI coupling between the posterior cingulate and bilateral inferior parietal cortex [60•]. RehaCom® also yielded significant SDMT improvement in 19 MS patients with cognitive deficits as compared to 19 patients watching a series of natural history, but this effect did not persist at follow-up 12 weeks after training [62]. Ten patients with deficits on the PASAT and Wisconsin Card Sorting Test exhibited significant improvement on these measures after 3 months of RehaCom® training, as compared to ten patients without intervention [69]. After 6 weeks of twice weekly RehaCom® training, 12 patients performed significantly better on a Stroop task than 11 patients undergoing visuomotor coordination training for the same period of time [63]. In perhaps the largest study to date, the 12-week adaptive PositScience BrainHQ® training for MS patients with altered SDMT resulted in a significant cognitive composite score improvement in 74 patients as compared to 61 patients playing non-specific video games [64]. Overall, computerized and neurotechnological training yields promising results with the RehaCom® representing the currently most extensively studied approach, that is also used in clinical routine. As we will discuss further below, inclusion criteria (existing cognitive deficits), personalized training content (e.g., targeting the patient’s specifically impaired cognitive domains), and adaptation, gamification, control conditions and study design are methodological issues that need to be resolved, although some of them have been tackled in the above studies.
Cognitive effects of physical exercise in MS
Aerobic exercise is believed to improve brain function through physiological adaptive processes including hemodynamics and oxygen metabolism [72], and physical exercise in combination with cognitive training has yielded greater beneficial effects than cognitive training alone [73]. The effects of various forms of physical exercise on cognition have also been evaluated in several small trials in MS patients. The largest randomized controlled trial (RCT) compared 60 patients who underwent supervised and home-based aerobic exercise during 3 months in addition to standard clinical care to 60 patients on standard clinical care alone. Whereas several measures including fatigue, social function, and quality of life were substantially improved in the aerobic exercise group; no significant benefit was found on attention as measured by the PASAT [13]. A similar design compared arm, bicycle, or rowing ergometry over 8–10 weeks in patients with advanced progressive MS and found all aerobic exercise patients performed better on the verbal memory and learning test (VLMT) as compared to waiting list controls [74]. Alertness and attention shifts also improved significantly, whereas the SDMT did not. An RCT of a home-based step training with video games promoting physical exercise (exergames) twice weekly over 12 weeks showed beneficial effects on the time-up-and-go dual task and several balance scores in 23 MS patients (vs no specific intervention in 21 patients), but only non-significant trends towards improvements in SDMT and trail-making test [75]. In a pilot randomized trial (n = 10), progressive treadmill exercise training over 12 weeks showed a promising SDMT effect size in the intervention vs waiting list group, but small sample size precluded assessment of significance [76]. Ten weeks of yoga dramatically improved selective attention in ten MS patients, whereas sports climbing over the same period did not affect cognition but significantly reduced fatigue and pyramidal deficits [14]. Combined aerobic, balance, and physical flexibility exercise over 8 weeks showed promising effects on SDMT, PASAT, and long-term memory in 17 MS patients, yet in the absence of a control group [77]. Taken together, the data on beneficial effects of physical exercise on cognition in MS are still rather sparse but appear encouraging. The selection of type and dose of exercise as well as sample sizes remain methodological issues that need to be addressed in the future.
Conclusions: common challenges and possible solutions
In summary, our ability to prevent, slow, and eventually improve cognitive impairment in people with MS is being bolstered by pharmacological, neuropsychological, and technological advances, as well as possibly physical activity. Despite these promising data, there is still a lack of clearly validated, widely accepted and accessible approaches for cognitive neurorehabilitation in MS.
Several factors may help explain this discrepancy between clinical research and practice. Most of the reviewed studies assessed 20 to 80 patients per treatment arm, representing rather moderate sample sizes. Major covariates such as different MS types, disease duration, age, and gender have only rarely been controlled for, although they may significantly influence the degree of cognitive impairment and training effects [4•, 11]. Future cognitive neurorehabilitation trials would ideally need to enroll several hundreds of patients in order to provide reliable conclusions on how rehabilitation benefits may depend on these factors. Establishment of truly efficient, evidence-based clinical procedures for cognitive neurorehabilitation in MS requires further optimized, standardized, and interdisciplinary development of targeted multimodal approaches inspired by cognitive and neurobiological models [19•], followed by large-scale clinical trials.
