Abstract
Purpose of review
This review will define morbid obesity and relationship between morbid obesity and heart failure syndromes. It will delve into unique challenges facing patients with dual diagnoses of heart failure and morbid obesity and examine the data that obesity should be a target in the treatment of heart failure.
Recent findings
Emerging literature has indicated the safety and efficacy of surgical weight loss in patients with heart failure. Furthermore, bariatric surgery with associated weight loss has been associated with improvements in heart failure symptoms and reverse remodeling on echocardiography. In patients with advanced heart failure, bariatric surgery has led to improvement in heart failure to obviate the need for cardiac transplantation or sufficient weight loss for cardiac transplant eligibility.
Summary
In heart failure patients who are morbidly obese, treatment of obesity is an effective therapeutic target with a myriad of potential benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is an epidemic that affects over one-third of adult Americans, and its incidence is growing in the USA and worldwide [1]. In 2015, the U.S. Department of Health and Human Services released statistics from 2011 to 2014 citing that 36% of adults and 17% youth are obese. Obesity is defined by body mass index (BMI), which is calculated by body weight in kilograms divided by the square of height in meters. According to the CDC, a normal BMI falls between 18.5 and less than 25. Overweight is defined as BMI from 25 to less than 30, and obesity is defined as a BMI greater than or equal to 30 [2]. However, obesity can be further subcategorized into class 1 with BMI of 30 to less than 35, class 2 with BMI from 35 to less than 40, and class 3 with BMI of 40 or greater. Morbid obesity is further defined as having a BMI of 40 or greater or a BMI of 35 or greater with obesity-related health conditions such as hypertension or diabetes.
Obesity is an established risk factor for heart failure [3]. In the Framingham Heart Study, an incremental increase of 1 BMI was associated with a 5% increased risk of heart failure for men and 7% increased risk of heart failure in women [4]. This finding was further supported by a Mendelian randomization study that reported an increase of one standard deviation in BMI (4.5 kg/m2) corresponds to a 93% increase in the risk of heart failure (HR 1.93, 95% CI 1.12–3.30) [5]. Furthermore, obesity is associated with metabolic syndrome, a constellation of abdominal obesity, dyslipidemia, hypertension, insulin resistance, and pro-inflammatory and pro-thrombotic states [6].
This review will provide an overview on the impact of morbid obesity in patients with heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF) and discuss medical and surgical management options for obese heart failure patients, with the perspective that morbid obesity is a potent therapeutic target in the management of heart failure.
Impact of obesity on heart failure with reduced ejection fraction
Impact on advanced therapy candidacy
When evaluating end-stage heart failure patients for advanced therapies such as left ventricular assist device (LVAD) and orthotopic cardiac transplant (OHT), morbid obesity is generally viewed as relative contraindication. Cardiac surgery confers higher morbidity and mortality in patients with morbid obesity (BMI ≥ 35); however, increase in adverse outcomes is not seen in patients with BMI in the overweight (BMI 25–29.9) or obese (BMI 30–34.9) ranges [7]. Morbidly obese patients who undergo OHT fare worse than those with BMI below 35. BMI > 35 is associated with increased rate of early complications post-operatively, and lower long-term survival [8]. Data suggest morbidly obese cardiac transplant recipients are at increased risk of high-grade acute rejection, though there is no difference in transplant-related coronary artery disease [9].
Interactions between morbid obesity and left ventricular assist devices
Clinical trials of durable mechanical circulatory support devices such as left ventricular assist devices (LVADs) enrolled few patients at the extremes of BMI. The ENDURANCE Supplemental Trial comparing HeartWare (Medtronic) to Heartmate II (Abbott) devices enrolled patients with an average BMI of 28 kg/m2 [10]. The landmark clinical trials that lead to approval of Heartmate II and Heartmate III pumps enrolled patients with an average body surface area of 2.0–2.1m2 [11, 12]. Therefore, there is a paucity of randomized clinical trial data regarding the upper limit of BMI in which LVAD technology can be safely deployed. However, small, observational studies have reported the feasibility of implantation of LVAD as a bridge to bariatric surgery and ultimately to qualify obese patients for cardiac transplantation in patients with BMI up to the mid-50s [13, 14].
