Abstract
Purpose of the review
Cardiovascular disease (CVD) has been and remains the leading cause of mortality in women in the United States. For decades, more women died every year of CVD compared to men. Heart centers for women (HCW) are developed in response to the need for greater patient and physician awareness of CVD in women and to conduct sex-specific research in women. Today, many HCW provide multispecialty and focused areas of cardiovascular care for women. HCW provide their female patients with expertise over the many stages of a woman’s life. And HCW partner with national organizations to advance research and education through specialized and focused care for women. The purpose of this review is to review the historical development of heart centers for women and discuss the types of care they provide for women.
Recent findings
Mortality rates from cardiovascular disease in women are finally reaching the levels of men after decades of focus on awareness, prevention, and evidence-based guideline-directed care for women.
Summary
Heart centers for women have evolved to provide subspecialty and comprehensive care for women that includes education and research. Heart centers for women are partnering with many other disease-based and patient advocacy organizations to provide care for all women at all stages of life. Alarmingly, there has been increasing CVD mortality in both men and women recently.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1994, an American Heart Association (AHA) statement reported that 45.2% of deaths in women were from a cardiovascular (CV) cause. In 1995, the AHA published the brochure Silent Epidemic and started encouraging awareness of heart disease in women. Three years later in 1997, a poll of 1000 women indicated that only 8% of those surveyed knew that cardiovascular disease (CVD) was a woman’s greatest health concern and less than a third knew that CVD was the number one cause of death in women [1]. In response to these concerning findings, Circulation published Cardiovascular Disease in Women: A Statement for Healthcare Professionals from the American Heart Association [2] which started to raise awareness but action was still forthcoming. A few years later, a survey of over 300 primary care physicians, 100 obstetricians/gynecologists, and 100 cardiologists revealed that less than one in five physicians were aware that CVD was the number one cause of death for women [3]. Physicians rate themselves as very ineffective in their ability to prevent CVD in women [3].
The remarkable decrease in CVD mortality starting in 2000 in women in the United States (US) coincided with the combined efforts by many organizations and the results of the landmark hormone replacement therapy trials on primary and secondary prevention of coronary artery disease in women. The Heart and Estrogen/progestin Replacement Study (HERS) and Women’s Health Initiative (WHI) study both showed increase CV events with hormone replacement therapy [4, 5]. CVD mortality in men began to decline in 1980 but was not seen in women until two decades later [6]. Since 1984, there were significantly more CVD deaths in women than men and yet heart disease continued to be considered a man’s disease [6]. In 2002, the National Heart, Lung, and Blood Institute (NHLBI) launched The Heart Truth®, the first federally sponsored national campaign to raise awareness, to reduce mortality in women in the US. The Red Dress symbol released as part of this campaign has now become a national symbol for women and heart disease. Subsequently, the AHA partnered with NHLBI and other organizations to launch the Go Red for Women initiative in February 2004. The campaign incorporated awareness of heart disease in women through celebrity speakers, National Wear Red Day, Go Red Luncheons, and events that promoted and empowered women to take action. These activities coincided with the release of the first ever evidence-based guidelines focused on prevention of heart disease in women [7]. The AHA Go Red for Women campaign has expanded to encompass development of risk assessment tools, disease management guidelines, implementation of these guidelines, and sex-specific research to decrease the high morbidity of CVD in women.
Several other national organizations emerged in response and have contributed to increased awareness of CVD in women. The WISEWOMAN (Well-Integrated Screening and Evaluation for WOMen Across the Nation) program, launched initially in 1995 by the Centers for Disease Control and Prevention (CDC), has grown significantly to provide heart and stroke risk factor screening and lifestyle interventions to low-income women. It has served over 150,000 women and is established in nine states and two Native American tribal organizations. In addition to individual support, the program promotes partnerships that bring about policy, culture, and systems changes that foster heart healthy behaviors. The US Department of Health and Human Services Office of Women’s Health launched the “Make the Call. Don’t Miss the Beat” campaign in 2011 to educate women about the importance of calling 9-1-1 when experiencing symptoms of a heart attack.
The remarkable decrease in CVD mortality in women in the US from 1984 to 2012 coincided with the combined efforts of these and many other organizations. Concerted local, regional, and national campaigns targeting education, advocacy, clinical practice, and research regarding CVD in women have undoubtedly contributed to the significant decline in CVD mortality rates in women resulting in comparable rates in both genders by 2012. Thereafter, in 2013, CVD mortality rates were slightly lower in women and unfortunately in 2014 and 2015, CVD mortality rates rose in both genders, yet rates remained lower in women [6].
