Abstract
Purpose of Review
While complementary and alternative medicine (CAM) use is prevalent in the general population and is known to be used in systemic rheumatic disease such as rheumatoid arthritis and systemic lupus erythematosus, its use in psoriatic arthritis (PsA) is less well-studied. The purpose of this review was to identify published data describing the use of CAM in patients with PsA.
Recent Findings
PsA patients report frequent use of CAM. Diet is believed to affect disease activity, and dietary approaches are used by patients to mitigate symptoms. Dietary supplements have been studied, especially fatty acids, with some positive results. Herbal remedies show promise, but more and better studies are needed, including evaluating medical cannabis. Studies of some the most commonly used CAM, such as acupuncture and massage, are conspicuously absent.
Summary
CAM use is common among patients with PsA. There is, however, a significant knowledge gap, and there is a critical need for rigorous research to ensure safe and effective use of CAM for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
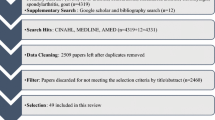
Complementary and alternative medicines (CAM) are popular strategies for treating systemic rheumatic disease, especially rheumatoid arthritis and systemic lupus erythematosus [1]. However, there is less information regarding CAM use in psoriatic arthritis (PsA). The purpose of this review is to identify published data on the use of CAM in PsA to better understand how it is used by patients with PsA and to identify knowledge and research gaps. To identify pertinent articles, we performed a literature search, with assistance from a medical librarian, utilizing PubMed, Cochrane, and Embase from inception through May 15, 2020. Abstracts were screened to identify publications relating to CAM use in PsA. Abstracts from the European League Against Rheumatism (EULAR) and American College of Rheumatology from 2015 onward were also reviewed.
Despite the lack of high-quality evidence, CAM interventions are frequently used by patients with PsA and other rheumatic diseases (Table 1). In the USA, PsA patients report using a wide range of CAMs, including massage, meditation, herbs, acupuncture, chiropractic, homeopathy, cognitive behavioral therapy, spiritual healing, reiki/therapeutic touch, naturopathy, traditional Chinese medicine, platelet-rich plasma, cannabis-based treatments, and vitamins/supplements [2]. CAM use has also been observed in PsA patients in the UK, where cod liver oil, oil of evening primrose, vitamin E, glucosamine/chondroitin, garlic, green-lipped mussel extract, starflower oil, sulfur, devil’s claw, Chinese herbs, and other vitamin/mineral supplements have been reported as popular options [5]. One of the barriers to better understanding CAM use in PsA is that some studies report CAM use in a combined group of patients with PsA and patients with only skin psoriasis, without specifying if CAM was used to relieve joint pain. Diet, herbs, acupuncture, relaxation techniques, and baths are reported to be used by European patients with psoriasis and PsA [4]. Patient members of the US-based National Psoriasis Foundation, roughly one-third of whom reported physician-diagnosed PsA, used similar therapies, though over half indicated lack of effectiveness for treating their psoriasis [3]. CAM use in psoriasis patients, some with PsA, has also been explored in the Nordic countries (Denmark, Finland, Norway, Sweden, Iceland, and the Faeroe Islands) [8]. The use of alternative approaches was reported in all countries, with Iceland having the highest rates of “alternative medicine” and “other alternative therapy” use in the last week [8]. Swedish patients with various rheumatic diseases, including rheumatoid arthritis, ankylosing spondylitis, and PsA, have reported CAM use for reasons such as pain, stiffness, and joint problems, most commonly omega-3 fatty acids, acupuncture, massage, homeopathy, and chiropractic [7]. A survey of CAM use among rheumatology patients in Leicestershire, UK, included a small proportion of PsA patients [6]. Ginger, turmeric, fish oil, CBD oil, and acupuncture were the most common therapies [6]. In rheumatology patients in Israel, acupuncture, homeopathy, diet, and spiritual healing were the most frequently reported [9]. The Australian Rheumatology Association Database evaluated complementary medicine in rheumatoid arthritis, ankylosing spondylitis, PsA, and juvenile idiopathic arthritis patients and found that the use of fatty acids, supplements, and herbs was popular [10]. CAM use has also been assessed in Chinese rheumatic disease patients, including some with PsA, and traditional Chinese medicine, acupuncture, and massage were among the most popular [11]. Whether CAM use might affect the use of traditional disease modifying anti-rheumatic drugs (DMARDs) in patients with PsA is an important question. The initiation of DMARDs was studied in 180 early inflammatory arthritis patients (EIA), 23 (12.8%) of whom had PsA [12]. Seventy-four EIA patients reported CAM use, with acupuncture being one of the most commonly used therapies [12]. CAM users were more likely to delay DMARD initiation, with a median time to use of 21.5 (IQR, 13.1–30.4) weeks compared with 15.6 (IQR, 9.4, 22.7) weeks in non-users (P value = 0.005) [12]. CAM users were also more likely to have a high disease activity assessed with the DAS28 [12]. Further study is needed to better understand how CAM use impacts uptake and adherence to DMARDs and biologics in PsA patients.
