Abstract
Purpose of Review
Review current literature for risk factors and strategies to prevent infection in urological prosthetic implants.
Recent Findings
Recent studies on risk factors and special patients are described. Strategies to decrease infection rate, role, and importance of biofilm is also discussed.
Summary
Infection on implanted devices for the treatment of erectile dysfunction and urinary incontinence is the most feared complication. Risk factors, where/when most infections occur, and the role of biofilm are discussed. Infection rates decreased with the advent of infection-resistant coated devices, and subsequently, bacteriological/isolate profiles changed. The bacteriology of implant infection is reviewed. Basic rules of perioperative implant prevention are ensuring no concurrent infections, proper alcohol-based skin preparation (not iodine), appropriate sterile technique, preoperative antimicrobial prophylaxis, reduced operative time, and limiting the implant from touching the skin. Future research is also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prosthetic devices are a well-documented treatment for refractory erectile dysfunction and urinary incontinence. [1,2,3] Device infection is one of the most feared complications following implant procedures. [4••] The traditional infection rates may vary from 2 to 5% during initial implantation up to 7–18% during revision surgery. [5]
Biofilm formation may play an important part in the increased infection rates during revision surgery. [6] The current belief is that bacteria are introduced during surgery, some of them secrete biofilm, and the body develops a capsule of tissue that covers the prosthesis within 3–7 days postoperatively, shielding the bacteria from future antibiotics. [7,8,9,10] In order to address the implant infections, the industry developed antibiotic and hydrophilic coating in an attempt to decrease infection rates. [11•, 1, 2, 4••, 12, 13] However, this advancement has led to a change in bacteriological/isolate profile of both uninfected prosthesis at reoperation and of infected ones. [11•, 4••] Other measures used to decrease implant infections are using rigorous techniques such as alcohol preoperative skin preps, perioperative prophylactic antibiotics, shorter OR time, copious antibiotic irrigation during secondary cases, decrease of device-skin contact, and strict operative sterile techniques. [6] Some complex penile prosthesis recipients may require special measures and care to avoid infection, i.e., complex surgery, substance abuse patient, immunocompromised, uncontrolled diabetic, and spinal cord injury. [14] Therefore, some complex penile prosthesis recipients will be discussed.
The goal of this report was to review the literature for the main risk factors and infection preventive measures during primary inflatable penile prostheses (IPP) and artificial urinary sphincter (AUS) placement and secondary surgeries.
Risk Factors
Special Patients
The risk of infection is individual to each patient, since the state of local host defenses will significantly influence the outcome. [15] Complex surgery, substance abuse, immunocompromised, uncontrolled diabetic, and spinal cord injury patients are all at increased risk for infection, [14] and special considerations are made regarding these cases.
Complex cases carry an increased risk of infection; for example, in patients requiring corporal reconstruction for Peyronie’s disease, fibrosis, or neophallus for transgender patients, the infection rate has been reported at 1.8%, 13.3%, and 21.7%, respectively. [16] The common factor in all these procedures was increased operative time. However, concomitant AUS implantation does not appear to increase risk of infection although this is counterintuitive; thus, most prosthetic urologists rarely do combined implantations. [14, 3] Infection-preventive strategies include minimizing skin contact (no touch technique) and minimizing operative time by making preparations in advance. [17, 14]
Polysubstance abusers have a nine-fold increase in infection risk. [14] Balen et al. in 2016 did a retrospective analysis of health and socioeconomic factors and concluded that active polysubstance abuse concomitant with surgery appears to be a newly identified infection risk factor in IPP placement. [18] In addition, these patients typically require more postoperative pain control.
Up to 50% of patients immunocompromised due to chronic diseases such as leukemia, chronic obstructive pulmonary disease, lupus, and rheumatoid arthritis may develop infection in IPP placement. [19] However, immunosuppression for solid organ transplant did not appear to increase infection risk. That suggests that the poor clinical condition of the chronically ill patient may play a major role in the increased infection rates. [19] There is no increased incidence of infection of an IPP when it is placed in a stable, otherwise healthy, HIV-positive patient. Since IPP surgery is an elective procedure, one could ensure undetectable viral loads and optimal CD4 counts for protection of the surgeon and patient. The ethics of operating on these patients used to be debated at meetings, but now, most prosthetic surgeons believe in implanting HIV patients. [14]
Traditionally, and in opposition to current belief, well-controlled diabetes does not appear to increase infection risk for primary implant procedures. [14, 20] In contrast, a 2018 paper states that increased A1C level above 8.5% had a 80% sensitivity and 65% specificity to predict infection, and it is recommended as a threshold for patient selection. [21] However, a serum glucose level > 200 mg/dl perioperatively had a four-fold increase in infection risk. [18] Good glycemic control before and during the hospital stay may help prevent infection. The jury is still out on infection rates among patients with well-controlled diabetes; to date, there are no good US or European papers showing any increased infection risk in this population.
For patients with spinal cord injury (SCI), the protocol should follow a strict regimen for negative preoperative urine cultures [16], as well as increased vigilance for breaks in skin integrity and optimization of bladder management. [14] Historically, in the setting of SCI, penile implants have been useful in managing both erectile dysfunction as well as urinary incontinence, especially for condom catheter assistance. When choosing a type of implant to place in the SCI patient, it is important to note that the rate of erosion with a malleable device is 18%, as compared with 2.4% for an inflatable model. [22] Malleable implants certainly allow for easier use in this population with limited manual dexterity, although with decreased/absent sensation, constant pressure on the penis inherent with rods may predispose the patient to increased risk of erosion. Inflatable devices should be used for implantation in the SCI population, and if needed, the patient’s partner can be taught how to cycle the device.
