Abstract
Purpose of Review
This paper aims to acquaint child and adolescent psychiatrists with the field of pharmacogenomics (PGX) and review the most up-to-date evidence-based practices to guide the application of this field in clinical care.
Recent Findings
Despite much research being done in this area, the field of PGX continues to yield controversial findings. In the adult world, studies have focused on the impact of combinatorial gene panels that guide medication selection by providing reports that estimate the impact of multiple pharmacodynamic and pharmacokinetic genes, but to date, these have not been directly examined in younger patient populations. Pharmacokinetic genes, CYP2D6 and CYP2C19, and hypersensitivity genes, HLA-A and HLA-B, have the strongest evidence base for application to pharmacotherapy in children.
Summary
Although the field is evolving, and the evidence is mixed, there may be a role for PGX testing in children to help guide dosing and monitoring strategies. However, evidence-based medicine, rather than PGX testing, continues to play the lead role in guiding medication selection in pediatric psychopharmacology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The advent of the human genome project and its completion at the start of the twenty-first century led to hope throughout the medical field that personalized medicine had arrived. Pharmacogenomics (PGX) arose from that work with the aim of individualizing drug therapy through genetic testing. In fact, in JAMA in 2001, it was predicted that by 2020, PGX testing would emerge as a standard of care [1, 2], improving efficacy and reducing the burden of adverse drug effects.
In certain areas of medicine, perhaps most widely in oncology, the use of genetic information in determining individualized treatment is rapidly advancing and, in many cases, considered standard of care. However, in psychiatry, PGX has not reached the standard of care. Psychiatric illness can be devastating, and our current approaches to pharmacotherapy unfortunately necessitate “wait and see/trial and error” strategies to try medications sequentially with safety and efficacy established through clinical trials. The hope of bypassing the extended time that is often needed to find the right drug makes the promise of PGX guidance extremely alluring. In child and adolescent psychiatry, that hope is even stronger as parents have many concerns about their child experiencing side effects or failing to respond to medications, if they are comfortable with medications at all.
The goal of PGX is to improve our drug selection and dosing strategies so that we may reduce adverse treatment effects, improve efficacy, and reduce time from drug implementation to response. These are factors that are critical in any area of medicine but of dire importance in both adults and children whose psychiatric illnesses carry such a burden of morbidity. For this reason, it is not surprising there has been such a rapid development of commercial products targeting the use of PGX guidance in psychotropic drug selection, which provide decision support algorithms to both providers and in some cases, directly to consumers. While there is emerging evidence, especially within the past year, to demonstrate that PGX may provide an important role in drug selection and dosing in specific medication-gene pairs, it is clear that it is not the standard of care in child and adolescent psychiatry. In fact, during this past year, new steps have been taken by regulatory agencies and professional organizations to publish position papers that warn practitioners of overreliance on PGX guidance. While many commentaries [3] and reviews [4] have stated that PGX is not ready for widespread use in our field, there are others [5] still that find the emerging evidence to be promising.
Pharmacokinetic and Pharmacodynamic Genes
Virtually, every step involved with drug metabolism, transport, and action is susceptible to genetic variation [6]. The genes that code for enzymes that metabolize medications are known as pharmacokinetic (PK) genes whereas those that code for the proteins that are targets of medication activity are known as pharmacodynamic (PD) genes. Due to the high genetic variability of these genetic markers in the general population, polymorphisms in the genes encoding these targets (often referred to as pharmacogenes) denote a potential vulnerability in drug impact but do not indicate an absolute outcome. In addition, when prescribing for children and adolescents, it is important to consider the developmental changes that occur in the system that may impact metabolism.
Given that a high percentage of psychotropic medications are metabolized by the cytochrome P450 (CYP) enzyme system within the liver, the genes that code for those enzymes have become the most relevant to psychiatry. Variations in alleles within these genes can result in stratification of functional significance. The current nomenclature for the resulting phenotype is defined as follows: Normal (previously referred to as extensive) metabolizers have two functional or active alleles, intermediate metabolizers have one functioning allele, ultrarapid metabolizers have three or more active alleles, and poor metabolizers have two nonfunctional or partially functional alleles [7, 8].
Most important to psychiatry and most well studied are CYP genes, 2D6 and 2C19. CYP2D6 is involved in the metabolism of several psychiatric medications including fluoxetine, paroxetine, venlafaxine, and atomoxetine. While CYP2C19 primarily metabolizes fewer medications, such as citalopram and escitalopram, it also secondarily contributes to the metabolism of some medications, namely, sertraline. CYP2D6 allelic frequencies vary widely across major ethnic groups, which is important in interpreting gene testing of these enzymes [9]. Likewise, for CYP2C19, while among Caucasian populations, metabolizer status is stratified in a normal distribution, in East Asian populations, the distribution is skewed with greater percentages of poor and intermediate metabolizers [8]. Refer to Table 1 for a summary of the CYP metabolism of antidepressants and other selected psychotropic drugs commonly used in children.
