Abstract
This paper reviews recent research on the use of electroconvulsive therapy (ECT) in elderly depressed patients. The PubMed database was searched for literature published within the past 4 years, using the search terms: “electroconvulsive elderly,” “electroconvulsive geriatric,” “ECT and elderly,” and “ECT elderly cognition.” The studies in this review indicate excellent efficacy for ECT in geriatric patients. Adverse cognitive effects of ECT in this population are usually transient and not typically severe. In addition, continuation/maintenance ECT (C/M-ECT) may be a favorable strategy for relapse prevention in the elderly after a successful acute course of ECT. ECT is an important treatment option for depressed geriatric patients with severe and/or treatment-resistant illness. New data add to the evidence demonstrating that ECT is a highly effective, safe, and well-tolerated antidepressant treatment option for geriatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electroconvulsive therapy (ECT) remains psychiatry’s “gold standard” treatment for severe mental illness, including mood disorders and psychosis [1]. It can be used in a variety of patient populations and has a particularly salient role in the treatment of geriatric patients with depression. The use of ECT should be considered in old-age patients who are treatment resistant to pharmacotherapy, unable to tolerate antidepressant medications, or urgently ill [2]. ECT is safe, even in frail elderly patients with multiple medical comorbidities, including cardiac, pulmonary, and neurological disease [3]. Moreover, ECT may be lifesaving in urgently ill geriatric patients with suicidal ideation or emergent medical conditions like catatonia [4].
Despite its proven efficacy and safety, shortcomings of ECT include its adverse effect profile (mainly temporary cognitive impairment), and the fact that benefits are limited to the current episode of illness (unless continuation/maintenance ECT (C/M-ECT)) is used [5].
New findings provide additional evidence that ECT is efficacious, safe, and tolerable in old-age patients. This review summarizes the available evidence for the safety and efficacy of ECT in geriatric depression.
Method
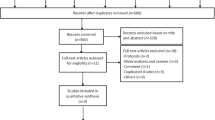
The PubMed database was searched using the following search terms for relevant articles published within the past 4 years: “electroconvulsive elderly,” “electroconvulsive geriatric,” “ECT and elderly,” and “ECT elderly cognition.” Citations with content not relevant to the current review and those over 4 years old were excluded.
Results
Efficacy and Speed of Response
Several recent studies offer insight into the efficacy of ECT as an antidepressant in elderly patients. Rhebergen et al. [6•] sought to define course trajectories of clinical response to ECT in a multicenter collaborative study that included two randomized control trials (RCT). A cohort of 120 patients with major depressive disorder (MDD) received twice weekly ECT. Depressive symptoms were assessed by weekly ratings, with the Hamilton Rating Scale for Depression, 17-item (HRSD-17), for 6 weeks following the initial treatment. Using a latent class growth analysis, Rhebergen and colleagues identified three subtypes of ECT course trajectory (rapid remission, moderate response, nonremitting) based on the HRSD-17 follow-up. They found that older age was associated with rapid remission. Mean age was significantly higher in the rapid remission group (mean = 65.3, sd = 13.4, n = 60) than both the moderate response (mean = 57.6, sd = 15.5, n = 36, p = 0.01) and nonremitting (mean = 51.5, sd = 16.8, n = 24, p < 0.001) groups. Older age also predicted a favorable course trajectory (OR 3.30 [95 % CI 1.60–6.85]). Further, the trajectory subtypes significantly differed in remission and response rates and number of ECT, with the highest percentage (∼80 %) of patients in the rapid remission subtype achieving remission. Their results lend support for older age as a positive predictor of response to ECT.
Rosen et al. [7] found a similar effect of age on clinical outcome after ECT in their retrospective chart review. They identified 482 patients over a period of 5 years with MDD who received an acute course of ECT, and compared psychiatric rehospitalization rates between geriatric patients 65 years and older (n = 210, mean age = 75.4) and non-geriatric patients (n = 272, mean age = 46.7). The geriatric group had lower rehospitalization rates (6.2 %) compared to the non-geriatric patients (22 %, p < 0.0001). In the geriatric group, approximately 77 % of rehospitalizations occurred within 6 months. Additionally, when analyzed as a continuous variable, older age was associated with lower risk of rehospitalization (per year adjusted hazard ratio, 0.97; 95 % CI 0.96–0.99, p < 0.0001).