Revision Surgery
While primary surgery has a 1–5% risk of infection, traditional revision surgery has a 7–18% risk of infection. [19, 16, 23, 9, 13, 6]. Reasons believed to contribute include decreased host resistance factors, diminished antibiotic penetration due to capsule formation, and decreased wound healing related to scar tissue. It is also believed that biofilm formed after primary surgery may harbor bacteria in a high percentage of patients. [6] Up to 66% of patients had positive swab cultures, and 43% had positive capsule tissue cultures among cases of revision for non-infective reasons. Biofilm is formed after the primary surgery in almost all cases, as determined by scanning laser microscopy at the time of clinically uninfected revisions. [24] Revision washout decreases the uninfected prosthesis capsule tissue culture positivity rate to 25%. While this is still a high percentage of patients, revision washout is an important means to decrease infection risk with IPP replacement surgery. [9]
Other techniques to decrease infection risks on primary implant cases include the use of coated devices and the “no touch” technique. The antibiotic coating InhibiZone consists of a combination of rifampin and minocycline impregnating the outside of the American Medical Systems (AMS) 700 IPPs (Boston Scientific, Minneapolis, MN). It decreases infection rate of primary implantation surgery; yet, it appears to have a lesser effect in revision cases. [9, 13] The biofilm present at the time of revision procedures may contain a bacterial colony count too overwhelming for the antibiotic coating. The amount of antibiotic contained in the InhibiZone of a 700 IPP penile prosthesis is less than a single oral pill, which may not be sufficient to treat the mature biofilm found in secondary cases. The “no touch” technique may reduce infection rate at reoperations and will be discussed below. [17]
Biofilm
With IPP implantation, mechanical failure rates have decreased over time, with advances in design. However, revision/replacement surgery is still performed for reasons including human factors, such as infection and medical problems. [25] The risk of infection remains higher in revision surgery, as compared with the primary procedure, despite many technical advances. [19, 16, 23, 8] Biofilm plays a huge part in the increased infection risk, due to its unique characteristics.
Biofilms develop when bacteria firmly attach to a surface and start to reproduce, therefore excreting extracellular polymers that support matrix formation and fixation. These microorganisms are first introduced during the initial procedure. Once in the host environment, they multiply and secrete a mucinous biofilm, composed of various protein forms, [26] and may develop a symbiotic relationship with the host, without causing clinical levels of infection [9]. As the organisms multiply within the biofilm, they create channels for water and nutrition. This results in a phenotypic alteration of the organisms in regard to gene transcription and growth rate. [27, 28]
Micro-organisms within the biofilm have a decreased antibiotic susceptibility, therefore, can possibly be causing the increase in revision/replacement infection risk. The bacteria that reside in the deep biofilm layers are not metabolically active and are resistant to antibacterial drugs and culture media. They may cause an immune response, which may be recognized as device infection. [17] In addition, the separation of planktonic bacteria from the established biofilm may cause a systemic infection. But this is dependent on many variants, including the immune system responses of the host. [27] The disturbance of biofilm during revision surgery may also release free bacteria and thus be responsible for the increased rates of infection compared with primary implants. [9]
Biofilm-forming pathogens include S epidermidis, Staphylococcus aureus, Klebsiella pneumonia, Escherichia coli, Pseudomonas aeruginosa, and Candida albicans. [29] Experimental evidence has shown that staphylococcal species adhere to foreign surfaces with much greater affinity than other bacteria. [19, 16, 25, 30] The surface characteristics may have an effect on the speed of micro-organism attachment. Generally, the rougher and more hydrophobic the materials, the faster they will develop biofilms. [2, 10, 28••]
Bacteriology of Infection
In 1995, Licht et al. [31] reported high culture positivity in devices during revisions of prosthesis for other reasons than infection. They observed 43% of IPPs and 36% of AUS’s cultured organisms, with S epidermidis being the most common organism found in infected prostheses. However, they hypothesized that the identified bacteria were at such a low colony count that they did not have a role in clinical infection. In 2004, Henry et al. [8] took aerobic and anaerobic culture swabs from the pump, capsule, liquid surrounding the pump, and from any suspicious biofilm area in the area of the components. They observed that patients with clinically uninfected penile prostheses were found to have positive cultures 70% of the time, and 90% of the positive cases had positive culture for Staphylococcus genus with ten different species. In 2002, InhibiZone, a combination of rifampin and minocycline coated on the outside of 700 series IPPs, became widely utilized, and the literature shows that it decreases primary infection rates by about half. [11•]
In 2008, Henry et al. [6] took swab cultures from revision surgeries of clinically uninfected penile implants; they observed that 66% of patients had positive cultures. In addition, implant capsule tissue cultures were positive in 43% of cases. After performing a revision washout procedure, the tissue culture positivity decreased to 25%. This study reported that surgical antiseptic lavage decreased bacterial culture positivity in penile implants at revision surgery and reduced incidence of ensuing device infection. The findings from this study also showed higher revision-free implant survival rates among patients with negative bacterial swab cultures than in those with positive cultures, for up to 1.6 years longer in patients with negative cultures; however, there is still no easy explanation for that. Dr. Cully Carson first postulated that increased bacterial presence/bioflim causes stiffness of the implant tubing, leading to earlier breakage of the tubing and subsequent loss of fluid.
