Abstract
Purpose of review
Cold snare polypectomy (CSP) has been emerging as increasingly popular technique for the removal of colorectal polyps with expanding indications with regard to larger polyps. We reviewed the recent literature to provide an overview of the indications, outcomes, and recent developments in the field of CSP.
Recent findings
There are currently 2 major guidelines recommending the use of CSP for 1–9 mm polyps, with one guideline suggesting its use for 10–19 mm polyps. There have been more than 30 published studies reporting on CSP outcomes in various patient populations, mostly in 1–9 mm polyps. Research suggests that CSP is safe and effective for the resections of 1–9 mm polyps, although its safety superiority over hot snare polypectomy (HSP) is not as clear except for patients on anticoagulation and antithrombotic medication. Data on CSP in 10–19 mm polyps is currently lacking; however, some research suggests higher incomplete resection compared to HSP. There is limited data suggesting that CSP could be non-inferior to HSP for 10–15 mm polyps and that hot endoscopic mucosal resection (EMR) could be superior to CSP for larger polyps with regard to recurrence risks. Cold EMR has been emerging as a potentially safe and effective tool for the resection of ≥ 20 mm sessile serrated lesions (SSLs); however, the potentially associated recurrence risk (especially for adenomas) requires further investigation in research studies.
Summary
CSP can be used safely and effectively in 1–9 mm polyps. There is a lack of data on the efficacy and safety of CSP over HSP and conventional EMR for polyps 10–19 mm. Cold EMR seems to be effective and safe in the resection of ≥ 20 mm SSLs. More research is needed to expand the indications of CSP for its use in routine endoscopic removal of ≥ 10 mm polyps.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colonoscopy-based screening and surveillance aim to reduce the morbidity and mortality associated with colorectal cancer (CRC). [1, 2] An estimated 2–9% of CRC occur post-colonoscopy, with 14–21% of polyps incompletely resected and 20–30% of interval CRC attributable to incomplete resection. [3•, 4, 4, 6, 7, 8, 9, 10, 11, 12, 13] Considerable resources have therefore been expended to perfect polypectomy efficacy to reduce incomplete polyp resection. Methods such as hot and cold biopsy forceps, hot snare polypectomy (HSP), and endoscopic mucosal resection (EMR) have been utilized with varying efficacy to treat colonic polyps. [3•] Cold snare polypectomy (CSP) is one such method, introduced in the 1990s but did not initially come into widespread use, with other methods such as biopsy excision and HSP dominating routine polypectomy practice. [14] Within the last decade, CSP has seen increased use gaining traction amongst endoscopists for its theoretical potential to reduce transmural injury and complications compared to hot snare. Recently, CSP has been the subject of prolific research looking to expand its indication for larger polyp sizes, utilizing newer dedicated snares, and testing adjunct EMR style techniques. With the recent advances in CSP, current research aims towards replacing HSP for most indications and strives towards routine implementation in clinical practice for most polypectomy situations.
The purpose of this review is to provide an overview of the current state of CSP in the colon, including indications, society recommendations, and optimal technique.
Available devices
Devices for cold polypectomy are divided into dedicated and non-dedicated cold snares. There are currently 4 currently available dedicated cold snares. The largest diameter for snare loops available is 15 mm which limits the ability for en bloc resection of large polyps. Currently, only one dedicated cold snare can also be used with electrocautery, allowing for hybrid cold/hot techniques (Table 1). There are multiple published studies evaluating the performance of traditional snares compared to dedicated hot snares. One study found no difference in IRR, while 2 studies found significantly lower IRR when using dedicated snares.[15, 16, 17] There was no difference in adverse event rates when using traditional snares versus dedicated cold snares. One study found 99.4% success rates when using dedicated snares for CSP of 1–10 mm polyps [18]. Dedicated snares therefore offer an effective and safe alternative to traditional cold snares.
Society recommendations
Society recommendations are summarized in Table 2. Two major European and North American guidelines have suggested optimal resection methods for polyps of different sizes. Ensuring implementation of these guidelines is crucial to reducing IRRs as uptake of other published guidelines has historically been low. [19]
European Society of Gastrointestinal Endoscopy (ESGE)
The ESGE has published guidelines in 2017 recommending the best practice methods for polypectomy based on polyp size. [20••] For 1–5 mm sessile or flat polyps, CSP was recommended as first-line therapy with the option to use cold forceps for 1–3 mm polyps that are difficult to resect with CSP. The ESGE cited high complete resection rates, low complication rates, and the avoidance of adverse events associated with thermal electrocautery as the basis for this recommendation. For 6–9 mm polyps, snare polypectomy was recommended over forceps, specifically citing CSP as preferred for its better safety profile. Although the ESGE stated that comparison with HSP in terms of safety was lacking. For 10–19 mm polyps, HSP with or without submucosal injection was the preferred recommended technique; however, the ESGE stated that there may be a role for piecemeal CSP resection in certain situations to reduce risks of deep thermal injury. CSP did not have a role to play for the resection of ≥ 20 mm polyps according to the guidelines.
