Opinion statement
Passive dissemination of guidelines in isolation is generally ineffective and results in only small changes in practice. The challenge is to motivate and support more physicians to routinely practice cardiovascular prevention. There is considerable potential to raise the standard of cardiovascular prevention through more effective lifestyle intervention, control of other risk factors and appropriate use of cardioprotective medication. A more comprehensive multidisciplinary and professional approach accessible to both patients with established disease as well as those who are at high risk of developing CVD and provided in each country by existing or adapted ‘prevention centres’ is needed. Cardiovascular prevention requires an integrated family-based approach, involving multidisciplinary teams of health care professionals, adapted to medical and cultural settings in each country in order to achieve better lifestyles, risk factor control and adherence with cardioprotective medications in our patients with coronary disease and to reduce their risk of recurrent cardiovascular events and improve quality of life and survival. Coronary intervention should always be followed by prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main objectives of cardiovascular disease (CVD) prevention are to reduce morbidity and mortality and increase the chances of a longer life expectancy [1–4, 5•, 6]. A wealth of scientific evidence from observational studies and randomised controlled trials now supports interventions in relation to lifestyle (smoking, diet and exercise), the treatment of hypertension, hyperlipidaemia and diabetes and the selective use of prophylactic drug therapies (antiplatelets, beta-blockers, ACE inhibitors/angiotensin receptor blockers (ARBs), lipid-modifying drugs and antithrombotics). All of these measures can reduce morbidity and mortality and improve quality of life in people with established coronary disease.
The European Society of Cardiology together with other partner societies has engaged in a comprehensive programme of CVD prevention in clinical practice since 1992. Guidelines on this important topic have been developed and updated at regular intervals over the last 15 years: 1994, 1998, 2003, 2007 and in 2012 [1–4, 5•]. The aim of the Joint European Societies (JES) guidelines on cardiovascular disease prevention is to improve the practice of cardiovascular prevention by encouraging the development of national guidance on cardiovascular disease prevention and its communication, implementation and evaluation through national societies in each country. Patients with coronary or other atherosclerotic cardiovascular disease, and those at high risk of developing CVD, have been defined as the highest clinical priorities for prevention. The 2012 Joint European Societies’ guidelines defined the lifestyle and risk factor goals for patients with established CHD and people at high CVD risk as follows: stop smoking, make healthy food choices and be physically active, a body mass index (BMI) <25 kg/m2, blood pressure <140/90 mmHg (<140/80 mmHg in patients with diabetes mellitus), LDL-cholesterol <1.8 mmol/L (<70 mg/dL) or at least 50 % reduction in people at very high risk and <2.5 mmol/L (<100 mg/dL) in people at high risk, glycated hemoglobin (HbA1C) <7.0 mmol/L (<53 mmol/mol) in people with diabetes mellitus and appropriate use of cardioprotective drug therapies [5•]. The objective was to agree a strategy on guideline implementation at a national level and the subsequent evaluation of cardiovascular prevention practice.
Surveys evaluating guideline implementations in clinical practice
EUROASPIRE surveys
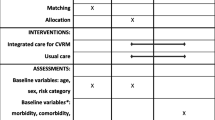
Guideline implementation in Europe was evaluated in a cross-sectional survey called European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) starting in 1995–1996 in nine countries under the auspices of the Working Group on Epidemiology and Prevention, and this was followed by a second and third surveys in 1999–2000 (15 countries), 2006–2008 (22 countries) through the Euro Heart Survey programme and again in 2012–2014 (26 countries) under the auspices of the European Society of Cardiology, EURObservational Research Programme [7–12, 13•, 14–16]. EUROASPIRE surveys were designed to identify risk factors in coronary patients, describe their management through lifestyle and use of drug therapies and provide an objective assessment of clinical implementation of current scientific knowledge. The objective of each survey was to determine whether clinical practice was achieving the standards set in the CVD prevention guidelines and whether there were any changes over time in lifestyle, risk factor and therapeutic management. The methodology used in EUROASPIRE I was duplicated in the second, third and forth surveys with standardised interviews and measurements, rather than data from medical records, which were often incomplete for risk factor recording, and a central laboratory for lipid and glucose analyses, so that time trends between surveys could be described. Therefore, this survey provided high-quality comparative information on preventive care. The fourth EUROASPIRE IV survey on cardiovascular disease prevention and diabetes merged with the Euro Heart Survey on diabetes mellitus [17–19] and incorporated an assessment of dysglycaemia (impaired fasting glycaemia, impaired glucose tolerance and new diabetes) in all patients. Consecutive patients, men and women (≥18 and <80 years of age at the time of their index event or procedure), with the following first or recurrent clinical diagnoses or treatments for CHD were retrospectively identified from diagnostic registers, hospital discharge lists or other sources: (i) elective or emergency CABG, (ii) elective or emergency PCI, (iii) acute myocardial infarction and (iv) acute myocardial ischaemia. The starting date for identification was ≥6 months and <3 years prior to the expected date of the study interview.