It is important to note that drug interactions and drug inhibition or induction of the CYP system can also impact the metabolic function of these enzymes (Table 1). For instance, if a patient who is an intermediate metabolizer for 2D6 is treated with aripiprazole (a 2D6 substrate) and is then placed on fluoxetine (a 2D6 inhibitor), that enzyme may convert to having poor metabolizer activity rendering that patient at increased risk for side effects or lack of efficacy. This means that PGX analysis must take into account what other medications a patient might be on in addition to the genetic findings [10].
The PD genes in many combinatorial panels have included various receptors, transporters, and enzymes; although, only the most well studied will be highlighted here. An area of much interest and research has involved the serotonin transporter (SERT or 5-HTT), which is a transmembrane protein responsible for the reuptake of serotonin from the synapse. SLC6A4 is the gene that encodes 5-HTT, and its altered expression can lead to reduced serotonin reuptake. One particular polymorphism involving the promoter region leads to either a long (l/l) or short variant (s/s). The s/s variant can result in decreased expression of the transporter, resulting in possibly decreased likelihood to achieve remission, while greater response has been reported in patients with l/l version when treated with selective serotonin reuptake inhibitors (SSRIs) [11,12,13]. Importantly, this effect was observed among Caucasians, but not among those of Asian ancestry. In children, a more recent study[14•] found no relation between genotype predicted levels of SLC6A4 expression and response time; interestingly, those with predicted low levels of SLC6A4 expression were treated longer suggesting a better tolerability. While some data is supportive of the relevance of SLC6A4 gene variability in antidepressant effectiveness, the evidence is not conclusive as to what the implications are for clinical practice.
Among receptors, HTR2A (serotonin receptor 2A) has also received significant attention. Many polymorphisms in HTR2A have been identified which may influence the clinical response to antidepressants. In adults, greater treatment responses have been observed in antidepressant treated-patients with certain polymorphisms (rs6313 and the closely linked rs6311), while others may also be associated with increased side effects [15]. In children, the polymorphism rs6313 was associated with response dose, in that patients with more G alleles at this site were prescribed lower doses of sertraline in order to achieve a response as measured by the Clinical Global Impressions Scale (CGI)[14•].
One of the enzymes that inactivates circulating catecholamines (norepinephrine, dopamine) is catecholamine-O-methyltransferase (COMT). A known polymorphism replacing amino acid valine for methionine causes decreased COMT activity and subsequent higher dopamine levels, which could in turn potentially lead to a decreased effectiveness of methylphenidate [16, 17]. In children, the data is limited to international studies [18, 19].
Another potentially relevant enzyme, and sometimes considered a PK gene, is the ABCB1 gene which encodes P-glycoprotein, a drug transporter at the blood brain barrier. Polymorphisms in this gene can lead to high P-glycoprotein expression, which is hypothesized to alter the concentration of substrate antidepressants, thereby possibly contributing to individual differences in response to antidepressants such as citalopram, escitalopram, fluoxetine, paroxetine, venlafaxine, amitriptyline, and more (data limited to adults) [20].
Among the PD genes, the only one that has reached the level of being actionable in both adults and children is the human leukocyte antigen (HLA) gene that encodes a cell surface protein involved in antigen presentation to immune cells and for which genetic variation seems to be implicated in specific cutaneous reactions to certain anticonvulsants. Though often referred to as a PD gene, HLA is actually a marker of hypersensitivity, rather than a gene with any drug targeted action. The HLA-B*1502 allele is associated with increased risk of Stevens-Johnson syndrome and toxic epidermal necrolysis in adult patients treated with carbamazepine [21]. In children, more specific genetic markers within this protein family, HLA-A 31:01 and HLA-B 15:02, have been identified as a genetic marker that carries increased risk for hypersensitivity to carbamazepine in children [22•].
A Primer on the Molecular Analysis of Pharmacogenetic Polymorphisms
In the field of PGX, buccal swabs have become the most common means of gathering DNA from patients. A buccal swab sample is collected with foam-tipped polystyrene plastic rods, and the DNA is then extracted from the collected epithelial tissue.
The most common methodology for determination of the status of the relevant alleles involves amplification of segments of the genes by PCR and genotyping binary single nucleotide polymorphisms in each gene. For genotyping, two specific probes in solution for each allele are hybridized to the amplified DNA, or the amplified DNA is applied to microchips containing each probe immobilized to a predetermined location in a grid. Fluorescent tags are linked to each probe for reporting hybridization results. Binding of only one of the alternate probes classifies the locus as homozygous for one allele or the other. Binding of both classifies the locus as heterozygous.