Diet
Diet is often considered an “alternative” approach to disease management in patients with PsA. Many patients with PsA believe there is a relationship between diet and PsA symptoms. When surveyed as part of a cohort of systemic rheumatic disease patients, 36% of PsA patients believed that diet had a “great influence” on their disease symptoms [13]. Patients reported that many different types of food, such as meat (pork, beef, lamb) and coffee, triggered symptoms [13]. A number of patients reported utilizing diet changes as a means of relieving disease symptoms, leading to improvements in pain, stiffness, and swelling [13]. Of 1206 psoriasis patients, 43.9% of whom self-reported PsA, 40% used a special diet for psoriasis, with gluten-free, low carbohydrate high protein, and Paleolithic diets being the most popular [14]. Although results were not reported separately for PsA, 82% took dietary supplements to treat their psoriasis, with vegetables, fish oil/omega-3, and oral vitamin D reported to be the most common and most effective [14].
Studies have evaluated specific diets as therapy for PsA. In a multicenter, open-label, prospective study, Ramadan fasting, a form of intermittent fasting lasting about 17 h daily, was studied in 37 subjects with PsA who planned to fast for the month of Ramadan [15]. Clinical presentations included peripheral arthritis in 32.4%, axial involvement in 35.1%, enthesitis in 64.9%, and dactylitis in 35.1% [15]. Following the month-long fasting period, there were significant improvements in C-reactive protein levels, Disease Activity index for PSoriatic Arthritis (DAPSA), Leeds Enthesitis Index (LEI), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), dactylitis severity score, and Psoriasis Area Severity Index (PASI) [15]. A small trial evaluated fasting and vegetarian diet in 20 patients, 10 with PsA [16]. Following a 2-week period of modified fasting, subjects were fed a vegetarian diet for 3 weeks, based on vegetables, millet, lentils, and buckwheat [16]. The self-reported arthritic symptoms improved for most of the patients during the fast and returned during the subsequent dieting period [16]. Following the 2-week fasting period, the authors found a significant correlation (r = − 0.70, P value ˂ 0.001) between serum lactoferrin levels and changes in improvement/impairment, particularly in PsA [16]. A cross-sectional observational study evaluated the relationship between adherence to Mediterranean diet, measured with a validated 14-item questionnaire [17], and disease activity in 211 PsA patients [18•]. A Mediterranean diet emphasizes fruits, vegetables, fish, and legumes with a low to moderate consumption of dairy products, eggs, and poultry and a low consumption of sweets, red meat, and wine [18•]. Low adherence to Mediterranean diet correlated with greater disease activity assessed with the DAPSA [18•].
Obesity is associated with higher disease activity in PsA, and dieting has been studied as an intervention to promote weight loss and improve disease activity. A group of 138 overweight/obese PsA patients starting TNFα blockers were randomized to either a hypocaloric diet or free self-managed diet [19]. At 6 months, subjects in the hypocaloric diet group had a significantly greater reduction in erythrocyte sedimentation rate and pain and were more likely to achieve minimal disease activity (MDA) [19]. Overall, weight loss ≥ 5% was the major independent predictor of achieving MDA, rather than a specific diet [19]. A second study, published only in abstract form, describes a 12-month randomized controlled trial in which 55 PsA patients with a BMI ≥ 30 kg/m2 were randomized to either diet, exercise, diet and exercise, or control [20]. At 12 months, all diet and exercise intervention groups were associated with improved disease activity [20]. Another abstract highlights a 12-week double-blinded, placebo-controlled trial in which 97 PsA patients were randomized to either hypocaloric diet with placebo supplementation, hypocaloric diet with omega-3 supplementation, or placebo [21]. Hypocaloric intervention appeared to control joint disease activity regardless of weight loss with no additional benefit from the omega-3 supplements [21]. The effect of weight loss through very low energy diet intervention to achieve MDA was evaluated in 46 obese PsA patients [22•]. At 6 months, BMI had significantly decreased from a median of 35.2 to 29.7 kg/m2, and significant improvements were observed for tender joint count, pain, fatigue, and DAPSA, among others [22•]. At baseline, 12 patients (29.3%) had MDA, which increased significantly to 53.7% with MDA at 6 months [22•].
While it remains unclear if a specific diet is best for PsA, it does appear that any diet leading to weight loss may be helpful in controlling arthritis symptoms. Larger, prospective trials of well-phenotyped PsA patients are needed to better understand how different diets and adherence to prescribed diets might affect disease outcomes, whether the effects are similar in diverse populations and how different diets impact clinical obesity and inflammatory biomarkers.
