Abstract
Purpose of review
Decades have passed since the underlying molecular etiologies of the most common hereditary forms of colorectal cancer (CRC), Lynch syndrome, and familial adenomatous polyposis (FAP) were first described. With the advent of next-generation sequencing (NGS) panels, the landscape of hereditary CRC testing has changed dramatically. We review available screening strategies, novel CRC predisposition genes, and challenges and opportunities in this field.
Recent findings
Improved sensitivity and availability of NGS panel testing have greatly expanded our understanding regarding the number of CRC syndromes and their phenotypic expression. A variety of screening strategies are available to identify heritable CRC syndromes, potentially decreasing morbidity and mortality in this population. However, these screening strategies remain imperfect and present challenges regarding their implementation in clinical practice. Screening strategies include universal screening of CRC tumors for Lynch syndrome, clinical prediction algorithms, and risk assessment questionnaires. Additionally, there remains a gap in our understanding of the clinical implications of novel gene mutations of variable penetrance and unexpected NGS panel test results. Incorporation of single nucleotide polymorphisms (SNPs) may help to further refine cancer risk assessment, and the clinical introduction of RNA analysis may allow us to clarify variants of unknown significance (VUSs) and identify deep intronic mutations that would otherwise be missed.
Summary
Recognition of genetic predisposition to CRC is critical for the practicing gastroenterologist. The evolving field of cancer genetics offers great challenges and opportunities for improved CRC management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incorporating cancer genetic risk assessment into gastroenterology practice provides an excellent opportunity to optimize screening and surveillance strategies for colorectal cancer (CRC). A genetic predisposition to CRC has been recognized for decades, and there are several well-defined hereditary CRC syndromes. Historically, syndrome-specific testing was the standard for detection of highly penetrant familial CRC syndromes [1, 2]. The clinical introduction of non-Sanger-based next-generation sequencing (NGS) panels in early 2012 has greatly enhanced the identification of families with a hereditary predisposition to cancer. Despite increased availability of NGS panels and improved management and outcomes for hereditary CRC syndromes, genetic counseling and testing are often not performed for this indication [3]. This is in contrast to hereditary breast cancer, which has greater public awareness, more providers with genetic expertise, and a better defined systematic approach in identifying affected patients [4].
Among patients diagnosed with CRC, approximately 30% report a family history of CRC [5]. However, only 3–6% of all CRC patients carry identifiable highly penetrant gene mutations associated with hereditary CRC syndromes [6]. As new cancer predisposition genes are discovered, this gap continues to lessen [7]. With decreased cost and increased data made available by NGS, it has become apparent that cancer genes not previously associated with CRC are being detected, expanding the phenotypic spectrum of hereditary CRC. This has led to increased complexity in characterization of these cancer syndromes. The authors of this review will discuss guidelines for CRC genetic risk assessment, available screening tools, referral of high-risk patients, novel CRC-associated genes, and new developments in this field.
Hereditary CRC syndromes
Highly penetrant hereditary CRC syndromes are a well-characterized group of diseases with established inheritance and diagnostic criteria but with variable phenotypes, cancer risk, and management. Some, such as classic familial attenuated polyposis (FAP) in which patients typically present in early adolescence with hundreds to thousands of colorectal polyps, are easily identified. These patients have a 100% reported incidence of CRC if left untreated. Other well-established hereditary CRC syndromes include Lynch syndrome, attenuated FAP, MUTYH-associated polyposis (MAP), Peutz-Jeghers syndrome (PJS), juvenile polyposis syndrome (JPS), Cowden/PTEN hamartoma tumor syndrome, and serrated polyposis syndrome (SPS) [8,9,10].
For the practicing gastroenterologist, characterization and management of these patients are well-described in National Comprehensive Cancer Network (NCCN) guidelines and will not be reviewed here in depth [11••]. Management recommendations, such as early endoscopic surveillance, prophylactic risk-reducing surgery, and chemoprevention have been proven to decrease mortality and prevent cancer in these patients.
Universal tumor testing for lynch syndrome
Lynch syndrome (previously called hereditary nonpolyposis colorectal cancer [HNPCC]) represents the most common hereditary CRC syndrome. It is inherited in an autosomal dominant fashion and accounts for 3% of all CRC cases with a lifetime risk of CRC between 20 and 80% depending on the gene mutation [12]. The clinical criteria for identifying Lynch syndrome, including Amsterdam II criteria and revised Bethesda Guidelines, are cumbersome and lead to lower genetic screening rates in these patients [13]. Furthermore, these clinical criteria fail to recognize between 30 and 50% of Lynch syndrome patients [14, 15]. To improve detection of Lynch syndrome, universal CRC tumor screening for a mismatch repair deficiency (MMR-d) is now recommended. MMR-d is present in approximately 90% of Lynch syndrome-associated CRC tumors [16]. If screening via immunohistochemical (IHC) and/or microsatellite instability (MSI) testing raises concern for Lynch syndrome, referral for genetic counseling and testing is recommended [17]. IHC testing for the four mismatch repair (MMR) proteins (MLH1, MSH2, MSH6, and PMS2) can be carried out in a pathology laboratory whereas DNA testing for MSI must be done in a molecular laboratory. Since results of both screening tests correlate highly with each other, IHC testing for MMR proteins has become more prevalent within universal screening programs. In order to reduce the number of patients with sporadic CRC tumors that must be referred for genetic counseling and testing, additional testing of tumors with absent MLH1 expression is required [8]. The presence of a somatic BRAF mutation in the colon tumor and/or MLH1 hypermethylation significantly lowers the likelihood of Lynch syndrome as these findings typically represent sporadic mechanisms for absent MLH1 expression. As a result, this reflex testing has been incorporated by many universal tumor testing programs.