The CYP2D6 and SLC6A4 genes are especially technically demanding for molecular characterization of multiple polymorphisms and determination of the functional phenotype. CYP2D6 is hypervariable and hypermutable with duplications, rearrangements, deletions, and highly diverse combinations of SNPs into haplotypes [23, 24]. SLC6A4 consists of a variable number of tandem repeats with a nested SNP in the repeated region [25]. In both cases, incorrect phenotypes could result if the combinations of multiple alleles are undetected or misconfigured. A recent study showed that different labs might assay different genotypes (and therefore different phenotypes) [26]. Given the complexity of genotyping the SLC6A4 gene, the lack of consistent research findings related to the serotonin transporter may be partially explained by these potential laboratory inconsistencies.
A Review of the Evidence
There are primarily three study designs that have been used to investigate the field of PGX: Genome-wide association studies (GWAS), combinatorial gene guidance and its impact on treatment outcome (PK and PD genes together), and specific gene to medication associations and treatment outcome. GWAS and combinatorial gene guidance and treatment outcome studies have only been completed in adults. In children, the most recent studies have focused on the latter study design of associating specific gene findings to treatment outcome when paired to a specific drug. Table 2 provides a summary of relevant studies highlighted in this section.
In general, the GWAS have not yielded much evidence for determining which genes might play an important role for determining medication tolerance and response. A meta-analysis was conducted in 2013 of three key large GWAS that combined a total of 2256 adult subjects with major depressive disorder (MDD) treated by antidepressants. These subjects were taken from the genome-based therapeutic drugs for depression (GENDEP) study, Munich antidepressant response signature (MARS), and sequenced treatment alternatives to relieve depression (STAR*D). Consistent with other studies, they found no genetic predictors for antidepressant treatment outcome [27]. However, a more narrow analysis among 1354 GENDEP and STAR*D subjects on citalopram or escitalopram identified a single-nucleotide polymorphism or SNP(rs12054895) in an intergenic region of chromosome 5 that was associated at genome-wide level of significance with greater improvement after 2 weeks [27].This finding provided some preliminary evidence that there might be subpopulations of patients for whom such testing could expedite treatment response, especially with regard to individual drug selection.
The research that has focused on combinatorial PGX results to guide treatment has been primarily industry-sponsored and utilizes the application of proprietary algorithms for combining the relative contribution of multiple genes and the resulting guidance on drug selection. Although these studies have yielded some evidence for the efficacy of applying gene panels to medication selection in order to enhance depression treatment [28•], reviewers have criticized these publications for lack of transparency regarding the algorithms used by companies to derive treatment recommendations and have warned of potential risks of interpreting results without appropriate clinical context or using them to replace established clinical practices [29]. There have also been limitations identified that these studies are of too short duration, are often unblinded, contain small sample sizes, and have only identified small magnitudes of statistically significant differences between study arms. However, it must be noted that the sample sizes and treatment duration of these studies are similar to those used in most clinical trials for the evaluation of drug efficacy. In most reviews of this research, the conclusions suggest that the current evidence does not support routine testing despite some possible relevant findings of enhanced treatment outcome in the cohort of patients for which PGX guidance is used [4].
However, some very recent studies in this area have addressed a few of these concerns with larger sample sizes and improved study designs that use randomized blinded trials comparing PGX-guided treatment and treatment as usual. In 2017, Perez completed a blinded study of 316 adult patients with MDD across 18 treatment centers in Spain, who were randomized to PGX-guided treatment or treatment as usual. Primary outcome was identified as sustained response (Patient Global Impression of Improvement (PGI-I) score ≤ 2 on consecutive occasions and at 12 weeks) and was not found to be significantly different between treatment arms. However, the study ultimately demonstrated significantly greater response rates (PGI-I score ≤ 2) at 12 weeks in the guided group, and secondary analyses showed that response in the guided group was more marked in patients who had a greater number of previous failed medication trials [30•]. Notably, subjects in this study did have comorbidities including anxiety and substance use, and a large population (up to 65%) had failed previous medication trials. Recently, the GUIDED (Genomics Used to Improve DEpression Decisions) trial[31•] compared the use of a PGX panel (including PK and PD genes) in drug selection to treatment as usual in 1167 adult subjects with MDD who had failed at least one medication trial, thus selecting a more narrow difficult to treat and perhaps treatment-resistant patient population. Response rate was measured by changes in Hamilton Depression Rating Scale (HAM-D) scores at week 8 of treatment with subjects and raters being blinded to treatment arm. While there was no statistically significant difference between treatment arms of the primary outcome, in secondary analyses, the PGX-guided arm, there was significant difference in treatment response (HAM-D improvement greater than or equal to 50%) and remission (HAM-D less than 7). Additionally, patients who had transitioned after 8 weeks from medication that was not in line with genomic-guided medication to that which was had significant improvement in symptoms per HAM-D ratings. This study was primarily limited by the lack of blinding of treating psychiatrists due to ethical concerns (as in the Perez study above), and similarly patients and raters were blinded. Furthermore, the study population was primarily Caucasian, an important factor when considering generalizability. Nonetheless, the study results have been cited to suggest that PGX testing in psychiatry may be warranted in adults who, whether due to lack of efficacy or tolerability from large side effect burden, have failed prior medication trials. This was furthermore supported by two recent meta-analyses (including the studies highlighted here) that examined the available published data [28•, 32•] and separately identified that PGX guided treatment increased the likelihood for remission as compared to treatment as usual.
