Abstract
Purpose of Review
Postcraniotomy headache (PCH) is a common adverse event and can lead to various complications and decreased quality of life.
Recent Findings
To reduce postcraniotomy pain and associated complications, a multimodal pain therapy including analgesics, analgesic adjuncts, and regional anesthesia is essential. The use of opioids should be minimized to facilitate prompt postoperative neurosurgical assessment. Here, we provide an update on the latest evidence regarding the role of scalp nerve blocks in the pain management of patients undergoing craniotomy procedure.
Summary
Nerve blocks are effective in alleviating postoperative pain after craniotomy. Scalp blocks contribute to lower pain levels and less opioid consumption in the first 48 h following surgery. Moreover, there is a significant decrease in patients suffering from PONV among patients who receive scalp block.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Elective craniotomy is a frequently performed neurosurgical intervention for various conditions such as brain tumor resection, treatment of intracranial aneurysms, arterial-venous malformations, or epilepsy surgery [1]. One of the most encountered medically significant events after craniotomy is postcraniotomy headache (PCH) [2,3,4]. Nearly 90% of patients undergoing craniotomy procedures experience postoperative pain within the first 24 h with 55% declaring moderate to severe pain [5, 6]. The International Headache Society (IHS) distinguishes between “Acute Headache Attributed to Craniotomy” that is defined as a headache that appears within 7 days following craniotomy and “Persistent Headache Attributed to Craniotomy” which is the headache lasting more than 3 months [7]. Not only is acute pain a common event after surgery, nearly 30% of patients suffer from chronic pain after 3 months postoperatively [8] and 12% after 1 year [9].
While acute PCH is usually attributed to a somatic origin following surgical procedure involving an injury of the scalp, the soft tissue, pericranial muscles, and the dura mater [10, 11, 12•, 13], the origin of chronic PCH remains unclear. In the literature, there are various factors which may contribute to the development of chronic pain including cerebrospinal fluid leakage, cervical muscle damage, dural traction, and scar tissue formation [2, 11]. Risk factors contributing to PCH are female gender and young age due to heightened pain levels. [2, 8, 11]. Anxiety, depression, and preoperative pain are also identified as potential risk factors [8, 13]. While some evidence suggests preoperative quantitative sensory testing can predict postoperative pain in patients undergoing various elective surgeries, its potential in neurosurgery remains unknown [14, 15]. In addition, the surgical procedure itself may influence postoperative pain levels, with infratentorial procedures tending to cause more pain than the supratentorial approach [13, 16].
Intraoperative inadequate analgesia can lead to various complications, including arterial hypertension, which may result in intracranial hemorrhage and high intracranial pressure [17]. Furthermore, it can result in increased mortality, or an extended hospital stay [18]. These complications can mimic the risk of other complications after neurosurgery [19]. In contrast, overuse of analgesics, in particular opioids, may lead to an impeded postoperative neurological assessment [20]. In addition, overuse of opioids can intensify opioid dependence in vulnerable patients, even when the opioid has been used only briefly [21•]. Finally, the prevention of postoperative pain after acute craniotomy may help reduce the risk for chronic pain [19]. A recently published systematic review of 53 randomized controlled trials (RCT) investigating pain management after elective craniotomy concluded that, in addition to paracetamol, non-steroidal anti-inflammatory drugs (NSAID), intravenous dexmedetomidine infusion, and opioids as rescue analgesics, a regional analgesic technique such as a scalp nerve block or incision-site infiltration should be applied [22••].
Regional anesthesia has significantly impacted postoperative pain management in the last few years in multiple areas of anesthesia. However, its importance in neurosurgery remains elusive. This narrative review aims to provide an overview of the current literature on the role of nerve blocks in craniotomy procedures. Therefore, we seek to explore the efficacy of scalp nerve blocks and their clinical outcomes, particularly in pain management. In addition to general anesthesia, performing scalp blocks during craniotomies is a crucial tool in postoperative pain management. Through a synthesis of existing literature, we aim to contribute to the ongoing discourse on optimal pain management strategies in craniotomy procedures.
The Innervation of the Scalp
The human scalp receives sensory input from various nerves, arising from both the cervical spine and cranial nerves (Fig. 1). The supratrochlear and the supraorbital nerves originate from the frontal nerve, which, in turn, arises from the ophthalmic division of the trigeminal nerve [23,24,25,26]. The supraorbital nerve provides sensation to the upper eyelid, the conjunctiva of the eye, the frontal sinus, and the skin on the anterior scalp. In contrast, the supratrochlear nerve innervates the skin of the forehead, the bridge of the nose, the conjunctiva, and the upper eyelid [25, 27, 28]. The supraorbital nerve exists in the majority as notches [29] and can be palpated 2–3 cm from the midline of the forehead [30] at the same sagittal plane as the pupil [24]. The supratrochlear nerve can be found around 1 cm medial to the supraorbital nerve [23] at the top of the angle formed by the eyebrow and the nasal spine [24]. Ultrasound guidance can be useful for targeting both nerves [25].