United States Multi-Society Task Force (USMSTF)
The USMSTF has published recommendations for preferred polypectomy methods in 2020. [21••] For 1–5 mm sessile or flat polyps, the USMSTF recommended CSP as mainstay therapy with the possibility to use cold jumbo or high-capacity forceps for 1–2 mm polyps that are potentially difficult to resect with CSP. For 6–9 mm polyps, CSP was recommended over HSP due to its high complete resection rates and safety profile. For 10–19 mm polyps, the USMSTF did not state any preference between the use of CSP or HSP, citing that both methods could be used. Polypectomy could also be performed with or without submucosal injection. No justification for the recommendation of the use of CSP in 10–19 mm polyps was provided in the guidelines; however, the recommendation was conditional, citing low-quality evidence. CSP did not have a role to play for the resection of ≥ 20 mm polyps according to the guidelines.
Incomplete resection and local recurrence
The complete resection of colorectal polyps is a crucial part of performing a high-quality colonoscopy as incomplete resection can be associated with polyp recurrence and CRC. [6, 22] The use of proven and effective polypectomy methods is therefore important to reduce incomplete resection rates (IRRs). Studies have shown that the IRR of polyps 1–20 mm is around 14% with increased IRR for larger polyp sizes and specific polypectomy techniques. [3•] To be used in routine clinical practice, CSP should perform equal to or better than other polypectomy techniques for this quality metric. There have been multiple studies evaluating IRRs of CSP for varying polyp sizes, with most studies performed for polyps 1–10 mm (Table 3). [15, 16, 18, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53] Different methods such as visual inspection, evaluating polyp margins, and biopsy of resection sites have been used to determine IRRs.[54] With the emergence of optical diagnosis–based strategies including diagnose-and-leave or simplified polyp surveillance strategies, ensuring complete resection of all polyps is important as patients could potentially undergo surveillance later than otherwise recommended by pathology, or advanced polyps could be potentially left in place. [55, 56, 57]
Polyps 1 to 9 mm
Incomplete resection of small (< 10 mm) and diminutive (< 5 mm) polyps has potentially less severe consequences when compared with larger polyps, as the risk of advanced histology is low. One study found a 0.8% advanced histology rate in this polyp category compared with 15% for ≥ 10 mm polyps. [58] However, with post-polypectomy surveillance trending towards longer intervals, incompletely resecting an adenoma leaves the theoretical potential for recurrence or neoplastic transformation given enough time. [59] Polypectomy for small and diminutive polyps should therefore strive to reduce IRR as much as possible. The American Gastroenterological Association (AGA) has recently cited the use of CSP for all polyps 3–9 mm as part of their colonoscopy best practice recommendations. [60] This is consistent with major European and American society recommendations. [20••, 21••] CSP has been shown to be superior to cold forceps for the resection of 1–5 mm polyps, with the cut-off of superiority likely around the 3 mm mark. [3•] For polyps 1–2 mm, large-capacity forceps could conceivably be used; however, these still often require more than one bite to completely remove small polyps, and the defects created after the first bite could render complete polypectomy difficult. [61] Forceps polypectomy shows high IRR for the resection of small and diminutive polyps; therefore, endoscopists should prioritise CSP when possible. [21••] Comparison of CSP to HSP for 1–9 mm polyps has shown no statistically significant difference in terms of IRR. [3•] A meta-analysis found a 14.2% IRR when HSP was used and 17.3% IRR for CSP.[3•] HSP and CSP are therefore both feasible options when resecting 1–9 mm polyps, and endoscopists can favour CSP over HSP if worries over electrocautery-related adverse events arise.