Kava et al. also suggested that S epidermidis cultured at revision surgery might be a contaminant, rather than actually present in the implant tissue space. [32] They observed that less than 10% of revision implants had positive cultures for asymptomatic bacteria, and S epidermidis was present in only 5% of implants. Differently from other surgical series, Kava et al. did not observe a correlation between positive cultures at revision surgery and increased risk of clinical infection. Kava findings are in opposition to actual scanning electron microscopy that has confirmed bacterial biofilm formation on nine out of ten (90%) of IPPs at time of replacement surgery. [24] Moreover, most series reported S epidermidis as the most common organism responsible for infections in penile prostheses; some of these studies attribute these bacteria in to up to 50% of infections. [33]
The development of antibacterial IPP coating is changing the bacteriological profile of asymptomatic biofilm and infection. In 2006, Abouassaly et al. [34] observed that positive cultures were found in 35% of clinically uninfected penile implants coated with InhibiZone. In a multicenter study, Jani [11•] showed that IPP coating with InhibiZone decreased the culture positivity of uninfected IPPs from 63.9% with noncoated IPPs to 42.7% with coated IPPs. The coating also reduced the culture positivity for Staphylococcus genus from 88 to 62.5%. In infected IPPs, the InhibiZone coating showed a tendency to decrease culture positivity to Staphylococcus genus.
The change in bacteriological profile is observed as an increase in culture positivity for Gram-negative bacteria and yeast. In a recent multicenter study, with culture from IPP infections, almost 70% were caused by Gram-positive organisms. [4••] However, a total of 39% of infections encompassed Gram-negative organisms, the most common being Escherichia coli. Furthermore, Candida species were identified in 11.1% of the positive cultures, and anaerobic bacterial infections occurred in 10.5% of positive cultures. The orthopedic literature has more data on anaerobic infections. It has been reported that 3% to 6% of prosthetic joint infections are related to anaerobes, although anaerobic bacteria are challenging to culture and diagnose. [35] In the recent study by Gross et al., roughly one third of infected penile implants exhibited negative cultures and 25% of positive cultures were multi-organism infections. [4••]
Prevention
Antibiotic-Coated and Hydrophilic Coated IPPs
In order to decrease the adherence of staphylococcal species to the prostheses, the industry developed not only antibiotic-coated penile prostheses, but also components coated with a hydrophilic coating that create a lubricious surface, when wet. [28••] The antibiotic coating InhibiZone of the AMS 700 penile prosthesis (Boston Scientific, Minneapolis, MN) consists of a combination of rifampin and minocycline, whereas the Coloplast Titan penile prosthesis (Coloplast, Minneapolis, MN) has a hydrophilic coating of the outside of the IPPs. These measures have been shown to reduce infection rates for primary implantation surgeries by roughly 50%. [11•, 13]
In a preclinical study, Chanyi [36] observed that immersion of IPP tubing with InhibiZone in antibiotic solution may further prevent bacterial growth of less commonly experienced causes of infection. The InhibiZone tubing was effective against the Gram-positive S. aureus and S. epidermidis, although it did not inhibit growth of Gram-negative E. coli and P. mirabilis in culture medium. The inhibition zone was increased when tubing was immersed in ampicillin or ciprofloxacin for 2 min. Further study is required to determine if immersion of InhibiZone devices in antibiotic solution may decrease infection rate caused by Gram-negative bacteria. The hydrophilic coating on the outside of the Titan IPP “soaks up” whatever liquid/antimicrobial it is submerged in.
Revision Washout
Multiple studies have shown an increased infection risk when revision operations are done on urological prostheses. [34, 37, 30] The increased infection rate has been hypothesized to result from decreased antibiotic penetration due to the capsule surrounding the components, decreased host resistance factors, and the decreased wound healing related to scar formation. It appears that the majority of clinically uninfected penile prostheses have organisms growing in the implant space at reoperation. [8] Revision surgery may stir inactive bacteria, causing a higher revision infection rate compared with primary implantation, as discussed previously. There is evidence to suggest that removing all the components of the prosthesis and washing out the implant space with an irrigation protocol and complete replacement of the original prosthesis with an infection retardant-coated IPP appears to decrease the infection rate of revision surgery performed on clinically uninfected penile prostheses. [6] However, without the revision washout, the replacement with an antibiotic coated prosthesis alone did not decrease revision infection rates. [9]
Revision washout appears to decrease the amount of bacteria present on the capsule surface for implantation of the new IPP. Henry et al. evaluated 148 patients with swab cultures of the fluid around the pump or biofilm. Before washout, 66% (97 patients) had positive bacterial cultures. Of the 65 implant capsule tissue cultures obtained before washout, 43% (28 patients) were positive for bacteria, while 25% (16 patients) obtained after revision washout cultured positive. [6] The authors concluded that revision washout appears to decrease the bacterial load on implant capsule tissue at revision surgery of previously non-infected IPPs. Of special note, despite being standard rule of surgery to irrigate infected wounds, at the time of the publication, there was no other paper in PubMed that compared tissue cultures before and after any type of surgical washout in any field of surgery.
The washout solution described in the Mulcahy salvage procedure [30] used several steps, including solutions with high concentrations of povidone-iodine (PVI) and peroxide. It is the authors’ current routine to use a large amount of a single saline-based solution, since peroxide and high concentrations of PVI may cause tissue damage. [38] There is evidence to suggest that even subclinical concentrations of H2O2 (0.03–0.06%) may promote inflammation and impair tissue healing [39], and its routine use in salvage or review washout should be reconsidered/eliminated. [38] High concentrations of PVI may also cause tissue damage [38]; however, there is some evidence to suggest that lower concentrations of PVI (0.35–3.5%) may be beneficial, without impairing tissue healing if left in contact for more 3 min [38].