Utilizing universal CRC tumor screening, 10% of all CRC patients will require further genetic testing for Lynch syndrome. This has been consistently demonstrated across different ethnic groups [18]. Compared to other screening strategies, universal CRC tumor testing has been shown to be an effective screening tool for Lynch syndrome, although it is not the most cost-effective [19]. Guidelines recommend universal tumor testing as well as the use of clinical criteria, but many clinical settings still lack a standardized approach.
Penn State Health embarked on a public health initiative to increase the identification of Lynch syndrome in our patient population. Beginning in May of 2014, all biopsy/surgical specimens containing invasive colorectal adenocarcinoma were screened for Lynch syndrome using IHC staining for the 4 MMR proteins. Patients whose specimens demonstrated absent protein expression for 1 or more of the MMR proteins were contacted by a member of the Cancer Genetics Program and offered an appointment for genetic counseling and testing. As of October 2018, 544 colorectal cancer specimens were screened for Lynch syndrome. Of the 51 (9.4%) specimens that demonstrated abnormal protein expression, 35 (68.6%) patients met with a genetic counselor/geneticist and elected to pursue genetic testing. Of those 35 patients who pursued testing, 9 (25.7%) patients were confirmed to have Lynch syndrome (4 MLH1+, 3 MSH2+, 1 MSH6+, and 1 PMS2+).
A recent study found that up-front tumor sequencing was simpler and had superior sensitivity than current approaches to Lynch syndrome screening, while simultaneously providing critical information for treatment selection [20]. In this study, the tumor sequencing identified KRAS, NRAS, or BRAF mutations that could affect therapy for stage IV CRC, thus helping to avoid another test. In addition, the tumor sequencing had the benefit of identifying patients with germline DPYD mutations which are associated with toxicity to fluorouracil chemotherapy, and thus could be useful for treatment selection.
Risk assessment screening tools
Identifying patients with hereditary CRC syndromes starts with a detailed personal and family history of cancer and premalignant GI conditions [11••]. Once this has been obtained, utilization of the NCCN guidelines can help clinicians assess the need for gene testing (Table 1).
In today’s healthcare environment, it is impractical for gastroenterologists to obtain a comprehensive, 3-generation family history that a genetic counselor would obtain. ACG clinical guidelines recommend a more practical approach to obtaining a CRC and polyp history of first- and second-degree relatives including age of diagnosis(es) [8]. While most gastroenterologists routinely seek personal and family history to risk-stratify patients for changes in screening age or surveillance intervals, genetic cancer risk assessment is often missed. This can have important implications for the patient and family members [21]. This issue is compounded by open-access colonoscopy in which gastroenterologists meet patient just minutes prior to the procedure. The ability of clinicians to determine the cumulative number of neoplastic polyps that a patient has had over time is limited. In attempts to overcome these problems, several different risk assessment tools have been developed to help identify hereditary CRC syndromes.
Clinical prediction algorithms
Clinical prediction algorithms are one type of risk assessment tool. These utilize comprehensive online questionnaires that allow for any individual to calculate the probability that a person carries a Lynch syndrome-associated germline mutation. One example is PREMM5, which calculates an individual’s risk of carrying a mutation in any of the known 4 MMR genes responsible for Lynch syndrome (MLH1, MSH2, MSH6, and PMS2) and/or EPCAM which is upstream of MSH2. PREMM5 incorporates age, gender, and personal and family history of cancer into a clinical prediction algorithm. A recent study found that the previously defined ≥ 5% threshold of these calculators may be inferior to the ≥ 2.5% threshold in the PREMM5 model. This lower threshold increases the number of identified mutation carriers while preserving a high negative predictive value of 99% [22•]. Nonetheless, NCCN guidelines recommend clinical judgment when determining threshold [11••]. Simulation models showed the PREMM5 screening strategy to be cost-effective and decreased the incidence of CRC by 43.9% in patients 25–35 years of age [23]. An earlier version of this prediction model (PREMM1,2,6) was assessed in the community setting utilizing a self-administered electronic tablet version. In addition to detecting 6 new cases of Lynch syndrome in over 3000 patients screened during a 6-month time period, there was high endoscopist and patient satisfaction [24]. This also allows for real-time feedback and incorporation into the patient’s medical record.