Polyps 10 to 19 mm
While 10–19 mm polyps have traditionally been resected with hot snares, recent society recommendations promoting the use of CSP as an alternative to HSP have sparked an increase in the use of cold snaring. [21••] Prior to the USMSTF guidelines, an international survey showed that 92.5% of endoscopists used HSP routinely, with only 4.6% using CSP. [62] 87.5% of surveyed endoscopists however have reported increased use of CSP over the last 5 years. Despite these new recommendations, relatively few studies have looked at IRRs and LRRs for polyps 10–19 mm. A recent meta-analysis published in 2020 found a 21% IRR for polyps 10–19 mm resected with hot snare, but cited that there were insufficient studies to estimate CSP IRRs for these polyp sizes. [3•] Since then, one study found a 15.5% IRR for cold snare resection of polyps 10–19 mm; however, this rose to 31% for the 16–19 mm subgroup. [50] Other studies showed much higher IRRs for these polyp sizes (35–45%) [44, 48]. It is important to determine the efficacy of CSP in this polyp size category as these polyps have increased potential of harbouring advanced pathology when compared with polyps < 10 mm. However, data on the efficacy of cold resection of intermediate polyp sizes is still lacking in the literature, and therefore this technique should be left in the hands of experienced endoscopists pending further research. Further studies are also needed to evaluate the role of cold EMR and the possible application of cold snare resection without submucosal injection exclusively in the 10–15 mm subgroup. The USMSTF currently recommends either CSP or HSP for these polyp sizes [21••]. These recommendations are very likely to change within the next years once further evidence is published detailing whether or not CSP is effective and safe for 10–19 mm polyps.
Polyps 20 mm or larger
HSP, EMR, and endoscopic submucosal dissection (ESD) have traditionally been the mainstay for the resection of ≥ 20 mm polyps. The resection of these polyps can be challenging, and these polyps harbour a high potential for aggressive histology, increasing the consequences of failed or incomplete polypectomy. Traditional cold snares suffer from smaller loop widths compared to hot snares which can render en bloc resection very challenging and increase procedure times. There has recently been increased interest in attempting cold polypectomy in ≥ 20 mm polyps. Studies including polyps ≥ 20 mm have focused on local recurrence rates (LRRs) as primary outcomes instead of IRRs. One study including polyps ≥ 20 mm found lower LRR after resection of sessile serrated lesions (SSLs) (3.6%) compared with tubular adenomas (TAs) (7.5%) and tubulovillous adenomas (TVAs) (14.3%) although this difference was not statistically significant [41]. Another study in ≥ 20 mm polyps found significant differences in recurrence rates based on polyp histology, with 13.3% recurrence for SSLs vs 29.6% for TAs and 52.6% for TVAs [46]. Studies including higher proportions of SSLs report lower proportions of recurrence on follow-up [41, 42, 46]. Studies performed exclusively on SSLs conversely show very low (0–5%) recurrence on follow-up. [40, 45] There therefore seems to be a significant difference in cold resection success for the largest polyps based on histology, with adenomas driving most of the recurrences on follow-up. Most studies used cold EMR for the resection of these polyps, and data on cold snare resection without submucosal injection is lacking. Based on the current data, cold EMR of SSLs seems to be effective in expert hands; however, attempting resection of other polyp histology would not be advised in routine practice outside of clinical trials. Cold EMR of SSLs seems to be exceptionally safe with no studies reporting perforations and very low reported IPB and PPB for the largest polyps. There are currently no head-to-head comparisons between hot and cold EMR for ≥ 20 mm SSLs; however, with the very low LRRs reported for cold EMR, this technique could be considered at the very least non-inferior for SSLs in the hands of expert endoscopists.
Adverse events
There has been growing research on the safety of CSP, with multiple studies showing low bleeding rates and non-existent perforation risks in small polyps. For > 10 mm polyps, a 2019 meta-analysis of 8 studies including polyps found 0.7% intraprocedural bleeding (IPB) rates, 0.5% post-polypectomy bleeding (PPB), 0.6% abdominal pain rate, and no perforation. [63] Multiple studies found very low rates of adverse events even for the resection of ≥ 20 mm polyps, mainly in SSLs (Table 4). [40, 41, 42, 45, 46]
Cold snare versus hot snare
CSP has also been touted as superior to HSP for the theoretical potential of reduced adverse events. Indeed, forgoing electrocautery would eliminate the issue of thermal injury to the submucosal and muscular layers and reduce the risk of perforation. The lack of thermal injury could also reduce the risk of developing ulcerations and subsequent delayed bleeding. Multiple studies have compared adverse events for CSP vs HSP, mostly in 1–10 mm polyps. One small systematic review of polyps 1–10 mm found lower IPB rates for HSP when compared with CSP (OR 0.48) while another study in 10–20 mm polyps found that the opposite was true. [64, 65] Multiple other studies directly comparing HSP to CSP did not find significant differences in IPB (Table 4). Intraprocedural bleeding can be immediately addressed during endoscopy and does not represent as severe of a complication as delayed bleeding or perforation. One study found lower rates of delayed or severe bleeding after implementation of CSP in a screening cohort. [66] Two studies similarly found decreased PPB for CSP compared to HSP while 6 others did not (Table 4). All studies directly comparing CSP to HSP found no perforations in both groups, except for 2 perforations for hot EMR in SSLs ≥ 20 mm in one study. [45] Direct comparisons of adverse event rates between CSP and HSP for larger polyp size categories are lacking; however, CSP seems to be generally safe. While forgoing electrocautery might theoretically reduce perforation rates, there is currently conflicting data on the superiority of CSP over HSP in terms of reduction of adverse events for 1–9 mm polyps. More studies with head-to-head comparisons need to be performed to answer this clinical question, especially for polyps 10 mm or larger (Table 5).