In pharmacological trials, such multi-site international cooperation has already become indispensable and enabled substantial development of DMTs [36, 38, 41]. Despite promising reports on potential beneficial DMT effects on cognition in MS patients, deeper insight would require additional trials with cognitive effects as main hypotheses, reflected in primary outcome measures and methodology. Indeed, some of the trials appear to have been confounded by practice effects, which can be reduced by repetitive test administration at baseline. The advent of new, more efficient DMTs for MS also offers the perspective for higher sustainability of cognitive neurorehabilitation once disease progression has been significantly reduced or even nearly halted.
Furthermore, the content of cognitive neurorehabilitation trials remains a crucial issue and would benefit from high quality standardization. This article reviews a multitude of interventions that have been developed and assessed so far. Although some studies have tested the same approaches, there is no consensus as to the most efficient strategy for cognitive neurorehabilitation in MS and, to the best of our knowledge, no intervention has been evaluated in terms of clinical implementation. The lack of translation into clinical practice underlines the need for designing an optimal, efficient, and accessible training program. The outcomes presented above suggest stepwise (from lower to higher order cognition) neuropsychological intervention assisted by state-of-the-art neurotechnology such as adaptive video games along with psychoeducation and physical exercise may represent a promising strategy. Clinically relevant cognitive neurorehabilitation in MS would require cutting edge, multi-component procedures developed in collaborative effort.
For instance, in order to obtain more homogeneous group responses, restricting inclusion to patients with cognitive deficits that can be quantified using standard tests and questionnaires may be helpful. Indeed, higher training benefits have been shown for cognitively impaired patients as compared to healthy controls [78], and the studies reviewed here tend to indicate more significant effects for patients with objective cognitive deficits than for patients without or only self-reported deficits. Furthermore, personalized training, such as mainly focusing on impaired domains [16], may produce better individual outcomes than one-fits-all approaches. Finding the training dose and duration allowing an optimal balance between efficacy and efficiency represents another challenge for cognitive neurorehabilitation. Yet, this challenge is even overshadowed by the need for appropriate control conditions for cognitive training. Obviously, waiting list or no-contact conditions result in different expectations than some kind of intervention and may thus yield lower placebo effects [79]. However, designing or selecting an optimal placebo condition that does not reproduce some beneficial effects of the specific cognitive training is not straightforward [80].
Outcome measures focusing on transfer of specific cognitive training effects to positive, measurable impact on everyday cognitive function, and their long-term persistence represent further principal challenges for cognitive neurorehabilitation. Only few of the above studies evaluated for or achieved such effects [16, 49••, 53, 56, 68]. However, in order to justify cognitive interventions over several weeks or months, such interventions have to yield measurable everyday life benefits.
Recent neurotechnological progress may significantly contribute to overcoming these limitations and to designing well-controlled, personalized, and adaptive cognitive interventions, as well as standardized tools to better test real-life cognitive function (such as virtual reality). Computerized procedures may afford home-based or even mobile cognitive training and thus help to improve accessibility, such as for patients having to commute between their residence and the neurorehabilitation clinic or for patients in societies with different levels of expectations, challenges, and clinical care across the world. Some promising data on home-based computerized training has been discussed above [17, 60•]. Furthermore, neurotechnological paradigms offer a high level of standardization across training sessions and centers, as compared to training that principally depends on the administering therapist. Gamified training is also known to harness participation and outcomes, mainly through motivational aspects [81]. Real-time performance assessment and adaptation of the difficulty level have been shown to represent key points for efficient cognitive interventions [82••, 83, 84]. Such online closed-loop adaptation minimizes both frustration and ceiling effects and affords personalized training [80]. Inclusion of physical exercise and interaction with other training participants may afford higher cognitive improvement, as shown for active vs sedentary versions of casual exergames [85] and a specifically developed exergame [86]. Whether a combination of cognitive with physical exercise would yield better effects than cognitive intervention alone has not yet been addressed in MS patients. Some data in elderly patients with and without cognitive decline suggest that combined exercise may outperform unimodal training [73]. Other research in healthy older adults suggests cognitive and particularly dual-task training alone drives cognitive benefits [87]. Implementation of fundamental multidisciplinary knowledge from cognitive and clinical neuroscience in designing such interventions [80] will pave the way towards personalized or precision neurorehabilitation.