History of the development of heart centers for women
In response to these numerous national and patient advocacy efforts, there became an improved appreciation of the prevalence, presentation, diagnosis, treatment, and outcome of CVD in women by the general public, physicians, researchers, and regulatory bodies. In addition to these efforts, medical centers and individual physicians and health care groups opened practices focused on preventing and treating heart disease in women. These heart centers for women (HCW) were dedicated to increasing awareness, improving education for women and their providers, expanding sex- and gender-specific research, and determining social barriers to CVD care in women. These HCW created collaboration between the many disciplines of medicine that care for women and crossed barriers from grassroots advocacy to government funding for research to advance clinical expertise.
HCW began emerging throughout the US in the 1990s. A decade later, there were a handful of women’s heart centers across the country. WomenHeart: The National Coalition for Women with Heart Disease was founded in 1999. In 2001, they created a national directory of women’s heart centers that originally listed eleven HCW but had grown twenty-nine listings in just 2 years [8]. Many of the early programs were private practice groups with seven of the early eleven being private, only four academic. But by 2003, the private groups had grown to twenty-one groups and eight academic groups were listed. Private practice cardiology groups promoted these programs as a way to increase awareness in the public, attract women to their practices, and provide female-focused CV care. Academic models promoted education and research and helped develop evidence-based guidelines for women [7, 9].
Today, many cities have programs targeting CVD in women including special focused HCW. Currently, there is no agency that accredits or catalogs these programs. Some of the leading programs for research and treatment are academic institutions which have received grants from AHA, National Institute of Health, and CDC, as well as private donors and other funding agencies. Today, HCW are an integral part of most large health care centers and many academic cardiology programs. Medical students, residents, and cardiology fellows as well as nursing, nurse practitioner, and physician assistant students have clinical rotations within these institutions and many HCW lead the academic education through the inpatient and outpatient settings.
CVD awareness in the US
Awareness among women of heart disease being the leading cause of mortality has nearly doubled from 30% in 1997 to 54% in 2009, but the rate has since plateaued and awareness among racial/ethnic minorities lagged compared to white women [10, 11]. Although awareness of atypical signs of heart attack has modestly increased from 10% in 1997 to 18% in 2012 and awareness to call 9-1-1 if experiencing signs of a heart attack rose from 53% in 2009 to 65% in 2012, these data underscore the fact that awareness gaps remain [11]. More recent data from the Women’s Heart Alliance survey demonstrated only 55% of women were aware of CVD being leading cause of mortality. Additionally, awareness is lower in younger women, racial/ethnic minorities, and those women with lower education and lesser income [12]. Overall awareness rates of CVD risks and mortality have increased, although remain suboptimal, yet much more efforts are needed to further reduce knowledge gaps, especially among racial/ethnic minority women and those from lower socioeconomic status.
Physician awareness of CVD in women is harder to assess due to the scarcity of data. Underutilization of preventative therapies and CVD guidelines in women has been associated with physicians’ lower perceived risks of CVD in women [3, 13]. In 2004, less than one in five physicians were aware that more women than men died each year from CVD based on an online national survey of physicians [3]. More recent data from The Women’s Heart Alliance in 2014 demonstrated only 22% of primary care physicians and 42% of cardiologists felt extremely prepared to assess CVD risks in women, although most did not feel that they received adequate training. Furthermore, the implementation of the AHA’s guidelines for CVD risk assessment in women was very low, only 16% of primary care physicians and 22% of cardiologists [12]. The limited application of CVD guidelines in women is unacceptable. Increased efforts to improve understanding of sex-based differences in CVD and to educate trainees and practicing physicians regarding the presence and adoption of CVD prevention are imperative.
HCW: specialized areas of care for women
A comprehensive HCW and CVD care model includes a team-based approach, consisting of CV subspecialty physicians and certified nurse practitioners, with available multidisciplinary and collaborative consultative resources to provide complete nutritional, physical activity, cognitive, behavioral, rehabilitative, complementary, integrative, interventional, and surgical consultation [14]. HCW provide the organization and structure to bring together multidiscipline and integrated care for women. Table 1 shows the special areas of focus that can be included in a HCW and the women who benefit from these programs.
