Abstract
Purpose of the Review
Progressive ankylosis is a feared consequence of long-standing axial spondyloarthritis. We aim to critically review current insights into the effect of therapy, the molecular pathways involved in this process, and to present a model explaining the sequence of events.
Recent Findings
Long-term follow-up data suggest that successful control of inflammation may slow down radiographic progression of disease in axial spondyloarthritis. Structural effects of new therapies such as interleukin-17 targeting need to be further studied. Bone loss and architectural changes could act as driver for the tissue remodeling process trying to maintain spinal stability in the presence of inflammation.
Summary
Despite some progress, the nature and mechanisms of new bone formation in axial spondyloarthritis still remain incompletely understood. However, long-term control of inflammation appears critical to avoid progressive disability due to structural damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
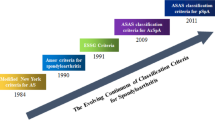
Progressive bony ankylosis of the spine is a daunting perspective for patients diagnosed with axial spondyloarthritis (AxSpA). The structural progression of disease causes loss of mobility and disability. AxSpA includes subtypes ankylosing spondylitis and non-radiographic AxSpA, separate entities discriminated by the structural damage to the sacroiliac joints and spine that is visible on conventional X-ray images [1]. Non-radiographic AxSpA patients do not show such signs of radiographic damage, but over time, at least a group of these patients will evolve towards ankylosing spondylitis [2].
The initial clinical presentation of AxSpA is usually triggered by inflammation: back pain, typically occurring at night or when resting, improving with exercise and accompanied by extended stiffness. In patients with ankylosing spondylitis, structural damage progressively becomes an important burden [3]. Treatment strategies have rapidly evolved since the beginning of the century. In case first-line non-steroidal anti-inflammatory drugs fail to achieve a satisfactory clinical response, patients are treated with cytokine-targeting biological drugs (antibodies or soluble receptors). Inhibitors of tumor necrosis factor have been used for more than 10 years with impressive clinical success and appear equally potent for both subgroups of patients with AxSpA [4•]. More recently, targeting interleukin-17 (IL-17) has been introduced [5, 6]. Other targets in the IL-23-IL-17 axis of immune activation are under further clinical investigation [7].
Despite the clinical successes achieved, many questions remain: the nature and mechanism of progressive ankylosis are still not well understood and the relationship between inflammation and new bone formation still being debated [8, 9]. This review discusses incremental steps in finding answers to these challenges as long-term effects of the different therapeutic interventions are slowly emerging. We also present an emerging paradigm integrating inflammation, inflammation-induced bone loss, and new bone formation. The review mainly discusses data presented in the literature between 2012 and 2016. A PubMed search was performed with search string: (“ankylosing spondylitis” OR “spondyloarthritis”) AND (“structural disease progression” OR “ankylosis” OR “new bone formation”).
Old and New Targets: Impact of Treatment on Structural Disease Progression
The great success of different anti-TNF strategies in the treatment of patients with AxSpA triggered considerable anticipation that the clinical effects would easily translate into effects on radiographic progression of disease, as was witnessed in patients with rheumatoid arthritis. However, initial comparisons between the prospective clinical trial populations and the historic OASIS cohort did not show such a beneficial effect within a 2-year time window [10,11,12]. These initial observations were obviously not without intrinsic limitations, in particular with regard to the historic control population and the relatively short-term evaluation of the process. More recent longer-term follow-up data of AxSpA patients treated with TNF inhibitors indicate a slow but detectable effect on radiographic disease progression [13,14,15•]. The recent study by Arends et al. nicely demonstrated that even in patients treated with TNF blocking agents a linear progression is seen within the first 4 years of therapy but that, subsequently, the progression curves flatten in individual patients [15•]. Whether this is due to a direct effect on new bone formation or secondary to a sustained effect on inflammation for instance preventing the occurrence of new disease sites in the spine [16] or normalizing bone metabolism remains unknown [17].