Brain imaging represents another promising tool for stratification of patients according to their potential for recovery and plasticity, and to plan or adapt training [88]. Measures of brain atrophy may contribute to patient stratification with respect to potential treatment outcomes [53], yet the state-of-the-art remains currently limited in terms of individual predictions [89]. Substantial progress would be required in procedures and understanding of brain plasticity and its neuroimaging markers on an individual level. Clinical implementation of advanced MRI techniques may provide additional insights into individual white but also gray matter affection [7, 90], and the same holds true for computational integration of measures of white-matter connectivity and functional communication between gray matter areas [91].
Understanding brain plasticity and functional recovery may also benefit from longitudinal functional MRI [92]. Some preliminary efforts have been undertaken towards linking recovery and brain activation on an individual level [93]. Furthermore, functional MRI shows higher cerebellar activation after cognitive interventions in MS patients that is associated to improvement in attention [63]. This is little surprising given increasing evidence on cerebellar involvement in various cognitive processes, through closed loops with the respective regions in the cerebral cortex [94]. The cerebellum is also a predominant site of affection in MS—imaging may thus help to assess early cerebellar damage and to reveal potentially limited compensatory potential [95]. On the other hand, given its remote position and connections to various areas relevant for cognition, the cerebellum may also represent a promising candidate for neuromodulation through brain stimulation [96].
Finally, electronic health records [97], online research platforms [98], and wearable device data on everyday activity and cognitive well-being [99] will contribute to enriched and more ecological patient data and outcome measures. Integration of unconventional albeit long-standing rehabilitation gears, such as rhythm and music may also be useful. Sung words were better recalled by MS patients than spoken ones, with stronger bilateral frontal engagement as evidenced by electroencephalography [100].
In conclusion, the reviewed data and state-of-the-art speak towards collaborative efforts in the development of cutting-edge multimodal training that optimally harnesses the current potential of different interventional components, such as conventional neuropsychological intervention, cognitive behavioral therapy, physical exercise, and serious video games, followed by large-scale clinical trials looking into ecological outcome measures.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wingerchuk DM, Weinshenker BG. Disease modifying therapies for relapsing multiple sclerosis. BMJ. 2016;354:i3518.
Montalban X, Hauser SL, Kappos L, Arnold DL, Bar-Or A, Comi G, et al. Ocrelizumab versus placebo in primary progressive multiple sclerosis. N Engl J Med. 2017;376:209–20.
Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7:1139–51.
• Ruano L, Portaccio E, Goretti B, Niccolai C, Severo M, Patti F, et al. Age and disability drive cognitive impairment in multiple sclerosis across disease subtypes. Mult Scler. 2017;23:1258–67 This work analyzes the effect of age and disease progression on cognition in multiple sclerosis.
Jones DK, Knosche TR, Turner R. White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. NeuroImage. 2013;73:239–54.
Dineen RA, Vilisaar J, Hlinka J, Bradshaw CM, Morgan PS, Constantinescu CS, et al. Disconnection as a mechanism for cognitive dysfunction in multiple sclerosis. Brain. 2009;132:239–49.
Bonnier G, Roche A, Romascano D, Simioni S, Meskaldji D, Rotzinger D, et al. Advanced MRI unravels the nature of tissue alterations in early multiple sclerosis. Ann Clin Transl Neurol. 2014;1:423–32.
Rocca MA, Amato MP, de Stefano N, Enzinger C, Geurts JJ, Penner IK, et al. Clinical and imaging assessment of cognitive dysfunction in multiple sclerosis. Lancet Neurol. 2015;14:302–17.
Simioni S, Amarù F, Bonnier G, Kober T, Rotzinger D, du Pasquier R, et al. MP2RAGE provides new clinically-compatible correlates of mild cognitive deficits in relapsing-remitting multiple sclerosis. J Neurol. 2014;261:1606–13.
Jacobsen C, Hagemeier J, Myhr KM, Nyland H, Lode K, Bergsland N, et al. Brain atrophy and disability progression in multiple sclerosis patients: a 10-year follow-up study. J Neurol Neurosurg Psychiatry. 2014;85:1109–15.