Screening questionnaires
Screening questionnaires are a practical type of risk assessment tool. Kastrinos et al. developed and validated a popular 3-question survey that can be incorporated into the pre-procedural evaluation for patients undergoing colonoscopy [25].
Kastrinos 3-question CRC risk assessment tool
-
Do you have a first-degree relative (mother, father, brother, sister, child) with any of the following conditions diagnosed before age 50:
-
Colon or rectal cancer?
-
Cancer of the uterus, ovary, stomach, small intestine, urinary tract (kidney, ureter, bladder), bile ducts, pancreas, or brain?
-
Do you have 3 or more relatives (this includes parents, brothers, sisters, children, grandparents, aunts, uncles, cousins) with a history of colon or rectal cancer?
-
Have you had any of the following conditions diagnosed before age 50:
-
Colon or rectal cancer?
-
Colon or rectal polyps?
Using a statistical analysis method called recursive partitioning analysis, 9 clinical risk factors were ranked based on ability to capture the most high-risk individuals when asked sequentially. This ultimately resulted in the 3-question survey above. The sensitivity was found to be 77%, which was also validated prospectively. In individuals with known Lynch syndrome and MMR gene defects, the survey was able to identify 95% of high-risk patients. A criticism of Kastrinos’s 3-question survey has been its lack of specificity with 20% of patients deemed high-risk and thus potentially warranting cancer genetics referral. A recent survey proposed by Guivatchian et al. included Kastrinos’s 3 question tool plus 1 question incorporating Lynch syndrome-associated cancers and 1 question on the lifetime cumulative polyp number [26••]. The Guivatchian questionnaire found 10% of patients to be high-risk, and of these patients, 10% were found to have heritable genetic mutations. Another study using mailed questionnaires on family history, sent to patients prior to outpatient colonoscopies, increased the number of patients referred to genetic counseling compared to standard of care (3.7% vs. 1.6%) [27]. In-office questionnaires can be completed by nurses with high patient satisfaction [28]. While feasible, the real-world efficacy of identifying germline mutations through questionnaires has been variable with one study identifying 2 germline mutations out of 6031 screened (3.3/10,000) [29].
A similar expanded 5-question version of the Kastrinos risk assessment tool was created and studied at Penn State Health. This expanded questionnaire incorporated 2 additional Lynch syndrome-associated cancer questions [30]. Patients 40 years of age and older in 10 different outpatient primary care sites were surveyed, and 2438 surveys were completed (23% response rate). Of these, 15.7% self-identified as high-risk. Only 31% of high-risk patients ages 40–49 were up-to-date on CRC screening compared to over 80% of average-risk and high-risk adults ≥ 50 years of age. In a subsequent study of Penn State Health employees over 40 years of age using a similar electronic questionnaire, 33.4% (878 individuals) self-identified as high-risk. In sub-group analysis, only 45.8% of high-risk individuals ages 40–49 reported up-to-date CRC screening [31]. Taken together, these two studies document a disparity in screening high-risk younger individuals for hereditary CRC syndromes.
There has also been the development of consumer-oriented CRC risk assessment tools to help patients collect their family history, such as the Office of the Surgeon General’s “My Family Health Portrait” (MFHP) [32]. MFHP has been externally validated with reasonable sensitivity and specificity compared to genetic counselor pedigree review although it is not used by most healthcare systems [33].
Limitations and barriers
There are several limitations and barriers to these various screening strategies. With all of these screening strategies, a great number of patients do not present for genetic counseling, decline testing, or do not follow through with testing [26••, 29, 34]. A limitation specific to PREMM5 is that it was not designed for screening for hereditary CRC syndromes other than Lynch syndrome. Furthermore, several of the screening strategies listed above are designed to be used in endoscopy centers where a patient may not present until 50 years of age. Other barriers to implementation of screening include physician motivation, time constraint, and knowledge. Prior to genetic testing, informed consent should include a discussion on the significance of a “positive” result including its potential psychological implications, the potential for genetic discrimination, and cost [8, 34, 35]. An increase in testing of a proband’s relatives has been noted with many genetics labs offering free testing within 90 days of the index patient’s pathogenic variant finding. While for Lynch syndrome, this cascade testing is recommended for all first-degree relatives 18 years of age or older; this frequently does not occur [36, 37]. There remains no single best way to screen for high-risk individuals for hereditary CRC syndromes, but at a minimum, gastroenterologists should strive to implement syndrome-specific NCCN guideline recommendations (Table 1) [19].