Data on NSAID use in patients with AxSpA first indicated that sustained and continuous NSAID intake could have a significant effect on structural disease progression [18, 19]. Such an effect was explained by not only the impact of the drugs on inflammation, but also the potential direct effects on the differentiating cells in the new bone formation process were hypothesized. However, more recent work did not confirm this earlier observation [20••]. The ENRADA trial included 85 AxSpA patients that received continuous treatment with diclofenac (62 completing the study) and 82 patients that used diclofenac on demand (60 completing the study) for 2 years. Radiographic progression was not statistically different between both groups, and average values were even higher in those patients treated continuously than in those with on demand use. This lack of replication more than a decade after the initial observation could suggest that the initial observations were false positive. However, gradual shifts in the patient population that is considered eligible for trial recruitment by their treating physicians may also explain the discrepancy. It cannot be excluded that the widespread availability of anti-TNF drugs has an impact on the recruitment of patients in trials and that patients with severe inflammation that would benefit most from any intervention were less considered. A post-study analysis of the original celecoxib trial from Wanders et al., demonstrating an effect of continuous celecoxib use on structural disease progression [18], revealed that the patient population that benefited most from the intervention were patients with elevated CRP and thus most likely more severe disease [21].
New therapies are becoming available for the treatment of patients with AxSpA. Secukinumab, the first anti-IL-17 biologic on the market in this indication, demonstrated very good efficacy against signs and symptoms of disease [5, 6]. In the pivotal phase III studies (MEASURE-1 and MEASURE-2), structural disease progression was also evaluated after 2 years [6]. No radiographic progression was observed in ∼80% of the patients receiving secukinumab over 104 weeks. The mean change in modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) was only 0.30 ± 2.53 in the secukinumab treated group, with no major difference between studied doses. Among patients that showed disease progression, male sex, baseline syndesmophytes, and elevated CRP were identified as predictive factors. The reported changes in mSASSS through 2 years appear lower than those reported in earlier observational and interventional studies in ankylosing spondylitis. However, whether an eventual difference in effect size measured in single trials between different biological translates into real-life differences for patients remains elusive. The analysis supports the concept that blocking IL-17 does not increase or accelerate structural disease progression and may even retard the process. Again, comparisons between drugs across different studies spanning more than a decade are challenging and error-prone as patient characteristics and selection may have changed together with the successful management of disease after the introduction of TNF blockers.
Links Between Inflammation and New Bone Formation
The abovementioned clinical studies and a number of animal model studies have triggered a debate on the relationship between inflammation and new bone formation [9, 22]. Over the last decade, the summarizing view has emerged that inflammation and new bone formation are linked but to a large extent molecularly and cellular uncoupled processes [22,23,24]. The existence of the link has been supported by the long-term clinical observations in patients treated with anti-TNF drugs, the more recent and still preliminary evidence on IL-17 targeting, and by the careful sequential analysis of affected areas using MRI imaging [25, 26]. The current paradigm suggests that fatty lesions are gradually replacing areas of active inflammation in the spine and sacroiliac joints. This change in microenvironment is permissive for the further evolution towards new bone formation and ankylosis [24, 27••], albeit that the suggested sequence of inflammation, fat metaplasia, and bone formation is still debated [28]. Additional circumstantial evidence has come from histological studies performed on a unique series of spinal specimens from patients undergoing corrective surgery [29••]. The images support the concept that the fatty lesions on MRI imaging are part of a transitory event that includes or is intimately associated with the presence of bone forming cells. Although attractive and progressively supported by circumstantial evidence, this view may not encompass all aspects of ankylosis as new syndesmophytes can be seen in sites without documentation of prior inflammation [30]. The scattered imaging studies, however, do not exclude the prior existence of inflammation that has not been captured, as the precise kinetics and duration of inflammatory changes in the bones of patients with AxSpA are not sufficiently understood [25,26,27,28,29••].