In the most recent EUROASPIRE IV survey, 7998 coronary patients were interviewed at least 6 months after admission for an acute coronary event or procedure. The results showed that a large majority of coronary patients did not achieve the guideline standards for secondary prevention with high prevalences of persistent smoking, unhealthy diets, physical inactivity and consequently most patients being overweight or obese with a high prevalence of diabetes [13•, 14]. A total of 16 % of patients smoked cigarettes, and 49 % of those smoking at the time of the event were persistent smokers, 60 % reported little or no physical activity, 38 % were obese (BMI ≥30 kg/m2) and 58 % centrally obese (waist circumference ≥102 cm in men or ≥88 cm in women). Risk factor control was inadequate despite high reported use of medications, and there were large variations in secondary prevention practice between countries (Fig. 1). Overall, 43 % had blood pressure ≥140/90 mmHg (≥140/80 mmHg in people with diabetes), 80 % had LDL-cholesterol ≥1.8 mmol/L (>70 mg/dL) and 27 % reported having diabetes. Cardioprotective medication was antiplatelets 94 %, beta-blockers 83 %, ACE inhibitors/ARBs 75 % and statins 86 %.
A comparison across the most recent three surveys provided a unique description of time trends for secondary prevention in the same countries, geographic areas and hospitals over a period of 14 years [15]. The results showed adverse lifestyle trends, a substantial increase in obesity, central obesity and diabetes and high prevalences of persistent smoking among younger patients and especially women. Although blood pressure and lipid management improved, these risk factors were still not optimally controlled. There appeared to be an apparent ceiling to prescribing cardioprotective medication, as their use did not change by comparison with the EUROASPIRE III. The rising prevalence of obesity and central obesity was probably contributing to the raising prevalence of diabetes, an absolute increase of about 9 % over 14 years, increasing the risk of recurrent macrovascular disease, the development of microvascular disease and a further reduction in life expectancy.
Other multinational studies
The results of EUROASPIRE IV are in accordance with earlier multinational surveys conducted in Europe, USA and other parts of the world, reporting high prevalences and an inadequate control of CVD risk factors in patients with CHD [20–32]. Although most patients were receiving evidence-based secondary preventive therapy, many subjects from all regions did not reach recommended secondary prevention goals. The results of the Reduction of Atherothrombosis for Continued Health (REACH) Registry [20], the WHO study on Prevention of Recurrences of Myocardial Infarction and Stroke (WHO-PREMISE) [21], STabilization of Atherosclerotic plaque By Initiation of darapLadIb TherapY (STABILITY) trial [22] and The Prospective Urban Rural Epidemiology (PURE) study [23, 24] demonstrated high prevalences and poor control of cardiovascular risk factors in patients with CHD. The results from REACH Registry showed that across the USA, 82 % of patients with known atherosclerotic disease were receiving at least one antiplatelet therapy, 83 % were on lipid-lowering medication, 65 % were on ACE inhibitors or ARBs and 57 % were on beta-blockers [21]. The report of STABILITY trial in 15,828 patients with CHD from 39 countries on five continents demonstrated even higher proportions of patients on cadioprotective medications, with 97 % being on statins, 96 % on antiplatelet therapy, 79 % on beta-blockers and 77 % on ACE inhibitor/ARBs [22]. However, a large proportion of patients did not achieve guideline-recommended targets; in 29 %, LDL-cholesterol was >2.5 mmol/L and in 46 % blood pressure was ≥140/90 mmHg or ≥130/80 mmHg in those with diabetes or renal impairment. A total of 36 % were obese, 54 % were centrally obese and 18 % were smoking. The regional differences in risk factor prevalence and target achievement were more marked for LDL-cholesterol and obesity. Findings from the PURE study among 7519 patients with self-reported CVD (CHD or stroke) from 17 high-, middle- or low-income countries worldwide demonstrated low prevalence of healthy lifestyles, with 18 % continuing to smoke, only 35 % undertaking high levels of work- or leisure-related physical activity and 39 % having healthy diets [23]. The use of cardioprotective medications was considerably lower than in EUROASPIRE IV, with only 25 % being on antiplatelet drugs, 17 % on beta-blockers, 20 % on ACE inhibitors or ARBs and 15 % on statins [24].