Once high-risk individuals are identified, it is recommended to refer these patients for cancer genetic counseling and testing. In-house referrals are optimal if genetic counselors are on staff, but alternative options exist. In today’s market of web-based services, a genetic counseling professional can be identified by visiting the National Society of Genetic Counselor’s website (www.nsgc.org), and searching for the nearest cancer genetics counselor [38]. Some academic centers have established comprehensive cancer genetics programs that have affiliations with other hospitals and care centers. This allows for broadened involvement in educational and patient care opportunities via videoconference and telemedicine, respectively [4]. If these options are not available, there is a growing number of telephone and web-based genetic counseling services. For clinicians looking for up-to-date and reliable information, a free online resource, GeneReviews®, is also available.
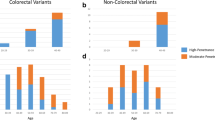
Early onset colorectal cancer
Recent studies looking at the prevalence of germline mutations in patients with CRC diagnosed less than 50 years of age using NGS panels further support the referral of all such cases for genetic counseling and testing. In one study looking at 450 patients with CRC diagnosed under 50 years of age, 72 (16%) were found to have an underlying germline mutation [39]. Overall, 8.4% of the patients were found to have Lynch syndrome while 8% were found to have other hereditary cancer syndromes involving mutations in high-penetrance CRC genes (5 APC; 1 APC/PMS2; 2 biallelic MUTYH; 1 SMAD4), low-penetrance CRC genes (3 APC c.3920 T > A, p.I1307K; 7 monoallelic MUTYH), and high- or moderate-penetrance genes not traditionally associated with CRC (3 ATM; 1 ATM/CHEK2; 2 BRCA1; 4 BRCA2; 1 CDKN2A; 2 PALB2). Importantly, 24 of 72 mutation positive patients (33.3%) did not meet established genetic testing criteria for the gene(s) in which they had a mutation.
Novel CRC predisposition genes
Multi-gene panel testing of cancer predisposition genes through a multitude of commercially available options has allowed for an increased number of genes to be analyzed at a markedly decreased cost. This can be as inexpensive as $250 for 84 genes with a turn-around time of 1–2 weeks [40]. Over the last several years, there has been the discovery of several new genes that may predispose individuals to CRC (Table 2).
These novel genes add to the expanding spectrum and overlap of CRC syndromes (Fig. 1). They have been characterized similarly to other well-described highly penetrant hereditary CRC syndromes based on inheritance patterns, clinical and histopathologic findings, and cellular mechanisms. For example, the polyp phenotype of polymerase proofreading-associated polyposis (PPAP) is similar to that of attenuated FAP. POLE is one of the gene mutations associated with PPAP. Its presence in sporadic tumors has been associated with a favorable prognosis, similar to microsatellite instability (MSI) highlighting the overlap of these genes [44]. Another novel syndrome, hereditary mixed polyposis syndrome (HMPS) associated with GREM1 gene mutation, presents with varied polyp histology and adds to the spectrum of hereditary CRC syndromes [45]. NTHL1- and MUTYH-associated polyposis (NAP and MAP, respectively) are both recessive polyposis syndromes which predispose to other cancer risks as well. The spectrum of benign and malignant tumors, though, in individuals with biallelic NTHL1 mutations appears to be broader [46].
Phenotypic classification of nonpolyposis and polyposis CRC syndromes, mode of inheritance, causal genes, and affected molecular pathways. Note: germline AXIN2 autosomal dominant mutations (Wnt pathway) may cause oligodontia-colorectal cancer syndrome characterized by severe permanent tooth agenesis and the presence of CRC or precancerous colonic or gastric lesions of variable types (adenomas, hyperplastic polyps). Due to the still undefined CRC and polyposis phenotype, it has not been included in the figure. BER, base excision repair; CMMRD, constitutional mismatch repair deficiency; HMPS, hereditary mixed polyposis syndrome; MAP, MUTYH-associated polyposis; MMR, DNA mismatch repair; PPAP, polymerase proofreading-associated polyposis; SPS, serrated polyposis syndrome. Used with permission from John C. Wiley and Sons [41].
The use of NGS technology has resulted in the discovery of novel cancer genes which are now being associated with previously described clinical diagnoses. The diagnosis of serrated polyposis syndrome (SPS) remains dependent on World Health Organization (WHO) clinical criteria, but NGS technology has identified an associated gene, RNF43, albeit at a low mutation frequency [47]. The diagnosis of Familial Colorectal Cancer Type X (FCCTX) requires that families meet Amsterdam criteria, have mismatch repair-proficient (MMR-p) tumors, and lack germline mutations [41]. These families carry a twofold increase in CRC and lack the extracolonic tumors seen in Lynch syndrome. More recently, limited data has shown an association with FCCTX and the RPS20 gene [42•].