Safety with anticoagulation and antithrombotic therapy
An important clinical question is the safety of performing polypectomy in patients undergoing endoscopy with polypectomy on anticoagulation or antithrombic therapy. The risk and benefits of discontinuing therapy should be explained to patients and polypectomy techniques should be tailored when discontinuation is not possible. CSP has recently been emerging as a possible alternative to HSP to forego the need for discontinuation of therapy while minimising bleeding risk. A RCT in 1–9 mm polyps comparing CSP with warfarin or direct oral anticoagulant found that this strategy was non-inferior to HSP with heparin bridging for polypectomy-related major bleeding. [67] This could potentially allow for the continuation of oral anticoagulation if CSP is undertaken. CSP was also found to cause less intraprocedural (6% vs 23%) and post-procedural (0% vs 14%) bleeding when compared with conventional polypectomy in a small cohort of high-risk patients on anticoagulation. [68] Two studies also found low bleeding risk after CSP in patients taking antithrombotic agents. [69, 70] Current data seems to favour CSP as the optimal choice to reduce bleeding risk in high-risk patients with 1–9 mm polyps; however, there is a distinct lack of data for safety in larger polyp sizes. More research needs to be performed in the 10–19 mm and ≥ 20 mm categories to demonstrate safety of CSP in high-risk patients.
Resection technique
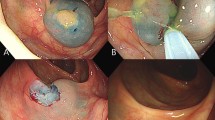
Resection of polyps using cold snares follows different principles than with HSP (Fig. 1). The polyp should be placed at a 5 or 6 o’clock position and the tip of the snare should be anchored several millimetres distal to the polyp and the scope angled down into the colonic wall while the snare is pushed forward. After anchoring, the snare wire should be closed to trap a few millimetres of healthy tissue margin. The snare is then closed in a continuous maneuver to completely cut the polyp and its healthy margin. [17] The polyp can be retracted close to the working channel before transection to ensure immediate retrieval of the specimen. The resection defect is then examined for residual lesion and additional cold snaring is performed until complete visual eradication of all polyp tissue. CSP can lead in some cases to cold snare defect protrusions (CSDP) with larger polyps at a higher risk for CSDP. [71] These protrusions do not generally show residual polyp on biopsy studies and contain submucosa or muscularis mucosa. [72] The clinical significance of these findings is as of yet unclear.
CSP can also be combined with submucosal injection in an EMR style technique for polyp resection. Cold EMR has not been extensively studied or compared to CSP but shows some promise. One RCT showed higher IRR for cold snare resection of polyps 6–20 mm when compared with cold EMR (19.4% vs 5.9%) with the highest difference observed for polyps 16–20 mm (53.1% vs 14.3%). [50] Hot EMR showed similar IRRs for polyps 16–20 mm in that study (8.9%). Cold EMR has been almost exclusively used in ≥ 20 mm polyps and no data comparing it to standard CSP is currently available. More research needs to be performed to establish cold EMR efficacy when compared with CSP or standard EMR especially for polyps ≥ 16 mm. With the emerging studies on very local recurrence rates for large polyps resected with hot EMR and systematic margin ablation, the place of cold EMR for large polyps is even more unclear. [73, 74] Cold EMR has potentially higher LRR when compared to hot EMR, and the benefits of cold EMR with margin ablation are unclear; however, this could potentially reduce the potential benefits of cold EMR with regards to adverse events rates. Currently, hot EMR with margin ablation should be considered the optimal polypectomy method for polyps 20 mm or larger with cold EMR potentially used for large SSLs.