The molecular pathways associated with new bone formation appear different from those that are driving inflammation [22]. Initial evidence that IL-22 was a driving factor in new bone formation in the enthesitis-driven arthritis model, triggered by systemic overexpression of IL-23 [31], was only confirmed in specific in vitro settings [32]. In contrast, earlier animal model studies, specifically dedicated to the process of new bone formation, have suggested a role for growth factor signaling cascades such as bone morphogenetic proteins (BMPs), Wnts, and Hedgehogs [8]. The BMP cascade drives endochondral bone formation during development and growth [33]. Inhibition of BMP signaling by overexpression of its antagonist noggin inhibits the growth of ankylosing enthesophytes in a spontaneous mouse model of ankylosing enthesitis [34]. Wnts play an important role in direct bone formation during skeletal modeling and remodeling and stimulate the last phases of endochondral bone formation [33]. Inhibition of Dickkopf-1, a Wnt antagonist, shifts the phenotypes of mouse arthritis models from destructive towards ankylosing [35], not only in peripheral but also in the sacroiliac joints resulting in fusion [36]. Hedgehog signaling has been specifically associated with chondrocyte hypertrophy [33]. A chemical antagonist of the pathway inhibits progressive new bone formation in mouse models [37].
Translational confirmation of the animal model concepts has been a challenge. Biomarker studies have somewhat corroborated the presence of elevated levels of growth factors that would stimulate bone formation or lower levels of their antagonists but such studies have limitations. Different research groups have tried to measure activation of the growth factor cascades as biomarkers for new bone formation. BMP-2 and BMP-7 serum levels were found to be upregulated in patients with AxSpA and correlated with disease activity assessments [38]. BMP-4 and BMP-7 serum levels were also linked to radiographic progression [39]. However, most of the data on BMP levels are based on small and relatively heterogeneous cohorts, and a validated biomarker for the activity of this pathway in AxSpA has not yet emerged.
More data are available on Dickkopf-1 (DKK1): in the original report demonstrating that inhibition of DKK1 triggers joint remodeling, serum levels in patients with ankylosing spondylitis were very low [35]. Further work indicated that high levels of functional DKK1 predict protection against syndesmophyte formation and thus radiographic progression in this patient group [40]. However, Daoussis et al. reported that serum levels are elevated in AxSpA patients but that the function of DKK1 is impaired [41]. Effectively, differences exist between a classical sandwich assay that measures DKK1 levels in serum and a functional assay that includes binding to the LRP5 Wnt receptor. Further studies confirmed not only that functional DKK1 levels are lower in the serum of patients with ankylosing spondylitis but also that levels are inversely associated with radiographic severity of disease [42]. Similarly, levels of sclerostin, another Wnt antagonist, also appear to be lower in patients with AxSpA as compared to controls [40, 43].
However, further investigations are needed to validate these molecules as true biomarkers of the ankylosing process. Most reports are cross-sectional studies, lack further prospective validation, and have limited sample size. In addition, evaluation of markers associated with bone turnover, either positive or negative, is hindered by the general effect of inflammation on bone remodeling that most likely supersedes markers of bone formation derived from the small number of developing syndesmophytes. Taking this perspective into account, growth factors such as Wnt and BMPs are better viewed as paracrine and autocrine factors that are concentrated within the extracellular matrix rich joint tissues. Thus, their systemic concentrations may not reflect what is happening in the target tissues. Some growth factors, in particular Wnts that have a lipid tail, are relatively insoluble and bind to extracellular matrix components.
Another challenge is the elucidation of the precise temporospatial signaling relationship between the disease-driving cytokines IL-17 and TNF and the activation of growth factor cascades. Gradually, the view is emerging that TNF and IL-17 have a mostly negative impact on chondro- or osteogenic differentiation, at least not only in vitro setups but also in vivo. Indeed, in the human TNF transgenic mouse model, which is characterized by persistent high levels of TNF, no tissue remodeling or repair is seen and the disease is strictly erosive [35]. However, in laboratory setups where the proinflammatory cytokines are added to differentiating cells after initiation of the differentiation process, their effect seems inversed and they may stimulate new bone formation. In particular, synergistic effects between IL-17 and BMP-2 have been demonstrated [44]. Importantly, in some in vivo situations, such as fracture healing, IL-17A appears to be part of the initial factors critical for the inflammatory onset of fracture repair. In fracture healing, IL-17 is produced by γδ T cells [45]. Again, this highlights the urgent need to obtain better translational data based on the analysis of the tissues and cells involved in patients.