Heart disease and pregnancy
From 2011 to 2013, the leading cause of maternal mortality in the US was CVD, accounting for 15.5% in 2013. However altogether, cardiovascular-related diseases (cardiovascular, cardiomyopathy, hypertensive disorder of pregnancy, and cerebrovascular accident) account for 40.5% of pregnancy-related deaths [15, 16]. Maternal mortality in the US has more than doubled over the last 25 years, increasing from 7.2 to 17.3 per 100,000 live births between 1987 and 2013 [15, 16], while declining in other developed countries [17]. Studies show that an increasing number of pregnant women in the US have chronic health conditions, including hypertension, diabetes, and heart disease [15]. Racial disparity in pregnancy-related deaths is even more disturbing. Between 2011 and 2013, pregnancy-related mortality ratios were 12.7 deaths per 100,000 live births for white women, 43.5 for black women, and 14.4 for women of other races [16]. This alarming increase of cardiovascular disease affecting childbearing women is especially devastating for the family and underscores the importance of specialty care for these women.
These high-risk pregnant patients with cardiovascular disease require a multispecialty team including healthcare providers from obstetrics and gynecology, maternal fetal medicine, internal medicine, cardiovascular disease, and pharmacology. HCW often have cardiologists who specialize in gravid patients with cardiovascular disease. The field of gestational cardiology, which encompasses hypertension disorders of pregnancy and gestational diabetes, is growing and delivering specialized care for women during pregnancy [9]. A keen knowledge of the physiology of pregnancy and how the hemodynamic changes might affect a particular cardiac condition is critical for the proper management of these patients and is best served in a subspecialty clinic such as a HCW. Also, research has shown that pregnancy is the equivalent of a metabolic stress test for the heart [18]. Women with pregnancy-related complications need follow-up after their pregnancies to reduce CV risk factors and further improve CVD mortality in these women.
Heart disease and neuro-cognitive disease
Advances in the management of CVD have contributed to decreased CVD-related mortality among women [6] and regularly survive to their eighth–tenth decades. This has resulted in increased prevalence of cognitive impairment (CI). Of great concern, statistics indicate that about two thirds of those diagnosed with dementia due to Alzheimer’s disease (AD) are women. Patients with midlife hypertension, diabetes, obesity, and strokes can also have CI [19]. Treatment of chronic medical disease and modification of lifestyle factors associated with CI could decrease the incidence of dementia [20]. A study showed that seven modifiable risk factors, six of which are CVD risk factors (diabetes, midlife hypertension, midlife obesity, smoking, depression, physical inactivity), and cognitive inactivity or low educational attainment accounts for up to half of all AD cases worldwide [21]. Modification (10–25% reduction) in all the seven risk factors could potentially prevent as many as 1.1–3.0 million AD cases worldwide [21]. Women with CVD are at especially high risk for CI and dementia [22]. One academic HCW practice (Rush Heart Center for Women) has added cognitive/brain health integration with heart disease evaluation and treatment. This clinic utilizes a new model for risk management and prevention of CI in patients with CVD. A diverse team of healthcare providers deliver care as a team including a cognitive neurologist, emphasizing reduction of modifiable CVD, stroke, and AD risk factors [23].
Cardio-oncology
Advances in cancer treatment have led to improved survival of cancer patients; however, the treatments used to cure cancer unfortunately can have untoward cardiotoxicities, including heart failure, arrhythmias, pericarditis, valvular disease, and coronary ischemia. These toxicities of cancer therapy are more frequent than previously reported and may contribute to morbidity and mortality in cancer survivors. The field of cardio-oncology has emerged to provide care of the cancer patient who develops CVD secondary to their cancer therapy or who has preexisting CVD [24].
Mortality in older breast cancer survivors is more likely from other diseases other than breast cancer itself, and CVD is the most frequent cause [25, 26]. Understanding the overlap of CVD and breast cancer risks factors as well as addressing CVD risks prior to, during, and post-cancer treatment is essential. It is well known that anthracycline exposure can result in myocardial toxicity, myocyte damage, and eventual heart failure. More recent treatment like HER-2-targeted therapies in breast cancer patients has also been shown to result in heart failure, which is mostly reversible; however, when used as adjuvant therapy, the myocardial toxicity risks can be higher. Additionally, other breast cancer therapies such as alkylating agents, taxanes, and antimetabolites; endocrine therapies; and radiation therapy can also have cardiotoxicities that impact overall morbidity and mortality in women with breast cancer and survivors. Awareness of potential early and latent CVD cardiotoxicities is imperative in the clinical care of breast cancer patients [27]. Some HCW have established a cardio-oncology clinic within their center while others have developed strong collaborative efforts with their institution’s cardio-oncology programs.