Dietary Supplements
Supplements have also been used as a popular complementary therapy to treat PsA. Vitamin D supplementation has been posited as beneficial based on its potential immunomodulatory effects [23]. In RANKL/M-CSF-stimulated peripheral blood mononuclear cells (PBMCs) from PsA patients, treatment with 1,25(OH)2D3 led to reductions in IL-1b, IL-17, IL-2, IFN-γ, TNF-α, IL-23, and RANTES [24]. In a 6-month open-label trial, oral 1,25-dihydroxyvitamin D3 (1,25(OH)2D3) was evaluated in 10 patients with active PsA [25]. In the intent-to-treat analysis, the mean tender joint count significantly decreased from 15.75 to 9.70 (P value ˂ 0.01), and the mean physician global assessment significantly improved from 4.45 to 2.80 (P value ˂ 0.05) [25]. There was also a non-statistically significant trend toward improvement in erythrocyte sedimentation rate [25]. The effects of vitamin D3 analogue, alphacalcidol, on clinical and laboratory parameters were assessed in 19 patients with PsA in another 6-month open-label study [26]. Ten subjects with osteopenia received alphacalcidol and were compared with 9 controls with normal bone density who did not receive alphacalcidol [26]. The authors found a significant decrease in the disease activity score (DAS28) in the patients treated with alphacalcidol from baseline to 6 months and non-significant improvements in PASI and patient’s global assessment [26]. Alphacalcidol led to significant decreases in the percentage of CD69-positive activated T cells, the percentage of IFN-γ-producing CD8-positive T lymphocytes, and serum IFN-γ levels at 3 months [26]. There were no significant clinical or immunological changes in the control group [26]. A different approach of supplementing with coenzyme Q10, vitamin E, and selenium aspartate was evaluated in a randomized, double-blind trial in patients with either PsA or erythrodermic psoriasis (EP) [27]. PsA patients were randomized to receive standard therapy together with coenzyme Q10 (50 mg/day ubiquinone acetate), vitamin E (50 mg/day RRR-α-tocopherol), and selenium aspartate (48 μg/day) [27]. The remaining PsA participants received standard therapy plus a soy lecithin placebo [27]. In PsA patients specifically, compared with placebo, this supplementation strategy led to lower PASI (16 ± 6 vs. 29 ± 10) and disease severity (1.9 ± 0.1 vs. 6.8 ± 0.2), which was measured by a severity score based on various skin and joint symptoms [27].
The use of polyunsaturated fatty acid supplementation has been evaluated as a possible treatment for PsA. Polyunsaturated ethyl ester lipids (Angiosan®) were evaluated in an 8-week open-label trial of 80 patients with psoriasis, 34 of whom had radiographic findings characteristic of PsA [28]. PASI scores decreased significantly, and joint pain in PsA improved [28]. Subjects with severe or moderate joint pain fell from 28 to 6, and 25 subjects had mild or no joint pain by the end of the trial [28]. Efamol® Marine, a combination of evening primrose oil and fish oil, was evaluated in PsA in a 9-month randomized, double-blind, placebo-controlled trial [29]. Nineteen patients were randomized to Efamol® Marine, and 19 received a liquid paraffin and vitamin E placebo [29]. Although there were no significant changes in arthritis activity in the Efamol® Marine group, leukotriene B4 levels decreased significantly compared with baseline, and serum thromboxane B2 levels were significantly lower than the placebo group [29]. In a 2-week, double-blind, placebo-controlled trial, 22 PsA patients were randomized to oral seal oil (polyunsaturated fatty acids) and compared with 21 participants receiving oral soy oil placebo [30]. A final assessment occurred 4 weeks after discontinuing treatment [30]. Seal oil was associated with improvements in patient global assessment and tender and swollen joint counts [30]. However, there were no significant differences between groups at the end of the trial in patient global assessment, joint pain intensity, tender and swollen joint counts, erythrocyte sedimentation rate, or calprotectin [30]. N-3 polyunsaturated fatty acids (PUFA) were compared with olive oil placebo in a randomized, double-blind, placebo-controlled trial [31••]. Supplementation with n-3 PUFA resulted in significant decreases (P value ˂ 0.05) at week 24 compared with baseline in tender joint count, DAS28-CRP, LEI, Spondyloarthritis Research Consortium of Canada Enthesitis Index, and PASI [31••]. However, there were no significant differences compared with the control group [31••]. By contrast, n-3 PUFA treatment did lead to statistically significant decreases in the use of NSAIDs and paracetamol compared with the control group [31••]. In a 12-week randomized, double-blind, placebo-controlled trial, n-3 long-chain (LC) PUFA and γ-linolenic acid (GLA) supplementation were evaluated in six patients with PsA and 54 patients with rheumatoid arthritis [32]. Subjects were randomized to receive either 3000 mg n-3 LC-PUFA daily, 3150 mg GLA daily, 1575 mg n-3 LC-PUFA and 1800 mg GLA daily, or 3000 mg olive oil daily [32]. The disease activity score (DAS28) decreased significantly in the 3000 mg n-3 LC-PUFA group and in the 3150 mg GLA group [32]. Furthermore, decreases in disease activity based on visual analogue scale were observed in the n-3 LC-PUFA treatment and GLA treatment, though results were not reported separately for PsA [32].