Debating the Impact of Genetics on Structural Disease Progression
AxSpA and, in particular, ankylosing spondylitis are highly inheritable disorders and typically defined as complex diseases with interaction of acquired and genetic factors. The discovery of disease susceptibility markers has further fueled genetic studies looking at radiographic progression. Among these, roles for the RANK/RANKL system and for PTGS2 have been suggested [46••]. The potential role for RANK points towards effects on osteoclasts, the inflammation-driven bone breakdown cellular machinery. Again, the current studies have limitations. Most cohorts are composed of patients with ankylosing spondylitis and have largely or completely excluded patients with non-radiographic AxSpA. Thus, only patients with existing radiographic damage have been included. Ideally, patients with and without radiographic progression should be compared. Again, the dynamics of the disease processes should be better understood, with current evidence suggesting a steady progression of disease in a large number, but most likely not all patients diagnosed with non-radiographic AxSpA.
A New Theoretical Framework
Based on all these observations, a new theoretical framework is presented here. In this concept, inflammation is the driver of bone loss in the spine or in the sacroiliac joints, as well as of bone erosions. These processes are driven by differentiation and activation of osteoclasts. Trabecular bone loss has been clearly and repeatedly demonstrated in the spine of patients with AxSpA using imaging and biomarkers [17]. A recent study by Haroon et al. compared bone density, structure, and strength between patients with ankylosing spondylitis and controls not only by classical bone densitometry but also by high-resolution peripheral quantitative CT and finite element analysis [47•]. Patients with ankylosing spondylitis have worse bone mineral density, microarchitecture, and strength at peripheral sites when compared to non-ankylosing spondylitis subjects in multiple regression analysis taking into account age and sex. Also, strength parameters, such as bone stiffness and stress, as estimated by finite element analysis, were significantly worse in patients than that of non-ankylosing spondylitis subjects. At the spine level, bone mineral density did not differ between patients and controls despite differences in bone microarchitecture. The small sample number and technical limitations could explain some of these discrepancies. The presence of syndesmophytes is another factor that underlines the limitations of densitometry in this context as earlier work and the clinical fracture incidence highlight the osteoporotic nature of the inflamed spine.
In the model proposed here, microarchitectural changes will affect the mechanical properties of the spine and should trigger a biomechanical response to sustain structure and stability (Fig. 1). However, the presence of inflammation is acting as an inhibitory mechanism on the normal bone cycle. Therefore, osteoblasts in the trabecular bone cannot compensate for the bone loss. As an alternative, periosteal osteoprogenitor cells are called upon to stabilize the spine by forming syndesmophytes eventually bridging the intervertebral space. Thus, the anabolic reaction that characterized structural disease progression in AxSpA could be a reactive effort to increase spinal stability. Based on this idea, it is not difficult to imagine that inflammation-driven bone loss triggers bone repair but at anatomically distinct sites. Since inflammation in the trabecular bone remains an issue if not treated, new bone formation presenting as eventually ankylosing syndesmophtyes could provide such stability to an inflammation-driven unstable spine. Sustained treatment will be required to overcome the initial loss of stability triggered by inflammation and preventing new disease sites. This may explain the delayed but increasingly recognized long-term effects of targeting TNF. Whether specific targeting of IL-17 has differential effects on bone loss and subsequently on new bone formation remains to be demonstrated but should indeed be a research priority. The fatty metaplasia seen during the process could be a signaling center for syndesmophyte formation. Successful treatment of the disease should not lead to acceleration of ankylosis as the trabecular bone can simultaneously recover, decreasing the need for external stabilization.