Community CVD screening and education/public health
A woman-centered holistic health care delivery approach which is inclusive of diverse factors that are culturally tailored to the individual woman is necessary to eliminate disparities of CV health care [28]. HCW can best address these disparities by partnering with the communities with high-risk patients. HCW community-based programs are working to address many of the barriers to care faced by the women in socioeconomically disadvantaged communities [29]. This is particularly important for African-American and Latino women who are at high risk for heart disease [30]. The HCW at Emory University developed a program to screen 10,000 African-American women in the Atlanta area for hypertension and CVD risk factors. The screenings are provided at churches and shopping centers in partnership with community organizations in locations most likely to serve high-risk women. Women need to be empowered to personalize and translate awareness and knowledge of heart healthy living as an ongoing process. Fostering a personal commitment to heart health and wellness combined with risk factor modification and appropriate gender-specific diagnostic and treatment approaches customized for the unique physical, mental, and social well-being of individual women is essential [31].
Partnering with special CVD interests/rare diseases
Research and data on disorders that are more common or more significant in women can be collected more easily through large data bases used at HCW. Multiple HCW across the country partner with these and many other organizations to provide evidence-based guideline-directed care and enroll large numbers of patients in registries and research studies. These are just a few examples of areas of expertise and special focus that are being addressed by HCW nationwide.
WomenHeart
WomenHeart is a national coalition for women with heart disease with a membership to 20,000 women living with and at-risk for heart disease, friends and family members, health care professionals, and media nationwide. The organization has trained more than 750 community educators via the WomenHeart Science & Leadership Symposium in collaboration with Mayo Clinic HCW to serve in different capacities to support other women with or at risk for heart disease as well as disseminate knowledge about heart disease in women. In addition, they formed the WomenHeart National Hospital Alliance (NHA) which is a partnership with hospitals to ensure that women with heart disease every community have access to information, education, and patient support services. They receive funding from different sources to help hospitals in disadvantaged neighborhoods to have access to the WomenHeart services including access to the training and technical assistance needed to start a post-discharge support group for your women with or at risk for heart disease.
SCAD Alliance
Spontaneous coronary artery dissection (SCAD) is frequently misdiagnosed or underdiagnosed, and it is a condition that occurs more frequently in younger women with minimal coronary atherosclerotic risk factors [32, 33]. Patients with SCAD often present with an acute coronary syndrome, myocardial infarction, and in some cases sudden death. A recent scientific statement from the AHA provides some further insight into SCAD, yet many knowledge gaps remain and more research is needed. The diagnosis of SCAD can have psychosocial effects of due to the dearth of data regarding management and prognosis [33]. Prior to 2013, there was very little available information or support groups for patients. The SCAD Alliance is a patient advocacy organization that was founded in 2013 with the mission to advance the science of SCAD through dissemination of information and expanded research. Additionally, SCAD Alliance collaborates with health care professionals from HCW, hospitals, patients, and other advocacy groups to advocate for prompt diagnosis of SCAD as well as to form collaborative research teams to investigate the current knowledge gaps in the management and prognosis of SCAD. Furthermore, SCAD Alliance’s website is a great resource for HCW to provide SCAD survivors and their families as well as health care professionals regarding the latest advances in SCAD. Additionally, SCAD Alliance has developed a registry (iSCAD) to collect data on the presentation, CVD risk factors, treatments, and outcomes of women and men who have had SCAD.
Lipoprotein(a) Foundation
The Lipoprotein(a) Foundation is a patient-founded, non-profit organization dedicated to preventing cardiovascular events due to high lipoprotein(a) [Lp(a)]. Women seem to have increased Lp(a) levels compared with men [34] with hormones and menopausal hormone therapy (MHT) also influencing circulating Lp(a) levels [35]. Estrogen and progestin therapy appears to have a more favorable effect (relative to placebo) in women with high initial Lp(a) levels than in women with low levels and may explain variations in how women respond to MHT [35, 36]. A study done in two HCW in collaboration showed a high prevalence of elevated Lp(a) among women presenting to a HCW. The presence of elevated Lp(a) may help identify women who may benefit from aggressive risk factor modification and pharmacologic therapy [37]. Partnership with this foundation and HCW may be beneficial by providing clinical trial participants to increase enrollment in studies. The foundation’s website directs women with elevated Lp(a), premature coronary artery disease (CAD), and family history of CAD to HCW who specialize in lipids and/or prevention.
