Abstract
Purpose of Review
To describe the complexities of diagnosis and management of neobladder-vaginal fistula (NVF) following orthotopic urinary diversion in women.
Recent Findings
Multiple recent single-institution series confirm the variability of outcomes for NVF repairs and caution regarding comorbid stress urinary incontinence which may necessitate further interventions including conversion to alternate diversions.
Summary
Although both abdominal and transvaginal approaches have been advocated for surgical management of NVF, contemporary series from reconstructive surgeons favor a vaginal approach to decrease overall operative morbidity. Patients should be carefully counseled regarding neobladder and sphincter function following fistula repair along with the risks of secondary urinary diversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
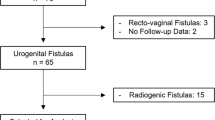
Bladder cancer remains a disease presenting significant morbidity and mortality with approximately 18,810 new cases diagnosed in women in the USA in 2018 including 4720 associated deaths [1]. The overall male/female ratio for bladder cancer is 3:1 with an increased incidence with age. An estimated 25% of newly diagnosed patients will present with muscle-invasive disease with many high-risk patients initially diagnosed with non–muscle-invasive bladder cancer progressing to invasive disease [2••]. For non-metastatic, muscle-invasive bladder cancer, neoadjuvant chemotherapy combined with radical cystectomy (RC) is currently considered standard of treatment. For select patients following RC, creation of an orthotopic neobladder (ONB) presents an excellent option with regard to lower urinary tract reconstruction. Despite generally excellent clinical outcomes for ONB, which aims to preserve normal volitional voiding per the urethra, several well-documented functional and anatomic issues have been described [3]. Severe impairments in quality of life have been demonstrated in women survivors of bladder cancer who suffer diversion-related complications [4]. One of the most devastating complications encountered is neobladder-vaginal fistula (NVF). Herein we aim to describe predisposing risks for NVF and outline surgical methods for both prevention and treatment of this impactful condition.
Pelvic Organ-Preserving Radical Cystectomy
Unsurprisingly, critical to prevention of postoperative issues with ONB is careful preoperative patient selection. Optimizing functional outcomes requires a delicate interplay of both patient-centered, oncologic, functional, and technical factors. Although outside the scope of this manuscript, with regard to NVF prevention, thorough assessment of both relevant history and the urethral and vaginal anatomy is critical. Oncologic concerns predominate the selection process with bladder neck and proximal urethral involvement of malignancy favoring concurrent urethrectomy thus precluding ONB diversion [5]. Additional considerations for adequate renal function and patient compliance with management is mandated evaluation prior to proceeding with ONB [6]. A history of current stress incontinence, prior surgery for stress incontinence, pelvic organ prolapse, or pelvic radiation may preclude appropriateness for ONB construction. Proceeding with ONB in women who have undergone prior mesh mid-urethral sling is strongly discouraged due to the exceptional risks of both stress urinary incontinence (SUI) and the foreign body implant. Pelvic examination should be performed not only to assess for extent of oncologic disease but also to evaluate vaginal epithelial atrophy, pelvic organ prolapse, SUI, and pelvic floor muscle strength to facilitate counseling regarding long-term expectations. Attention should be directed during cystoscopic examinations performed for bladder cancer diagnosis or treatment to assess the trigone, bladder neck, and mucosal lining of the urethra to determine adequacy for ONB diversion. Substantial urethral fibrosis and fixation may be associated with significant SUI issues following ONB.
Traditional radical cystectomy (RC) in women includes anterior exenteration with removal of the bladder, anterior vagina, uterus, salpingo-oophorectomy, distal ureters, and regional lymph nodes [7, 8]. In efforts to improve functional results from ONB reconstruction for women, including recovery in voiding, continence, and sexual function, techniques have been pioneered for pelvic-organ preservation which have not demonstrated compromise to oncologic efficacy [5, 9••, 10]. Surgical techniques for pelvic organ-preserving radical cystectomy (POPRC) have emerged to optimize the aforementioned functional outcomes. In brief, these techniques collectively involve sparing of the entire anterior vaginal wall, preservation of the endopelvic fascia surrounding the urethra, uterus, or cervix, as well as conserving the neurovascular bundles [11, 12, 13••]. Preservation of the vaginal wall, which may enhance functional consequences such as urinary retention or incontinence as well as retain ability for penetrative sexual intercourse, unfortunately places the patient at primary risk for development of NVF. NVF is fortunately uncommon, occurring in multiple series at an incidence of 0–10% of women undergoing ONB diversion [14•, 15]. Timing of fistula occurrence is variable due to several comorbid issues deferring diagnosis, so literature reports range from very early presentation following ONB to many months following initial surgical intervention, with most identified in the 3–5-month range [15, 16].