Discussion
The current practice in endoscopy tends towards the increased use of cold methods to achieve optimal polypectomy success while reducing adverse events rates. CSP has been emerging as a safe and effective technique for the removal of colorectal polyps. Current guidelines recommend the use of CSP exclusively for polyps 1–9 mm and recommend the use of CSP as well as HSP for polyps 10–19 mm. Incomplete resection rates are important quality metrics that need to be followed to reduce potential interval CRC. Reducing IRRs by using the most optimal polypectomy method is therefore crucial. Current research favours the use of CSP for 1–9 mm polyps as it is superior to forceps polypectomy in terms of IRRs and non-inferior to HSP. For larger-sized polyps, the current literature does not support the routine use of CSP as of yet, there are indications that CSP could offer similar efficacy to HSP in 10–19 mm polyps, particularly for the 10–15 mm subgroup. Data on CSP in 10–19 mm polyps is scarce and more research is needed in that area. For the largest of polyps, there is emerging data that CSP can be extremely safe and effective specifically for SSLs. The avoidance of electrocautery-related adverse events could prove to be very advantageous for the resection of ≥ 20 mm polyps. However, the resection of ≥ 20 mm adenomas should currently not be attempted with cold snares due to limited data showing high (20–30%) rates of recurrence. As not all incompletely resected polyps recur on follow-up colonoscopy, it is safe to assume that IRRs for non-SSL ≥ 20 mm polyps using cold EMR are much higher than 30%. Cold EMR is an emerging technique that shows promise in the resection of ≥ 16 mm polyps. Published data is currently lacking to formally recommend its use over CSP; however, with the success of hot EMR with systematic margin ablation, it is likely that cold EMR will be reserved for polyps 1–19 mm except for the resection of ≥ 20 mm SSLs.
The current literature on adverse events shows that the superiority of CSP over HSP in terms of reduction of adverse events is currently unclear. The paradigm of the safety of CSP does not seem to be as evident in the literature for small polyps. There is however data on the safety of CSP in patients on anticoagulation or antithrombic medication. CSP should therefore be favoured in that population when possible. Research on adverse event rates in 10–19 mm polyps is lacking; however, it is possible that the improved safety profile of CSP could be more evident in larger polyps at a higher risk of bleeding and perforation. The research field in CSP is currently thriving, with many questions still unanswered for how and when to implement CSP safely and effectively within colonoscopy programs.
Conclusion
CSP seems effective and safe for 1–9 mm polyps, especially for patients under active anticoagulation. More studies are required to expand the implementation of CSP and prove its safety over HSP in larger polyps. Cold EMR is an emerging technique that needs further study in larger polyps to prove efficacy when compared to HSP and conventional EMR with margin ablation, especially for adenomas ≥ 20 mm.
Abbreviations
- AGA:
-
American Gastroenterological Association
- CRC:
-
Colorectal cancer
- CSP:
-
Cold snare polypectomy
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- ESGE:
-
European Society of Gastrointestinal Endoscopy
- HSP:
-
Hot snare polypectomy
- IRR:
-
Incomplete resection rate
- IPB:
-
Intraprocedural bleeding
- LR:
-
Local recurrence rate
- SSL:
-
Sessile serrated lesion
- TA:
-
Tubular adenoma
- TVA:
-
Tubulovillous adenoma
- USMSTF:
-
United States Multi-Society Task Force
References
Papers of particular interest, published recently, have been highlighted as: • of importance •• of major importance
Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–96.
Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–81.
Djinbachian R, Iratni R, Durand M, et al. Rates of incomplete resection of 1- to 20-mm colorectal polyps: a systematic review and meta-analysis. Gastroenterology. 2020 159:904-914.e12 Systematic Review and meta-analysis on IRRs for 1-20mm polyps and factors associated with incomplete resection
Robertson DJ, Lieberman DA, Winawer SJ, et al. Colorectal cancers soon after colonoscopy: a pooled multicohort analysis. Gut. 2014;63:949–56.
Farrar WD, Sawhney MS, Nelson DB, et al. Colorectal cancers found after a complete colonoscopy. Clin Gastroenterol Hepatol. 2006;4:1259–64.
Tollivoro TA, Jensen CD, Marks AR, et al. Index colonoscopy-related risk factors for postcolonoscopy colorectal cancers. Gastrointest Endosc. 2019;89:168-176.e3.
Kim KO, Huh KC, Hong SP, et al. Frequency and characteristics of interval colorectal cancer in actual clinical practice: a KASID multicenter study. Gut Liver. 2018;12:537–43.
Samadder NJ, Curtin K, Tuohy TMF, et al. Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology. 2014;146:950–60.
J Adler D Toy JC Anderson et al 2019 Metachronous neoplasias arise in a higher proportion of colon segments from which large polyps were previously removed, and can be used to estimate incomplete resection of 10–20 mm colorectal polyps. Clin Gastroenterol Hepatol
Bressler B, Paszat LF, Chen Z, et al. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterol. 2007;132:96–102.
Morris EJ, Rutter MD, Finan PJ, et al. Post-colonoscopy colorectal cancer (PCCRC) rates vary considerably depending on the method used to calculate them: a retrospective observational population-based study of PCCRC in the English National Health Service. Gut. 2015;64:1248–56.
Adler J, Robertson DJ. Interval colorectal cancer after colonoscopy: exploring explanations and solutions. Am J Gastroenterol. 2015;110:1657–64.