Zakzanis KK. Distinct neurocognitive profiles in multiple sclerosis subtypes. Arch Clin Neuropsychol. 2000;15:115–36.
Morrow SA, Weinstock-Guttman B, Munschauer FE, Hojnacki D, Benedict RH. Subjective fatigue is not associated with cognitive impairment in multiple sclerosis: cross-sectional and longitudinal analysis. Mult Scler. 2009;15:998–1005.
Carter A, Daley A, Humphreys L, Snowdon N, Woodroofe N, Petty J, et al. Pragmatic intervention for increasing self-directed exercise behaviour and improving important health outcomes in people with multiple sclerosis: a randomised controlled trial. Mult Scler. 2014;20:1112–22.
Velikonja O, Curic K, Ozura A, Jazbec SS. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin Neurol Neurosurg. 2010;112:597–601.
Pusswald G, Mildner C, Zebenholzer K, Auff E, Lehrner J. A neuropsychological rehabilitation program for patients with multiple sclerosis based on the model of the ICF. NeuroRehabilitation. 2014;35:519–27.
Mattioli F, Stampatori C, Bellomi F, Danni M, Compagnucci L, Uccelli A, et al. A RCT comparing specific intensive cognitive training to aspecific psychological intervention in RRMS: the SMICT study. Front Neurol. 2014;5:278.
Shatil E, Metzer A, Horvitz O, Miller A. Home-based personalized cognitive training in MS patients: a study of adherence and cognitive performance. NeuroRehabilitation. 2010;26:143–53.
Smith A. Symbol digit modalities test. Los Angeles: Western Psychological Services; 1982.
• Sumowski JF, Benedict R, Enzinger C, Filippi M, Geurts JJ, Hamalainen P, et al. Cognition in multiple sclerosis: State of the field and priorities for the future. Neurology. 2018;90:278–88 Informative article on cognitive assessment and rehabilitation in multiple sclerosis.
Benedict RH, DeLuca J, Phillips G, LaRocca N, Hudson LD, Rudick R, et al. Validity of the symbol digit modalities test as a cognition performance outcome measure for multiple sclerosis. Mult Scler. 2017;23:721–33.
Gronwall DM. Paced auditory serial-addition task: a measure of recovery from concussion. Percept Mot Skills. 1977;44:367–73.
Buschke H. Selective reminding for analysis of memory and learning. J Verbal Learn Verbal Behav. 1973;12:543–50.
Delis DC, Kramer JH, Kaplan E, Ober BA. California verbal learning test–II, second edition. San Antonio: The Psychological Corporation; 2000.
Benedict RHB. Brief visuospatial memory test - revised: Professional manual. Lutz: Psychological Assessment Resources, Inc.; 1997.
Rao SM. A manual for the brief repeatable battery of neuropsychological tests in multiple sclerosis. New York: National Multiple Sclerosis Society; 1990.
Niccolai C, Portaccio E, Goretti B, Hakiki B, Giannini M, Pastò L, et al. A comparison of the brief international cognitive assessment for multiple sclerosis and the brief repeatable battery in multiple sclerosis patients. BMC Neurol. 2015;15:204.
Delis DC, Kaplan E, Kramer JH. Delis-Kaplan Executive Function System (D-KEFS). San Antonio: The Psychological Corporation; 2001.
Benedict RH, et al. Brief international cognitive assessment for MS (BICAMS): international standards for validation. BMC Neurol. 2012;12:55.
•• Langdon DW, Amato MP, Boringa J, Brochet B, Foley F, Fredrikson S, et al. Recommendations for a Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS). Mult Scler. 2012;18:891–8 Study establishing the rationale, benefits, and roadmap to using the BICAMS as a rapid, feasible in-clinic screen for cognitive impairment in people with MS.
Penner IK, Stemper B, Calabrese P, Freedman MS, Polman CH, Edan G, et al. Effects of interferon beta-1b on cognitive performance in patients with a first event suggestive of multiple sclerosis. Mult Scler. 2012;18:1466–71.