Within the pediatric world, the studies have primarily focused on specific gene findings and their association with either side effects or treatment outcome. Although these studies have explored both PK and PD genes (including CYP enzymes, 5-HTT, HTR2A, COMT, and HLA) and were mentioned in the section above, most recently, the focus has been on CYP2C19 and CYP2D6, genes which are highly relevant to the metabolism of many psychotropic medications. In fact, drug labeling for two very relevant pediatric medications, atomoxetine (metabolized by CYP2D6) and citalopram (metabolized predominantly by CYP2C19), include warnings for patients with CYP2D6 and CYP2C19 vulnerabilities. As far back as 2007, a retrospective review of subjects (N = 894) aged 6 to 18 years old with ADHD on atomoxetine showed that poor metabolizer status in CYP2D6 was associated with greater reduction in mean symptom severity scores and more frequently reported adverse events (including decreased appetite, tremor, and increases in heart rate or diastolic blood pressure) relative to normal metabolizers [33]. A recent study of single-dose atomoxetine among children and adolescents diagnosed with ADHD demonstrated 30-fold differences in dose-corrected plasma concentrations of active drug in extensive CYP2D6 metabolizers relative to poor metabolizers [34]. This suggested that among children and adolescents, there may be a need for more individualized dosing strategies for atomoxetine based on metabolizer status of CYP2D6. Most excitingly, in the past year, with the demonstrated approach that the highest yield for using PGX might lie in a specific gene to drug analysis, there have been new studies in children exploring the relationship between individual gene polymorphisms and specific drug response.
Two recent studies utilizing a database of children who had undergone routine PGX testing at the time of admission to the inpatient psychiatric unit at Cincinnati Children’s Hospital have demonstrated significant associations between CYP enzyme gene variability and drug response, including tolerability and efficacy. Aldrich [35•] analyzed the treatment of 263 subjects under age 19 with anxiety and depression who were treated with citalopram or escitalopram from their inpatient cohort and found that patients with a slower CYP2C19 metabolizer status had decreased drug tolerability, higher discontinuation rates, and increased likelihood of additional psychiatric inpatient days relative to their more rapid metabolizer counterparts. While the metabolizer phenotype did not influence the overall proportion of responders, the faster metabolizers responded more quickly to either drug. A similar retrospective study performed by the same group analyzed routine genetic testing of 369 subjects under age 19 hospitalized with anxiety and depression and treated with sertraline [14•]. Subjects were stratified based on number of reduced functioning alleles in CYP2C19. Patients with slower CYP2C19 metabolism, defined as having two reduced functioning alleles (RFA), were ultimately prescribed lower maximum doses of sertraline. This suggested that a less steep titration was necessary in slower metabolizers. However, no association was found between number of RFAs and either dose at the time of response or number of side effects.
The results of these studies are preliminary. However, the trends and associations demonstrated by the large datasets described here suggest that CYP2D6 and CYP2C19 may play an important role in medication tolerance and contribute to dose-based efficacy in children. Additional prospective controlled studies in children and adolescents will be required to draw more complete conclusions about the relationship between PGX testing of individual genes and drug response in this patient population.
Pharmacogenomics in Product Labeling, Consensus Guidelines, and Professional Organization Position Statements
Examining and understanding the evidence base for PGX is essential for appropriate application to patient care. As of 2019, over 250 drugs contain mention of a PGX biomarker in the product labeling [https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling]. Of these, 57 have indications for psychiatric or neurologic conditions, 21of which have indications for use in patients under 18 years of age, and the level of evidence regarding those biomarkers is summarized including whether that association is “actionable” or “informative” (see Table 3). These genetic biomarkers mentioned are predominantly those related to drug metabolism or hypersensitivity reactions. To date, there are no pharmacodynamic genes mentioned in the product labeling for psychiatric or neurologic conditions.
The presence or absence of PGX information in product labeling is dependent on the extent to which these data were evaluated in the drug development process, submitted as part of New Drug Application materials, or commissioned as part of post-approval studies. Beyond drug development studies, extensive research on the mechanistic, pharmacokinetic, and clinical implications of genetic variability in pharmacogenes has been completed for many psychiatric or neurologic medications [36]. The vastness of these data along with different study designs (e.g., single dose, multiple dose, healthy participants, patients, etc.) underscores the need for an organized approach to the evaluation of the evidence base for clinically relevant PGX relationships. The Clinical Pharmacogenetics Implementation Consortium (CPIC) was established in 2009 as an NIH-supported effort to provide freely available, evidence-based, peer-reviewed, and rigorously conducted clinical guideline reviews and recommendations [37].