Impact of obesity on heart failure with preserved ejection fraction
Similar to patients with reduced ejection fraction, patients with heart failure with preserved ejection (HFpEF) who are morbidly obese also present unique diagnostic and treatment challenges. Morbidly obese individuals often experience dyspnea that can be multifactorial and difficult to attribute to heart failure alone. Clinical exam in this patient population for signs of intravascular congestion and cardiac dysfunction may be difficult. Furthermore, echocardiography and laboratory testing such as NT-proBNP can be difficult to interpret due to challenges in anatomy and falsely low NT-proBNP levels, respectively [15,16,17]. In light of these diagnostic challenges, the diagnosis of HFpEF should only be made in the setting of hospitalizations for heart failure with clinical finding of intravascular volume overload or congestion. In patients whom the diagnosis of dyspnea is indeterminate, a right heart catheterization with direct measurement of right- and left-sided filling pressures, with the addition of exercise provocation if measurements are normal at baseline, should be used to clarify the diagnosis of HFpEF.
Medical and surgical interventions for morbid obesity and heart failure outcomes
Given the challenges facing morbidly obese patients with heart failure syndromes, this section will focus on treatment options for morbid obesity and the promise of treating obesity as a therapeutic target in heart failure. Optimal treatment of morbid obesity should be multifaceted to target medical, psychosocial, and educational contributors to the disease process; thus, we propose a multidisciplinary approach to address dietary education, psychosocial support, and consideration of medical or surgical weight loss. Successful weight reduction with bariatric surgery has been correlated with reduction in other disease states associated with metabolic syndrome including diabetes mellitus, hypertension, dyslipidemia, sleep apnea, fatty liver disease, as well as in depression and migraines [18, 19].
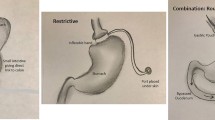
Outcomes with intensive lifestyle medication and medications
Intensive behavioral interventions to target weight loss have met with modest weight reduction success [20]. However, there is controversy to the duration of effect of intensive behavioral therapy. There are nine classes of medications with FDA approval for weight loss, each demonstrating modest improvements in weight compared with placebo control. The nine classes of drugs include pancreatic lipase inhibitor (orlistat), serotonin-2C receptor agonist (lorcaserin), combination phentermine-topiramate, combination bupropion-naltrexone, GLP-1 agonist (liraglutide), and noradrenergic sympathomimetic drugs approved for short-term use (benzphetamine, diethylpropion, phentermine, and phendimetrazine). However, due to side effect profiles of worsening hypertension, heart rate, and other sympathomimetic properties, many classes of these medications are contraindicated in patients with heart failure or hypertension. Additionally, many of these drugs have only been studied for short-term use. SGLT2 inhibitors principally studied for the management of type II diabetes mellitus may also play a role in weight reduction especially in obese heart failure patients with metabolic syndrome [21]. Head-to-head trials of medical intervention weight loss to surgical weight loss thus far have demonstrated the superiority of surgical weight loss in terms of weight reduction and remission of diabetes mellitus and hypertension [22, 23]. Therefore, the remainder of this review will focus on the outcomes of surgical weight loss in patients with morbid obesity (Table 1).
Surgical management of obesity and heart failure outcomes
Alpert and colleagues first reported improvements in echocardiographic parameters and left ventricular remodeling following bariatric surgery in a case series of patients with baseline left ventricular dysfunction [32]. Since this early study, subsequent observational studies have been published describing the safety and efficacy of bariatric surgery in morbidly obese patients with depressed left ventricular function [33, 34]. Supporting evidence for bariatric surgery includes findings that a history of bariatric surgery in patients with heart failure is associated with reduction in hospitalization and emergency department visits [25]. Bariatric surgery also improves quality of life and functional capacity in patients with heart failure [24, 29]. An extensive literature dating from 1950 to 2012 encompassing 73 studies and over 19 thousand subjects suggests that bariatric surgery is an effective method of treating hypertension, diabetes, dyslipidemia, and ameliorating heart failure [30]. On echocardiography, bariatric surgery has been associated with statistically significant reductions in left ventricular mass, E/A ratio, and isovolumetric relaxation time [26, 35,36,37]. These studies suggest that reduction in weight, accompanied by resolution of metabolic syndrome, may be particularly attractive target for HFpEF patients.