Rutter MD, Beintaris I, Valori R, et al. World endoscopy organization consensus statements on post-colonoscopy and post-imaging colorectal cancer. Gastroenterol. 2018;155:909-925 e3.
Tappero G, Gaia E, De Giuli P, et al. Cold snare excision of small colorectal polyps. Gastrointest Endosc. 1992;38:310–3.
Dwyer JP, Tan JYC, Urquhart P, et al. A prospective comparison of cold snare polypectomy using traditional or dedicated cold snares for the resection of small sessile colorectal polyps. Endosc International Open. 2017;5:E1062–8.
Horiuchi A, Hosoi K, Kajiyama M, et al. Prospective, randomized comparison of 2 methods of cold snare polypectomy for small colorectal polyps. Gastrointest Endosc. 2015;82:668–75.
J Roberts J Anderson H Pohl 2018 Safety and efficacy of dedicated cold versus standard snares: 488. Official journal of the American College of Gastroenterology | ACG 113:S281-S282.
Schett B, Wallner J, Weingart V, et al. Efficacy and safety of cold snare resection in preventive screening colonoscopy. Endosc Int Open. 2017;5:E580–6.
Djinbachian R, Dube AJ, Durand M, et al. Adherence to post-polypectomy surveillance guidelines: a systematic review and meta-analysis. Endosc. 2019;51:673–83.
Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017; 49:270-297Major European guideline recommending best practices for polypectomyMajor European guideline recommending best practices for polypectomy
Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic removal of colorectal lesions— recommendations by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2020;158:1095-1129. Major American guideline recommending best practices for polypectomy
Pohl H, Anderson JC, Aguilera-Fish A, et al. Recurrence of colorectal neoplastic polyps after incomplete resection. Annals of Internal Medicine 2021.
Lee CK, Shim JJ, Jang JY. Cold snare polypectomy vs. cold forceps polypectomy using double-biopsy technique for removal of diminutive colorectal polyps: a prospective randomized study. Am J Gastroenterol. 2013;108:1593–600.
Pohl H, Srivastava A, Bensen SP, et al. Incomplete polyp resection during colonoscopy - results of the complete adenoma resection (CARE) study. Gastroenterology. 2013;144:74-80.e1.
Din S, Ball AJ, Riley SA, et al. A randomized comparison of cold snare polypectomy versus a suction pseudopolyp technique. Endoscopy. 2015;47:1005–10.
Gomez V, Badillo RJ, Crook JE, et al. Diminutive colorectal polyp resection comparing hot and cold snare and cold biopsy forceps polypectomy Results of a pilot randomized single-center study (with videos). Endosc Int Open. 2015;3:76–80.
Kim JS, Lee BI, Choi H, et al. Cold snare polypectomy versus cold forceps polypectomy for diminutive and small colorectal polyps: a randomized controlled trial. Gastrointest Endosc. 2015;81:741–7.
Park SK, Ko BM, Han JP, et al. A prospective randomized comparative study of cold forceps polypectomy by using narrow-band imaging endoscopy versus cold snare polypectomy in patients with diminutive colorectal polyps. Gastrointestinal Endosc. 2016;83:527-532.e1.
Hirose R, Yoshida N, Murakami T, et al. Histopathological analysis of cold snare polypectomy and its indication for colorectal polyps 10–14 mm in diameter. Dig Endosc. 2017;29:594–601.
Komeda Y, Kashida H, Sakurai T, et al. Removal of diminutive colorectal polyps: a prospective randomized clinical trial between cold snare polypectomy and hot forceps biopsy. World J Gastroenterol. 2017;23:328–35.
Matsuura N, Takeuchi Y, Yamashina T, et al. Incomplete resection rate of cold snare polypectomy: a prospective single-arm observational study. Endoscopy. 2017;49:251–7.
Chien N-H, Ni M-H, Huang S-H, et al. Cold snare polypectomy vs cold forceps biopsy in endoscopic treatment of colonic small and diminutive polyps—effectiveness and safety in the real world. Advances in Digestive Medicine. 2018;5:127–31.
Hasegawa H, Bamba S, Takahashi K, et al. Efficacy and safety of cold forceps polypectomy utilizing the jumbo cup: a prospective study. Intest Res 2018.
Kawamura T, Takeuchi Y, Asai S, et al. A comparison of the resection rate for cold and hot snare polypectomy for 4–9 mm colorectal polyps: a multicentre randomised controlled trial (CRESCENT study). Gut. 2018;67:1950–7.
Maruoka D, Arai M, Akizue N, et al. Residual adenoma after cold snare polypectomy for small colorectal adenomas: a prospective clinical study. Endoscopy. 2018;50:693–700.