Kappos L, Freedman MS, Polman CH, Edan G, Hartung HP, Miller DH, et al. Long-term effect of early treatment with interferon beta-1b after a first clinical event suggestive of multiple sclerosis: 5-year active treatment extension of the phase 3 BENEFIT trial. Lancet Neurol. 2009;8:987–97.
Edan G, Kappos L, Montalban X, Polman CH, Freedman MS, Hartung HP, et al. Long-term impact of interferon beta-1b in patients with CIS: 8-year follow-up of BENEFIT. J Neurol Neurosurg Psychiatry. 2014;85:1183–9.
Kappos L, Edan G, Freedman MS, Montalbán X, Hartung HP, Hemmer B, et al. The 11-year long-term follow-up study from the randomized BENEFIT CIS trial. Neurology. 2016;87:978–87.
Patti F, et al. Subcutaneous interferon beta-1a may protect against cognitive impairment in patients with relapsing-remitting multiple sclerosis: 5-year follow-up of the COGIMUS study. PLoS One. 2013;8:e74111.
Patti F, Amato MP, Bastianello S, Caniatti L, di Monte E, Ferrazza P, et al. Effects of immunomodulatory treatment with subcutaneous interferon beta-1a on cognitive decline in mildly disabled patients with relapsing-remitting multiple sclerosis. Mult Scler. 2010;16:68–77.
Rudick RA, Stuart WH, Calabresi PA, Confavreux C, Galetta SL, Radue EW, et al. Natalizumab plus interferon beta-1a for relapsing multiple sclerosis. N Engl J Med. 2006;354:911–23.
Weinstock-Guttman B, Galetta SL, Giovannoni G, Havrdova E, Hutchinson M, Kappos L, et al. Additional efficacy endpoints from pivotal natalizumab trials in relapsing-remitting MS. J Neurol. 2012;259:898–905.
Polman CH, O'Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354:899–910.
Iaffaldano P, et al. Impact of natalizumab on cognitive performances and fatigue in relapsing multiple sclerosis: a prospective, open-label, two years observational study. PLoS One. 2012;7:e35843.
Wilken J, Kane RL, Sullivan CL, Gudesblatt M, Lucas S, Fallis R, et al. Changes in fatigue and cognition in patients with relapsing forms of multiple sclerosis treated with Natalizumab: the ENER-G study. Int J MS Care. 2013;15:120–8.
Kappos L, Radue EW, O'Connor P, Polman C, Hohlfeld R, Calabresi P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362:387–401.
Calabresi PA, Radue EW, Goodin D, Jeffery D, Rammohan KW, Reder AT, et al. Safety and efficacy of fingolimod in patients with relapsing-remitting multiple sclerosis (FREEDOMS II): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:545–56.
Kappos L, Radue EW, Chin P, Ritter S, Tomic D, Lublin F. Onset of clinical and MRI efficacy occurs early after fingolimod treatment initiation in relapsing multiple sclerosis. J Neurol. 2016;263:354–60.
Krupp LB, Christodoulou C, Melville P, Scherl WF, Pai LY, Muenz LR, et al. Multicenter randomized clinical trial of donepezil for memory impairment in multiple sclerosis. Neurology. 2011;76:1500–7.
Sumowski JF, Chiaravalloti N, Erlanger D, Kaushik T, Benedict RHB, DeLuca J. L-amphetamine improves memory in MS patients with objective memory impairment. Mult Scler. 2011;17:1141–5.
Ford-Johnson L, DeLuca J, Zhang J, Elovic E, Lengenfelder J, Chiaravalloti ND. Cognitive effects of modafinil in patients with multiple sclerosis: a clinical trial. Rehabil Psychol. 2016;61:82–91.
Broicher SD, Filli L, Geisseler O, Germann N, Zörner B, Brugger P, et al. Positive effects of fampridine on cognition, fatigue and depression in patients with multiple sclerosis over 2 years. J Neurol. 2018;265:1016–25.
Pavsic K, Pelicon K, Ledinek AH, Sega S. Short-term impact of fampridine on motor and cognitive functions, mood and quality of life among multiple sclerosis patients. Clin Neurol Neurosurg. 2015;139:35–40.
•• Chiaravalloti N, Moore NB, Nikelshpur OM, DeLuca J. An RCT to treat learning impairment in multiple sclerosis: the MEMREHAB trial. Neurology. 2013;81:2066–72 First study to convincingly show an effect of cognitive remediation on improvement in verbal learning in people with MS.