The 9-year trends (1998–2006) in achievement of risk factor goals in patients with cardiovascular disease showed that adherence to guidelines was suboptimal and lower in Europe than in the USA [29]. The results from six consecutive National Health and Nutrition Examination Surveys (NHANES) from 1999–2000 to 2009–2010 showed improvement of LDL-C. However, in 2009–2010, only 58 % of individuals with CHD or risk equivalents had controlled LDL-C [30]. In patients with CVD and diabetes type 2, NHANES reported significant improvements in blood pressure, LDL-cholesterol and triglycerides but only modest improvements in lifestyle [31]. The NHANES data from 2007 to 2010 in patients with CHD showed that the use of beta-blockers, ACE inhibitors/ARBs and lipid-lowering therapies was 55, 45 and 62 %, respectively. The non-smoking status and control of blood pressure, LDL-cholesterol and for those with diabetes, HbA1c was 73, 67, 59 and 60 %, and only 20 and 29 % were at the recommended BMI and waist circumference targets, respectively [32].
The results of EUROASPIRE and other similar surveys conducted in EUROPE, USA or other parts of the world revealed that despite the compelling scientific evidence for prevention and rehabilitation following the development of coronary disease, a large majority of coronary patients are failing to achieve the lifestyle, risk factor and therapeutic targets set by the prevention guidelines. There is a large variation between countries both in lifestyle and risk factor management, the use of cardioprotective medications and the provision of cardiac prevention and rehabilitation services.
Secondary prevention or cardiac rehabilitation
Lifestyle and risk factor management
There is a wealth of evidence that achieving a healthier lifestyle reduces the risk of recurrent cardiovascular events in coronary patients and improves quality of life. The effect of smoking cessation on total and cardiovascular mortality is supported by a number of systematic reviews and randomised controlled trials [33–35]. A meta-analysis of smoking cessation after a myocardial infarction showed a relative risk reduction of coronary mortality by 46 % in those who stopped smoking [33]. Cochrane meta-analysis of 20 prospective cohort studies on smoking cessation with mean follow-up 3–7 years showed that stopping smoking in patients with CHD reduced all-cause mortality by 36 % [34]. All cigarette smokers should be professionally encouraged and offered pharmacological support to stop smoking. A specialist smoking cessation clinic achieved abstinence in one third of patients with cardiovascular disease, which was associated with significant reduction in rehospitalisations and all-cause mortality after 2 years [35]. In a randomised controlled trial of a nurse-led behavioural smoking intervention in high-risk persistent smokers, supplemented with optional varenicline, 51 % of vascular patients had stopped smoking at 16 weeks [36].
The 2012 JES guidelines on CVD prevention recommended higher blood pressure target of <140/90 mmHg (<140/80 mmHg in patients with diabetes) as the previous target was not consistently supported by trial evidence. Post hoc analyses of large-scale trials (ONTARGET, INVEST, VALUE) suggested that there might be no advantage or even harm in lowering systolic blood pressure (SBP) below 130 mmHg in patients with coronary disease and a J-curve phenomenon for SBP <130 mmHg cannot be excluded [37]. Following myocardial infarction, elevated blood pressure is associated with an increased risk of reinfarction, coronary death or stroke. All coronary patients require specific lifestyle advice and where appropriate, antihypertensive medication. Lifestyle modification can reduce blood pressure and the number of drugs required to control it. The meta-analysis of randomised trials of blood pressure-lowering medication in patients with coronary disease showed that the reduction of systolic blood pressure by 10 mmHg or diastolic blood pressure by 5 mmHg reduces CHD events (fatal and non-fatal) by about a quarter (RR 0.76; 95 % CI 0.68–0.86) and stroke by about a third (RR 0.65; 95 % CI 0.53–0.80) [38].