Papastergiou V, Paraskeva KD, Fragaki M, et al. Cold versus hot endoscopic mucosal resection for nonpedunculated colorectal polyps sized 6–10 mm: a randomized trial. Endosc. 2018;50:403–11.
Tutticci NJ, Hewett DG. Cold EMR of large sessile serrated polyps at colonoscopy (with video). Gastrointest Endosc. 2018;87:837–42.
Zhang Q, Gao P, Han B, et al. Polypectomy for complete endoscopic resection of small colorectal polyps. Gastrointest Endosc. 2018;87:733–40.
Desai S, Gupta S, Copur-Dahi N, et al. A prospective randomized study comparing jumbo biopsy forceps to cold snare for the resection of diminutive colorectal polyps. Surg Endosc 2019.
Huh CW, Kim JS, Choi HH, et al. Jumbo biopsy forceps versus cold snares for removing diminutive colorectal polyps: a prospective randomized controlled trial. Gastrointestinal Endosc 2019.
Mangira D, Cameron K, Simons K, et al. Cold snare piecemeal EMR of large sessile colonic polyps ≥20 mm (with video). Gastrointest Endosc. 2020;91:1343–52.
Piraka C, Saeed A, Waljee AK, et al. Cold snare polypectomy for non-pedunculated colon polyps greater than 1 cm. Endosc Int Open. 2017;05:E184–9.
Arimoto J, Chiba H, Ashikari K, et al. Safety and efficacy of cold snare polypectomy for pedunculated (Ip) polyps measuring less than 10 mm in diameter. Int J Colorectal Dis. 2020;35:859–67.
Yabuuchi Y, Imai K, Hotta K, et al. Efficacy and safety of cold-snare endoscopic mucosal resection for colorectal adenomas 10 to 14 mm in size: a prospective observational study. Gastrointest Endosc. 2020;92:1239–46.
van Hattem WA, Shahidi N, Vosko S, et al. Piecemeal cold snare polypectomy versus conventional endoscopic mucosal resection for large sessile serrated lesions: a retrospective comparison across two successive periods. Gut. 2021;70:1691.
Suresh S, Zhang J, Ahmed A, et al. Risk factors associated with adenoma recurrence following cold snare endoscopic mucosal resection of polyps ≥ 20 mm: a retrospective chart review. Endosc Int Open. 2021;09:E867–73.
Shimodate Y, Itakura J, Takayama H, et al. Impact of submucosal saline solution injection for cold snare polypectomy of small colorectal polyps: a randomized controlled study. Gastrointest Endosc. 2020;92:715-722.e1.
Yoshida N, Inoue K, Tomita Y, et al. Cold snare polypectomy for large sessile serrated lesions is safe but follow-up is needed: a single-centre retrospective study. United Eur Gastroenterol J. 2021;9:370–7.
Barros RA, Monteverde MJ, Dumonceau J-M, et al. Cold snare polypectomy without submucosal injection: safety and efficacy in 615 large serrated lesions. Endosc Int open. 2021;9:E1421–6.
Li D, Wang W, Xie J, et al. Efficacy and safety of three different endoscopic methods in treatment of 6–20 mm colorectal polyps. Scand J Gastroenterol. 2020;55:362–70.
Kimoto Y, Sakai E, Inamoto R, et al. Safety and efficacy of cold snare polypectomy without submucosal injection for large sessile serrated lesions: a prospective study. Clin Gastroenterol Hepatol 2020.
Tate DJ, Awadie H, Bahin FF, et al. Wide-field piecemeal cold snare polypectomy of large sessile serrated polyps without a submucosal injection is safe. Endosc. 2018;50:248–52.
Yamamoto T, Suzuki S, Kusano C, et al. Histological outcomes between hot and cold snare polypectomy for small colorectal polyps. Saudi journal of gastroenterology : official journal of the Saudi Gastroenterology Association. 2017;23:246–52.
Djinbachian R, Renteln DV. Endoscopic polypectomy: how should we determine complete resection status? Clin Gastroenterol Hepatol 2020.
Duong A, Pohl H, Djinbachian R, et al. Evaluation of the polyp-based resect and discard strategy: a retrospective study. Endoscopy 2021.
Taghiakbari M, Pohl H, Djinbachian R, et al. The location-based resect and discard strategy for diminutive colorectal polyps: a prospective clinical study. Endoscopy 2021.
Djinbachian R, Dubé AJ, von Renteln D. Optical diagnosis of colorectal polyps: recent developments. Curr Treat Options Gastroenterol. 2019;17:99–114.