Chiaravalloti ND, Wylie G, Leavitt V, DeLuca J. Increased cerebral activation after behavioral treatment for memory deficits in MS. J Neurol. 2012;259:1337–46.
Ernst A, et al. Autobiographical memory in multiple sclerosis patients: assessment and cognitive facilitation. Neuropsychol Rehabil. 2012
Ernst A, Blanc F, De Seze J, Manning L. Using mental visual imagery to improve autobiographical memory and episodic future thinking in relapsing-remitting multiple sclerosis patients: a randomised-controlled trial study. Restor Neurol Neurosci. 2015;33:621–38.
Fink F, Rischkau E, Butt M, Klein J, Eling P, Hildebrandt H. Efficacy of an executive function intervention programme in MS: a placebo-controlled and pseudo-randomized trial. Mult Scler. 2010;16:1148–51.
Rilo O, Peña J, Ojeda N, Rodríguez-Antigüedad A, Mendibe-Bilbao M, Gómez-Gastiasoro A, et al. Integrative group-based cognitive rehabilitation efficacy in multiple sclerosis: a randomized clinical trial. Disabil Rehabil. 2018;40:208–16.
Mani A, Chohedri E, Ravanfar P, Mowla A, Nikseresht A. Efficacy of group cognitive rehabilitation therapy in multiple sclerosis. Acta Neurol Scand. 2018;137:589–97.
Hanssen KT, Beiske AG, Landro NI, Hofoss D, Hessen E. Cognitive rehabilitation in multiple sclerosis: a randomized controlled trial. Acta Neurol Scand. 2016;133:30–40.
Shevil E, Finlayson M. Pilot study of a cognitive intervention program for persons with multiple sclerosis. Health Educ Res. 2010;25:41–53.
Pottgen J, Lau S, Penner I, Heesen C, Moritz S. Managing neuropsychological impairment in multiple sclerosis: pilot study on a standardized metacognitive intervention. Int J MS Care. 2015;17:130–7.
Amato MP, Goretti B, Viterbo RG, Portaccio E, Niccolai C, Hakiki B, et al. Computer-assisted rehabilitation of attention in patients with multiple sclerosis: results of a randomized, double-blind trial. Mult Scler. 2014;20:91–8.
• Bonavita S, Sacco R, Della Corte M, Esposito S, Sparaco M, d'Ambrosio A, et al. Computer-aided cognitive rehabilitation improves cognitive performances and induces brain functional connectivity changes in relapsing remitting multiple sclerosis patients: an exploratory study. J Neurol. 2015;262:91–100 Study reporting improvement in processing speed, attention and memory after twice weekly computerized training at home during 8 weeks. The improvements were paralleled by increased resting-state functional MRI connectivity between the posterior cingulate and bilateral inferior parietal cortex.
Brissart H, Leroy M, Morele E, Baumann C, Spitz E, Debouverie M. Cognitive rehabilitation in multiple sclerosis. Neurocase. 2013;19:553–65.
Campbell J, Langdon D, Cercignani M, Rashid W. A randomised controlled trial of efficacy of cognitive rehabilitation in multiple sclerosis: a cognitive, behavioural, and MRI study. Neural Plast. 2016;2016:4292585.
Cerasa A, Gioia MC, Valentino P, Nisticò R, Chiriaco C, Pirritano D, et al. Computer-assisted cognitive rehabilitation of attention deficits for multiple sclerosis: a randomized trial with fMRI correlates. Neurorehabil Neural Repair. 2013;27:284–95.
Charvet LE, Yang J, Shaw MT, Sherman K, Haider L, Xu J, et al. Cognitive function in multiple sclerosis improves with telerehabilitation: results from a randomized controlled trial. PLoS One. 2017;12:e0177177.
De Giglio L, et al. A low-cost cognitive rehabilitation with a commercial video game improves sustained attention and executive functions in multiple sclerosis: a pilot study. Neurorehabil Neural Repair. 2015;29:453–61.
Hancock LM, Bruce JM, Bruce AS, Lynch SG. Processing speed and working memory training in multiple sclerosis: a double-blind randomized controlled pilot study. J Clin Exp Neuropsychol. 2015;37:113–27.