Many of these newly described genes are only documented in a limited number of individuals and/or families, which make clinical correlations and optimal management strategies challenging. One recent study concluded that patients with either CHEK2 or APC p.I1307K should start screening for CRC at age 45 and screening for those with monoallelic MUTYH should begin at age 50 [43]. The numerous other hereditary cancer genes not traditionally associated with CRC continue to be investigated with regard to their possible role in CRC. These include ATM, BRCA1, BRCA2, CDKN2A, PALB2, and TP53. The absolute risk of CRC associated with these genes is debated. It is unclear if the data is skewed by background population mutations or pleiotropism (gene manifests itself in a variety of clinical phenotypes) [48, 49]. On the other hand, various gene mutations previously believed to predispose to CRC, such as FANCM, FAN1, BUB1, BUB3, LRP6, and PTPN12, have recently been shown to lack this association [42•]. Other novel candidate genes that appear to play a role as moderate- or low-risk genes have been described including AXIN2, GALNT12, and biallelic MSH3 (Table 2) [50,51,52]. One problem with NGS panels is the absence in consistency of included genes, which points to the current lack of consensus inclusion criteria. In one study of 10 different commercially available NGS panels, only 6 of the well-characterized genes (APC, MLH1, MSH2, MSH6, PMS2, and MUTYH) were consistently included in all 10 panels [53].
Variants of uncertain significance
Results of gene testing return as one of three general possibilities: pathogenic variant, variant of uncertain significance (VUS), or benign variant. VUSs ultimately result in proteins with unclear function (absent, identical, increased, decreased, or altered). With this, cancer risk is unclear, and therefore, VUS carrier results lie on a spectrum from benign to pathogenic. Approximately 20–30% of patients undergoing CRC gene testing will receive a VUS result [54, 55]. Given that a VUS cannot be used to stratify patients into high or low risk, the result cannot be used to guide the medical management of patients and/or their families [38, 55]. If a VUS is found, patients are counseled to follow guidelines based on personal and family history. Unfortunately, though, many physicians misinterpret VUSs as pathogenic variants [56].
New developments
When multi-gene panel testing does not identify a CRC-predisposing mutation, CRC screening is based on personal and family history alone. Through the technology of NGS, genome-wide studies have been able to find single nucleotide polymorphisms (SNPs) that are associated with an increased risk of CRC. A recent study that utilized a 45 SNP panel found that individuals with two first-degree relatives with CRC who were also in the highest risk SNP quintile should undergo CRC screening 16 years earlier compared to average risk adults [57•]. The authors acknowledge the lack of evaluation of cost-effectiveness, resource feasibility, and insurance implications. Another study that used a 63 SNP panel and evaluated lifestyle and environmental factors determined the risk of CRC better than family history alone [58]. Although not yet mainstream, polygenetic risk scores, utilizing a validated set of SNPs, in combination with NGS panels including both high and moderate cancer risk susceptibility genes, will likely become increasingly utilized in clinical care to risk stratify and guide medical management.
The use of RNA analysis to re-categorize or clarify VUSs is also under investigation. Using this technique, an exonic duplication in the MSH2 gene was found to result in abnormal transcription leading to Lynch syndrome [59•]. RNA analysis is now being offered by some labs in conjunction with DNA analysis to better classify VUSs involving splice site junctions and duplications that may be in tandem, as well as to detect deep intronic mutations. A recent study using a methylation tolerance (MT) assay evaluated cellular response to cytotoxic effects of methylating agents to determine the effect on VUSs in MMR genes [60]. This novel technique may be used to reclassify VUSs found in up to 30% of patients.
Lastly, recent studies have shown that not only Lynch-associated tumors, but tumors with high microsatellite instability (MSI-h)/mismatch repair deficiency (MMR-d) are particularly susceptible to immune-based therapies (i.e., pembrolizumab) with patients showing durable responses in treatment-refractory advanced metastatic disease. This finding is due to the accumulation of frameshift mutations at hotspot repeat sequences due to MSI and in turn leads to the development of immunogenic neopeptides/neoantigens which are recognized by CD8 + tumor infiltrating lymphocytes. Interestingly, patients with Lynch syndrome who are cancer-free have been found to harbor circulating cytotoxic T cells targeted against MSI-induced frameshift neoantigens which suggests the possibility that immune-based therapies (i.e., immune checkpoint inhibitors, vaccination) may be used to prevent cancer in patients with Lynch syndrome. Clinical trials, such as NCT03631641, are beginning to study the application of such novel concepts and give hope to all patients with a hereditary predisposition to cancer.
Conclusion
The widespread use of NGS technology has expanded the spectrum of hereditary CRC genes which can be analyzed at significantly less cost and, as a result, has significantly increased access to testing. It is imperative that gastroenterologists utilize various screening strategies to identify high-risk individuals who may benefit from genetic counseling and testing. Future research should focus on optimizing practical strategies for risk assessment, further characterizing CRC predisposition genes, clarifying VUSs, and standardizing management strategies for these patients.