FH Foundation
Familial hypercholesterolemia (FH) affects families with an autosomal dominance genetic inheritance that markedly increases premature atherosclerosis leading to premature CVD and death [38, 39]. Early identification of patients with FH is essential for timely intervention and treatment. Detection in a female is essential as these women need to start treatment before their childbearing years and the treatment will likely need to be interrupted during pregnancy. Women with FH need information and counseling on treatment before and after pregnancy. Some HCW partner with the FH Foundation to encourage women to join the CASCADE registry for FH and get proper education and treatment for their families and provide support during pregnancy and breastfeeding.
Conclusions
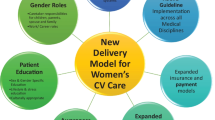
HCW have developed and spread throughout the private and academic communities in response to the increasing focus on women and CVD. Guideline-driven, evidence-based, and sex- and gender-specific evaluations; diagnostic testing; lifestyle management; and treatment recommendations have led to improved outcomes for women. These HCW continue to expand and provide multidiscipline and integrated care for women throughout the lifetime of a woman from her childbearing years to menopause and beyond. And these HCW have opportunities to engage the community and special areas of care such as gestational cardiology, cardio-oncology, and cardio-cognitive care. Figure 1 shows the components of a HCW and the interactions they have with other specialties and organizations. We believe HCW will continue to contribute to improved awareness, education, and patient care for women and provide sex-specific science, research, and education for all providers of women’s cardiovascular care.
Abbreviations
- AD:
-
Alzheimer’s disease
- AHA:
-
American Heart Association
- CAD:
-
coronary artery disease
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
cognitive impairment
- CV:
-
cardiovascular
- CVD:
-
cardiovascular disease
- FH:
-
familial hypercholesterolemia
- HCW:
-
heart centers for women
- Lp(a):
-
lipoprotein(a)
- MHT:
-
menopausal hormone therapy
- NHLBI:
-
National Heart, Lung, and Blood Institute
- SCAD:
-
spontaneous coronary artery dissection
- US:
-
United States
- WISEWOMAN:
-
Well-Integrated Screening and Evaluation for WOMen Across the Nation
References and Recommended Reading
Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women’s Heart Disease and Stroke Campaign Task Force. Arch Fam Med. 2000;9(6):506–15.
Mosca L, Manson JE, Sutherland SE, Langer RD, Manolio T, Barrett-Connor E. Cardiovascular disease in women: a statement for healthcare professionals from the American Heart Association. Writing Group. Circulation. 1997;96(7):2468–82.
Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510.
Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA. 1998;280(7):605–13.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–33.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492.
Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra-Strobos N, Fabunmi RP, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109(5):672–93.
Disease WTNCfWwH. National directory of women’s heart center. 2001.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123(11):1243–62.
Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3(2):120–7.
Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation 2013;127(11):1254–1263, e1-29.
Bairey Merz CN, Andersen H, Sprague E, Burns A, Keida M, Walsh MN, et al. Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the Women’s Heart Alliance. J Am Coll Cardiol. 2017;70:123–32.
Barnhart J, Lewis V, Houghton JL, Charney P. Physician knowledge levels and barriers to coronary risk prevention in women: survey results from the Women and Heart Disease Physician Education Initiative. Womens health issues. 2007;17:93-100.
Garcia M, Miller VM, Gulati M, Hayes SN, Manson JE, Wenger NK, et al. Focused cardiovascular care for women: the need and role in clinical practice. Mayo Clin Proc. 2016;91(2):226–40.
Hirshberg A, Srinivas SK. Epidemiology of maternal morbidity and mortality. Seminars in Perinatology: WB Saunders; 2017.
Centers for Disease Control and Prevention. Reproductive health https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html Published June 29, 2017 [October 22, 2017]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.
Collaborators GBDMM. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1775–1812.
Roberts JM, Hubel CA. Pregnancy: a screening test for later life cardiovascular disease. Womens Health Issues. 2010;20(5):304–7.
Launer LJ, Hughes T, Yu B, Masaki K, Petrovitch H, Ross GW, et al. Lowering midlife levels of systolic blood pressure as a public health strategy to reduce late-life dementia: perspective from the Honolulu Heart Program/Honolulu Asia Aging Study. Hypertension. 2010;55(6):1352–9.