Spaans et al. [8•] compared antidepressant efficacy of ECT and pharmacotherapy in a cohort of unipolar depressed geriatric inpatients participating in either a 6-week ECT RCT or a 12-week pharmacotherapy RCT. They found that ECT patients remitted faster (mean = 3.07 weeks, sd = 1.11, n = 47) than those receiving pharmacotherapy (mean = 3.95 weeks, sd = 1.03, n = 81, p = 0.008) when using the Montgomery-Asberg Depression Rating Scale (MADRS) as an outcome measure. Remission rates were 63.8 and 33.3 %, respectively, at the end of each RCT.
Bjølseth et al. [9] compared bifrontal (BF) and right unilateral (RUL) electrode placement in 73 bipolar and unipolar depressed elderly patients (mean age = 74 years). They found no significant difference in response rates (BF = 63.9 %, RUL = 67.6 %, p = 0.741) or remission rates (BF = 51.4 %, RUL = 38.9 %, p = 0.285) between the two groups. Their low remission rates are at odds with those in previously published studies [10, 11]. Overall, this study indicates that BF and RUL electrode placements are equally efficacious in treating depressed elderly patients.
In a case series of four elderly depressed patients, Mahgoub et al. [12] reported a dissociation between the time course of improvement in objective signs versus subjective symptoms during an acute course of ECT, with subjective improvement lagging behind objective improvement. In all instances, patients improved in observable behaviors (social interactions, appetite, sleep, activity, hygiene, etc.) earlier than their subjective reports of their symptoms improved (motivation, energy, mood, etc.). This discrepancy may influence when response and remission criteria are achieved and should be taken into consideration when making clinical decisions about the duration of an acute course of ECT.
In a series of three publications, Oudega et al. [13–15] investigated the relationship between brain structural features on magnetic resonance imaging (MRI) scans, neuropsychological test performance, and clinical variables, before and after ECT. In their earliest communication [13], they sought to determine whether baseline brain structural abnormalities (medial temporal lobe atrophy (MTA), white matter hyperintensities (WMH), global cortical atrophy (GCA)) served as predictors of ECT response. A cohort of 81 elderly patients with MDD received MRI scans before a course of twice weekly ECT (initiated with RUL electrode placement). Clinical symptoms were assessed using the MADRS before, during, and after the treatment course. Approximately 48 % of patients remitted and 74 % responded to ECT. Patients with severe MTA had a significantly lower mean decrease in MADRS scores (37.9 % decrease, n = 6) than those with mild MTA (53.4 % mean decrease, n = 15) and no MTA (66.2 % mean decrease, n = 55). Further, patients without MTA were three times more likely to remit compared to those with moderate or severe MTA (hazard ratio for remission = 3.22 [95 % CI 1.30–7.69, p = 0.01]). The presence of WMH or GCA did not significantly affect change in MADRS scores. The authors suggest that evaluation of MTA in depressed elderly patients may be useful in predicting clinical outcome of ECT.
In a subsequent publication [14], Oudega and colleagues reported the relationship between WMH and cognitive impairment, as assessed by the Mini Mental State Examination (MMSE) during ECT in the same cohort of elderly depressed patients. They found no significant difference in MMSE scores between patients with and without WMH at baseline. Patients with WMH, however, had significant worsening of MMSE scores acutely with ECT, but the differences were no longer significant within 6 weeks after ECT.
In their most recent publication [15], a follow-up of the original cohort up to 12 years later, Oudega et al. reported that the subtype of psychotic depression was not associated with cognitive decline and that WMH before ECT were associated with higher mortality. They noted a weak association with GCA at baseline and subsequent cognitive decline.