Change history
23 December 2019
The original article unfortunately contained a mistake. On page 8, Table 2, the row with “POLE POLD1” has been shifted right so all the columns are not correct.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Schuster SC. Next-generation sequencing transforms today’s biology. Nat Methods. 2008;5(1):16–8.
Kastrinos F, Stoffel EM. History, genetics, and strategies for cancer prevention in Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12(5):715–27 quiz e41–3.
Karlitz JJ, Hsieh MC, Liu Y, Blanton C, Schmidt B, Jessup JM, et al. Population-based lynch syndrome screening by microsatellite instability in patients ≤50: prevalence, testing determinants, and result availability prior to colon surgery. Am J Gastroenterol. 2015;110(7):948–55.
Llor X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14(11):1516–20.
Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, et al. Environmental and heritable factors in the causation of cancer--analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med. 2000;343(2):78–85.
Giardiello FM, Brensinger JD, Petersen GM. AGA technical review on hereditary colorectal cancer and genetic testing. Gastroenterology. 2001;121(1):198–213.
Valle L. Recent discoveries in the genetics of familial colorectal cancer and polyposis. Clin Gastroenterol Hepatol. 2017;15(6):809–19.
Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, et al. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110(2):223–62 quiz 63.
Giardiello FM, Allen JI, Axilbund JE, Boland CR, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of lynch syndrome: a consensus statement by the US multi-society task force on colorectal cancer. Gastroenterology. 2014;147(2):502–26.
Jasperson K, Burt RW. The genetics of colorectal cancer. Surg Oncol Clin N Am. 2015;24(4):683–703.
Provenzale D, Gupta S, Ahnen DJ, Chen LM, Chung DC, Cooper G, et al. Genetic/familial high-risk assessment: colorectal version 2. NCCN Clinical Practice Guidelines in Oncology. 2019.The NCCN guidelines are the recognized standard for clinical policy in cancer care and are the most detailed and most frequently updated clinical practice guidelines available in any area of medicine. This particular guideline addresses the identification and management of patients at risk for hereditary colorectal cancer.
Stoffel E, Mukherjee B, Raymond VM, Tayob N, Kastrinos F, Sparr J, et al. Calculation of risk of colorectal and endometrial cancer among patients with lynch syndrome. Gastroenterology. 2009;137(5):1621–7.
Singh H, Schiesser R, Anand G, Richardson PA, El-Serag HB. Underdiagnosis of Lynch syndrome involves more than family history criteria. Clin Gastroenterol Hepatol. 2010;8(6):523–9.
Tranø G, Wasmuth HH, Sjursen W, Hofsli E, Vatten LJ. Awareness of heredity in colorectal cancer patients is insufficient among clinicians: a Norwegian population-based study. Color Dis. 2009;11(5):456–61.
Sjursen W, Haukanes BI, Grindedal EM, Aarset H, Stormorken A, Engebretsen LF, et al. Current clinical criteria for lynch syndrome are not sensitive enough to identify MSH6 mutation carriers. J Med Genet. 2010;47(9):579–85.
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, et al. Feasibility of screening for lynch syndrome among patients with colorectal cancer. J Clin Oncol. 2008;26(35):5783–8.
Stoffel EM, Yurgelun MB. Genetic predisposition to colorectal cancer: implications for treatment and prevention. Semin Oncol. 2016;43(5):536–42.
Berera S, Koru-Sengul T, Miao F, Carrasquillo O, Nadji M, Zhang Y, et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14(8):1163–71.
Barzi A, Sadeghi S, Kattan MW, Meropol NJ. Comparative effectiveness of screening strategies for Lynch syndrome. J Natl Cancer Inst. 2015;107(4).
Hampel H, Pearlman R, Beightol M, Zhao W, Jones D, Frankel WL, et al. Assessment of tumor sequencing as a replacement for lynch syndrome screening and current molecular tests for patients with colorectal cancer. JAMA Oncol. 2018;4(6):806–13.
Lu KH, Wood ME, Daniels M, Burke C, Ford J, Kauff ND, et al. American Society of Clinical Oncology expert statement: collection and use of a cancer family history for oncology providers. J Clin Oncol. 2014;32(8):833–40.
• Kastrinos F, Uno H, Ukaegbu C, Alvero C, McFarland A, Yurgelun MB, et al. Development and validation of the PREMM. J Clin Oncol. 2017;35(19):2165–72.This paper incorporates all Lynch-associated genes into a new clinical prediction model, PREMM5, and discusses the use of a lower threshold of 2.5%.
Dinh TA, Rosner BI, Atwood JC, Boland CR, Syngal S, Vasen HF, et al. Health benefits and cost-effectiveness of primary genetic screening for Lynch syndrome in the general population. Cancer Prev Res (Phila). 2011;4(1):9–22.
Luba DG, DiSario JA, Rock C, Saraiya D, Moyes K, Brown K, et al. Community practice implementation of a self-administered version of PREMM. Clin Gastroenterol Hepatol. 2018;16(1):49–58.