The effect of supplements in PsA remains unclear, as most studies are very small, of short duration, and/or unblinded. Blinding can be challenging when supplements have a distinct taste or odor, but creative placebos can be manufactured to mimic a supplement’s distinctive flavor and texture. While large blinded trials of adequate duration are clearly needed, such trials are expensive. As most supplements are inexpensive non-patented products, securing the necessary financing to carry out definitive trials may present a barrier for advancing this area of inquiry.
Herbal Therapies
Traditional Chinese medicine (TCM) often utilizes herbs with immunomodulatory and anti-inflammatory effects [33]. Tripterygium wilfordii Hook F (TwHF), or “thunder god vine”, is a vine-like plant native to southern China, often used to treat inflammatory and autoimmune disorders including rheumatoid arthritis, systemic lupus erythematosus, and PsA [34]. Although in rheumatoid arthritis TwHF has been shown to be non-inferior to methotrexate [35], to our knowledge, there are no English language studies systemically evaluating TwHF in PsA. Studies evaluating TwHF extracts in PsA have included few patients and evaluated them over only brief periods of time. Tripterygium reportedly led to “good to excellent results” after 20–30 days in 16 of 18 PsA patients [36]. Another study noted that 5 PsA patients had “significant improvement” or “improvement” after treatment with a TwHF extract [37].
Extracts of paeony, another traditional Chinese herb, have been evaluated in a 12-week, open-label study of 19 PsA patients [38]. Six subjects showed a decrease in DAS28 of ≥ 25% [38]. These “responders” also displayed decreases in circulating Tregs, Th1 cells, and IL-6 production [38].
A 2020 EULAR abstract evaluated the effect of plant-based delphinidin in PBMCs from 24 PsA patients and 16 healthy controls [39•]. The authors found that in vitro treatment with delphinidin led to reductions in IL-17 and IFN-γ production in PsA and controls [39•].
Curcumin, the bioactive constituent of the plant Curcuma longa (commonly known as turmeric), is a popular nutraceutical with anti-inflammatory effects that are, in part, achieved through modulation of NF-κB signaling and pro-inflammatory cytokine production, as well as affecting cyclooxygenase-2 and 5-lipoxygenase pathways [40, 41]. In vitro, curcumin significantly decreased the percentage of IFN-γ-producing CD4(+) and CD8(+) T cells and IFN-γ-producing NK and NKT cells from patients with PsA [42]. A 2016 systematic review and meta-analysis of randomized clinical trials evaluating the efficacy of turmeric and its extracts found that turmeric or curcumin was better than placebo and similar to NSAIDs or glucosamine for improving pain [41]. However, the review only identified randomized clinical trials of rheumatoid arthritis and osteoarthritis [41]. More research is needed to better understand the clinical effectiveness of turmeric or curcumin in PsA.
The use of cannabis-based treatments among patients with rheumatic diseases is common [43]. The endocannabinoid system influences both the innate and adaptive immune responses and is involved in the regulation of pain and inflammation [44, 45]. The cannabis plant contains cannabinoids Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD), which have analgesic and anti-inflammatory effects [46]. While randomized controlled trials of cannabinoids have been performed in osteoarthritis, rheumatoid arthritis, and fibromyalgia [45], we are not aware of any published data in PsA. One randomized, placebo-controlled trial with blinded outcome assessments is ongoing in patients with hand osteoarthritis and PsA, which will assess the efficacy and safety of oral CBD tablets (NCT03693833) [47]. A second clinical trial will evaluate the effects of cannabis on pain and inflammation in PsA and rheumatoid arthritis patients (NCT04269993) [48].
There are observational reports of the use of cannabis in PsA. A topical preparation (patent filed) that combined flower and seed-based extracts from cannabis improved swelling and erythema in a 55-year-old man with PsA [49, 50]. In a CreakyJoints survey of 1059 arthritis patients (9% with PsA), which evaluated the prevalence of marijuana and CBD use, 57% of patients used marijuana or CBD medically for symptoms such as pain, fatigue, and sleep problems [43]. While 97% and 93% reported that marijuana and CBD use, respectively, helped improve symptoms, only 64% of patients had discussed usage with their healthcare provider [43]. Another study evaluating medical cannabis use in 1000 rheumatology patients (10.0% with PsA) found that 126 (12.6%) reported ever using medical cannabis, with ever use among PsA patients being slightly higher at 16.0% [51]. Patients who used medical cannabis had greater pain, worse physician global assessment, and worse patient global assessment, though this was not stratified by condition [51].