In the addition to the above studies, the recently completed Prolonging Remission in Depressed Elderly (PRIDE) [16] study will contribute to the evidence base for the antidepressant efficacy of RUL ultrabrief pulse (UBP) ECT in geriatric patients. In phase I of the two-phase study, unipolar depressed patients, aged 60 years and older, received an acute course of RUL UBP ECT and antidepressant medication (venlafaxine (VLF)), along with a neuropsychological test battery throughout the course of treatment. In phase II of PRIDE, remitters were randomized to one of two maintenance treatment arms: pharmacotherapy (VLF plus lithium) or STABLE+, a fixed schedule of continuation ECT plus rescue ECT plus VLF plus lithium. Results of the PRIDE study have not yet been published, but preliminary analyses of phase I showed that approximately 60 % of patients remitted after an acute course of RUL UBP ECT [17].
We also encourage readers to refer to recently published reviews [2, 18, 19] for further information about the role and practice of ECT in geriatric depression.
Cognition
Bjølseth et al. [20] investigated whether cognitive impairments before ECT predict short-term treatment outcomes. A cohort of 65, unipolar or bipolar depressed, non-demented elderly patients, aged 60 to 85 years old, was assessed at baseline using nine neuropsychological tests that measured processing speed, verbal learning, memory, and executive function. Among the 27 patients with mild cognitive impairment (MCI) at baseline measurements, 15 (55.6 %) were no longer classified as having MCI after a course of twice weekly ECT with BF or RUL electrode placement. Electrode placement was determined by clinician choice, and both groups were analyzed together rather than separately, because no difference was seen a priori in the two groups. Baseline performance on the word reading task was the only assessment that was significantly associated with ECT treatment outcome, with a poorer performance increasing the odds of remission (adjusted OR = 0.92 [95 % CI 0.86–0.99, p = 0.021]). Overall, cognitive deficits in elderly patients at baseline did not predict treatment outcomes following a course of ECT.
Similarly, Dybedal et al. [21] examined whether geriatric patients with “cognitive impairment no dementia” (CIND) or with “no cognitive impairment” (NCI) were more vulnerable to cognitive side effects of ECT. A total of 54 unipolar or bipolar, depressed inpatients (CIND = 18, NCI = 36) and 17 healthy controls, aged 60 to 85 years old, received neurocognitive testing at three time points (baseline, 1 week post-ECT, 3 months post ECT) with either RUL or BF electrode placement. Both groups demonstrated transient short-term cognitive effects at the second time point; however, neither group showed long-term decline in neurocognitive functioning. CIND patients did not experience increased retrograde or anterograde memory impairment compared to the NCI group, suggesting that CIND patients were not more vulnerable to amnesia from ECT.
In an earlier publication from the study described above, Dybedal et al. [22] examined cognition in non-demented, depressed elderly patients (n = 62) before and after a course of ECT compared to cognition of healthy controls (n = 17). Both groups showed either no change or improved cognitive performance on all neuropsychological tests, with the exception of letter fluency, which was significantly worse in the ECT group. However, using reliable change indices (RCIs), the authors found that 11 % of ECT patients had retrograde amnesia for public events and 40 % exhibited significantly reduced neuropsychological functioning, most notably anterograde memory impairment. Thus, in this study, a portion of elderly patients receiving ECT experienced mild cognitive impairments during the acute phase of treatment.
Verwijk et al. [23•] offer support for ECT as a safe/well tolerated treatment option in elderly patients. A cohort of 42 unipolar or bipolar depressed patients over 55 years old received twice weekly ECT (age dosed). All patients started with RUL electrode placement, with the exception of four patients who started with BL electrode placement due to life-threatening conditions. Electrode placement was switched to BL from RUL if symptoms did not improve after six acute treatments. The patients showed no significant decrease in global cognitive function, memory, or executive function measures 1 week and 6 months after ECT compared to baseline. In fact, the cohort significantly improved on several measures of cognition at both post-ECT time points.