Large-scale clinical trials and meta-analyses have demonstrated that cholesterol-lowering therapies, especially statins, reduce recurrent cardiovascular events and can prolong survival in patients with established CVD. A prospective meta-analysis of data from 90,056 individuals in 14 randomised trials showed that statin therapy can safely reduce the 5-year incidence of major coronary events, coronary revascularisation and stroke by about one fifth per mmol/L reduction in LDL-cholesterol (RR 0.79; 95 % CI 0.77–0.81), largely irrespective of the initial lipid profile or other presenting characteristics [39]. Recent trials addressing more aggressive lipid-lowering therapy confirmed that lowering LDL-cholesterol to ≤1.8 mmol/L (<70 mg/dL) is associated with the lowest risk of recurrent CVD events in patients with established CVD [40]. Therefore, in the most recent 2012 JES5 guidelines, the recommended target for LDL-cholesterol was reduced to <1.8 mmol/L or at least 50 % reduction from baseline LDL-cholesterol. As a result, in order to achieve this lower target, a large majority of coronary patients will require more intensive cholesterol management and optimal use of lipid-lowering drug therapies. The new ACC/AHA guidelines do not have a specific numerical LDL-cholesterol target and recommend a statin treatment strategy of high-intensity statins for patients with coronary heart disease [41]. There was a 2-fold increase in the proportion of patients on high-intensity statins between EUROASPIRE III and IV, but still, less than half of patients in the most recent study achieved this treatment goal.
The risk of dying for patients with coronary artery disease and diabetes is substantially higher than for those free from diabetes [42]. In a mortality follow-up of the EUROASPIRE I cohort of coronary patients, the independent modifiable risk factors associated with an increased risk of dying were smoking, cholesterol and glucose [43]. The Euro Heart Survey on diabetes and the heart demonstrated that abnormal glucose regulation affected a majority of patients with coronary artery disease [17]. Patients with diabetes compared to those without diabetes had a much poorer prognosis, which could be improved considerably with multifactorial evidence-based management [18]. A meta-analysis of intensive vs conventional glycaemic control including the UKPDS, ACCORD, ADVANCE and VADT trials found a significant reduction in CHD and CVD events but no reduction in cardiovascular or total mortality and increased the risk for severe hypoglycemia [44, 45]. Using a multifactorial, comprehensive and target-driven intervention directed towards lifestyle, risk factor control and use of evidence-based medications as recommended in available guidelines can effectively reduce microvascular and to a lesser degree macrovascular complications in patients with type 2 DM [42, 46].
The following cardioprotective drug therapies shown to reduce morbidity and mortality in clinical trials in addition to drugs used for treatment of elevated blood pressure and glucose are recommended in the JES5 guidelines for CVD prevention: aspirin or other platelet-modifying drugs in all patients, beta-blockers in those after myocardial infarction, ACE inhibitors/ARBs in those with impaired left ventricular function and statins in all patients [5•]. Possible explanations for poor blood pressure and lipid control can be that treatment is initiated with low dose prescriptions, and then not titrating up, as well as with poor patient adherence, or both. Therefore, many patients will require more intensive blood pressure and cholesterol management and optimal use of cardioprotective medications to achieve their targets. Patients with poor adherence have higher cardiovascular event rates and all-cause mortality and increased health care costs compared to those with good adherence [47, 48]. Improving treatment adherence is a very important step in optimizing cardiovascular risk factor management. A meta-analysis of observational studies on the association between medication adherence and mortality demonstrated that good adherence is associated with positive health outcomes [49]. There is further potential to reduce recurrent cardiovascular events through optimizing the prescription of cardioprotective medications, combining different drugs and up-titrating them to the doses showing efficacy and safety in randomised controlled clinical trials and by improving patient adherence over long term.