CPIC guidelines provide recommendations and strength of evidence for clinical actions that may be made based on existing PGX information. CPIC by design does not address the question of whether to order a test, as this may be influenced by nonbiological factors (e.g., economics). The premise for this approach is that as cost of genetic testing continues to decrease, more people will possess PGX information, necessitating that providers understand what to do with that information, as opposed to whether or not to obtain it. As of 2019, CPIC has published 23 guidelines [37]. Guidelines related to psychiatric or neurologic agents used in children have been published for tricyclic antidepressants (TCAs) [38], SSRIs [39], carbamazepine and oxcarbazepine [40], phenytoin [41], and atomoxetine [42]. Of these, data supporting the current version of the guidelines included younger patients, albeit significantly fewer for SSRIs as compared to the other drugs, at the time of publication. Internationally, the Dutch Pharmacogenetics Working Group (DPWG) also conducts guideline reviews for the clinical relevance of drug-gene pairs [43]. DPWG and CPIC guidelines are similar, but with some nuanced differences due to the guideline development process of each [44]. DPWG updates are maintained on their website https://upgx.eu/guidelines/, and CPIC guidelines are published and made available through guidelines.gov as well as PubMed/PubMed Central.
In the fall of 2018, the FDA issued warnings about some PGX tests marketed towards mental health indications with a goal of eliminating what were viewed as unsubstantiated claims for efficacy. Task force or position statements about the use of PGX, particularly focusing on tests that offer combinatorial results, have been put forth by the American Psychiatric Association [4] as well as the American Academy of Child and Adolescent Psychiatry (pending release, personal communication), both stating that existing evidence does not support widespread use of testing at the current time. Additionally, the International Society for Psychiatric Genetics (ISPG) has recently published an update of their position statement on genetic and pharmacogenetic testing [45]. All three of these organizations adequately highlight that one knowledge gap is not knowing which patients may benefit from testing and when in the course of treatment tests might be helpful. All three note that drug metabolizing enzyme genetics, such as those included in product labeling or guidelines, may be helpful if known. Additionally, hypersensitivity genes may be useful for some patient populations considered for treatment with carbamazepine or oxcarbazepine. Thus, while there is agreement that knowing certain pieces of PGX information may be helpful, consensus on the method and the circumstances under which it should be obtained is lacking.
Conclusion: the Clinician’s Dilemma
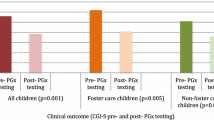
Given the controversy that has surrounded the field of PGX, psychiatric providers are often faced with the dilemma of how to best understand the role of PGX testing in clinical care. The industry has promoted the notion that gene results are best interpreted in aggregate as a combinatorial panel that often yields a chart of medications with colored designations indicating which medications have low risk versus high risk. Often, these findings are interpreted to mean that certain medications will work for your patient and certain medications should be avoided. The risk in this approach is that providers may be influenced to prescribe “use as directed” medications in hopes that that will avoid any untoward reaction and increase the likelihood of a positive response to the medications prescribed, causing the practitioner to deviate from best evidence practices. For instance, in many of the commercially available panels, if the PD gene that encodes the serotonin transporter is heterozygous s/l or homozygous s/s, the entire class of SSRIs will be in the “use with caution” zone even if the PK genes that code for the enzymes that metabolize these medications are fully intact and without vulnerable polymorphisms. A practitioner who is treating an adolescent for anxiety or depression, and who may not be aware of the literature or does not know that the PK genes have more actionable evidence than the PD genes, might be influenced by the listing of all SSRIs within a warning zone. They may thus consider using an SNRI instead, which would be a deviation from the current consensus guidelines that SSRIs remain first-line medications for the treatment of pediatric anxiety and depression. In a study we completed in 2018, we showed that physicians were highly influenced by the combinatorial analysis of PK genes and tended to avoid prescribing “yellow” or “red” medications, leading to a marked increase in desvenlafaxine use, which to date has not been established as an evidence-based medication for depression in children and adolescents [46, 47].
Psychiatric providers have been drawn to the field of PGX because it promised an alternative to the “trial and error approach.” As physicians, we have taken an oath to “above all do no harm.” We are also trained to only order tests we can interpret and to not order tests that are unnecessary or not indicated. Yet with certain patients whose history of medication reactions seem unusual or extreme, or where the testing is already available, how might psychiatrists integrate evidence-based medicine with PGX testing? It is essential that we understand the science behind any test we are interpreting. When considering pharmacotherapy, we should start with a thorough evaluation of the symptoms and develop a clear diagnostic formulation. Using that clinical data, we then determine if pharmacotherapy is indicated. If so, providers should select the medication based on the best evidence practices for the condition we are targeting in treatment. If PGX testing results are available, the psychiatric provider should review the gene results that are relevant to the medication that is being prescribed. As an example, the current data would support utilizing the results of the CYP2D6 gene for atomoxetine, or CYP2C19 for sertraline, citalopram, or escitalopram. If we are considering carbamazepine or oxcarbazepine, the results of the HLA genes can guide us regarding risk of hypersensitivity reactions. We can use CPIC guidelines to consider the dosing options if any of the gene findings are relevant or select a different medication of the same class if the gene findings suggest complexities that might confer vulnerability (Fig. 1). Throughout this process, it will be important to be sure to educate families about how we apply these results and understand their limitations. The key point is that PGX testing provides information about potential vulnerabilities and does not predict outcome.