Schematic of scalp innervation, adapted from [12•]
The zygomaticotemporal nerve arises from the maxillary division of the trigeminal nerve. It innervates the skin of the temple and a small area of the forehead [26, 27]. Palpating the lateral orbital rim posterior to the frontozygomatic suture can help locate this nerve [23, 30].
The auriculotemporal nerve derives from the mandibular division of the trigeminal nerve [24, 26]. It provides the sensory innervation of the posterior part of the skin of the temple [24] and the tragus and anterior portions of the ear [26, 27]. It is typically found approximately 1.5 cm anterior to the ear at the tragus level [24, 27].
The great postauricular nerve, originating from the cervical plexus, is located approximately 1.5 cm posterior to the pinna at the level of the tragus [23, 24].
The greater occipital nerve arises from the dorsal ramus of the second cervical root [26, 27]. It provides sensory innervation of the major part of the posterior scalp. The nerve is medially located to the occipital artery and can be anesthetized via landmarks—the injection site is 2 cm lateral and inferior to the occipital protuberance—or ultrasound-guided [26, 30, 31].
The lesser occipital nerve, arising from the ventral rami of the spinal nerves C2 and C3, innervates the skin on the lateral part of the scalp behind the ear [25, 27]. It is typically found 7 cm lateral to the occipital protuberance along the nuchal ridge [23].
The third occipital nerve arises from the dorsal ramus of C3 and provides sensory innervation of the skin over the occipital regions and the facet joints in the upper cervical spine [27].
Collectively, the block of these seven nerves is referred to as “scalp block.” For the sake of simplicity, we only use the term “scalp block” in the following text.
Comparison of Different Analgesic Regimes to Treat PCH
Regional Anesthesia for Prevention of Pain
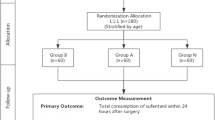
A recent systematic review and meta-analysis including 22 RCTs and 1550 patients [32•] analyzed the effect of scalp block in craniotomy procedures for postoperative pain and opioid use. Overall, it showed a reduction of pain at all postoperative time points and a decreased opioid consumption postoperatively. The mean difference of the visual analog scale (VAS) 2 h postoperative was − 1.4 (95% confidence interval (CI) − 1.8, − 0.99; ̸2 = 84%), at 12 h − 0.75 (95% CI − 1.07, − 0.42; ̸2 = 60%), at 24 h − 0.95 (95% CI − 1.33, − 0.57; ̸2 = 82%), at 48 h − 1.24 (95% CI − 1.7, − 0.78; ̸2 = 77%), and at 72 h − 1.3 (95% CI − 1.67, − 0.93; ̸2 = 0%). The opioid use within 48 h was less with a mean difference of − 15.61 (95% CI − 25.76, − 5.49; ̸2 = 22).
Another recent systematic review and meta-analysis analyzing the effect of scalp blocks for prevention of pain after craniotomy showed similar results. There were 12 RCTS with 833 patients included (10 studies as well in the systematic review mentioned above). The mean difference of the VAS at the early period (between 2 and 6 h postoperative) was -1.84 (95% CI − 2.95, − 0.73; ̸2 = 84%, p-value = 0.00), at the intermediate period (between 6 and 12 h) − 1.16 (95% CI − 1.84, − 0.49; ̸2 = 50.1%, p-value = 0.062) and at the late period (between 12 and 24 h) − 0.98 (95% CI − 2.13, 0.17; ̸2 = 88.3%, p-value = 0.00) [33].
There was only one study in the whole research investigating pain outcomes after hospital discharge. Rigamonti et al. conducted a RCT including a treatment group with bilateral scalp blocks with 0.5% bupivacaine and a control group with saline. They conducted a phone interview on the fifth, 30th, and 60th postoperative day revealing no significant difference in postoperative pain. However, only 7 out of 85 initially included patients responded at day 60 [18].
Influence of the Type of Local Anesthetic Agents
Comparing Different Types of Blocks
One RCT, from Kulikov et al., investigated in 2021 the difference between preoperative and postoperative scalp block in patients undergoing craniotomy. They found no significant difference in postoperative pain levels at 24 h [34]. Another study showed a similar effect [35]. In most of the other identified studies, the nerve block was performed preoperatively, resulting in favorable pain relief after craniotomy [36,37,38,39,40,41,42,43,44,45]. If the scalp block was performed postoperatively [18, 33, 40, 56, 57], this also led to significantly lower pain levels up to 6 h postoperatively compared to patients receiving only saline [46], whereas another study showed lower VAS scores even up to 24 h after craniotomy [47]. In addition, the time interval to the first use of PCA drug and rescue analgesics was longer than in the control group [48].