Cardiac rehabilitation
There is compelling scientific evidence that cardiac rehabilitation is an effective treatment for patients with CHD and reduces both cardiac and total mortality [50–55]. A systematic review of 47 studies including 10,794 patients randomised to exercise-based cardiac rehabilitation or usual care demonstrated that exercise-based cardiac rehabilitation was effective in reducing total and cardiovascular mortality in medium to longer term studies [RR 0.87 (95 % CI 0.75, 0.99) and 0.74 (95 % CI 0.63, 0.87)], respectively, and hospital admissions in shorter term studies [RR 0.69 (95 % CI 0.51, 0.93)] [51].
The contribution of secondary prevention programs with or without exercise was evaluated in a separate meta-analysis of 63 randomised controlled trials including 21,295 patients with CHD [52]. Secondary prevention programs reduced all-cause mortality [RR 0.85 (95 % CI 0.77 to 0.94], and this result differed over time: RR 0.97 (95 % CI 0.82 to 1.14) at 12 months, RR 0.53 (95 % CI 0.35 to 0.81) at 24 months and RR 0.77 (95 % CI 0.63 to 0.93) at 5 years. The risk ratio for recurrent myocardial infarction was 0.83 (95 % CI 0.74 to 0.94) over a median follow-up of 12 months. The effects on mortality and myocardial infarction were similar for programs without exercise, programs with exercise and exercise only programs.
Recent data from the OASIS clinical trial of 18,809 patients with acute coronary syndromes showed that adherence to behavioural advice (diet, exercise and smoking cessation) after acute coronary syndrome was associated with a substantially lower risk of recurrent cardiovascular events [53]. Quitting smoking and diet and exercise adherence were associated with a decreased risk of myocardial infarction [odds ratio 0.57; 95 % CI, 0.36 to 0.89 and 0.52; 95 % CI, 0.4 to 0.69, respectively]. Patients who reported persistent smoking and non-adherence to diet and exercise had a 3.8-fold (95 % CI, 2.5 to 5.9) increased risk of myocardial infarction/stroke/death compared with never smokers who modified diet and exercise. A systematic review and meta-analysis including 23 trials (involving 11,085 randomised patients) demonstrated that lifestyle modification programs were associated with reduced all-cause and cardiac mortality, and cardiac readmissions and non-fatal reinfarctions [54]. Furthermore, lifestyle modification programs positively affected risk factors and related lifestyle behaviours, and some of these benefits were maintained at long-term follow-up. Improvements in dietary and exercise behaviour were greater for programs incorporating all four self-regulation techniques (i.e. goal setting, self-monitoring, planning and feedback techniques) compared to interventions that included none of these techniques. A post hoc analysis of Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) showed that multiple risk factors (RF) control of a protocol-guided intensive medical therapy in patients with coronary disease and diabetes mellitus type 2 is feasible and is related to cardiovascular morbidity and mortality [55]. This non-randomised analysis evaluated the relationship between survival/cardiovascular events and control of six RFs (no smoking, non-high-density lipoprotein cholesterol <130 mg/dL, triglycerides <150 mg/dL, blood pressure <130 mmHg, HbA1c <7 %). In 2265 patients followed up for 5 years, the number of RFs at target was strongly related to death and the composite of death, myocardial infarction and stroke. Participants with zero to two RFs in control during follow-up had a 2-fold higher risk of death (hazard ratio 2.0; 95 % confidence interval 1.3 to 3.3; p = 0.0031) and a 1.7-fold higher risk of the composite endpoint (hazard ratio 1.7; 95 % confidence interval 1.2 to 2.5; p = 0.0043), compared with those with six RFs in control.
However, despite the strength of this evidence, cardiac rehabilitation continues to be considerably underused with poor referral and a low participation rate. Only half of EUROASPIRE IV patients were advised to participate in a cardiac rehabilitation program (CRP) after their coronary event, and four fifths of them attended at least half of the sessions, only two fifths (41 %) of the whole study population [13•]. These results are similar to those of the EUROASPIRE III survey, which demonstrated that only two in five coronary patients reported receiving advice to follow a CRP and only one third actually attended some form of cardiac rehabilitation [56]. So, there is considerable potential to further reduce the risk of CVD in existing cardiac rehabilitation programs. Recent studies, such as EUROACTION and GlObal Secondary Prevention strategiEs to Limit (GOSPEL) studies, provided scientific evidence for the beneficial long-term effect and improved prognosis in patients with CHD [57, 58]. A health economics analysis from EUROASPIRE III showed mainly favourable results with an average incremental cost-effectiveness ratio (ICER) of Euro12,484 per quality-adjusted life year (QALY). [59] Therefore, all patients should be offered a structured, multidisciplinary prevention and rehabilitation program that gives an opportunity for a comprehensive evaluation and cardiovascular risk reduction.