Hausner et al. [24•] studied cognitive performance as a function of preexisting cognitive impairment in 44 geriatric inpatients with MDD after a course of RUL or RUL followed by BL ECT (if patients required this switch). Patients were assigned to three groups based on the severity of their cognitive impairment: no cognitive impairment (NCI, n = 13), mild cognitive impairment (MCI, n = 19), or dementia (n = 12). Outcome measures included the MMSE at four time points (before the first ECT, after the sixth ECT, and 6 weeks and 6 months after the end of their treatment course), and a Hamilton Rating Scale for Depression, 21-item (HRSD-21) at two time points (before the first ECT and 6 weeks after ECT). At all time points, the NCI group had the highest scores on cognitive testing, while the dementia group had the lowest. Despite the fact that that all three groups had an initial, nonsignificant cognitive decrement after the acute course of ECT, the NCI group significantly improved in cognitive performance 6 weeks after the last ECT compared to baseline (p = 0.018), and both the NCI and MCI groups significantly improved 6 months after ECT (p = 0.027 and p = 0.036, respectively). There were no significant changes in cognition seen in the dementia group over the course of ECT. Additionally, affective symptoms improved significantly in all groups 6 weeks after the end of ECT. The results of this study showed that ECT induced temporary and reversible cognitive deficits in patients without dementia and that depressive symptoms were successfully treated regardless of baseline cognitive impairment.
In the recently completed PRIDE study, described above, RUL UBP ECT was associated with stable cognitive function as assessed by the Mini Mental State Examination (MMSE) in a large cohort of unipolar depressed geriatric patients. More detailed neuropsychological data from this trial are forthcoming [17].
Continuation/Maintenance ECT
Prevention of relapse after successful acute antidepressant treatment remains an important clinical challenge and is particularly salient for ECT [25, 26]. If the antidepressant effect of ECT cannot be maintained with pharmacotherapy, C/M-ECT becomes an important option for relapse prevention. Van Schaik et al. systematically reviewed the literature on M-ECT in depressed elderly patients. Twenty-two studies (n = 690) met their selection criteria, with 9 including only geriatric patient 55 years and older, and 13 including mixed-age adults with a mean of 55 years or older. They concluded, “On the basis of available literature, M-ECT is probably as effective as continuation medication in severely depressed elderly patients after a successful course of ECT and is generally well tolerated.” [27]
In a retrospective chart review of 42 elderly patients (mean age = 71.54) with schizophrenia (n = 22) and severe affective disorders (n = 20), Shelef et al. [28•] examined the effectiveness of M-ECT in preventing hospital readmissions and reducing admission duration. The number of psychiatric hospitalizations was significantly lower during M-ECT (0.38) compared to pre-M-ECT (1.88) (p < 0.001), accounting for a 79.8% reduction in admissions. Likewise, patients stayed in the hospital for significantly fewer days during M-ECT (12.45) than before M-ECT (215.93) (p < 0.01). The average length of an M-ECT course was 34 months. The results did not differ among patient diagnoses. In this study, M-ECT following an acute course significantly improved clinical outcomes.
Conclusions
In summary, recent findings confirm that ECT is an efficacious, safe, and tolerable antidepressant treatment in an old-age population [27]. This is welcome information for practitioners who treat severely depressed geriatric patients, since many of these patients will have failed to respond to, or could not tolerate, other antidepressant treatment modalities. The accumulating evidence base for the favorable profile of ECT in geriatric patients should help to combat the long-standing stigma associated with the treatment and the resultant reluctance to prescribe it.
The studies in this review suggest that older age is a positive predictor of response to ECT. In elderly patients, ECT results in faster and higher remission rates compared to antidepressant treatment with pharmacotherapy. Time to response and remission, however, may be influenced by the discrepancy between a patient’s subjective report of improvement of symptoms and observed improvement in objective signs. Further, evaluation of brain abnormalities, particularly medial temporal lobe atrophy may be useful in predicting clinical outcomes after ECT in elderly patients.
There has been concern surrounding the cognitive vulnerability of geriatric patients receiving ECT. The data summarized here, however, suggest that the cognitive effect profile of ECT in the elderly is comparable to that in mixed-age populations [29]; following an initial and transient decline, baseline decrements (often attributable to the depression, itself) are usually reversed after an acute course of ECT. The data suggest that baseline cognitive impairment should not necessarily exclude a recommendation for ECT in geriatric patients. However, this finding does not preclude the possibility that certain elderly patients with baseline cerebral impairment may be at greater risk of more prolonged disorientation and/or the development of transient delirium with ECT [30]. Data presented in this review are also encouraging regarding the use of newer ECT techniques, particularly RUL UBP ECT, which holds the promise of maintaining antidepressant efficacy while minimizing adverse cognitive effects. An important limitation of many studies of cognition and ECT is that the most seriously depressed, and possibly cognitively impaired, patients are necessarily excluded because of their inability to participate in neuropsychological testing, or the consent process.