Ritchie K, Carriere I, Ritchie CW, Berr C, Artero S, Ancelin ML. Designing prevention programmes to reduce incidence of dementia: prospective cohort study of modifiable risk factors. BMJ. 2010;341:c3885.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–28.
Alzheimer’s Association 2014 Alzheimer’s disease facts and figures. Alzheimers Dement: J Alzheimer’s Assoc. 2014;10(2):e47–92.
Garg AK, Verma P. Cardiovascular disease among South Asians. CMAJ : Can Med Assoc J = J Assoc Med Canadienne. 2010;182(12):1334. author reply
Barac A, Murtagh G, Carver JR, Chen MH, Freeman AM, Herrmann J, et al. Cardiovascular health of patients with cancer and cancer survivors: a roadmap to the next level. J Am Coll Cardiol. 2015;65(25):2739–46.
Chapman JA, Meng D, Shepherd L, Parulekar W, Ingle JN, Muss HB, et al. Competing causes of death from a randomized trial of extended adjuvant endocrine therapy for breast cancer. J Natl Cancer Inst. 2008;100(4):252–60.
Hanrahan EO, Gonzalez-Angulo AM, Giordano SH, Rouzier R, Broglio KR, Hortobagyi GN, et al. Overall survival and cause-specific mortality of patients with stage T1a,bN0M0 breast carcinoma. J Clin Oncol. 2007;25(31):4952–60.
Mehta LS, Watson KE, Barac A, Beckie TM, Bittner V, Cruz-Flores S, et al. Cardiovascular disease and breast cancer: where these entities intersect: a scientific statement from the American Heart Association. Circulation. 2018;137(8):e30–66.
Shaw LJ, Butler J. Targeting priority populations to reduce disparities in cardiovascular care: health equity for all. J Am Coll Cardiol. 2014;64(4):346–8.
Gilstrap LG, Malhotra R, Peltier-Saxe D, Slicas D, Pineda E, Culhane-Hermann C, et al. Community-based primary prevention programs decrease the rate of metabolic syndrome among socioeconomically disadvantaged women. Journal of women’s health (2002). 2013;22(4):322–9.
Hayes SN, Wood SF, Mieres JH, Campbell SM, Wenger NK. Taking a giant step toward women’s heart health: finding policy solutions to unanswered research questions. Womens Health Issues. 2015;25(5):429–32.
World Health Organization. Social determinants of health: women and gender equality. http://www.who.int/social_determinants/themes/womenandgender/en. World Health Organization, 2017 August 3, 2017. Report No.
Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133(9):916–47.
Hayes SN, Kim ESH, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation. 2018;137:e523–57.
Kostakou PM, Hatzigeorgiou G, Kolovou V, Mavrogeni S, Kolovou GD. Lipoprotein (a) evolution: possible benefits and harm. Genetic and non-genetic factors influencing its plasma levels. Curr Med Chem. 2017;24(10):969–78.
Shlipak MG, Simon JA, Vittinghoff E, Lin F, Barrett-Connor E, Knopp RH, et al. Estrogen and progestin, lipoprotein (a), and the risk of recurrent coronary heart disease events after menopause. JAMA. 2000;283(14):1845–52.
Suk Danik J, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), hormone replacement therapy, and risk of future cardiovascular events. J Am Coll Cardiol. 2008;52(2):124–31.
Costello BT, Silverman ER, Doukky R, Braun LT, Aggarwal NT, Deng Y, et al. Lipoprotein(a) and increased cardiovascular risk in women. Clin Cardiol. 2016;39(2):96–102.
Wong B, Kruse G, Kutikova L, Ray KK, Mata P, Bruckert E. Cardiovascular disease risk associated with familial hypercholesterolemia: a systematic review of the literature. Clin Ther. 2016;38(7):1696–709.
Kjaergaard KA, Christiansen MK, Schmidt M, Olsen MS, Jensen HK. Long-term cardiovascular risk in heterozygous familial hypercholesterolemia relatives identified by cascade screening. J Am Heart Assoc. 2017;6(6):e005435.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Women’s Health
Rights and permissions
About this article
Cite this article
Lundberg, G.P., Mehta, L.S. & Volgman, A.S. Specialized Care for Women: the Impact of Women’s Heart Centers. Curr Treat Options Cardio Med 20, 76 (2018). https://doi.org/10.1007/s11936-018-0656-5
Published:
DOI: https://doi.org/10.1007/s11936-018-0656-5