The results of EUROASPIRE and other studies in the USA and different parts of the world show that despite the existence and wide dissemination of evidence-based guidelines, their implementation in everyday clinical practice is far from optimal. The high prevalences of smoking, unhealthy diet, physical inactivity, obesity, central obesity and diabetes are alarming. Although most patients are receiving evidence-based secondary preventive therapy, large proportions of coronary patients do not achieve their lifestyle, risk factor and therapeutic targets for CVD prevention. In addition, those groups less likely to be referred, to attend and to complete such programs are often those in greatest need: elderly, women, low social class and ethnic minority groups. The clinical challenge is to increase access to and participation in comprehensive prevention and rehabilitation programs for all patients with atherosclerotic disease.
Conclusions
At present, the health care systems in Europe are predominantly focused on patients with coronary disease and especially those who have had a myocardial infarction or been revascularised through medical interventions, devices and pharmacological treatments, and not on addressing the underlying causes of the disease to prevent further morbidity and mortality. Patients require professional support to make lifestyle changes and to have their other risk factors monitored and managed according to the standards defined in the guidelines. All patients with atherosclerotic cardiovascular disease—coronary heart disease, stroke, peripheral arterial disease—are eligible for secondary prevention. The distinction between cardiac rehabilitation and secondary prevention is artificial, and the meta-analyses demonstrate, from different perspectives, the benefits of a comprehensive approach to reducing total cardiovascular risk. However good our clinical prevention programs are, ultimately it is very difficult for patients to quit smoking, eat healthily and be physically active for the rest of their lives if the society in which they live is not conducive to a healthy lifestyle. What is required is a comprehensive risk reduction approach to lifestyle, risk factor and therapeutic management to reduce total cardiovascular risk. A modern cardiovascular prevention program could be created by integrating ‘cardiac rehabilitation’ and ‘secondary prevention’ to deliver one comprehensive risk reduction service. This modern program will address lifestyle through a behavioural approach to smoking cessation, healthy eating, physical activity and weight management. At the same time, it will address effective therapeutic control of blood pressure, lipids and glucose, and prescribe and support adherence to cardioprotective drug therapies. All patients with acute coronary syndromes, or any other atherosclerotic disease, should have guaranteed access to a modern cardiovascular prevention program in every country.
References and Recommended Reading
Papers of particular interest, published recently have been highlighted as: • Of importance
Pyörälä K, De Backer G, Graham I, Poole-Wilson PA, Wood D. Prevention of coronary heart disease in clinical practice. Recommendations of the Task Force of the European Society of Cardiology, European Atherosclerotic Society and European Society of Hypertension. Eur Heart J. 1994;15:1300–31.
Wood D, De Backer G, Faergeman D, Graham I, Mancia G, Pyörälä K. Prevention of coronary heart disease in clinical practice. Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J. 1998;19:1434–503.
De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2003;10 Suppl 1:S1–S78.
Graham I, Atar D, Borch-Johnsen K, et al. European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14 Suppl 2:S1–S113.
Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2012;33:1635–701. The most recent JES guidelines on CVD prevention in clinical practice.
Smith Jr SC, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–73.
EUROASPIRE Study Group. EUROASPIRE. A European Society of Cardiology survey of secondary prevention of coronary heart disease: principal results. Eur Heart J. 1997;18:1569–82.
EUROASPIRE Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries. Principal results from EUROASPIRE II. Euro Heart Survey Programme. Eur Heart J. 2001;22.
EUROASPIRE Study Group. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. Lancet. 2001;357:995–1001.
Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U, on behalf of EUROASPIRE study Group. EUROASPIRE III: A survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from twenty two European countries. EUROASPIRE Study Group. Europ J Cardiovasc Prev Rehab 2009;16:121–37.
Kotseva K, Wood D, De Backer G, De Bacquer D,Pyorala K, Keil U, on behalf of EUROASPIRE study Group Cardiovascular prevention guidelines - the clinical reality: a comparison of EUROASPIRE I, II and III surveys in 8 European countries. Lancet 2009;372:929–40.
Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U, et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high risk subjects in general practice: cross-sectional survey in 12 European countries. Eur J Cardiovasc Prev Rehab. 2010;17:530–40.
Kotseva K, Wood D, De Bacquer D, et al. On behalf of the EUROASPIRE Investigators. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from twenty four European countries. Eur J Prev Cardiol. 2015. doi:10.1177/2047487315569401. EUROASPIRE surveys are widely published and their results demonstrate the implementation of cardiovascular disease prevention guidelines in everyday clinical practice in Europe.
Kotseva K, Rydén L, De Backer G, De Bacquer D, Wood D. EURObservational Research Programme: EUROASPIRE survey of cardiovascular prevention and diabetes in 24 countries in Europe. Eur Heart J. 2015;36:950–55.
Kotseva K, De Bacquer D, Jennings C, et al, on behalf of EUROASPIRE Investigators. Adverse lifestyle trends counter improvements in cardiovascular risk factor management in coronary patients: results from three EUROASPIRE cross sectional surveys 1999 – 2013 of the European Society of Cardiology. JACC 2015;66:1633–36
Gyberg V, De Bacquer D, Kotseva K, et al, on behalf of EUROASPIRE Investigators. Screening for dysglycemia in patients with coronary artery disease as reflected by fasting glucose, oral glucose tolerance test and HbA1c. A report from EUROASPIRE IV. Eur Heart J 2015; doi:10.1093/eurheartj/ehv008
Bartnik M, Ryden L, Ferrari R, et al., on behalf of Euro Heart Survey Investigators. The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The Euro Heart Survey on diabetes and the heart. Eur Heart J. 2004;25:1880–90
Lenzen M, Rydén L, Ohrvik J, et al. Diabetes known or newly detected, but not impaired glucose regulation, has a negative influence on 1-year outcome in patients with coronary artery disease: a report from the Euro Heart Survey on Diabetes and the Heart. Eur Heart J. 2006;27:2969–74.
Anselmino M, Bartni M, Öhrvik J, Rydén L. The Euro Heart Survey on diabetes and the heart. Int Diabetes Monitor. 2010;22:1–9.
Mehta RH, Bhatt DL, Steg PG, et al. REACH Registry Investigators. Modifiable risk factors control and its relationship with 1 year outcomes after coronary artery bypass surgery: insights from the REACH registry. Eur Heart J. 2008;29:3052–60.
Mendis S, Abegunde D, Yusuf S, Ebrahim S, Shaper G, Ghannem H. Shengelia B (WHO-PREMISE (Phase I) study group). Bull World Health Organ. 2005;83:820–8.
Vedin O, Hagstrom E, Stewart R, et al. Secondary prevention and risk factor target achievement in a global, high-risk population with established coronary heart disease: baseline results from the STABILITY study. Eur J Prev Cardiol. 2013;20:678–85.
Teo K, Lear S, Islam S, PURE Investigators, et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: The Prospective Urban Rural Epidemiology (PURE) study. JAMA. 2013;309:1613–21.
Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–43.
Libungan B, Stensdotter L, Hjalmarson A. Secondary prevention in coronary artery disease. Achieved goals and possibilities for improvements. Int J Cardiol. 2012;161:18–24.
Farkouh ME, Boden WE, Bittner V, et al. Risk factor control for coronary artery disease secondary prevention in large randomized trials. J Am Coll Cardiol. 2013;61:1607–15.
Sabouret P, Asseman P, Dallongeville J, Dujardin JJ, Philippe F, Herrmann MA, Montalescot G. CONNECT Study Investigators. Observational study of adherence to European clinical practice guidelines for the management of acute coronary syndrome in revascularized versus non-revascularized patients - the CONNECT Study. Arch Cardiovasc Diseases 2010;103:437–46.
Hermans MP, Castro Cabezas M, Strandberg T, et al. Centralized Pan-European survey on the under-treatment of hypercholesterolaemia (CEPHEUS): overall findings from eight countries. Curr Med Res Opin. 2010;26:445–54.
Steinberg BA, Bhatt DL, Mehta S, et al. Nine-year trends in achievement of risk factor goals in the US and European outpatients with cardiovascular disease. Am Heart J. 2008;156:719–27.