Manual Therapies
There are limited studies on the use of acupuncture and chiropractic in PsA, and no studies specifically evaluating massage. An abstract reports a 39-year-old woman with PsA who was treated with acupuncture, together with topical and other medications, had a decrease in PASI and pain after a 4-week hospital stay [52]. A case report of acupuncture in a 34-year-old PsA patient found that after 14 weeks of acupuncture treatment, pain had decreased, and she no longer required pain medication [53]. A third case report of a 17-year-old with PsA found that after 4 weeks of treatment, the patient reported improvement in pain, and her Psoriatic Arthritis Impact of Disease (PsAID12) score decreased from 7 at baseline to 3.6 [54]. One open-label cohort study evaluated acupuncture in patients with long-standing psoriasis (average disease duration 16.3 years) who had failed western therapy [55]. Of the 61 patients, 25 had PsA [55]. After acupuncture, 36% of PsA patients “had complete or almost complete relief of their pains,” 16% “moderate relief,” and 48% “slight” or “no relief” [55]. A prospective open-label cohort study evaluated acupuncture treatment in PsA patients [56]. However, the primary outcome was reduction in PASI, acupuncture was not assigned randomly, and arthritic outcomes in these PsA patients were not addressed [56]. Despite the lack of high-quality evidence supporting the use of acupuncture in PsA, it is conditionally recommended for patients with active PsA by the American College of Rheumatology and the National Psoriasis Foundation [57], based on a systematic review of randomized controlled trials in osteoarthritis patients [58].
We identified only one case report of chiropractic therapy for PsA, which involved a 38-year-old man with osteoarthrosis of the cervical and thoracic spine, a 24-year history of skin psoriasis, and axial and peripheral PsA [59]. Previous chiropractic had been unhelpful [59]. He had also been treated previously with NSAIDs, PUVA, narcotics, and low-dose methotrexate [59]. After an integrated approach of chiropractic in conjunction with nutritional counseling, soft tissue manipulation, and exercise, he was able to discontinue all pain medication and had pain-free periods of up to 12 days [59].
We could identify no trials of massage for PsA. However, as with acupuncture, massage is conditionally recommended for patients with active PsA by the American College of Rheumatology and the National Psoriasis Foundation [57], based on a systematic review of randomized controlled trials of massage therapy in patients with osteoarthritis and rheumatoid arthritis [60].
Conclusions
CAM interventions are commonly used for PsA, but there remain significant knowledge gaps. While positive results have been reported in open-label trials, there is a lack of randomized controlled studies. There are very few trials that focus specifically on CAM in PsA, and frequently PsA patients are only mentioned as a subset of subjects with inflammatory arthritis or as a subset of patients with psoriatic skin disease. In particular, there is a research gap with little data to inform therapeutic decision-making regarding some of the CAM most commonly chosen by patients with PsA, such as chiropractic, acupuncture, and massage. These are critical areas for future funding to ensure the provision of the best evidence-based care for patients with PsA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Phang JK, Kwan YH, Goh H, Tan VIC, Thumboo J, Østbye T, et al. Complementary and alternative medicine for rheumatic diseases: a systematic review of randomized controlled trials. Complement Ther Med. 2018;37:143–57. https://doi.org/10.1016/j.ctim.2018.03.003.
Roberts J IV, Mandl L, Abutalib Z, Schwartzman S. Use of complementary and alternative medicine (CAM) in a psoriatic arthritis cohort [abstract]. Arthritis Rheumatol. 2019;71(suppl 10).
Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137:280–4.
Dubertret L, Mrowietz U, Ranki A, van de Kerkhof PCM, Chimenti S, Lotti T, et al. European patient perspectives on the impact of psoriasis: the EUROPSO patient membership survey. Br J Dermatol. 2006;155:729–36. https://doi.org/10.1111/j.1365-2133.2006.07405.x.
Williamson L, Dockerty JL, Dalbeth N. Treatment of psoriatic arthritis. Rheumatology (Oxford). 2004;43:938–9. https://doi.org/10.1093/rheumatology/keh189.
Tharakan CS, Ungcharoen N, Sabu J, Moorthy A. Complementary and alternative medicine in rheumatology: a survey of its use for common rheumatological conditions among multi-ethnic patients in Leicestershire. Ann Rheum Dis. 2019;78(supplement 2):A621. https://doi.org/10.1136/annrheumdis-2019-eular.6493.
Klingberg E, Wallerstedt SM, Torstenson T, Håwi G, Forsblad-d’Elia H. The use of complementary and alternative medicine in outpatients with inflammatory rheumatic diseases in Sweden. Scand J Rheumatol. 2009;38:472–80. https://doi.org/10.3109/03009740902994280.
Zachariae H, Zachariae R, Blomqvist K, Davidsson S, Molin L, Mørk C, et al. Treatment of psoriasis in the Nordic countries: a questionnaire survey from 5739 members of the psoriasis associations. Data from the Nordic quality of life study. Acta Derm Venereol. 2001;81:116–21. https://doi.org/10.1080/00015550152384254.
Breuer GS, Orbach H, Elkayam O, Berkun Y, Paran D, Mates M, et al. Use of complementary and alternative medicine among patients attending rheumatology clinics in Israel. Isr Med Assoc J. 2006;8:184–7.
Fletcher A, Staples M, Hill C, Lassere M, March L, Carroll G, et al. Use of oral complementary medicine in inflammatory arthritis: data from the Australian Rheumatology Association Database (ARAD) [abstract]. Arthritis Rheumatol. 2018;70(suppl 10).