Proposed sequence of events leading to ankylosis in axial spondyloarthritis. Inflammation at the enthesis, vertebral body, and synovium is triggered by inflammatory and biomechanical stress leading to bone loss. Reduced bone strength triggers a stabilizing anabolic effort resulting in syndesmophyte formation and progressive ankylosis. Successful treatment reduces inflammation and allows the bone metabolism to normalize, thereby taking away instability as driver of ankylosis
Conclusion
Despite the vastly improved treatment options for patients with axial spondyloarthritis, progressive ankylosis remains a specific concern. Increasing evidence suggests that long-term sustained control of inflammation is necessary in patients at risk. A key role for inflammation-induced instability in triggering the remodeling response is proposed. Optimal control of disease progression will likely require therapies that target both inflammation and bone turnover.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Taurog JD, Chhabra A, Colbert RA. Ankylosing spondylitis and axial spondyloarthritis. N Engl J Med. 2016;374(26):2563–74. doi:10.1056/NEJMra1406182.
Poddubnyy D, Rudwaleit M, Haibel H, Listing J, Marker-Hermann E, Zeidler H, et al. Rates and predictors of radiographic sacroiliitis progression over 2 years in patients with axial spondyloarthritis. Ann Rheum Dis. 2011;70(8):1369–74. doi:10.1136/ard.2010.145995.
Machado P, Landewe R, Braun J, Hermann KG, Baker D, van der Heijde D. Both structural damage and inflammation of the spine contribute to impairment of spinal mobility in patients with ankylosing spondylitis. Ann Rheum Dis. 2010;69(8):1465–70. doi:10.1136/ard.2009.124206.
• Callhoff J, Sieper J, Weiss A, Zink A, Listing J. Efficacy of TNFalpha blockers in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: a meta-analysis. Ann Rheum Dis. 2015;74(6):1241–8. doi:10.1136/annrheumdis-2014-205322. This study provides an interesting summary on the use of TNF inhibitors in axial SpA.
Baeten D, Baraliakos X, Braun J, Sieper J, Emery P, van der Heijde D, et al. Anti-interleukin-17A monoclonal antibody secukinumab in treatment of ankylosing spondylitis: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382(9906):1705–13. doi:10.1016/S0140-6736(13)61134-4.
Baeten D, Sieper J, Braun J, Baraliakos X, Dougados M, Emery P, et al. Secukinumab, an interleukin-17A inhibitor, in ankylosing spondylitis. N Engl J Med. 2015;373(26):2534–48. doi:10.1056/NEJMoa1505066.
Poddubnyy D, Hermann KG, Callhoff J, Listing J, Sieper J. Ustekinumab for the treatment of patients with active ankylosing spondylitis: results of a 28-week, prospective, open-label, proof-of-concept study (TOPAS). Ann Rheum Dis. 2014;73(5):817–23. doi:10.1136/annrheumdis-2013-204248.
Lories RJ, Haroon N. Bone formation in axial spondyloarthritis. Best Pract Res Clin Rheumatol. 2014;28(5):765–77. doi:10.1016/j.berh.2014.10.008.
Maksymowych WP, Elewaut D, Schett G. Motion for debate: the development of ankylosis in ankylosing spondylitis is largely dependent on inflammation. Arthritis Rheum. 2012;64(6):1713–9. doi:10.1002/art.34442.
van der Heijde D, Landewe R, Baraliakos X, Houben H, van Tubergen A, Williamson P, et al. Radiographic findings following two years of infliximab therapy in patients with ankylosing spondylitis. Arthritis Rheum. 2008;58(10):3063–70. doi:10.1002/art.23901.
van der Heijde D, Landewe R, Einstein S, Ory P, Vosse D, Ni L, et al. Radiographic progression of ankylosing spondylitis after up to two years of treatment with etanercept. Arthritis Rheum. 2008;58(5):1324–31. doi:10.1002/art.23471.
van der Heijde D, Salonen D, Weissman BN, Landewe R, Maksymowych WP, Kupper H, et al. Assessment of radiographic progression in the spines of patients with ankylosing spondylitis treated with adalimumab for up to 2 years. Arthritis Res Ther. 2009;11(4):R127. doi:10.1186/ar2794.