Alcohol-Based Skin Preparation
Since the pathogens found on the patient’s skin appear to be the major source of surgical site infection, an optimal preoperative skin preparation may decrease device infection. A prospective, multicenter, randomized clinical trial compared chlorhexidine–alcohol and PVI for surgical site antisepsis. Patients who had their skin prepped with chlorhexidine–alcohol had less surgical site infections than those prepped with PVI (9.5% vs. 16.1%; P = 0.004). [40] In the systematic review and meta-analysis conducted by Lee and colleagues, [41] chlorhexidine-based agents were found to decrease the risk of surgical site infections considerably, with an adjusted risk ratio of 0.64, and to decrease positivity of skin culture results (adjusted risk ratio, 0.44) when compared to iodine antisepsis. [41, 42]
In 2011, Kava et al. [32] reported a similar result in IPP placement. A total of 117 primary and 72 revision penile implant procedures were analyzed. The first 106 patients had in infection rate of 7.5%. In the last 83 patients, an adjuvant alcohol-based skin prep applied lowered the risk of infection to 1.2% (1 out of 83 patients vs. 8 of the first 106). [28]
Perioperative Prophylactic Antibiotics
The new guidelines for antibiotic selection from the American Urological Association (AUA) and European Association of Urology (EAU) have broadened perioperative prophylaxis to encompass the bacteria expected to cause infection. [43, 44] In a recent study, Gross et al. [4••] observed and compared the results of retrospective analysis of culture results and profile of antibiotic resistance with the AUA and EAU guidelines. The AUA suggests an aminoglycoside (or aztreonam in patients with renal compromise) in combination with a first- or second-generation cephalosporin or vancomycin. The combination of an aminoglycoside (or aztreonam) and vancomycin showed the highest efficacy, killing 86% of the bacteria cultured in their series. Nonetheless, this combination had weak anaerobic coverage (25%) and did not have fungal coverage. The EAU recommends a second- or third-generation cephalosporin or a penicillin agent with anti-penicillinase. Ampicillin-sulbactam was the most efficient single anti-penicillinase agent in the EAU guidelines and eliminated 72% of the cultured microbes in their series. Anaerobic coverage was 100%, but the Gram-positive and Gram-negative coverage decreased to 72% and 73%, respectively. Also, it did not cover Candida species and was not used by their surgeons. [4••] These findings of increased fungal infections have led the authors and several other prosthetic urologists to add, though not covered by the guidelines, an antifungal agent such as fluconazole pre-operatively.
Prevention of Hematoma Formation
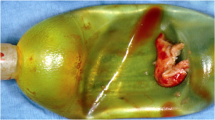
Techniques to reduce hematoma formation will also decrease nutrient sources available to microorganisms. [45, 46] Large hematomas can cause dark “currant jelly” appearing drainage, which can act like a Petri dish for bacteria to grow in. In the past, some prominent prosthetic surgeons advocated for immediate surgical evacuation of large scrotal hematomas to try to avoid high infection rates. The vast majority of high-volume surgeons would agree avoidance of scrotal hematomas is a good idea to prevent infections.
Suction Drain
There is controversy on whether or not to place a drain. In order to avoid postoperative hematoma, Sadeghi-Nejad and colleagues conducted a multi-institutional study on the efficacy of closed-suction drainage of the scrotum in three-piece IPP surgery. They studied 425 patients and observed a 3.3% infection rate and 0.7% hematoma rate during an 18-month follow-up period. The authors concluded that short-term, closed-suction drainage decreased the rate of hematoma formation following penile implant without increasing the risk of infection [46].
In spite of the data presented in that paper, there is still a concern that a drain placed near an implant might increase rates of infection and some may prefer alternative methods of hematoma prevention rather than a closed-suction drain. Since the source of scrotal hematoma may be corporal bleeding, another approach consists of closing the corporotomy with a running water-tight suture after cylinder placement. Arguments against this method include longer operative times to perform the suturing and suturing risks of inadvertent cylinder puncture. Another technique is to place a hemostatic agent along the corporal incision to aid in decrease of post-surgical scrotal hematoma. Alternatively, a newer method to prevent hematomas may be advanced dressings such as a “mummy wrap” procedure.
Wilson et al. initially sought to identify methods to decrease scrotal hematoma formation following penile prosthesis surgery. Men were separated into three groups, pressure dressing alone, pressure dressing with drain, and pressure dressing with drain as well as implant inflation. Decreased rate of hematoma was only seen with the combination of all three methods [47].
Further evaluating the potential increase of infection caused by drains, Wallen et al. recently analyzed drain tubing cultures in over 100 IPP procedures. Both distal and proximal (1 cm below skin level) tubing segments were sent for standard culture after 48–72-h placement time following surgery. All distal drain tips were negative for growth and only 1 proximal section had growth. No cases were noted to be infected on follow-up. As a side note, hematoma formation was not seen in any patient at the time of drain removal [48].