Muntnera P, Levitana E, Brown TM, et al. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among US adults from 1999–2000 through 2009–2010. Am J Cardiol. 2013;112:664–70.
Wong ND, Patao C, Wong K, et al. Trends in control of cardiovascular risk factors among US adults with type 2 diabetes from 1999 to 2010: comparison by prevalent cardiovascular disease status. Diabetes Vasc Dis Res. 2013;10:505–13.
Tang L, Patao C, Chuang J, Wong ND. Cardiovascular risk factor control and adherence to recommended lifestyle and medical therapies in persons with coronary heart disease (from the National Health and Nutrition Examination Survey 2007-2010). Am J Cardiol. 2013;112:1126–32.
Wilson K, Gibson N, Willan A, Cook D. Effect of smoking cessation on mortality after myocardial infarction: meta-analysis of cohort studies. Arch Intern Med. 2000;160:939–44.
Chritchley J, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003;290:86–97.
Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168:1950–60.
Jennings C, Kotseva K, De Bacquer D, et al, on behalf of EUROACTION PLUS Study Group. Effectiveness of a preventive cardiology programme for high CVDrisk persistent smokers: the EUROACTION PLUS Varenicline trial. Eur Heart J 2014 doi:10.1093/eurheartj/ehu051.
Mancia G, Laurent S, Fagard R, et al. ESH/ESC Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; doi:10.1093/eurheartj/eht151.
Law MR, Morris JK, Wald NJ. Blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of cholesterol = lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78.
Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Ryden L, Grant P, Anker S, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. The task force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in colaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013. doi:10.1093/eurheartj/eht108.
De Bacquer D, Dallongeville J, Kotseva K, et al. Residual risk of cardiovascular mortality in patients with coronary heart disease: the EUROASPIRE risk categories. Int J Cardiol. 2013;168:910–14.
Turnbull FM, Abraira C, Anderson RJ, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009;52:2288–98.
Kelly TN, Bazzano LA, Fonseca VA, Thethi TK, Reynolds K, He J. Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med. 2009;151:394–403.
Gaede P, Vedel P, Larsen N, Jensen GV, Parving H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348:383-93.
Ho PM, Magid DJ, Shetterly SM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–79.
Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177.
Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15. doi:10.1136/bmj.38875.675486.55.
Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92.
Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev (Online). 2011; (7): CD001800.
Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–72.
Chow CK, Jolly S, Rao-Melacini P, Fox KAA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121:750–8.
Janssen V, De Gucht V, Dusseldorp E, Maes S. Lifestyle modification programmes for patients with coronary heart disease: a systematic review and meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2012;20:620–40.
Bittner V, Bertolet M, Barraza R, et al., and the BARI 2D Study Group. Comprehensive Cardiovascular Risk Factor Control Improves Survival. The BARI 2D Trial. J Am Coll Cardiol. 2015;66:765–73.
Kotseva K, Wood D, De Backer G, De Bacquer D. Use and effects of cardiac rehabilitation in patients with coronary heart disease: results from the EUROASPIRE III survey. Eur J Prev Cardiol. 2012. doi:10.1177/2047487312449591.
Wood DA, Kotseva K, Connolly S, et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008;371:1999–2012.
Giannuzzi P, Temporelli PL, Marchioli R, et al. Global secondary prevention strategies to limit event recurrence after myocardial infarction: results of the GOSPEL study, a multicenter, randomized controlled trial from the Italian Cardiac Rehabilitation Network. Arch Intern Med. 2008;168:2194–204.
De Smedt D, Kotseva K, De Bacquer D, et al. Cost-effectiveness of optimizing prevention in patients with coronary heart disease: the EUROASPIRE III health economics project. Eur Heart J. 2012;33:2865–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kornelia Kotseva reports research grants fromEuropean Society of Cardiology to Imperial College London for coordination of the EUROASPIRE surveys.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Prevention
Rights and permissions
About this article
Cite this article
Kotseva, K. Implementation of Cardiovascular Disease Prevention Guidelines in Clinical Practice—Can We Do Better?. Curr Treat Options Cardio Med 17, 58 (2015). https://doi.org/10.1007/s11936-015-0415-9
Published:
DOI: https://doi.org/10.1007/s11936-015-0415-9