NVF Prevention Strategies
One of the primary risk factors for development of NVF is direct inadvertent injury to the anterior vaginal wall at the time of RC [11, 17]. Additional risk factors include pelvic radiation impairing vascularity, as well as local tumor recurrence [18]. Technical modifications during RC which may decrease risk of fistula development have emerged over the past several decades. Rigorous closure of the vaginal cuff, vascular flap interpositions such as omentum between the anterior vaginal wall and ONB, limiting blunt dissection in the vicinity of the bladder neck, and avoidance of overlapping suture lines between the urethroileal anastomosis and vaginal reconstruction are solid principles for avoidance of NVF [19]. Intraoperative recognition of anterior vaginal wall injury, even with appropriate closure and interposition grafting, may still culminate with NVB formation [11]. NVF has additionally been reported to occur de novo following injection of urethral bulking agents for treatment of postoperative SUI [16, 20,21,22].
NVF Diagnosis
Although a seemingly overt presentation of continuous drainage of straw-colored vaginal discharge, NVF may frequently be incorrectly diagnosed as SUI due to the high concurrent incidence in this demographic and mimic of increased leak with activity [16]. In this complex diversion population, SUI and NVF indeed often occur simultaneously and vigilance with diagnostics should be appreciated. Most fistulas are characterized by continuous incontinence; however, with the intricacies of ONB, some series report only 58% of patients presenting with this finding [20]. In this long-term series of 12 patients with ONB treated for incontinence, 50% actually presented with a previously undiagnosed NVF. Physical examination for the female ONB patients presenting with incontinence postoperatively is key to directly identify the NVF. For less overt fistula, endoscopic examination will be key for identification. Insuring appropriate ONB function with regard to hypercontinence, nocturnal enuresis, and SUI must also be explored. For less overt cases, proceeding with cystogram or dye test via a neobladder catheter may be a useful adjunct to physical examination to identify the location and number of fistulous tracts. Current modalities of CT cystogram may be preferred for diagnosis of elusive fistula, ideally combined with cystoscopy and vaginoscopy for surgical repair planning. A useful diagnostic algorithm has been proposed for women presenting with incontinence following ONB to guide decision-making and optimize management [20].
Challenges with NVF repair include the attenuated neobladder wall anatomy, vaginal foreshortening following RC, and vaginal epithelial atrophy due to estrogen depletion, in combination with potential functional deficits of the neobladder leading to hypercontinence or concomitant SUI. Surgical approach to repair of NVF recapitulates concepts employed in classic native vesicovaginal fistula surgery, namely circumferential dissection of the fistula tract, closure in multiple water-tight layers, non-overlapping suture lines, and tissue interposition. Additionally, critical in these procedures is sparing of the external rhabdosphincter to avoid de novo development or exacerbation of SUI symptoms.
Minimally Invasive Treatment of Fistula
While traditionally advocated with native vesicovaginal fistula, a trial of catheter drainage will very rarely be effective treatment for NVF [10]. Several reports exist indicating injection of chemical or biological sealant agents such as fibrin facilitate closure of neobladder-cutaneous fistula; however, no literature is available to describe experience with injectable agents for NVF [23, 24]. In general, conservative options in this complex postoperative NVF population will be fraught with poor outcomes and delay in definitive intervention with surgical repair.
Transvaginal Repair
Although treatment strategies must be optimized for the individual patient, for most contemporary NVF, operative repair with a vaginal approach presents the least morbidity with acceptable clinical outcomes. In a relatively large series of 13 patients undergoing transvaginal repair of NVF, 61.5% of patient experienced a successful repair [25]. The remaining seven patients underwent conversion to non-orthotopic diversions either due to ineffective fistula repair [4] or severe urinary incontinence following fistula repair despite further interventions. Carmel et al. reported a series of eight patients who underwent NVF repair from a transvaginal approach without a fistula recurrence during the study follow-up of 33 months [14•]. However, five of these eight patients did require interventions for SUI following fistula reconstruction.
In general, the authors of both of the aforementioned series and multiple additional reports utilize techniques for NVF surgical management which are essentially similar to those employed for repair of classic vesicovaginal fistula to a native bladder [26]. Preoperative treatment of the vaginal epithelium when feasible with topical estrogen cream may promote tissue pliability and ultimately potentiate healing. The patient is traditionally positioned in dorsal lithotomy, although occasionally a prone jack-knife position will optimize presentation of the fistula on the anterior vaginal wall. A weighted vaginal speculum and either labial sutures or a self-retaining retractor is utilized to augment exposure. A catheter is placed per the urethra, and in select instances a catheter can be placed via the fistula tract for mobility to assist with dissection. Likewise, stay sutures surrounding the tract may be helpful for the dissection of the epithelium to maintain appropriate countertraction. The fistula tract is circumferentially marked and sharply circumscribed. Following sharp dissection to create vaginal flaps, the neobladder is optimally reapproximated in two tension-free layers with absorbable suture although the availability of robust tissue may preclude such closure. In these cases, a single layer closure of the attenuated neobladder wall must be utilized. When a second layer is feasible, it should ideally imbricate the first suture line. Integrity of the water-tight closure is interrogated with instillation of methylene blue solution into the neobladder via the urethral catheter. An interposition tissue layer is then added with either Martius labial fat flap, omental flap, gracilis flap, vaginal flap, autologous fascia graft, or peritoneal flap. In extreme cases, biological glue has been utilized to augment the closure. Vaginal epithelium is then closed in a running fashion. Catheter drainage is maintained for 2–3 weeks and a cystogram performed to ensure healing prior to catheter removal. A large bore catheter should be employed to allow irrigation of mucus as catheter plugging and neobladder distention places the delicate reconstruction at significant risk.