Furthermore, C/M-ECT is emerging as an important treatment strategy for relapse prevention in this population. Treatment outcomes, as measured by hospital readmissions and duration of stays, improve during, compared to before, an M-ECT schedule.
Despite this growing evidence base of support for the use of ECT in the elderly, many questions remain unanswered. Future research should be directed toward further refining ECT technique, as well as optimizing C/M-ECT schedules in order to sustain response after an acute course. Research into biological markers and predictors of response will also be critical to improving and personalizing clinical care with ECT.
References
Papers of particular interest, published recently, have been highlighted as • Of importance
Task Force on Electroconvulsive Therapy. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging. 2nd ed. Washington: American Psychiatric Publishing; 2001.
Kerner N, Prudic J. Current electroconvulsive therapy practice and research in the geriatric population. Neuropsychiatry. 2014;4(1):33–54.
Kellner CH et al. ECT in treatment-resistant depression. Am J Psychiatry. 2012;169(12):1238–44.
Greenberg RM. Electroconvulsive therapy: a selected review. Am J Geriatr Psychiatry. 2015;13(4):268–81.
Manly DT, Oakley Jr SP, Bloch RM. Electroconvulsive therapy in old-old patients. Am J Geriatr Psychiatry. 2000;8(3):232–6.
Rhebergen D et al. Older age is associated with rapid remission of depression after electroconvulsive therapy: a latent class growth analysis. Am J Geriatr Psychiatry. 2015;23(3):274–82. The authors sought to define three course trajectories of clinical response to ECT (rapid remission, moderate response, nonremitting) in patients with MDD based on 6 weeks of follow-up using the HRSD-17. They found that old age was associated with rapid remission.
Rosen BH, Kung S, Lapid MI. Effect of Age on Psychiatric Rehospitalization Rates After Electroconvulsive Therapy for Patients With Depression. J ECT. 2015. [Epub ahead of print].
Spaans HP et al. Speed of remission in elderly patients with depression: electroconvulsive therapy v. medication. Br J Psychiatry. 2015;206(1):67–71. In comparing an ECT RCT with a pharmacotherapy RCT, the authors found that unipolar depressed elderly patients receiving ECT remitted faster than those in the pharmacotherapy RCT.
Bjølseth TM et al. Clinical efficacy of formula-based bifrontal versus right unilateral electroconvulsive therapy (ECT) in the treatment of major depression among elderly patients: a pragmatic, randomized, assessor-blinded, controlled trial. J Affect Disord. 2015;175:8–17.
Kellner CH et al. Bifrontal, bitemporal and right unilateral electrode placement in ECT: randomized trial. Br J Psychiatry. 2010;196(3):226–34.
Bailine S et al. Electroconvulsive therapy is equally effective in unipolar and bipolar depression. Acta psychiatry Scand. 2010;121(6):431–6.
Mahgoub N et al. Symptoms and observations: differences in time course during electroconvulsive therapy in geriatric depressed patients. J ECT. 2014;30(1):e7–8.
Oudega ML et al. White matter hyperintensities, medial temporal lobe atrophy, cortical atrophy, and response to electroconvulsive therapy in severely depressed elderly patients. J Clin Psychiatry. 2011;72(1):104–12.
Oudega ML et al. White matter hyperintensities and cognitive impairment during electroconvulsive therapy in severely depressed elderly patients. Am J Geriatr Psychiatry. 2014;22(2):157–66.
Oudega ML et al. Contribution of white matter hyperintensities, medial temporal lobe atrophy and cortical atrophy on outcome, seven to twelve years after ECT in severely depressed geriatric patients. J Affect Disord. 2015;185:144–8.
Prolonging Remission in Depressed Elderly (PRIDE). ClinicalTrials.gov Identifier: NCT01028508.