Kastrinos F, Allen JI, Stockwell DH, Stoffel EM, Cook EF, Mutinga ML, et al. Development and validation of a colon cancer risk assessment tool for patients undergoing colonoscopy. Am J Gastroenterol. 2009;104(6):1508–18.
•• Guivatchian T, Koeppe ES, Baker JR, Moisa C, Demerath M, Foor-Pessin C, et al. Family history in colonoscopy patients: feasibility and performance of electronic and paper-based surveys for colorectal cancer risk assessment in the outpatient setting. Gastrointest Endosc. 2017;86(4):684–91.This study uses an expanded 5-question version of the Kastrinos questionairre for risk assessment of hereditary CRC syndromes.
Kessels K, Eisinger JD, Letteboer TG, Offerhaus GJA, Siersema PD, Moons LMG. Sending family history questionnaires to patients before a colonoscopy improves genetic counseling for hereditary colorectal cancer. J Dig Dis. 2017;18(6):343–8.
Walker JG, Bickerstaffe A, Hewabandu N, Maddumarachchi S, Dowty JG, Jenkins M, et al. The CRISP colorectal cancer risk prediction tool: an exploratory study using simulated consultations in Australian primary care. BMC Med Inform Decis Mak. 2017;17(1):13.
Gunaratnam NT, Akce M, Al Natour R, Bartley AN, Fioritto AF, Hanson K, et al. Screening for cancer genetic syndromes with a simple risk-assessment tool in a community-based open-access colonoscopy practice. Am J Gastroenterol. 2016;111(5):589–93.
McAllister B, McGarrity T, Soriano C, Cooper J, Walter V, Loloi J, et al. Comparison of colorectal cancer (CRC) screening rates obtained by electronic medical record (EMR) query versus patient-directed Ssurvey in primary care practice. American College of Gastroenterology. 2018:P0223.
McGarrity T, Soriano C, McAllister B, Cooper J, Zhu J, Peiffer L, et al. Results of an electronic patient survey to determine up-to-date colorectal cancer screening status and identify high-risk individuals. American College of Gastroenterology. 2018:P0230.
Rubinstein WS, Acheson LS, O'Neill SM, Ruffin MT, Wang C, Beaumont JL, et al. Clinical utility of family history for cancer screening and referral in primary care: a report from the family Healthware impact trial. Genet Med. 2011;13(11):956–65.
Feero WG, Facio FM, Glogowski EA, Hampel HL, Stopfer JE, Eidem H, et al. Preliminary validation of a consumer-oriented colorectal cancer risk assessment tool compatible with the US Surgeon General’s My Family Health Portrait. Genet Med. 2015;17(9):753–6.
Walker JG, Licqurish S, Chiang PP, Pirotta M, Emery JD. Cancer risk assessment tools in primary care: a systematic review of randomized controlled trials. Ann Fam Med. 2015;13(5):480–9.
Snyder C. Evolution of cancer risk assessment and counseling related to psychological, financial and legal implications. Familial Cancer. 2016;15(3):493–6.
Hampel H. Genetic counseling and cascade genetic testing in Lynch syndrome. Familial Cancer. 2016;15(3):423–7.
Sharaf RN, Myer P, Stave CD, Diamond LC, Ladabaum U. Uptake of genetic testing by relatives of lynch syndrome probands: a systematic review. Clin Gastroenterol Hepatol. 2013;11(9):1093–100.
Robson ME, Bradbury AR, Arun B, Domchek SM, Ford JM, Hampel HL, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33(31):3660–7.
Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017;3(4):464–71.
Cragun D, Radford C, Dolinsky JS, Caldwell M, Chao E, Pal T. Panel-based testing for inherited colorectal cancer: a descriptive study of clinical testing performed by a US laboratory. Clin Genet. 2014;86(6):510–20.
Lindor NM, Rabe K, Petersen GM, Haile R, Casey G, Baron J, et al. Lower cancer incidence in Amsterdam-I criteria families without mismatch repair deficiency: familial colorectal cancer type X. JAMA. 2005;293(16):1979–85.
Broderick P, Dobbins SE, Chubb D, Kinnersley B, Dunlop MG, Tomlinson I, et al. Validation of recently proposed colorectal cancer susceptibility gene variants in an analysis of families and patients-a systematic review. Gastroenterology. 2017;152(1):75-7.e4.This study used high-throughput sequencing analysis to validate association between gene variants and development of CRC.
Katona BW, Yurgelun MB, Garber JE, Offit K, Domchek SM, Robson ME, et al. A counseling framework for moderate-penetrance colorectal cancer susceptibility genes. Genet Med. 2018;20(11):1324–7.
Rayner E, van Gool IC, Palles C, Kearsey SE, Bosse T, Tomlinson I, et al. A panoply of errors: polymerase proofreading domain mutations in cancer. Nat Rev Cancer. 2016;16(2):71–81.