Example of transvaginal repair of a large NVF are demonstrated in Figs. 1, 2, 3, 4, 5, and 6. In this patient, optimal exposure was evidenced in the prone jack-knife position instead of lithotomy due to the substantially foreshortened vaginal vault. Additionally, a Martius labial fat graft was employed for interposition tissue.
Abdominal Repair
Some authors advocate for abdominal approaches for particularly large NVF or in the setting of vaginal fibrosis precluding appropriate mobility to allow adequate dissection and placement of robust interposition tissue [26]. Likewise, situations may occur for NVF which mimic those experienced with native vesicovaginal fistula which favor a combined abdominal and vaginal approach to allow wide mobilization of the vaginal wall and bladder as well as complete excision of the fibrotic fistula tract [16]. For abdominal approaches, the patient is generally placed in the low lithotomy position to ensure access to both the urethra, vagina, and abdomen during the procedure. Utilizing the previous cystectomy incision, the abdomen is carefully entered avoiding inadvertent injury to the neobladder, diversion mesentery, or adherent bowel which may be fused to the anterior abdominal wall. Endoscopy during an abdominal approach is exceptionally useful for wire/catheter placement through the fistula tract to aid dissection as well as for direct identification of the neobladder anatomy during distention. The anterior wall is opened to identify the fistulous tract which is circumferentially incised with sharp dissection then utilized to develop the neobladder-vaginal space. Several layers of perpendicular suture lines are placed along with an interposition graft of easily accessible vascular omentum prior to anterior neobladder closure.
For situations where the neobladder is to be abandoned due to refractory fistula, incontinence, or hypercontinence, conversions to either incontinent or catheterizable pouch diversions are feasible [27, 28]. Conversion rates to alternative urinary diversions are approximated to be around 32% and women should be counseled accordingly prior to ONB construction [14•].
Conclusion
NVF represent a distressing complication for women following orthotopic diversion and evaluation may be delayed due to the common comorbidity of SUI. Expedient diagnosis should be endeavored, and transvaginal operative management is the contemporary preferred surgical approach. Use of interposition grafts and meticulous surgical techniques mirroring those used for traditional vesicovaginal fistula repair will manifest optimal results. However, women should be extensively counseled regarding comorbid SUI and risks of conversion to alternative urinary diversion such that patient expectations match eventual outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
•• Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP, et al. Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO Guideline. J Urol. 2017;198(4):552–9 Critical guideline for evaluation and management of muscle-invasive bladder malignancy.
Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH, Holm HV, et al. ICUD–EAU international consultation on bladder cancer 2012: urinary diversion. Eur Urol. 2013;63(1):67–80.
Gakis G, Stenzl A. Considerations for orthotopic diversions in women. Curr Opin Urol. 2015;25(6):550–4.
Gakis G, Jentzmik F, Schrader M, Stenzl A, Sievert KD. Benefits and risks of orthotopic neobladder reconstruction in female patients. Aktuelle Urol. 2011;42(2):109–14.
Smith AB, Crowell K, Woods ME, Wallen EM, Pruthi RS, Nielsen ME, et al. Functional outcomes following radical cystectomy in women with bladder cancer: a systematic review. Eur Urol Focus. 2017;3(1):136–43.
Stenzl A, Nagele U, Kuczyk M, et al. Cystectomy-technical considerations in male and female patients. EAU Updat Ser. 2005;3(3):138–46.
Veskimae E, Neuzillet Y, Rouanne M, MacLennan S, Lam TBL, Yuan Y, et al. Systematic review of the oncological and functional outcomes of pelvic organ-preserving radical cystectomy (RC) compared with standard RC in women who undergo curative surgery and orthotopic neobladder substitution for bladder cancer. BJU Int. 2017;120(1):12–24.
•• Zlatev DV, Skinner EC. Orthotopic urinary diversion for women. Urol Clin North Am. 2018;45(1):49–54 Outstanding synopsis of technical considerations during radical cystectomy which may limit eventual functional and anatomic complications.