Janssen A, Boster A, Lee H, Patterson B, Prakash RS. The effects of video-game training on broad cognitive transfer in multiple sclerosis: a pilot randomized controlled trial. J Clin Exp Neuropsychol. 2015;37:285–302.
Mantynen A, et al. Neuropsychological rehabilitation does not improve cognitive performance but reduces perceived cognitive deficits in patients with multiple sclerosis: a randomised, controlled, multi-Centre trial. Mult Scler. 2014;20:99–107.
Mattioli F, Stampatori C, Zanotti D, Parrinello G, Capra R. Efficacy and specificity of intensive cognitive rehabilitation of attention and executive functions in multiple sclerosis. J Neurol Sci. 2010;288:101–5.
Perez-Martin MY, Gonzalez-Platas M, Eguia-Del Rio P, Croissier-Elias C, Jimenez Sosa A. Efficacy of a short cognitive training program in patients with multiple sclerosis. Neuropsychiatr Dis Treat. 2017;13:245–52.
Stuifbergen AK, Becker H, Perez F, Morison J, Kullberg V, Todd A. A randomized controlled trial of a cognitive rehabilitation intervention for persons with multiple sclerosis. Clin Rehabil. 2012;26:882–93.
Leeuwis AE, et al. Design of the ExCersion-VCI study: the effect of aerobic exercise on cerebral perfusion in patients with vascular cognitive impairment. Alzheimers Dement. 2017;3:157–65.
Lauenroth A, Ioannidis AE, Teichmann B. Influence of combined physical and cognitive training on cognition: a systematic review. BMC Geriatr. 2016;16:141.
Briken S, Gold SM, Patra S, Vettorazzi E, Harbs D, Tallner A, et al. Effects of exercise on fitness and cognition in progressive MS: a randomized, controlled pilot trial. Mult Scler. 2014;20:382–90.
Hoang P, Schoene D, Gandevia S, Smith S, Lord SR. Effects of a home-based step training programme on balance, stepping, cognition and functional performance in people with multiple sclerosis--a randomized controlled trial. Mult Scler. 2016;22:94–103.
Sandroff BM, Balto JM, Klaren RE, Sommer SK, DeLuca J, Motl RW. Systematically developed pilot randomized controlled trial of exercise and cognition in persons with multiple sclerosis. Neurocase. 2016;22:443–50.
Sangelaji B, Estebsari F, Nabavi SM, Jamshidi E, Morsali D, Dastoorpoor M, et al. The effect of exercise therapy on cognitive functions in multiple sclerosis patients: a pilot study. Med J Islam Repub Iran. 2015;29:205.
Sumowski JF, Chiaravalloti N, DeLuca J. Retrieval practice improves memory in multiple sclerosis: clinical application of the testing effect. Neuropsychology. 2010;24:267–72.
Foroughi CK, Monfort SS, Paczynski M, PE MK, Greenwood PM. Placebo effects in cognitive training. Proc Natl Acad Sci U S A. 2016;113:7470–4.
Mishra J, Anguera JA, Gazzaley A. Video games for neuro-cognitive optimization. Neuron. 2016;90:214–8.
Green CS, Bavelier D. Exercising your brain: a review of human brain plasticity and training-induced learning. Psychol Aging. 2008;23:692–701.
•• Anguera JA, Boccanfuso J, Rintoul JL, Al-Hashimi O, Faraji F, Janowich J, et al. Video game training enhances cognitive control in older adults. Nature. 2013;501:97–101 A series of experiments demonstrates that adapative video games can improve cognitive control even in older individuals, and establishes a novel approach to cognitive remediation through videogames.
Mishra J, de Villers-Sidani E, Merzenich M, Gazzaley A. Adaptive training diminishes distractibility in aging across species. Neuron. 2014;84:1091–103.
deBettencourt MT, Cohen JD, Lee RF, Norman KA, Turk-Browne NB. Closed-loop training of attention with real-time brain imaging. Nat Neurosci. 2015;18:470–5.
Gao Y, Mandryk R. The acute cognitive benefits of casual exergame play. Proceedings of the 2012 ACM annual conference on Human Factors in Computing Systems. 2012;12:1863.