In patients with advanced heart failure, bariatric surgery may result in cardiac remodeling to obviate the need for further advanced therapies such as LVAD or OHT, or it may serve as a bridge to heart transplant eligibility. Leviner and colleagues presented an intriguing case of a patient with ejection fraction of 25% and low output heart failure deemed ineligible for transplant based on BMI of 40 kg/m2 who subsequently underwent HMII LVAD implant prior to laparoscopic sleeve gastrectomy [38]. Ultimately, the patient demonstrated significant weight loss with BMI improvement to 29 kg/m2 and recovery of ejection fraction to 40% allowing LVAD explant. A similar case has been reported in a male with BMI of 50 kg/m2 and LVEF 25% who underwent bariatric surgery with subsequent improvement of BMI to 27 kg/m2 accompanied by improvement in LVEF to 35–40% and reduction in LV posterior wall thickness [39]. Ristow et al. present two cases of patients with morbid obesity (BMI 43 and 56 kg/m2) and systolic heart failure who were ineligible for transplantation who underwent laparoscopic gastrectomy with subsequent significant improvement in LVEF and LV dimensions such that neither required cardiac transplantation [40]. These case reports suggest that in some individuals with severely depressed left ventricular function, bariatric surgery can lead to reverse remodeling and significant clinical improvement to obviate the need for OHT.
For patients in whom OHT is necessary, bariatric surgery, often supported by LVADs, has been associated with observational studies with significant weight loss leading to transplant eligibility [28, 41, 42]. Chaudhry and colleagues reported successful implantation of LVADs in six patients with average BMI of 47.6 kg/m2 and mean LVEF < 20% initially deemed ineligible for transplant due to morbid obesity. Subsequently, all patients lost sufficient weight to be listed for OHT, with 2 patients undergoing successful transplant at time of publication. A retrospective analysis of seven patients with depressed ejection fraction, average LVEF 25%, and BMI 42.8 kg/m2, who underwent bariatric surgery, demonstrated significant reduction in weight and improvement in ejection fraction and successful bridge to cardiac transplantation in 2 of these patients [27]. A case-controlled study of 12 patients with morbid obesity with an average BMI of 53 kg/m2 and LVEF 22% who underwent bariatric surgery compared with a control group of morbidly obese HF patients revealed greater improvement in NYHA class, reduction in hospital admission, and bridge to transplant eligibility in the surgical group [31].
Targeting obesity in heart failure—the metabolic link
Excess energy is stored in adipose tissue; however, when the surplus of energy exceeds the storage capacity of peripheral adipose tissue, fat is then deposited in organs including the heart. Intramyocardial lipid overload is seen in obese patients and animal models of obesity and is linked to alterations in gene expression and cardiac dysfunction [43]. Adipokines, signaling molecules associated with adipose tissue, such as leptin, resistin, TNF-α, IL-6, and angiotensinogen have been implicated in adverse left ventricular remodeling, in promotion of insulin resistance, and in the creation of pro-inflammatory milieu [44]. Activation of the renin-angiotensin (RAAS) pathway has been further implicated in the development of cardiorenal syndrome in obese patients [45]. Leichman and colleagues have demonstrated reduction in plasma leptin, restoration of insulin sensitivity, and improvements in metabolic derangements in 43 consecutive patients undergoing bariatric surgery [46].
Surgical weight loss has been shown to improve outcomes in diabetes, which provides insight on putative salutary effects of weight loss surgery on heart failure [47]. The STAMPEDE trial randomized type II diabetes mellitus patients with BMI 27–43 to bariatric surgery versus optimal medical therapy [48]. At 5 years, the surgical intervention group achieved statistically significantly greater reduction in hemoglobin A1c (2.1% versus 0.3%), weight loss, lower triglyceride level, reduced use of insulin, and higher quality of life than the group treated with medical therapy. Given the neurohormonal dysregulation in both HFpEF and HFrEF that predisposes to congestion, bariatric surgery offers an attractive potential therapeutic target in the management of heart failure.
Conclusion
A significant portion of patients with heart failure syndrome are also obese. This review provides an overview of the special challenges facing morbidly obese heart failure patients and sheds light onto emerging evidence that targeting excess weight leads to improvements in cardiac function, quality of life, and reduction in heart failure hospitalizations. In the subset of patients with advanced heart failure for whom cardiac transplantation is indicated, surgical weight loss, often supported by LVADs, has led to significant weight loss resulting in transplant eligibility. Randomized trial data, however, is lacking and would further solidify the role of targeting morbid obesity in heart failure.
References and recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ogden CL, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. 2015;8.
Defining adult overweight and obesity | overweight & obesity | CDC. 2019. Available at: https://www.cdc.gov/obesity/adult/defining.html. Accessed 2nd July 2019.
Ahmad FS, Ning H, Rich JD, Yancy CW, Lloyd-Jones DM, Wilkins JT. Hypertension, obesity, diabetes, and heart failure-free survival: the cardiovascular disease lifetime risk pooling project. JACC Heart Fail. 2016;4:911–9.