Mummy Wrap
Since the insurance reimbursement rules are changing, there is a tendency to do most cases as truly outpatient (same-day) surgeries. The use of a drain or complicated “spider web” tape dressing pushes the physician to use an overnight stay in the hospital. The Henry Mummy Wrap™ uses a non-sticky dressing, e.g., a Kerlix™ (Covidien, Dublin Ireland) 4-in. dressing roll. Starting at the top of the penis, the dressing is wrapped loosely, gradually wrapping around the shaft. After the shaft of the penis has been encircled, the dressing is wound around the base of the entire genitalia—lifting the testicles, the pump, and the scrotum, superiorly, in a “broccoli stalk” shaping maneuver. [45]
The dressing is then additionally wrapped a few times compressing the already present bandage. The key element is getting the dressing beneath both testicles (the “broccoli stalk”), with the pump positioned in the desired long-term location. Obese patients or those with a small, tight scrotum may need numerous circumferential wraps around the base of the whole genitalia to guarantee that the testicles and pump are pushed forward into the “cast.” The soft cast that develops at the end of this wrap procedure resembles an orthopedic ankle cast. After the dressing is placed, a soft cloth surgical tape, such as Medipore™ (3M, St. Paul, MN), is applied around the soft cast, with minimal tape adhering to the patient’s skin. The Foley catheter is left inside until the dressing is removed, with the tubing taped to the patient’s abdominal wall to alleviate tension on the Foley catheter, as patients may have difficulty voiding with the dressing in position. Without expansion of the scrotum, there should be minimal to no hematoma while the dressing is in place. One should always leave the glans exposed and avoid aggressive compressive dressing circumferentially.
Minimization of Device Skin Contact (“No Touch”)
The “no touch” technique [49] consists of decreasing skin contact with the prosthetic material. By changing gloves and surgical tools after opening the skin, subcutaneous tissue, and dartos to the level of Buck’s fascia, and usage of a special drape to completely isolate the surgical field from the skin, Eid and Wilson in 2012 showed a decrease in infection rate from 2% with the standard technique and coated devices to only 0.46% with the no touch technique. There was no difference in the AMS and Coloplast infection rates and no difference between virgin and revision operation infection rates. [17]
In a recent study by Weinberg et al., 200 men were operated with a modified “no touch technique” and “mummy wrap” dressing. Using a subcoronal incision and complete penile degloving to place the IPP, the researchers observed that three men developed infections (1.5%). It is important to observe that 74% of patients had diabetes, 24% had Peyronie’s plaque plication, and 22% had Peyronie’s relaxing incisions to correct penile curvature. [50]
Strict Operative Sterile Technique
Even with sterile procedures, every surgical incision is potentially contaminated with bacteria. Commonly, these are bacteria from the patient’s own endogenous flora; yet, a strict sterile operative technique should be maintained. [15] Notwithstanding the importance of hand scrubbing, and appropriate use of sterile gloves and gowns, other perioperative measures include hair removal, perioperative warming, and optimization of the operating room environment. The lowest risk of surgical site infection (SSI) has always been associated with not removing hair. If hair needs to be removed because of interference with the procedure, then it should be done immediately before the surgery. While clipping has been shown to be better than shaving for cardiac bypass grafting [51], it can be difficult and abrasive to clip the scrotum. However, Grober et al. [52] showed “that preoperative hair removal on the scrotal skin using a razor results in less skin trauma and improved overall shave quality with no apparent increased risk of SSIs”. [52] Perioperative hypothermia, however, is associated with a significant increase in surgical site infection risk. [42]
The use of double gloves may offer additional benefit. In a recent study, Makama et al. [53] encouraged the use of double gloves. After analyzing total of 1536 gloves, a perforation rate of 15.2% was observed in single gloves and 14.4% in double gloves. However, the number of through and through puncture from outer to the inner gloves was only 1.17%. Thus, the double glove technique offered a protection for 98.83% of cases of outer glove perforation.
Future Research, Ideas, Advancements
Planktonic bacteria are different from bacteria in a biofilm. Biofilm bacteria can alter their local environment, distinguishing themselves even further from planktonic cells. Bacteria in a biofilm can sustain slow growth rates and remain inactive for long periods. Since conventional laboratory bacterial cultures were developed to identify planktonic bacteria, they are often unable to identify bacteria present in a biofilm, thus increasing the likelihood of failure when culturing biofilm for an implanted device. [6]
Taking into account these difficulties, there is an increase in the use of clinical molecular microbiological methods to investigate the microbiota of chronic infections. Molecular testing is more sensitive than culturing, which results in markedly different results being reported to clinicians. When comparing molecular and culture testing, the culture-free 16S ribosomal DNA sequencing and its relative abundance score can help clinicians decide the best course of treatment by displaying the bacteria more common in a sample and therefore more likely to be responsible for the infection.
The slow growth speeds of the biofilm offer protection against immune defenses and many antimicrobial agents, such as antibiotics and biocides. The bacteria deep into the biofilm can withstand antibiotic concentrations 1000 to 1500 times higher than the concentrations that kill same species freely floating (planktonic) bacteria. [54] Thus, biofilms are particularly hard to prevent and even harder to destroy once they are formed, increasing the risk of persistent/chronic infection. [55, 56] Molecular testing delivers fast results even in the setting of a negative culture and will detect dormant bacteria. Additionally, biofilm pathogens are evaluated against 34 unique antimicrobial agents, more than a standard culture’s susceptibility testing. Clinical molecular microbiological methods are now considered the gold standard in other medical specialties such as wound care. DNA sequencing data have not been published in a peer-reviewed paper in prosthetic urology yet.
Other ideas for future research in decreasing implant infections should include different types of surface/shielding of the surface of the implant—for example, a surface that does not allow attachment of the bacteria on a scanning microscopy level. It has been reported that the European Union is soon to require a large clinical study of InhibiZone in order to keep using it after 2020, and this may be not feasible to the company. Therefore, expanded research of IPP surface design may be imminent.
While discussed and presented at several meetings including those of the Sexual Medicine Society of North America (SMSNA) and the AUA, the authors were discouraged to write up “observation of local clinical penile prostheses infections instead of immediate salvage rescue/removal” in cases of draining clear fluid from the postoperative incision in patients with no systemic symptoms. [57, 58] The point of when to observe the patient versus surgical readmission of a patient for implant removal versus salvage rescue remains indeterminate and controversial. The authors believe it is time to move forward with defining these issues with research. In addition, despite it being mandatory to irrigate infected wounds, there is only one paper found in PubMed that compared tissue cultures before and after any type of surgical washout in any field of surgery and there should be more.