Kellner CH et al. Brief pulse and ultrabrief pulse right unilateral electroconvulsive therapy (ECT) for major depression: efficacy, effectiveness, and cognitive effects. J Clin Psychiatry. 2014;75(7):777.
Dines P, Hu W, Sajatovic M. Depression in later-life: an overview of assessment and management. Psychiatr Danub. 2014;26 Suppl 1:78–84.
Riva-Posse P, Hermida AP, McDonald WM. The role of electroconvulsive and neuromodulation therapies in the treatment of geriatric depression. Psychiatr Clin North Am. 2013;36(4):607–30.
Bjølseth TM et al. Baseline cognitive function does not predict the treatment outcome of electroconvulsive therapy (ECT) in late-life depression. J Affect Disord. 2015;185:67–75.
Dybedal GS et al. The Role of Baseline Cognitive Function in the Neurocognitive Effects of Electroconvulsive Therapy in Depressed Elderly Patients. Clin Neuropsychol. 2015;29(4):487–508.
Dybedal GS et al. Cognitive side-effects of electroconvulsive therapy in elderly depressed patients. Clin Neuropsychol. 2014;28(7):1071–90.
Verwijk E et al. Short- and long-term neurocognitive functioning after electroconvulsive therapy in depressed elderly: a prospective naturalistic study. Int Psychogeriatr. 2014;26(2):315–24. Elderly depressed patients receiving 2X/weekly ECT showed no significant decrease in global cognitive function, memory, or executive function measures within one week and six months after ECT compared to baseline. Significant improvements were seen on several neuropsychological measures at both time points.
Hausner L et al. Efficacy and cognitive side effects of electroconvulsive therapy (ECT) in depressed elderly inpatients with coexisting mild cognitive impairment or dementia. J Clin Psychiatry. 2011;72(1):91–7. Hausner and colleagues studied cognitive performance in geriatric patients after an acute course of ECT as a function of pre-existing (baseline) cognitive impairment. After an initial, nonsignificant cognitive decline in all patients following an acute course of ECT, patients with or without mild cognitive impairment showed improvements at various time points after the acute course, while those with dementia showed no significant change in cognition.
Jelovac A, Kolshus E, McLoughlin DM. Relapse following successful electroconvulsive therapy for major depression: a meta-analysis. Neuropsychopharmacology. 2013;38(12):2467–74.
Kellner CH. Relapse after electroconvulsive therapy (ECT). J ECT. 2013;29(1):1–2.27.
van Schaik AM et al. Efficacy and safety of continuation and maintenance electroconvulsive therapy in depressed elderly patients: a systematic review. Am J Geriatr Psychiatry. 2012;20(1):5–17.
Shelef A et al. Acute electroconvulsive therapy followed by maintenance electroconvulsive therapy decreases hospital re-admission rates of older patients with severe mental illness. J ECT. 2015;31(2):125–8. In a retrospective chart review, the authors used psychiatric readmission rates and duration of admission to assess the efficacy of M-ECT in elderly patients with schizophrenia and severe affective disorders. Readmission rates and length of admission were both decreased with M-ECT.
Semkovska M, McLoughlin DM. Objective cognitive performance associated with electroconvulsive therapy for depression: a systematic review and meta-analysis. Biol Psychiatry. 2010;68(6):568–77.
Coffey CE, Kellner CH. Electroconvulsive therapy. In CE Coffey, JL Cummings, MR Lovell, & GD Pearlson (Eds.), The American Psychiatric Press textbook of geriatric neuropsychiatry (pp. 829–859). Whashington, DC: American Psychiatric Press; 2000.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Emma T. Geduldig declares no conflict of interest.
Charles H. Kellner reports grant support from the National Institute of Mental Health, royalties from Cambridge University Press, and honoraria from Psychiatric Times, UpToDate, and the North Shore-LIJ Health System.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Disorders
Rights and permissions
About this article
Cite this article
Geduldig, E.T., Kellner, C.H. Electroconvulsive Therapy in the Elderly: New Findings in Geriatric Depression. Curr Psychiatry Rep 18, 40 (2016). https://doi.org/10.1007/s11920-016-0674-5
Published:
DOI: https://doi.org/10.1007/s11920-016-0674-5