Kenchaiah S, et al. Obesity and the risk of heart failure. (2009). https://doi.org/10.1056/NEJMoa020245
Hägg S, et al. Adiposity as a cause of cardiovascular disease: a Mendelian randomization study. Int J Epidemiol. 2015;44:578–86.
Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C. Definition of metabolic syndrome. Circulation. 2004;109:433–8.
Johnson AP, et al. Body mass index, outcomes, and mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc. 2015;4.
Nagendran J, et al. The varying effects of obesity and morbid obesity on outcomes following cardiac transplantation. Int J Obes. 2016;2005(40):721–4.
Lietz K, John R, Burke EA, Ankersmit JH, McCue JD, Naka Y, et al. Pretransplant cachexia and morbid obesity are predictors of increased mortality after heart transplantation. Transplantation. 2001;72:277–83.
Milano CA, Rogers JG, Tatooles AJ, Bhat G, Slaughter MS, Birks EJ, et al. HVAD: the ENDURANCE supplemental trial. JACC Heart Fail. 2018;6:792–802.
Mehra MR, Uriel N, Naka Y, Cleveland JC Jr, Yuzefpolskaya M, Salerno CT, et al. A fully magnetically levitated left ventricular assist device — final report. N Engl J Med. 2019;380:1618–27.
Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361:2241–51.
Caceres M, Czer LSC, Esmailian F, Ramzy D, Moriguchi J. Bariatric surgery in severe obesity and end-stage heart failure with mechanical circulatory support as a bridge to successful heart transplantation: a case report. Transplant Proc. 2013;45:798–9.
Lockard KL, Allen C, Lohmann D, Severyn DA, Schaub RD Jr, Kauffman KE, et al. Bariatric surgery for a patient with a HeartMate II ventricular assist device for destination therapy. Prog Transplant Aliso Viejo Calif. 2013;23:28–32.
Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Wilson PWF, et al. Impact of obesity on plasma natriuretic peptide levels. Circulation. 2004;109:594–600.
Das SR, Drazner MH, Dries DL, Vega GL, Stanek HG, Abdullah SM, et al. Impact of body mass and body composition on circulating levels of natriuretic peptides. Circulation. 2005;112:2163–8.
Sugisawa T, et al. Association of plasma B-type natriuretic peptide levels with obesity in a general urban Japanese population: the Suita Study. Endocr J. advpub, 2010;1005060418–1005060418.
Beamish AJ, Olbers T, Kelly AS, Inge TH. Cardiovascular effects of bariatric surgery. Nat Rev Cardiol. 2016;13:730–43.
Vest AR, Heneghan HM, Schauer PR, Young JB. Surgical management of obesity and the relationship to cardiovascular disease. Circulation. 2013;127:945–59.
Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–68.
Pham D, De Albuquerque Rocha N, McGuire DK, Neeland IJ. Impact of empagliflozin in patients with diabetes and heart failure. Trends Cardiovasc Med. 2017;27:144–51.
Andersen T, Stokholm KH, Backer OG, Quaade F. Long-term (5-year) results after either horizontal gastroplasty or very-low-calorie diet for morbid obesity. Int J Obes. 1988;12:277–84.
Obesity-related cardiovascular risk factors after weight loss: a clinical trial comparing gastric bypass surgery and intensive lifestyle intervention. Eur J Endocrinol. 2010;163(5). Available at: https://eje.bioscientifica.com/view/journals/eje/163/5/735.xml. Accessed 28th June 2019.
Berger S, et al. Bariatric surgery among patients with heart failure: a systematic review and meta-analysis. Open Heart. 2018;5. Systematic review of recent populations suggesting bariatric surgery is associated with improvements in quality of life, re-duced hospital admissions, and improvements in heart failure symptoms in patients with obese patients with HF.
Shimada YJ, Tsugawa Y, Brown DFM, Hasegawa K. Bariatric surgery and emergency department visits and hospitalizations for heart failure exacerbation: population-based, self-controlled series. J Am Coll Cardiol. 2016;67:895–903 Bariatric surgery in HF patients is associated with reduction in emergency department visits and heart failure hospitalizations.
Vest Amanda R, et al. Clinical and echocardiographic outcomes after bariatric surgery in obese patients with left ventricular systolic dysfunction. Circ Heart Fail. 2016;9:e002260 Patients with left ventricular ejection fraction < 50% undergoing bariatric surgery compared with matched cohort of patients without surgery demonstrating greater improvement in LV ejection fraction post-op. No excess mortality detected at 1 year compared with bariatric surgery patients without depressed ejection fraction.