Conclusions
Care must be taken with special patients and complicated implant procedures. Good glycemic control before and immediately after surgery, ensuring proper alcohol-based skin preparation (not PVI), preoperative antibiotics, reduced operative time, proper surgical technique, use of coated IPPs, and limiting the implant from touching the skin are probably the best ways to reduce the infection rate. Appropriate antimicrobial prophylaxis should be used based on the current guidelines and local hospital’s resistance profile. Revision washout appears to significantly reduce infection rates in clinically uninfected revision and is considered more and more to be the standard of care. Precaution to avoid hematoma formation must also be taken with use of closed suction drain and/or mummy wrap.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Le B, Burnett AL. Evolution of penile prosthetic devices. Korean J Urol. 2015;56(3):179–86. https://doi.org/10.4111/kju.2015.56.3.179.
Chung E. Penile prosthesis implant: scientific advances and technological innovations over the last four decades. Transl Androl Urol. 2017;6(1):37–45. https://doi.org/10.21037/tau.2016.12.06.
Boysen WR, Cohen AJ, Kuchta K, Park S, Milose J. Combined placement of artificial urinary sphincter and inflatable penile prosthesis does not increase risk of perioperative complications or impact long-term device survival. Urology. 2019;124:264–70. https://doi.org/10.1016/j.urology.2018.10.033.
•• Gross MS, Phillips EA, Carrasquillo RJ, Thornton A, Greenfield JM, Levine LA, et al. Multicenter Investigation of the Micro-Organisms Involved in Penile Prosthesis Infection: An Analysis of the Efficacy of the AUA and EAU Guidelines for Penile Prosthesis Prophylaxis. J Sex Med. 2017;14(3):455–63. https://doi.org/10.1016/j.jsxm.2017.01.007. Analyses culture results and antibiotic resistance of a large number of infected IPPs from 25 centers and compares with current AUA and EAU guidelines for antibiotic prophylaxis. It found a high incidence of anaerobic, Candida, and methicillin-resistant S aureus infections. Micro-organisms identified in this study were not covered by the AUA and EAU antibiotic guidelines in at least 14% to 38% of cases.
Mellon MJ, Broghammer JR, Henry GD. The Mulcahy salvage: past and present innovations. J Sex Med. 2015;12(Suppl 7):432–6. https://doi.org/10.1111/jsm.12986.
Henry GD, Carson CC, Wilson SK, Wiygul J, Tornehl C, Cleves MA, et al. Revision washout decreases implant capsule tissue culture positivity: a multicenter study. J Urol. 2008;179(1):186–90; discussion 90. https://doi.org/10.1016/j.juro.2007.08.168.
Nehra A, Carson CC 3rd, Chapin AK, Ginkel AM. Long-term infection outcomes of 3-piece antibiotic impregnated penile prostheses used in replacement implant surgery. J Urol. 2012;188(3):899–903. https://doi.org/10.1016/j.juro.2012.04.116.
Henry GD, Wilson SK, Delk JR 2nd, Carson CC, Silverstein A, Cleves MA, et al. Penile prosthesis cultures during revision surgery: a multicenter study. J Urol. 2004;172(1):153–6. https://doi.org/10.1097/01.ju.0000132141.48587.f1.
Henry GD, Wilson SK, Delk JR 2nd, Carson CC, Wiygul J, Tornehl C, et al. Revision washout decreases penile prosthesis infection in revision surgery: a multicenter study. J Urol. 2005;173(1):89–92. https://doi.org/10.1097/01.ju.0000146717.62215.6f.
Serefoglu EC, Mandava SH, Gokce A, Chouhan JD, Wilson SK, Hellstrom WJ. Long-term revision rate due to infection in hydrophilic-coated inflatable penile prostheses: 11-year follow-up. J Sex Med. 2012;9(8):2182–6. https://doi.org/10.1111/j.1743-6109.2012.02830.x.
• Jani K, Smith C, Delk JR 2nd, Carson CC, Donatucci CF, Cleves MA, et al. Infection Retardant Coatings Impact on Bacterial Presence in Penile Prosthesis Surgery: A Multicenter Study. Urology. 2018;119:104–8. https://doi.org/10.1016/j.urology.2018.05.028. Studied the effect of infection retardant coating on culture positive isolates found in uninfected and infected IPPs. It shows a change in bacteriological profile with IRC, fewer cultured isolates of Staphylococcus genus.
Pastuszak AW, Lentz AC, Farooq A, Jones L, Bella AJ. Technological improvements in three-piece inflatable penile prosthesis design over the past 40 years. J Sex Med. 2015;12(Suppl 7):415–21. https://doi.org/10.1111/jsm.13004.
Carson CC. Efficacy of antibiotic impregnation of inflatable penile prostheses in decreasing infection in original implants. J Urol. 2004;171(4):1611–4. https://doi.org/10.1097/01.ju.0000118245.66976.e1.
Carrasquillo RJ, Munarriz RM, Gross MS. Infection prevention considerations for complex penile prosthesis recipients. Curr Urol Rep. 2019;20(3):12. https://doi.org/10.1007/s11934-019-0875-7.
Tacconelli E, Muller NF, Lemmen S, Mutters NT, Hagel S, Meyer E. Infection risk in sterile operative procedures. Dtsch Arztebl Int. 2016;113(16):271–8. https://doi.org/10.3238/arztebl.2016.0271.