PGX testing should not replace clinical assessments, consensus algorithms, or evidence-based medicine. However, if PGX data is available, there are many resources that can help a practitioner become more comfortable with the individual gene results and their applicability and whether these results are “actionable” or simply informative. Although that can feel daunting to a psychiatric provider who is burdened with many other tasks, given that this technology is available, and in certain states can be obtained directly by the consumer, it will benefit our patients to stay as current as possible and to be aware of both the potential applications and the current limitations of this ever-expanding field.
Abbreviations
- 5-HTT:
-
Serotonin Transporter
- CGI:
-
Clinical Global Impressions Scale
- COMT:
-
Catecholamine-O-methyltransferase
- CPIC:
-
Clinical Pharmacogenetics Implementation Consortium
- CYP:
-
Cytochrome P450
- DPWG:
-
Dutch Pharmacogenetics Working Group
- GENDEP:
-
Genome-Based Therapeutic Drugs for Depression
- GWAS:
-
Genome Wide Association Study
- HAM-D:
-
Hamilton Depression Rating Scale
- HLA:
-
Human Leukocyte Antigen
- HTR2A:
-
Serotonin receptor 2A
- ISPG:
-
International Society for Psychiatric Genetics
- MARS:
-
Munich Antidepressant Response Signature
- PD:
-
Pharmacodynamic(s)
- PGI-I:
-
Patient Global Impression of Improvement Scale
- PGX:
-
Pharmacogenomic(s)
- PK:
-
Pharmacokinetic(s)
- SERT:
-
Another name for the Serotonin Transporter
- SNP:
-
Single Nucleotide Polymorphism
- STAR*D:
-
Sequenced Treatment Alternatives to Relieve Depression
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Collins FS, McKusick VA. Implications of the human genome project for medical science. J Am Med Assoc. 2001. https://doi.org/10.1001/jama.285.5.540.
Phillips KA, Veenstra DL, Oren E, Lee JK, Sadee W. Potential role of pharmacogenomics a systematic review. JAMA J Am Med Assoc. 2001;286:2270–9.
Nemeroff C (2019) Pharmacogenomic tests in psychiatry: not ready for prime time. Psychiatr News 54:appi.Pn.2019.5b12.
Zeier Z, Carpenter LL, Kalin NH, Rodriguez CI, McDonald WM, Widge AS, et al. Clinical implementation of pharmacogenetic decision support tools for antidepressant drug prescribing. Am J Psychiatry. 2018;175:873–86.
Singh AB, Bousman CA. Antidepressant pharmacogenetics. Am J Psychiatry. 2017;174:417–8.
Tansey KE, Guipponi M, Hu X, Domenici E, Lewis G, Malafosse A, et al. Contribution of common genetic variants to antidepressant response. Biol Psychiatry. 2013;73:679–82.
Caudle KE, Sangkuhl K, Whirl-Carrillo M, et al. Standardizing CYP2D6 genotype to phenotype translation: consensus recommendations from the clinical pharmacogenetics implementation consortium and Dutch pharmacogenetics working group. Clin Transl Sci. 2020;13:116–24.
Caudle KE, Dunnenberger HM, Freimuth RR, et al. Standardizing terms for clinical pharmacogenetic test results: consensus terms from the Clinical Pharmacogenetics Implementation Consortium (CPIC). Genet Med. 2017;19:215–23.
Gaedigk A, Sangkuhl K, Whirl-Carrillo M, Klein T, Steven Leeder J. Prediction of CYP2D6 phenotype from genotype across world populations. Genet Med. 2017;19:69–76.
Ramsey LB, Brown JT, Vear SI, Bishop JR, Van Driest SL. Gene-based dose optimization in children. Annu Rev Pharmacol Toxicol. 2019;60:1–21.
Porcelli S, Fabbri C, Serretti A. Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with antidepressant efficacy. Eur Neuropsychopharmacol. 2012;22:239–58.
Huezo-Diaz P, Uher R, Smith R, et al. Moderation of antidepressant response by the serotonin transporter gene. Br J Psychiatry. 2009. https://doi.org/10.1192/bjp.bp.108.062521.
Kronenberg S, Apter A, Brent D, Schirman S, Melhem N, Pick N, et al. Serotonin transporter polymorphism (5-HTTLPR) and citalopram effectiveness and side effects in children with depression and/or anxiety disorders. J Child Adolesc Psychopharmacol. 2007. https://doi.org/10.1089/cap.2006.0144.