Chang SS, Cole E, Cookson MS, Peterson M, Smith JA Jr. Preservation of the anterior vaginal wall during female radical cystectomy with orthotopic urinary diversion: technique and results. J Urol. 2002;168(4 Pt 1):1442–5.
Ali-El-Dein B, Mosbah A, Osman Y, El-Tabey N, Abdel-Latif M, Eraky I, et al. Preservation of the internal genital organs during radical cystectomy in selected women with bladder cancer: a report on 15 cases with long term follow-up. Eur J Surg Oncol. 2013;39(4):358–64.
Skinner EC, Comiter CV. Can we improve the functional outcomes of orthotopic diversion in women? Eur Urol. 2015;68(4):672–3.
•• Carmel ME, Goldman HB, Moore CK, Rackley RR, Vasavada SP. Transvaginal neobladder vaginal fistula repair after radical cystectomy with orthotopic urinary diversion in women. Neurourol Urodyn. 2016;35(1):90–4 Superior synopsis of large series of neobladder-vaginal fistula repairs utilizing a transvaginal approach. Excellent review of both center outcomes and available literature.
• Littlejohn N, Cohn JA, Kowalik CG, Kaufman MR, Dmochowski RR, Reynolds WS. Treatment of pelvic floor disorders following neobladder. Curr Urol Rep. 2017;18(1):5. Excellent review of contemproary literature on functional outcomes from orthotopic diversion.
Gelber K, Bohrer J, Kim CO, Minaglia S. Vaginal repair of neobladder-vaginal fistula: a case report and review of the literature. Int Urogynecol J. 2013;24(1):175–8.
Rapp DE, O'Connor RC, Katz EE, Steinberg GD. Neobladder-vaginal fistula after cystectomy and orthotopic neobladder construction. BJU Int. 2004;94(7):1092–5 discussion 5.
Gschwend JE, May F, Paiss T, Gottfried HW, Hautmann RE. High-dose pelvic irradiation followed by ileal neobladder urinary diversion: complications and long-term results. Br J Urol. 1996;77(5):680–3.
Ali-el-Dein B, Shaaban AA, Abu-Eideh RH, el-Azab M, Ashamallah A, Ghoneim MA. Surgical complications following radical cystectomy and orthotopic neobladders in women. J Urol. 2008;180(1):206–10 discussion 10.
Bailey GC, Blackburne A, Ziegelmann MJ, Lightner DJ. Outcomes of surgical management in patients with stress urinary incontinence and/or neovesicovaginal fistula after orthotopic neobladder diversion. J Urol. 2016;196(5):1478–83.
Pruthi RS, Petrus CD, Bundrick WJ. New onset vesicovaginal fistula after transurethral collagen injection in women who underwent cystectomy and orthotopic neobladder creation: presentation and definitive treatment. J Urol. 2000;164(5):1638–9.
Tunuguntla HS, Manoharan M, Gousse AE. Management of neobladder-vaginal fistula and stress incontinence following radical cystectomy in women: a review. World J Urol. 2005;23(4):231–5.
Selli C, De Maria M, Manica M, Turri FM, Manassero F. Minimally invasive treatment of urinary fistulas using N-butyl-2-cyanoacrylate: a valid first line option. BMC Urol. 2013;13:55.
Morita T, Tachikawa N, Tokue A. Successful closure of neovesicocutaneous fistula with fibrin glue. Urol Int. 1998;61(2):130–1.
Rosenberg S, Miranda G, Ginsberg DA. Neobladder-vaginal fistula: the University of Southern California experience. Neurourol Urodyn. 2018;37(4):1380–5.
Ali-El-Dein B, Ashamallah A. Vaginal repair of pouch-vaginal fistula after orthotopic bladder substitution in women. Urology. 2013;81(1):198–202.
Alcantara-Quispe C, Machado RD, Magnabosco WJ, Santos AC, Faria EF. Neovagina construction and continent cutaneous urinary reservoir using a previous orthotopic ileal neobladder. Int Braz J Urol. 2018;44(5):1036–41.
Hautmann RE, de Petriconi R, Schwarz J, Volkmer B. Single center experience with secondary urinary diversion after initial radical cystectomy and primary urinary diversion. J Urol. 2016;195(2):406–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
M.R.K. is a principal investigator for Cook Myosite, resident course instructor for Boston Scientific, on the data safety monitoring board for Valencia Technologies, and is an assistant editor for the Journal of Urology.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article if part of the Topical Collection on Lower Urinary Tract Symptoms & Voiding Dysfunction
Rights and permissions
About this article
Cite this article
Kaufman, M.R. Neobladder-Vaginal Fistula: Surgical Management Techniques. Curr Urol Rep 20, 67 (2019). https://doi.org/10.1007/s11934-019-0934-0
Published:
DOI: https://doi.org/10.1007/s11934-019-0934-0