Haroon N, Inman RD, Learch TJ, Weisman MH, Lee M, Rahbar MH, et al. The impact of tumor necrosis factor alpha inhibitors on radiographic progression in ankylosing spondylitis. Arthritis Rheum. 2013;65(10):2645–54. doi:10.1002/art.38070.
Baraliakos X, Haibel H, Listing J, Sieper J, Braun J. Continuous long-term anti-TNF therapy does not lead to an increase in the rate of new bone formation over 8 years in patients with ankylosing spondylitis. Ann Rheum Dis. 2014;73(4):710–5. doi:10.1136/annrheumdis-2012-202698.
• Maas F, Arends S, Brouwer E, Essers I, van der Veer E, Efde M et al. Reduction in spinal radiographic progression in ankylosing spondylitis patients receiving prolonged treatment with TNF-alpha inhibitors. Arthritis Care Res (Hoboken). 2016. doi:10.1002/acr.23097. Novel data about the potential effects of anti-TNF on radiographic progression.
Song IH, Hermann KG, Haibel H, Althoff CE, Poddubnyy D, Listing J, et al. Prevention of new osteitis on magnetic resonance imaging in patients with early axial spondyloarthritis during 3 years of continuous treatment with etanercept: data of the ESTHER trial. Rheumatology (Oxford). 2015;54(2):257–61. doi:10.1093/rheumatology/keu263.
Carter S, Lories RJ. Osteoporosis: a paradox in ankylosing spondylitis. Curr Osteoporos Rep. 2011;9(3):112–5. doi:10.1007/s11914-011-0058-z.
Wanders A, Heijde D, Landewe R, Behier JM, Calin A, Olivieri I, et al. Nonsteroidal antiinflammatory drugs reduce radiographic progression in patients with ankylosing spondylitis: a randomized clinical trial. Arthritis Rheum. 2005;52(6):1756–65. doi:10.1002/art.21054.
Poddubnyy D, Rudwaleit M, Haibel H, Listing J, Marker-Hermann E, Zeidler H, et al. Effect of non-steroidal anti-inflammatory drugs on radiographic spinal progression in patients with axial spondyloarthritis: results from the German Spondyloarthritis Inception Cohort. Ann Rheum Dis. 2012;71(10):1616–22. doi:10.1136/annrheumdis-2011-201252.
•• Sieper J, Listing J, Poddubnyy D, Song IH, Hermann KG, Callhoff J, et al. Effect of continuous versus on-demand treatment of ankylosing spondylitis with diclofenac over 2 years on radiographic progression of the spine: results from a randomised multicentre trial (ENRADAS). Ann Rheum Dis. 2016;75(8):1438–43. doi:10.1136/annrheumdis-2015-207897. Important data about the difficulties to demonstrate a structure modifying effect of NSAID therapy.
Kroon F, Landewe R, Dougados M, van der Heijde D. Continuous NSAID use reverts the effects of inflammation on radiographic progression in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71(10):1623–9. doi:10.1136/annrheumdis-2012-201370.
Lories RJ, Schett G. Pathophysiology of new bone formation and ankylosis in spondyloarthritis. Rheum Dis Clin North Am. 2012;38(3):555–67. doi:10.1016/j.rdc.2012.08.003.
Maksymowych WP. Disease modification in ankylosing spondylitis. Nat Rev Rheumatol. 2010;6(2):75–81. doi:10.1038/nrrheum.2009.258.
Maksymowych WP, Morency N, Conner-Spady B, Lambert RG. Suppression of inflammation and effects on new bone formation in ankylosing spondylitis: evidence for a window of opportunity in disease modification. Ann Rheum Dis. 2013;72(1):23–8. doi:10.1136/annrheumdis-2011-200859.
Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ. Fat metaplasia and backfill are key intermediaries in the development of sacroiliac joint ankylosis in patients with ankylosing spondylitis. Arthritis Rheumatol. 2014;66(11):2958–67. doi:10.1002/art.38792.
Chiowchanwisawakit P, Lambert RGW, Conner-Spady B, Maksymowych WP. Focal fat lesions at vertebral corners on magnetic resonance imaging predict the development of new syndesmophytes in ankylosing spondylitis. Arthritis Rheum-Us. 2011;63(8):2215–25. doi:10.1002/art.30393.
•• Machado PM, Baraliakos X, van der Heijde D, Braun J, Landewe R. MRI vertebral corner inflammation followed by fat deposition is the strongest contributor to the development of new bone at the same vertebral corner: a multilevel longitudinal analysis in patients with ankylosing spondylitis. Ann Rheum Dis. 2016;75(8):1486–93. doi:10.1136/annrheumdis-2015-208011. The paper provides good evidence for a sequential process leading to ankylosis.
Baraliakos X, Heldmann F, Callhoff J, Listing J, Appelboom T, Brandt J, et al. Which spinal lesions are associated with new bone formation in patients with ankylosing spondylitis treated with anti-TNF agents? A long-term observational study using MRI and conventional radiography. Ann Rheum Dis. 2014;73(10):1819–25. doi:10.1136/annrheumdis-2013-203425.
•• Baraliakos X, Boehm H, Samir A, Schett G, Braun J. Which cells correspond to typical signals for fatty and inflammatory lesions seen on MRI in AS? Clin Exp Rheumatol. 2016;34(4):744. New knowledge on the histological appearance of fatty lesions on MRI in SpA.
van der Heijde D, Machado P, Braun J, Hermann KGA, Baraliakos X, Hsu B, et al. MRI inflammation at the vertebral unit only marginally predicts new syndesmophyte formation: a multilevel analysis in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71(3):369–73. doi:10.1136/annrheumdis-2011-200208.
Sherlock JP, Joyce-Shaikh B, Turner SP, Chao CC, Sathe M, Grein J, et al. IL-23 induces spondyloarthropathy by acting on ROR-gammat+ CD3+CD4-CD8- entheseal resident T cells. Nat Med. 2012;18(7):1069–76. doi:10.1038/nm.2817.
El-Sherbiny Y, Elzayadi A, Fragkakis EM, Cuthbert R, Baboolal T, Jones E et al. IL-22 drives the proliferation and differentiation of human bone marrow mesenchymal stem cells (MSCs); a novel pathway that may contribute to aberrant new bone formation in human spa and beyond. Arthritis & Rheumatology. 2015;67
Lefebvre V, Bhattaram P. Vertebrate skeletogenesis. Curr Top Dev Biol. 2010;90:291–317. doi:10.1016/S0070-2153(10)90008-2.
Lories RJ, Derese I, Luyten FP. Modulation of bone morphogenetic protein signaling inhibits the onset and progression of ankylosing enthesitis. J Clin Invest. 2005;115(6):1571–9. doi:10.1172/JCI23738.
Diarra D, Stolina M, Polzer K, Zwerina J, Ominsky MS, Dwyer D, et al. Dickkopf-1 is a master regulator of joint remodeling. Nat Med. 2007;13(2):156–63. doi:10.1038/nm1538.
Uderhardt S, Diarra D, Katzenbeisser J, David JP, Zwerina J, Richards W, et al. Blockade of Dickkopf (DKK)-1 induces fusion of sacroiliac joints. Ann Rheum Dis. 2010;69(3):592–7. doi:10.1136/ard.2008.102046.
Ruiz-Heiland G, Horn A, Zerr P, Hofstetter W, Baum W, Stock M, et al. Blockade of the hedgehog pathway inhibits osteophyte formation in arthritis. Ann Rheum Dis. 2012;71(3):400–7. doi:10.1136/ard.2010.148262.