• Poweleit EA, Aldrich SL, Martin LJ, Hahn D, Strawn JR, Ramsey LB. Pharmacogenetics of sertraline tolerability and response in pediatric anxiety and depressive disorders. J Child Adolesc Psychopharmacol. 2019;29:348–61 A retrospective analysis of pediatric patients treated with sertraline that found association between CYP2C19, HTR2A, and SLC6A4 gene variability and sertraline tolerability and efficacy.
Kirchheiner J, Nickchen K, Bauer M, Wong ML, Licinio J, Roots I, et al. Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry. 2004;9:442–73.
Mattay VS, Goldberg TE, Fera F, Hariri AR, Tessitore A, Egan MF, et al. Catechol O-methyltransferase val158-met genotype and individual variation in the brain response to amphetamine. Proc Natl Acad Sci U S A. 2003;100:6186–91.
Shield AJ, Thomae BA, Eckloff BW, Wieben ED, Weinshilboum RM. Human catechol O-methyltransferase genetic variation: gene resequencing and functional characterization of variant allozymes. Mol Psychiatry. 2004;9:151–60.
Cheon KA, Jun JY, Cho DY. Association of the catechol-O-methyltransferase polymorphism with methylphenidate response in a classroom setting in children with attention-deficit hyperactivity disorder. Int Clin Psychopharmacol. 2008;23:291–8.
Kereszturi E, Tarnok Z, Bognar E, Lakatos K, Farkas L, Gadoros J, et al. Catechol-O-methyltransferase Val158Met polymorphism is associated with methylphenidate response in ADHD children. Am J Med Genet Part B Neuropsychiatr Genet. 2008;147:1431–5.
Brückl TM, Uhr M. ABCB1 genotyping in the treatment of depression. Pharmacogenomics. 2016. https://doi.org/10.2217/pgs.16.18.
Ferrell PB, McLeod HL. Carbamazepine, HLA-B*1502 and risk of Stevens-Johnson syndrome and toxic epidermal necrolysis: US FDA recommendations. Pharmacogenomics. 2008. https://doi.org/10.2217/14622416.9.10.1543.
• Amstutz U, Ross CJD, Castro-Pastrana LI, Rieder MJ, Shear NH, Hayden MR, et al. HLA-A*31:01 and HLA-B*15:02 as genetic markers for carbamazepine hypersensitivity in children. Clin Pharmacol Ther. 2013. https://doi.org/10.1038/clpt.2013.55This is the first study to demonstrate assoication of HLA-A*31:01 polymorphism with carbamazepine hypersensitivity including Stevens-Johsnon syndrome and drug-incudced hypersensititivity syndrome in children.
Gaedigk A. Complexities of CYP2D6 gene analysis and interpretation. Int Rev Psychiatry. 2013;25:534–53.
Ruaño G, Kocherla M, Graydon JS, Holford TR, Makowski GS, Goethe JW. Practical interpretation of CYP2D6 haplotypes: comparison and integration of automated and expert calling. Clin Chim Acta. 2016;456:7–14.
Odgerel Z, Talati A, Hamilton SP, Levinson DF, Weissman MM. Genotyping serotonin transporter polymorphisms 5-HTTLPR and rs25531 in European- and African-American subjects from the National Institute of Mental Health’s collaborative Center for Genomic Studies. Transl Psychiatry. 2013;3:e307–6.
Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. Pharmacogenomics J. 2018;18:613–22.
Uher R, Tansey KE, Rietschel M, et al. Common genetic variation and antidepressant efficacy in major depressive disorder: a meta-analysis of three genome-wide pharmacogenetic studies. Am J Psychiatry. 2013;170:207–17.
• Bousman CA, Arandjelovic K, Mancuso SG, Eyre HA, Dunlop BW. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20:37–47 A meta-analysis of prospective, randomized controlled trials that examined use of combinatorial gene test results in tratment of MDD which found that use of PGX guided decision support tools is associated with greater likelihood of symptom remission than treatment as usual.
Zubenko GS, Sommer BR, Cohen BM. On the marketing and use of pharmacogenetic tests for psychiatric treatment. JAMA Psychiatry. 2018;75:769–70.
• Pérez V, Salavert A, Espadaler J, et al. Efficacy of prospective pharmacogenetic testing in the treatment of major depressive disorder: results of a randomized, double-blind clinical trial. BMC Psychiatry. 2017;17:1–13 Double-blinded, randomized controlled trial of adults with MDD found that although there was no difference in sustained drug response, those in the PGX guided group had a greater responder rate especially if they had failed more than one drug trial.
• Greden JF, Parikh SV, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111:59–67 A blinded, randomized controlled trial of adults with MDD who had failed at least one medication trial with an antidepressant which found through secondary analyses that response and remission were greater in the PGX-guided groups.