Mok C, Pak C, Wong C, To C, Tse S, Ho L. Use of complementary and alternative medicine (CAM) in Chinese patients with rheumatic diseases: prevalence and associated demographic, clinical and social factors. Ann Rheum Dis. 2015;74(supplement 2):307. https://doi.org/10.1136/annrheumdis-2015-eular.3423.
Lahiri M, Santosa A, Teoh LK, Clayton JA, Lim SY, Teng GG, et al. Use of complementary and alternative medicines is associated with delay to initiation of disease-modifying anti-rheumatic drug therapy in early inflammatory arthritis. Int J Rheum Dis. 2017;20:567–75. https://doi.org/10.1111/1756-185X.13091.
Haugen M, Kjeldsen-Kragh J, Nordvåg BY, Førre O. Diet and disease symptoms in rheumatic diseases--results of a questionnaire based survey. Clin Rheumatol. 1991;10:401–7. https://doi.org/10.1007/bf02206660.
Afifi L, Danesh MJ, Lee KM, Beroukhim K, Farahnik B, Ahn RS, et al. Dietary behaviors in psoriasis: patient-reported outcomes from a U.S. National Survey. Dermatol Ther (Heidelb). 2017;7:227–42. https://doi.org/10.1007/s13555-017-0183-4.
Adawi M, Damiani G, Bragazzi NL, Bridgewood C, Pacifico A, Conic RRZ, et al. The impact of intermittent fasting (Ramadan fasting) on psoriatic arthritis disease activity, enthesitis, and dactylitis: a multicentre study. Nutrients. 2019;11:601. https://doi.org/10.3390/nu11030601.
Lithell H, Bruce A, Gustafsson IB, Höglund NJ, Karlström B, Ljunghall K, et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acta Derm Venereol. 1983;63:397–403.
Martínez-González MA, García-Arellano A, Toledo E, Salas-Salvadó J, Buil-Cosiales P, Corella D, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One. 2012;7:e43134. https://doi.org/10.1371/journal.pone.0043134.
• Caso F, Navarini L, Carubbi F, Picchianti-Diamanti A, Chimenti MS, Tasso M, et al. Mediterranean diet and psoriatic arthritis activity: a multicenter cross-sectional study. Rheumatol Int. 2020;40:951–8. https://doi.org/10.1007/s00296-019-04458-7. This study showed that low adherence to Mediterranean diet was associated with higher PsA disease activity.
Di Minno MND, Peluso R, Iervolino S, Russolillo A, Lupoli R, Scarpa R, et al. Weight loss and achievement of minimal disease activity in patients with psoriatic arthritis starting treatment with tumour necrosis factor α blockers. Ann Rheum Dis. 2014;73:1157–62. https://doi.org/10.1136/annrheumdis-2012-202812.
Abou-Raya A, Abou-Raya S, Helmii M. Effect of exercise and dietary weight loss on symptoms and systemic inflammation in obese adults with psoriatic arthritis: randomized controlled trial. Ann Rheum Dis. 2014;73:89–90. https://doi.org/10.1136/annrheumdis-2014-eular.2760.
Leite BF, Morimoto MA, Gomes C, Klemz BN, Genaro PS, Shivappa N, et al. Benefits of hipocaloric diet-induced weight loss on psoriatic arthritis disease activity is not improved by fish oil: the DIETA trial. J Psoriasis Psoriatic Arthritis. 2019;4:161–2. https://doi.org/10.1177/2475530319855519.
• Klingberg E, Bilberg A, Björkman S, Hedberg M, Jacobsson L, Forsblad-d’Elia H, et al. Weight loss improves disease activity in patients with psoriatic arthritis and obesity: an interventional study. Arthritis Res Ther. 2019;21:17. https://doi.org/10.1186/s13075-019-1810-5. This study showed that weight loss treatment with very low energy diet was associated with improvements in PsA disease activity, with more weight loss showing larger improvements.
Cutolo M, Plebani M, Shoenfeld Y, Adorini L, Tincani A. Vitamin D endocrine system and the immune response in rheumatic diseases. Vitam Horm. 2011;86:327–51. https://doi.org/10.1016/B978-0-12-386960-9.00014-9.
Cubillos S, Krieg N, Norgauer J. Effect of vitamin D on peripheral blood mononuclear cells from patients with psoriasis vulgaris and psoriatic arthritis. PLoS One. 2016;11:e0153094. https://doi.org/10.1371/journal.pone.0153094.
Huckins D, Felson DT, Holick M. Treatment of psoriatic arthritis with oral 1,25-dihydroxyvitamin D3: a pilot study. Arthritis Rheum. 1990;33:1723–7. https://doi.org/10.1002/art.1780331117.
Gaál J, Lakos G, Szodoray P, Kiss J, Horváth I, Horkay E, et al. Immunological and clinical effects of alphacalcidol in patients with psoriatic arthropathy: results of an open, follow-up pilot study. Acta Derm Venereol. 2009;89:140–4. https://doi.org/10.2340/00015555-0555.