Park MC, Park Y, Lee SK. Relationship of bone morphogenetic proteins to disease activity and radiographic damage in patients with ankylosing spondylitis. Scand J Rheumatol. 2008;37(3):200–4. doi:10.1080/03009740701774941.
Chen HA, Chen CH, Lin YJ, Chen PC, Chen WS, Lu CL, et al. Association of bone morphogenetic proteins with spinal fusion in ankylosing spondylitis. J Rheumatol. 2010;37(10):2126–32. doi:10.3899/jrheum.100200.
Heiland GR, Appel H, Poddubnyy D, Zwerina J, Hueber A, Haibel H, et al. High level of functional dickkopf-1 predicts protection from syndesmophyte formation in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71(4):572–4. doi:10.1136/annrheumdis-2011-200216.
Daoussis D, Liossis SN, Solomou EE, Tsanaktsi A, Bounia K, Karampetsou M, et al. Evidence that Dkk-1 is dysfunctional in ankylosing spondylitis. Arthritis Rheum. 2010;62(1):150–8. doi:10.1002/art.27231.
Yucong Z, Lu L, Shengfa L, Yongliang Y, Ruguo S, Yikai L. Serum functional dickkopf-1 levels are inversely correlated with radiographic severity of ankylosing spondylitis. Clin Lab. 2014;60(9):1527–31.
Nocturne G, Pavy S, Boudaoud S, Seror R, Goupille P, Chanson P, et al. Increase in dickkopf-1 serum level in recent spondyloarthritis. Data from the DESIR cohort. PLoS One. 2015;10(8):e0134974. doi:10.1371/journal.pone.0134974.
Croes M, Oner FC, van Neerven D, Sabir E, Kruyt MC, Blokhuis TJ, et al. Proinflammatory T cells and IL-17 stimulate osteoblast differentiation. Bone. 2016;84:262–70. doi:10.1016/j.bone.2016.01.010.
Ono T, Okamoto K, Nakashima T, Nitta T, Hori S, Iwakura Y, et al. IL-17-producing gammadelta T cells enhance bone regeneration. Nat Commun. 2016;7:10928. doi:10.1038/ncomms10928.
•• Cortes A, Maksymowych WP, Wordsworth BP, Inman RD, Danoy P, Rahman P, et al. Association study of genes related to bone formation and resorption and the extent of radiographic change in ankylosing spondylitis. Ann Rheum Dis. 2015;74(7):1387–93. doi:10.1136/annrheumdis-2013-204835. First study to link specific genes to disease progression in SpA.
• Nigil Haroon N, Szabo E, Raboud JM, McDonald-Blumer H, Fung L, Josse RG, et al. Alterations of bone mineral density, bone microarchitecture and strength in patients with ankylosing spondylitis: a cross-sectional study using high-resolution peripheral quantitative computerized tomography and finite element analysis. Arthritis Res Ther. 2015;17:377. doi:10.1186/s13075-015-0873-1. A novel approach to asses structural changes in axial spondyloarthritis.
Acknowledgements
B.N obtained an “aspirant” fellowship from the Fund for Scientific Research Flanders (FWO Vlaanderen). Laboratory studies by the authors on the topic are supported by FWO grant G.0946.14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Barbara Neerinckx declares that she has no conflict of interest.
Rik Lories reports grants and personal fees from Pfizer, personal fees from Abbvie, personal fees from Celgene, personal fees from Jansen, personal fees from UCB, grants from Boehringer-Ingelheim, and personal fees from Novartis during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Spondyloarthritis
Rights and permissions
About this article
Cite this article
Neerinckx, B., Lories, R.J. Structural Disease Progression in Axial Spondyloarthritis: Still a Cause for Concern?. Curr Rheumatol Rep 19, 14 (2017). https://doi.org/10.1007/s11926-017-0639-7
Published:
DOI: https://doi.org/10.1007/s11926-017-0639-7