• Rosenblat JD, Lee Y, Mcintyre RS. The effect of pharmacogenomic testing on response and remission rates in the acute treatment of major depressive disorder: a meta-analysis. J Affect Disord. 2018. https://doi.org/10.1016/j.jad.2018.08.056A meta-analysis of two randomized controlled trials and two open label cohort studies comparing use of PGX guided and unguided treatment that found combined response and remission likelihood in these four studies to significantly support PGX guided treatment.
Michelson D, Read HA, Ruff DD, Witcher J, Zhang S, McCracken J. CYP2D6 and clinical response to atomoxetine in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2007;46:242–51.
Brown JT, Abdel-Rahman SM, Van Haandel L, Gaedigk A, Lin YS, Leeder JS, et al. Single dose, CYP2D6 genotype-stratified pharmacokinetic study of Atomoxetine in children with ADHD. Clin Pharmacol Ther. 2016;99:642–50.
• Aldrich SL, Poweleit EA, Prows CA, Martin LJ, Strawn JR, Ramsey LB. Influence of CYP2C19 metabolizer status on escitalopram/citalopram tolerability and response in youth with anxiety and depressive disorders. Front Pharmacol. 2019;10:1–12 A retrospective analysis in pediatric patients on escitalopram or citalopram who had undergone routine PGX testing which found that slower CYP2C19 metabolizers had more side effects and were more likely to discontinue treatment and faster metabolizers responded more likely.
Bishop JR. Pharmacogenetics. Handb Clin Neurol. 2018;147:59–73.
Relling MV, Klein TE, Gammal RS, Whirl-Carrillo M, Hoffman JM, Caudle KE. The clinical Pharmacogenetics implementation consortium: 10 years later. Clin Pharmacol Ther. 2019. https://doi.org/10.1002/cpt.1651.
Hicks JK, Sangkuhl K, Swen JJ, et al (2016) Clinical Pharmacogenetics Implementation Consortium guideline (CPIC®) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update.
Hicks JK, Bishop JR, Sangkuhl K, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98:127–34.
Phillips EJ, Sukasem C, Whirl-Carrillo M, et al Clinical Pharmacogenetics Implementation Consortium Guideline for HLA Genotype and Use of Carbamazepine and Oxcarbazepine: 2017 Update. https://doi.org/10.1002/cpt.1004.
Caudle K, Rettie A, Whirl-Carrillo M, Smith L, Mintzer S, Lee M, Klein T, Callaghan J (2014) Clinical Pharmacogenetics Implementation Consortium Guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. https://doi.org/10.1038/clpt.2014.159.
Brown JT, Bishop JR, Sangkuhl K, et al (2019) Clinical Pharmacogenetics Implementation Consortium Guideline for cytochrome P450 (CYP)2D6 genotype and atomoxetine Therapy 1.
Swen J, Wilting I, de Goede A, et al. Pharmacogenetics: from bench to byte. Clin Pharmacol Ther. 2008;83:781–7.
Bank PCD, Caudle KE, Swen JJ, Gammal RS, Whirl-Carrillo M, Klein TE, Relling MV, Guchelaar H-J A comparison of the guidelines of the Clinical Pharmacogenetics Implementation Consortium and the Dutch Pharmacogenetics Working Group https://doi.org/10.1002/cpt.762.
Genetic Testing Statement | ISPG - International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Accessed 19 Nov 2019.
Atkinson S, Lubaczewski S, Ramaker S, England RD, Wajsbrot DB, Abbas R, et al. Desvenlafaxine versus placebo in the treatment of children and adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2018;28:55–65.
Namerow LB, Walker SA, Stevens M, Kesten K, Graydon JS, Ruano G. 2.24 utilization of Cyp450 genotyping in the treatment of adolescent mood disorders: a look at the impact within an outpatient setting. J Am Acad Child Adolesc Psychiatry. 2018;57:S166.
Funding
Gualberto Ruaño reports support from Genomas Inc., outside the submitted work. In addition, Dr. Ruano has Patent No. US 9,558,320 B2 Physiogenomic Method for Predicting Drug Metabolism Reserve for Antidepressants and Stimulants issued.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sophia A. Walker, Mirela Loftus, and Salma Malik each declare no potential conflicts of interest.
Lisa B. Namerow received a grant from Hartford Hospital to support a research coordinator for her research project conducted and cited in this paper.
Jeffrey R. Bishop is a member of the Clinical Pharmacogenetics Implementation Consortium and is a consultant to OptumRx.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Child and Adolescent Disorders
Rights and permissions
About this article
Cite this article
Namerow, L.B., Walker, S.A., Loftus, M. et al. Pharmacogenomics: an Update for Child and Adolescent Psychiatry. Curr Psychiatry Rep 22, 26 (2020). https://doi.org/10.1007/s11920-020-01145-4
Published:
DOI: https://doi.org/10.1007/s11920-020-01145-4