Kharaeva Z, Gostova E, De Luca C, Raskovic D, Korkina L. Clinical and biochemical effects of coenzyme Q10, vitamin E, and selenium supplementation to psoriasis patients. Nutrition. 2009;25:295–302. https://doi.org/10.1016/j.nut.2008.08.015.
Lassus A, Dahlgren AL, Halpern MJ, Santalahti J, Happonen HP. Effects of dietary supplementation with polyunsaturated ethyl ester lipids (Angiosan®) in patients with psoriasis and psoriatic arthritis. J Int Med Res. 1990;18:68–73. https://doi.org/10.1177/030006059001800109.
Veale DJ, Torley HI, Richards IM, O’Dowd A, Fitzsimons C, Belch JJ, et al. A double-blind placebo controlled trial of Efamol marine on skin and joint symptoms of psoriatic arthritis. Br J Rheumatol. 1994;33:954–8. https://doi.org/10.1093/rheumatology/33.10.954.
Madland TM, Björkkjaer T, Brunborg LA, Fröyland L, Berstad A, Brun JG. Subjective improvement in patients with psoriatic arthritis after short-term oral treatment with seal oil. A pilot study with double blind comparison to soy oil. J Rheumatol. 2006;33:307–10.
•• Kristensen S, Schmidt EB, Schlemmer A, Rasmussen C, Johansen MB, Christensen JH. Beneficial effect of n-3 polyunsaturated fatty acids on inflammation and analgesic use in psoriatic arthritis: a randomized, double blind, placebo-controlled trial. Scand J Rheumatol. 2018;47:27–36. https://doi.org/10.1080/03009742.2017.1287304. This study showed that n-3 polyunsaturated fatty acid supplementation permitted decreased use of NSAIDs and paracetamol and led to a decrease in leukotriene B4 levels.
Dawczynski C, Hackermeier U, Viehweger M, Stange R, Springer M, Jahreis G. Incorporation of n-3 PUFA and γ-linolenic acid in blood lipids and red blood cell lipids together with their influence on disease activity in patients with chronic inflammatory arthritis - a randomized controlled human intervention trial. Lipids Health Dis. 2011;10:130. https://doi.org/10.1186/1476-511X-10-130.
Cyong J, Otsuka Y. A pharmacological study of the anti-inflammatory activity of Chinese herbs. A review. Acupunct Electrother Res. 1982;7:173–202. https://doi.org/10.3727/036012982816952116.
Ma J, Dey M, Yang H, Poulev A, Pouleva R, Dorn R, et al. Anti-inflammatory and immunosuppressive compounds from Tripterygium wilfordii. Phytochemistry. 2007;68:1172–8. https://doi.org/10.1016/j.phytochem.2007.02.021.
Zhou Y-Z, Zhao L-D, Chen H, Zhang Y, Wang D-F, Huang L-F, et al. Comparison of the impact of Tripterygium wilfordii hook F and methotrexate treatment on radiological progression in active rheumatoid arthritis: 2-year follow up of a randomized, non-blinded, controlled study. Arthritis Res Ther. 2018;20:70. https://doi.org/10.1186/s13075-018-1563-6.
Xu WY, Zheng JR, Lu XY. Tripterygium in dermatologic therapy. Int J Dermatol. 1985;24:152–7. https://doi.org/10.1111/j.1365-4362.1985.tb05746.x.
Lipsky PE, Tao XL. A potential new treatment for rheumatoid arthritis: thunder god vine. Semin Arthritis Rheum. 1997;26:713–23. https://doi.org/10.1016/s0049-0172(97)80040-6.
Wang YN, Zhang Y, Wang Y, Zhu DX, Xu LQ, Fang H, et al. The beneficial effect of total glucosides of paeony on psoriatic arthritis links to circulating Tregs and Th1 cell function. Phytother Res. 2014;28:372–81. https://doi.org/10.1002/ptr.5005.
• Mavropoulos A, Tsiogkas S, Skyvalidas D, Liaskos C, Roussaki-Schulze A, Zafiriou E, et al. Delphinidin dose-dependently diminishes peripheral IL-17 and IFN-γ producing lymphocytes in psoriatic arthritis. Ann Rheum Dis. 2020;79(supplement 1):1124. This study demonstrated that in vitro treatment with delphinidin of peripheral blood mononuclear cells from patients with PsA led to reductions in IL-17 and IFN-γ production.
Pulido-Moran M, Moreno-Fernandez J, Ramirez-Tortosa C, Ramirez-Tortosa M. Curcumin and health. Molecules. 2016;21:264. https://doi.org/10.3390/molecules21030264.
Daily JW, Yang M, Park S. Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: a systematic review and meta-analysis of randomized clinical trials. J Med Food. 2016;19:717–29. https://doi.org/10.1089/jmf.2016.3705.
Skyvalidas DΝ, Mavropoulos A, Tsiogkas S, Dardiotis E, Liaskos C, Mamuris Z, et al. Curcumin mediates attenuation of pro-inflammatory interferon γ and interleukin 17 cytokine responses in psoriatic disease, strengthening its role as a dietary immunosuppressant. Nutr Res. 2020;75:95–108. https://doi.org/10.1016/j.nutres.2020.01.005.