Lim C-P, Fisher OM, Falkenback D, Boyd D, Hayward CS, Keogh A, et al. Bariatric surgery provides a ‘bridge to transplant’ for morbidly obese patients with advanced heart failure and may obviate the need for transplantation. Obes Surg. 2016;26:486–93.
Wikiel KJ, McCloskey CA, Ramanathan RC. Bariatric surgery: a safe and effective conduit to cardiac transplantation. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2014;10:479–84.
Miranda WR, et al. Impact of bariatric surgery on quality of life, functional capacity, and symptoms in patients with heart failure. Obes Surg. 2013;23:1011–5.
Vest AR, Heneghan HM, Agarwal S, Schauer PR, Young JB. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart Br Card Soc. 2012;98:1763–77.
Ramani GV, McCloskey C, Ramanathan RC, Mathier MA. Safety and efficacy of bariatric surgery in morbidly obese patients with severe systolic heart failure. Clin Cardiol. 2008;31:516–20.
Alpert MA, Terry BE, Kelly DL. Effect of weight loss on cardiac chamber size, wall thickness and left ventricular function in morbid obesity. Am J Cardiol. 1985;55:783–6.
Department of General Surgery, University General Hospital Gregorio Marañón, Calle del Doctor Esquerdo, 46, 28007 Madrid, Spain et al. Improvement of ventricular ejection fraction after bariatric surgery in obese patients with dilated cardiomyopathy. Obes Res - Open J. 2015;1:1–3.
Samaras K, Connolly SM, Lord RV, Macdonald P, Hayward CS. Take heart: bariatric surgery in obese patients with severe heart failure. Two case reports. Heart Lung Circ. 2012;21:847–9.
Grapsa J, et al. The effect of bariatric surgery on echocardiographic indices: a review of the literature. Eur J Clin Investig. 2013;43:1224–30.
Iyengar S, Leier CV. Rescue bariatric surgery for obesity-induced cardiomyopathy. Am J Med. 2006;119:e5–6.
Mukerji R, Petruc M, Fresen JL, Terry BE, Govindarajan G, Alpert MA. Effect of weight loss after bariatric surgery on left ventricular mass and ventricular repolarization in normotensive morbidly obese patients. Am J Cardiol. 2012;110:415–9.
Leviner DB, Keidar A, Ben-Gal T, Medalion B. Cardiac function recovery following LVAD implantation and bariatric surgery in a morbidly obese patient. J Card Surg. 2014;29:740–2.
Reigle J. Heart failure, Obesity and Bariatric Surgery. Prog Cardiovasc Nurs. 2009;24:36–8.
Ristow B, Rabkin J, Haeusslein E. Improvement in dilated cardiomyopathy after bariatric surgery. J Card Fail. 2008;14:198–202.
Chaudhry UI, Kanji A, Sai-Sudhakar CB, Higgins RS, Needleman BJ. Laparoscopic sleeve gastrectomy in morbidly obese patients with end-stage heart failure and left ventricular assist device: medium-term results. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2015;11:88–93.
Jeng EI, Aranda JM, Ahmed M, Klodell CT. Left ventricular assist device and bariatric surgery: a bridge to heart transplant by weight and waiting time reduction. J Card Surg. 2016;31:120–2.
Algahim MF, Sen S, Taegtmeyer H. Bariatric surgery to unload the stressed heart: a metabolic hypothesis. Am J Physiol Heart Circ Physiol. 2012;302:H1539–45.
Vest AR, Young JB. Should we target obesity in advanced heart failure? Curr Treat Options Cardiovasc Med. 2014;16:284.
Fenske W, Athanasiou T, Harling L, Drechsler C, Darzi A, Ashrafian H. Obesity-related cardiorenal disease: the benefits of bariatric surgery. Nat Rev Nephrol. 2013;9:539–51.
Leichman JG, Wilson EB, Scarborough T, Aguilar D, Miller CC III, Yu S, et al. Dramatic reversal of derangements in muscle metabolism and left ventricular function after bariatric surgery. Am J Med. 2008;121:966–73.
Johnson BL, et al. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severely obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216:545–56; discussion 556–558.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. N Engl J Med. 2017;376:641–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there are no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Albert, C.L. Morbid Obesity as a Therapeutic Target for Heart Failure. Curr Treat Options Cardio Med 21, 52 (2019). https://doi.org/10.1007/s11936-019-0754-z
Published:
DOI: https://doi.org/10.1007/s11936-019-0754-z