McKenna DB, Van Den Akker J, Zhou AY, Ryan L, Leon A, O’Connor R, et al. Identification of a novel GREM1 duplication in a patient with multiple colon polyps. Familial Cancer. 2019;18(1):63–6.
Weren RD, Ligtenberg MJ, Geurts van Kessel A, De Voer RM, Hoogerbrugge N, Kuiper RP. NTHL1 and MUTYH polyposis syndromes: two sides of the same coin? J Pathol. 2018;244(2):135–42.
Quintana I, Mejías-Luque R, Terradas M, Navarro M, Piñol V, Mur P, et al. Evidence suggests that germline. Gut. 2018;67(12):2230–2.
AlDubayan SH, Giannakis M, Moore ND, Han GC, Reardon B, Hamada T, et al. Inherited DNA-repair defects in colorectal cancer. Am J Hum Genet. 2018;102(3):401–14.
Oh M, McBride A, Yun S, Bhattacharjee S, Slack M, Martin JR, et al. BRCA1 and BRCA2 gene mutations and colorectal cancer risk: systematic review and meta-analysis. J Natl Cancer Inst. 2018;110(11):1178–89.
Rivera B, Perea J, Sánchez E, Villapún M, Sánchez-Tomé E, Mercadillo F, et al. A novel AXIN2 germline variant associated with attenuated FAP without signs of oligondontia or ectodermal dysplasia. Eur J Hum Genet. 2014;22(3):423–6.
Clarke E, Green RC, Green JS, Mahoney K, Parfrey PS, Younghusband HB, et al. Inherited deleterious variants in GALNT12 are associated with CRC susceptibility. Hum Mutat. 2012;33(7):1056–8.
Adam R, Spier I, Zhao B, Kloth M, Marquez J, Hinrichsen I, et al. Exome sequencing identifies Biallelic MSH3 Germline mutations as a recessive subtype of colorectal adenomatous polyposis. Am J Hum Genet. 2016;99(2):337–51.
Lorans M, Dow E, Macrae FA, Winship IM, Buchanan DD. Clin Colorectal Cancer. 2018;17(2):e293–305.
Susswein LR, Marshall ML, Nusbaum R, Vogel Postula KJ, Weissman SM, Yackowski L, et al. Pathogenic and likely pathogenic variant prevalence among the first 10,000 patients referred for next-generation cancer panel testing. Genet Med. 2016;18(8):823–32.
Yurgelun MB, Allen B, Kaldate RR, Bowles KR, Judkins T, Kaushik P, et al. Identification of a variety of mutations in cancer predisposition genes in patients with suspected Lynch syndrome. Gastroenterology. 2015;149(3):604–13.e20.
Eccles BK, Copson E, Maishman T, Abraham JE, Eccles DM. Understanding of BRCA VUS genetic results by breast cancer specialists. BMC Cancer. 2015;15:936.
Jenkins MA, Win AK, Dowty JG, MacInnis RJ, Makalic E, Schmidt DF, et al. Ability of known susceptibility SNPs to predict colorectal cancer risk for persons with and without a family history. Fam Cancer. 2019.Incorporation of SNPs into CRC screening strategies compared to family history.
Jeon J, Du M, Schoen RE, Hoffmeister M, Newcomb PA, Berndt SI, et al. Determining risk of colorectal cancer and starting age of screening based on lifestyle, environmental, and genetic factors. Gastroenterology. 2018;154(8):2152–64.e19.
• Conner BR, Hernandez F, Souders B, Landrith T, Boland CR, Karam R. RNA analysis identifies pathogenic duplications in MSH2 in patients with lynch syndrome. Gastroenterology. 2019;156(6):1924–5.e4.Use of RNA analysis to further clarify VUSs in patients with MSH2 mutations.
Bouvet D, Bodo S, Munier A, Guillerm E, Bertrand R, Colas C, et al. Methylation tolerance-based functional assay to assess variants of unknown significance in the MLH1 and MSH2 genes and identify patients with lynch syndrome. Gastroenterology. 2019;157(2):421–31.
Acknowledgements
The primary author acknowledges Heather Stern for her editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
References for readers
PREMM5 model = https://premm.dfci.harvard.edu/
GeneReviews® = https://www.ncbi.nlm.nih.gov/books/NBK1116/
2019 NCCN guidelines = https://www.nccn.org
National Society of Genetics Counselors = www.nsgc.org
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: Table 2 layout in pdf is incorrect while html version is correct.
This article is part of the Topical Collection on Genetics in Gastroenterology Practice
Rights and permissions
About this article
Cite this article
Stern, B., McGarrity, T. & Baker, M. Incorporating Colorectal Cancer Genetic Risk Assessment into Gastroenterology Practice. Curr Treat Options Gastro 17, 702–715 (2019). https://doi.org/10.1007/s11938-019-00267-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-019-00267-w