Gelman L. 57% of arthritis patients have tried marijuana or cbd for medical reasons (and more than 90% say it helped) [Internet]. CreakyJoints. 2019 [cited 2020 May 4]. Available from: https://creakyjoints.org/eular-2019/medical-marijuana-cbd-usage-arthritis-patients-study/.
Barrie N, Manolios N. The endocannabinoid system in pain and inflammation: its relevance to rheumatic disease. Eur J Rheumatol. 2017;4:210–8. https://doi.org/10.5152/eurjrheum.2017.17025.
Fitzcharles M-A, Ste-Marie PA, Häuser W, Clauw DJ, Jamal S, Karsh J, et al. Efficacy, tolerability, and safety of cannabinoid treatments in the rheumatic diseases: a systematic review of randomized controlled trials. Arthritis Care Res (Hoboken). 2016;68:681–8. https://doi.org/10.1002/acr.22727.
Ko GD, Bober SL, Mindra S, Moreau JM. Medical cannabis - the Canadian perspective. J Pain Res. 2016;9:735–44. https://doi.org/10.2147/JPR.S98182.
CBD Treatment in hand osteoarthritis and psoriatic arthritis [Internet]. clinicaltrials.gov. [cited 2020 May 20]. Available from: https://clinicaltrials.gov/ct2/show/NCT03693833.
Impact of cannabis on pain and inflammation among patients with rheumatoid or psoriatic arthritis [Internet]. clinicaltrials.gov. [cited 2020 June 3]. Available from: https://clinicaltrials.gov/ct2/show/NCT04269993.
Nascimento Menezes PM, Valença Pereira EC, Gomes da Cruz Silva ME, da Silva BAO, de Souza Duarte Filho LAM, de Lima Araújo TC, et al. Cannabis and cannabinoids on treatment of inflammation: a patent review. Recent Pat Biotechnol 2019;13:256–267. https://doi.org/10.2174/1872208313666190618124345.
Lansky EP. Pharmaceutical and cosmeceutical compositions containing cannabis flower and seed extracts. 2010.
Fitzcharles M-A, Rampakakis E, Sampalis J, Shir Y, Cohen M, Starr M, et al. Medical cannabis use by rheumatology patients following recreational legalization: a prospective observational study of 1000 patients in Canada. ACR Open Rheumatol. 2020;2:286–93. https://doi.org/10.1002/acr2.11138.
Kendler M, Shimshoni R, Lasaroff I. Fallbericht: psoriasis vulgaris et osteoarthritis. Deutsche Zeitschrift für Akupunktur. 2004;47:46–8. https://doi.org/10.1078/0415-6412-00040.
Chiu E. Psoriatic arthritis managed with multiple styles of acupuncture: a case report. Meridians. 2016;3:17–22.
Marchetti G, Vittori A, Mascilini I, Francia E, Picardo SG. Acupuncture for pain management in pediatric psoriatic arthritis: a case report. Acupunct Med. 2020. https://doi.org/10.1177/0964528420920281.
Liao SJ, Liao TA. Acupuncture treatment for psoriasis: a retrospective case report. Acupunct Electrother Res. 1992;17:195–208. https://doi.org/10.3727/036012992816357611.
Chen P, Xin T, Zeng Y. Effects of acupuncture on Chinese adult patients with psoriatic arthritis: a prospective cohort study. Res Rev J Med Health Sci. 2017;6:19–23.
Singh JA, Guyatt G, Ogdie A, Gladman DD, Deal C, Deodhar A, et al. 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol 2019;71:5–32. https://doi.org/10.1002/art.40726.
Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, et al. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med. 2014;14:312. https://doi.org/10.1186/1472-6882-14-312.
Green BN. Chiropractic management of a case of combined osteoarthrosis and psoriatic arthritis. J Sports Chiropract Rehabil. 2000;14:75–83.
Nelson NL, Churilla JR. Massage therapy for pain and function in patients with arthritis: a systematic review of randomized controlled trials. Am J Phys Med Rehabil. 2017;96:665–72. https://doi.org/10.1097/PHM.0000000000000712.
Acknowledgments
We would like to thank Bridget Jivanelli and Sarah Page from the Hospital for Special Surgery medical library for their assistance with the literature review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Roberts IV has no conflicts of interest to disclose. Dr. Lisa Mandl has the following conflicts of interest to disclose: Annals of Internal Medicine (Associate Editor), UpToDate (Royalties), and Regeneron Pharmaceuticals (Research support).
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Complementary and Alternative Medicine
Rights and permissions
About this article
Cite this article
Roberts, J.A., Mandl, L.A. Complementary and Alternative Medicine Use in Psoriatic Arthritis Patients: a Review. Curr Rheumatol Rep 22, 81 (2020). https://doi.org/10.1007/s11926-020-00956-x
Published:
DOI: https://doi.org/10.1007/s11926-020-00956-x