Jarow JP. Risk factors for penile prosthetic infection. J Urol. 1996;156(2 Pt 1):402–4.
Eid JF, Wilson SK, Cleves M, Salem EA. Coated implants and "no touch" surgical technique decreases risk of infection in inflatable penile prosthesis implantation to 0.46%. Urology. 2012;79(6):1310–5. https://doi.org/10.1016/j.urology.2011.11.076.
Balen A, Gross MS, Phillips EA, Henry GD, Munarriz R. Active polysubstance abuse concurrent with surgery as a possible newly identified infection risk factor in inflatable penile prosthesis placement based on a retrospective analysis of health and socioeconomic factors. J Sex Med. 2016;13(4):697–701. https://doi.org/10.1016/j.jsxm.2016.01.010.
Wilson SK, Delk JR 2nd. Inflatable penile implant infection: predisposing factors and treatment suggestions. J Urol. 1995;153(3 Pt 1):659–61.
Minervini A, Ralph DJ, Pryor JP. Outcome of penile prosthesis implantation for treating erectile dysfunction: experience with 504 procedures. BJU Int. 2006;97(1):129–33. https://doi.org/10.1111/j.1464-410X.2005.05907.x.
Habous M, Tal R, Tealab A, Soliman T, Nassar M, Mekawi Z, et al. Defining a glycated haemoglobin (HbA1c) level that predicts increased risk of penile implant infection. BJU Int. 2018;121(2):293–300. https://doi.org/10.1111/bju.14076.
Zermann D-H, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: long-term Followup. J Urol. 2006;175(3):1041–4. https://doi.org/10.1016/s0022-5347(05)00344-7.
Lotan Y, Roehrborn CG, McConnell JD, Hendin BN. Factors influencing the outcomes of penile prosthesis surgery at a teaching institution. Urology. 2003;62(5):918–21. https://doi.org/10.1016/s0090-4295(03)00665-4.
Silverstein AD, Henry GD, Evans B, Pasmore M, Simmons CJ, Donatucci CF. Biofilm formation on clinically noninfected penile prostheses. J Urol. 2006;176(3):1008–11. https://doi.org/10.1016/j.juro.2006.04.034.
Carson CC. Diagnosis, treatment and prevention of penile prosthesis infection. Int J Impot Res. 2003;15(S5):S139–S46. https://doi.org/10.1038/sj.ijir.3901091.
Ingraham FD, Alexander E Jr, Matson DD. Synthetic plastic materials in surgery. N Engl J Med. 1947;236(10):362; passim. https://doi.org/10.1056/NEJM194703062361004.
Donlan RM. Biofilm formation: a clinically relevant microbiological process. Clin Infect Dis. 2001;33(8):1387–92. https://doi.org/10.1086/322972.
•• Dawn LE, Henry GD, Tan GK, Wilson SK. Biofilm and Infectious Agents Present at the Time of Penile Prosthesis Revision Surgery: Times Are a Changing. Sex Med Rev. 2017;5(2):236–43. https://doi.org/10.1016/j.sxmr.2017.01.002. Discusses the role of biofilm in clinical infections and current changes in the bacteriology of infections. The abundance of staphylococcal species-particularly coagulase-negative organisms-in positive cultures has decreased in infected implants, and clinically uninfected implants also have shown a decrease in the proportion of staphylococcal species. Conversely, other isolates such as fungi, Escherichia coli, and Enterococcus species have increased in clinically uninfected and infected implants, and there has been an overall increase in unique isolates that form the biofilm.
Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15(2):167–93. https://doi.org/10.1128/cmr.15.2.167-193.2002.
Brant MD, Ludlow JK, Mulcahy JJ. The prosthesis salvage operation: immediate replacement of the infected penile prosthesis. J Urol. 1996;155(1):155–7.
Licht MR, Montague DK, Angermeier KW, Lakin MM. Cultures from genitourinary prostheses at reoperation: questioning the role of Staphylococcus epidermidis in Periprosthetic infection. J Urol. 1995;154(2):387–90. https://doi.org/10.1016/s0022-5347(01)67058-7.
Kava BR, Kanagarajah P, Ayyathurai R. Contemporary revision penile prosthesis surgery is not associated with a high risk of implant colonization or infection: a single-surgeon series. J Sex Med. 2011;8(5):1540–6. https://doi.org/10.1111/j.1743-6109.2011.02222.x.
Wilson SK, Costerton JW. Biofilm and penile prosthesis infections in the era of coated implants: a review. J Sex Med. 2012;9(1):44–53. https://doi.org/10.1111/j.1743-6109.2011.02428.x.
Abouassaly R, Angermeier KW, Montague DK. Risk of infection with an antibiotic coated penile prosthesis at device replacement for mechanical failure. J Urol. 2006;176(6 Pt 1):2471–3. https://doi.org/10.1016/j.juro.2006.08.010.
Shah NB, Tande AJ, Patel R, Berbari EF. Anaerobic prosthetic joint infection. Anaerobe. 2015;36:1–8. https://doi.org/10.1016/j.anaerobe.2015.08.003.
Chanyi RM, Alzubaidi R, Leung EJY, Wilcox HB, Brock GB, Burton JP. Inflatable penile prostheses implantation: does antibiotic exposure matter? Sex Med. 2018;6(3):248–54. https://doi.org/10.1016/j.esxm.2018.05.004.
Wolter CE, Hellstrom WJG. The hydrophilic-coated inflatable penile prosthesis: 1-year experience. J Sex Med. 2004;1(2):221–4. https://doi.org/10.1111/j.1743-6109.2004.04032.x.