Gupta N, Bansal A, Rao D, et al. Prevalence of advanced histological features in diminutive and small colon polyps. Gastrointest Endosc. 2012;75:1022–30.
Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2020;91:463-485 e5.
Keswani RN, Crockett SD, Calderwood AH. AGA clinical practice update on strategies to improve quality of screening and surveillance colonoscopy: expert review. Gastroenterol. 2021;161:701–11.
Draganov PV, Chang MN, Alkhasawneh A, et al. Randomized, controlled trial of standard, large-capacity versus jumbo biopsy forceps for polypectomy of small, sessile, colorectal polyps. Gastrointest Endosc. 2012;75:118–26.
Willems P, Orkut S, Ditisheim S, et al. An international polypectomy practice survey. Scand J Gastroenterol. 2020;55:497–502.
Thoguluva Chandrasekar V, Spadaccini M, Aziz M, et al. Cold snare endoscopic resection of nonpedunculated colorectal polyps larger than 10 mm: a systematic review and pooled-analysis. Gastrointest Endosc. 2019;89:929-936.e3.
Jegadeesan R, Aziz M, Desai M, et al. Hot snare vs. cold snare polypectomy for endoscopic removal of 4 - 10 mm colorectal polyps during colonoscopy: a systematic review and meta-analysis of randomized controlled studies. Endosc Int Open 2019;7:E708-E716.
Ket SN, Mangira D, Ng A, et al. Complications of cold versus hot snare polypectomy of 10–20 mm polyps: a retrospective cohort study. JGH open : an open access journal of gastroenterology and hepatology. 2019;4:172–7.
Chang L-C, Shun C-T, Hsu W-F, et al. Risk of delayed bleeding before and after implementation of cold snare polypectomy in a screening colonoscopy setting. Endosc Int open. 2019;7:E232–8.
Takeuchi Y, Mabe K, Shimodate Y, et al. Continuous anticoagulation and cold snare polypectomy versus heparin bridging and hot snare polypectomy in patients on anticoagulants with subcentimeter polyps. Ann Intern Med. 2019;171:229–37.
Horiuchi A, Nakayama Y, Kajiyama M, et al. Removal of small colorectal polyps in anticoagulated patients: a prospective randomized comparison of cold snare and conventional polypectomy. Gastrointest Endosc. 2014;79:417–23.
Aizawa M, Utano K, Nemoto D, et al. Risk of delayed bleeding after cold snare polypectomy in patients with antithrombotic therapy. Digestive Diseases and Sciences 2021.
Arimoto J, Chiba H, Ashikari K, et al. Safety of cold snare polypectomy in patients receiving treatment with antithrombotic agents. Dig Dis Sci. 2019;64:3247–55.
Ishii T, Harada T, Tanuma T, et al. Histopathologic features and fragmentation of polyps with cold snare defect protrusions. Gastrointest Endosc. 2021;93:952–9.
Tutticci N, Burgess NG, Pellise M, et al. Characterization and significance of protrusions in the mucosal defect after cold snare polypectomy. Gastrointest Endosc. 2015;82:523–8.
Klein A, Tate DJ, Jayasekeran V, et al. Thermal ablation of mucosal defect margins reduces adenoma recurrence after colonic endoscopic mucosal resection. Gastroenterol. 2019;156:604-613 e3.
Sidhu M, Shahidi N, Gupta S, et al. Outcomes of thermal ablation of the mucosal defect margin after endoscopic mucosal resection: a prospective, international, multicenter trial of 1000 large nonpedunculated colorectal polyps. Gastroenterol. 2021;161:163-170.e3.
Liu S, Ho SB, Krinsky ML. Quality of polyp resection during colonoscopy: are we achieving polyp clearance? Dig Dis Sci. 2012;57:1786–91.
Aslan F, Camcı M, Alper E, et al. Cold snare polypectomy versus hot snare polypectomy in endoscopic treatment of small polyps. Turk J Gastroenterol. 2014;25:279–83.
Yamashina T, Fukuhara M, Maruo T, et al. Cold snare polypectomy reduced delayed postpolypectomy bleeding compared with conventional hot polypectomy: a propensity score-matching analysis. Endosc Int Open. 2017;05:E587–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roupen Djinbachian declares that he has no conflict of interest. Daniel von Renteln is supported by the “Fonds de Recherche du Québec Santé” career development award and has received research funding from ERBE, Ventage, Pendopharm, and Pentax and is a consultant for Boston Scientific and Pendopharm.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Djinbachian, R., von Renteln, D. Cold Snare Resection of Colorectal Polyps: Updates and Recent Developments. Curr Treat Options Gastro 20, 221–237 (2022). https://doi.org/10.1007/s11938-022-00369-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-022-00369-y