Maillot P, Perrot A, Hartley A. Effects of interactive physical-activity video-game training on physical and cognitive function in older adults. Psychol Aging. 2012;27:589–600.
Desjardins-Crepeau L, Berryman N, Fraser S, Vu TTM, Kergoat MJ, Li K, et al. Effects of combined physical and cognitive training on fitness and neuropsychological outcomes in healthy older adults. Clin Interv Aging. 2016;11:1287–99.
Filippi M, Rocca MA, Benedict RHB, DeLuca J, Geurts JJG, Rombouts SARB, et al. The contribution of MRI in assessing cognitive impairment in multiple sclerosis. Neurology. 2010;75:2121–8.
Rocca MA, Battaglini M, Benedict RHB, de Stefano N, Geurts JJG, Henry RG, et al. Brain MRI atrophy quantification in MS: from methods to clinical application. Neurology. 2017;88:403–13.
Weiskopf N, Suckling J, Williams G, Correia MM, Inkster B, Tait R, et al. Quantitative multi-parameter mapping of R1, PD(*), MT, and R2(*) at 3T: a multi-center validation. Front Neurosci. 2013;7:95.
Sokolov AA, et al. Linking structural and effective brain connectivity: structurally informed parametric empirical Bayes (si-PEB). submitted.
Enzinger C, Pinter D, Rocca MA, de Luca J, Sastre-Garriga J, Audoin B, et al. Longitudinal fMRI studies: exploring brain plasticity and repair in MS. Mult Scler. 2016;22:269–78.
Hubacher M, et al. Case-based fMRI analysis after cognitive rehabilitation in MS: a novel approach. Front Neurol. 2015;6:78.
Sokolov AA, Miall RC, Ivry RB. The cerebellum: adaptive prediction for movement and cognition. Trends Cogn Sci. 2017;21:313–32.
Romascano D, Meskaldji DE, Bonnier G, Simioni S, Rotzinger D, Lin YC, et al. Multicontrast connectometry: a new tool to assess cerebellum alterations in early relapsing-remitting multiple sclerosis. Hum Brain Mapp. 2015;36:1609–19.
Grimaldi G, Argyropoulos GP, Boehringer A, Celnik P, Edwards MJ, Ferrucci R, et al. Non-invasive cerebellar stimulation--a consensus paper. Cerebellum. 2014;13:121–38.
Xia Z, et al. Modeling disease severity in multiple sclerosis using electronic health records. PLoS One. 2013;8:e78927.
Bove R, et al. Evaluation of an online platform for multiple sclerosis research: patient description, validation of severity scale, and exploration of BMI effects on disease course. PLoS One. 2013;8:e59707.
Bove R, et al. Evaluating more naturalistic outcome measures: a 1-year smartphone study in multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2015;2:e162.
Thaut MH, Peterson DA, McIntosh GC, Hoemberg V. Music mnemonics aid verbal memory and induce learning - related brain plasticity in multiple sclerosis. Front Hum Neurosci. 2014;8:395.
Funding
This work was supported by fellowships from the Leenaards Foundation and the Baasch-Medicus Foundation, a Clinical Medicine Plus scholarship from the Dr. Max Cloëtta Foundation and the Uniscientia Foundation Vaduz, and a grant from the Helmut Horten Foundation to A.A.S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Riley Bove reports grants from Akili Interactive, personal fees from Roche Genentech, personal fees from Genzyme Sanofi, personal fees from Novartis, outside the submitted work. Arseny A. Sokolov reports fellowships from the Leenaards Foundation, from the Dr. Max Cloëtta Foundation and the Uniscientia Foundation Vaduz, from the Baasch-Medicus Foundation, and a grant from the Helmut Horten Foundation during the conduct of the study. Petr Grivaz declares no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Multiple Sclerosis and Related Disorders
Rights and permissions
About this article
Cite this article
Sokolov, A.A., Grivaz, P. & Bove, R. Cognitive Deficits in Multiple Sclerosis: Recent Advances in Treatment and Neurorehabilitation. Curr Treat Options Neurol 20, 53 (2018). https://doi.org/10.1007/s11940-018-0538-x
Published:
DOI: https://doi.org/10.1007/s11940-018-0538-x