Pan S, Rodriguez D, Thirumavalavan N, Gross MS, Eid JF, Mulcahy J, et al. The use of antiseptic solutions in the prevention and Management of Penile Prosthesis Infections: areview of the cytotoxic and microbiological effects of common irrigation solutions. J Sex Med. 2019;16(6):781–90. https://doi.org/10.1016/j.jsxm.2019.03.271.
Wilgus TA, Bergdall VK, Dipietro LA, Oberyszyn TM. Hydrogen peroxide disrupts scarless fetal wound repair. Wound Repair Regen. 2005;13(5):513–9. https://doi.org/10.1111/j.1067-1927.2005.00072.x.
Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26. https://doi.org/10.1056/NEJMoa0810988.
Lee I, Agarwal RK, Lee BY, Fishman NO, Umscheid CA. Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol. 2010;31(12):1219–29. https://doi.org/10.1086/657134.
Young PY, Khadaroo RG. Surgical site infections. Surg Clin North Am. 2014;94(6):1245–64. https://doi.org/10.1016/j.suc.2014.08.008.
Wolf JS Jr, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179(4):1379–90. https://doi.org/10.1016/j.juro.2008.01.068.
G.Bonkat, R.Pickard, R.Bartoletti, F.Bruyère, S.E.Geerlings, F.Wagenlehner et al. EAU guidelines on urological infections. 2017.
Henry GD. Surgical techniques: the Henry mummy wrap™ and the Henry finger sweep™ surgical techniques. J Sex Med. 2009;6(3):619–22. https://doi.org/10.1111/j.1743-6109.2008.01200.x.
Sadeghi-Nejad H, Ilbeigi P, Wilson SK, Delk JR, Siegel A, Seftel AD, et al. Multi-institutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005;17(6):535–8. https://doi.org/10.1038/sj.ijir.3901354.
Wilson SC, Cleves M, Mulcahy JJ. Scrotal Hematoma formation following penile prosthesis implantation: To drain or not to drain. J Urol. 1996;155:634A.
Wallen J, Beilan J, Emtage J, Bickell M, Martinez D, Carrion R, et al. 062 “Just the Tip” Closed Suction Drain Cultures after Implantation of Penile Prosthesis. J Sex Med. 2016;13(5):S30. https://doi.org/10.1016/j.jsxm.2016.02.065.
Eid JF. No-touch technique. J Sex Med. 2011;8(1):5–8. https://doi.org/10.1111/j.1743-6109.2010.02137.x.
Weinberg AC, Pagano MJ, Deibert CM, Valenzuela RJ. Sub-coronal inflatable penile prosthesis placement with modified no-touch technique: astep-by-step approach with outcomes. J Sex Med. 2016;13(2):270–6. https://doi.org/10.1016/j.jsxm.2015.12.016.
Graf K, Sohr D, Haverich A, Kuhn C, Gastmeier P, Chaberny IF. Decrease of deep sternal surgical site infection rates after cardiac surgery by a comprehensive infection control program. Interact Cardiovasc Thorac Surg. 2009;9(2):282–6. https://doi.org/10.1510/icvts.2009.205286.
Grober ED, Domes T, Fanipour M, Copp JE. Preoperative hair removal on the male genitalia: clippers vs. razors. J Sex Med. 2013;10(2):589–94. https://doi.org/10.1111/j.1743-6109.2012.02904.x.
Makama JG, Okeme IM, Makama EJ, Ameh EA. Glove perforation rate in surgery: arandomized, controlled study to evaluate the efficacy of double gloving. Surg Infect. 2016;17(4):436–42. https://doi.org/10.1089/sur.2015.165.
Nickel JC, Olson M, McLean RJ, Grant SK, Costerton JW. An ecological study of infected urinary stone genesis in an animal model. Br J Urol. 1987;59(1):21–30.
Stewart PS, William CJ. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358(9276):135–8. https://doi.org/10.1016/s0140-6736(01)05321-1.
Lewis K. Riddle of biofilm resistance. Antimicrob Agents Chemother. 2001;45(4):999–1007. https://doi.org/10.1128/AAC.45.4.999-1007.2001.
Henry G, Price G, Pryor M, Greenfield J, Jones L, Perito P, et al. Observation of local clinical penile prostheses infections instead of immediate salvage rescue/removal: ten center study with surprising results. Abstract #92. Proceedings of the 20(th) Annual Fall Scientific Meeting of the Sexual Medicine Society of North America, Miami Beach, USA, November 20–23, 2014. J Sex Med. 2015;12(Suppl 2):101–83. https://doi.org/10.1111/jsm.12808.
Henry G, Price G, Pryor M, Greenfield J, Jones L, Perito P, et al. Pd20–04 Observation of Local Clinical Penile Prostheses Infections Instead of Immediate Salvage Rescue / Removal: Multicenter Study with Surprising Results. J Urol. 2014;191(4S):e1–e958. https://doi.org/10.1016/j.juro.2014.02.1694.
Abbreviations and Acronyms
IPPinflatable penile prosthesis
PPpenile prosthesis
SSIsurgical site infection
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Gerard Henry reports personal fees from Boston Scientific as an investigator and consultant, Coloplast as an investigator, Medtonic as a consultant, and MicrogenDX as an investigator and consultant, outside of submitted work.
Geraldo Macedo declares no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Male and Female Surgical Interventions
Rights and permissions
About this article
Cite this article
Macedo, G.M., Henry, G.D. Preventing Infections in Prosthetic Surgery. Curr Sex Health Rep 11, 176–184 (2019). https://doi.org/10.1007/s11930-019-00208-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-019-00208-9