However, significant hemodynamic improvements during surgery were observed when the scalp block was performed preoperatively [32•]. Furthermore, if the block was conducted preoperatively, the amount of fentanyl was significantly lower [34].
Importantly, the operation duration was not prolonged due to preoperative scalp block administration [32•].
Comparing Different Types of Local Anesthetic Agents
Scalp nerve block with ropivacaine instead of (levo)bupivacaine showed further promising results. A RCT from 2019 investigated the effect of preoperative scalp block with 0.75% ropivacaine on postoperative outcomes. It revealed lower postoperative pain intensity, a longer duration before the first dose of oxycodone was needed, and less overall consumption of opioids. In addition, a decreased level of interleukin-6 in plasma 6 h after craniotomy was shown, indicating an attenuated inflammatory response [42]. Comparing the effectiveness of ropivacaine 0.2%, 0.33% and 0.5%, a study found no significant difference among the three concentrations up to 4 h after craniotomy. However, after 4 h, ropivacaine 0.5% led to significantly lower VAS scores [43]. A prospective study from 2014 investigating the effect of a mixture of lidocaine 2% with ropivacaine 0.75% for scalp block in cases of patients undergoing awake craniotomy showed effective outcomes as well [49]. Hussien et al. compared intravenous fentanyl to a scalp block with 2% lidocaine, 0.5% bupivacaine, and 1:200,000 epinephrine. The study revealed that scalp block led to less opioid consumption, lower VAS scores, and significantly lower heart rate and mean arterial pressure (MAP) after head pinning [40].
Comparing to Wound Infiltration
Skutuliene et al. conducted a RCT in 2021 comparing a scalp block group with a wound infiltration group and a control group receiving only systemic analgesia (1 g of paracetamol and 2 mg/kg ketoprofen). The scalp block group experienced significantly lower postoperative pain scores [50]. While another study revealed a similar positive effect of the scalp block compared to a local incision [42], no such effect has been shown by Akcil et al. [36].
Comparing Regional Anesthesia vs. Intravenous Drugs
Combining regional anesthesia with postoperative intravenous steroids, such as 8 mg dexamethasone, resulted in decreased opioid consumption and improved hemodynamic stability [51]. Another study from 2013 revealed similar results—preoperative steroids led to lower Numeric Rating Scale (NRS) scores postoperatively [6]. While systemic dexamethasone may be beneficial in the short run, its potential negative oncologic effects should be considered in patients undergoing craniotomy for glioblastoma resection [52].
An RCT from 2023 by Stachtari et al. involved 150 patients and investigated the effect of adding dexmedetomidine to a scalp block with ropivacaine 0.5%. Patients in the combined group reported less heart rate increase during incision and closure of the dura and the skin than the control group only using saline and the group only using ropivacaine. In addition, the consumption of remifentanil was significantly lower in the combined group [53].
Overall, a preoperative- and postoperative-conducted scalp block shows promising results leading to less pain levels postoperative. Furthermore, doing it preoperatively leads to less hemodynamic changes and less need of opioids intraoperative. Both ropivacaine and bupivacaine, in various concentrations, seem to be equal potential local anesthetic agents leading both to reduced pain levels and less opioid consumption. A combination with intravenous steroids may be effective in some patients. However, there is high-quality evidence regarding pain levels after hospital discharge and therefore the transition from acute to chronic pain remains scarce.
Complications
Specific Complications of Regional Anesthesia
When blocking the auriculotemporal nerve and the greater occipital nerve, the anesthetist should be cautious since the artery is close [26]. In the systematic analyses of Chen and Duda, both from 2022, no other complication than PONV was found [32•, 33]. However, in another study, 7 of 42 included patients receiving a scalp block developed postoperative facial nerve palsy in a 1-year postoperative period [54].
General Complications
General complications may occur after a local anesthetic infiltration such as hematoma, infection, or intravascular injection [24]. In a study from 2022, including 151 patients, there were 2 patients suffering from an incision site infection and one patient suffering from intracranial infection after elective craniotomy [44].
Patients diagnosed with malignant glioma tend to have a lower likelihood of recurrence when a scalp block was conducted for surgery. The progression-free survival was significantly better in a study from 2021 comprising 230 patients. This may be explained due to the lower postoperative systemic and local inflammatory response in well pain-controlled patients [55].
Effect on Heart Rate and Arterial Blood Pressure
Various studies indicated that scalp blocks lead to significant lower intraoperative mean arterial pressure (MAP) and heart rate [38, 40, 42, 49, 53]. Conversely, these effects are particularly seen during noxious events such as head pinning or during working with the bone [40]. Carella et al. found an increased MAP 1, 3, and 5 min after head pinning and at skin incision in the control group without regional anesthesia, but no effect at the time of dura incision was observed [38].
Postoperative Nausea and Vomiting (PONV)
Postoperative nausea and vomiting (PONV) are frequent complications after neurosurgical procedures with 50% of patients experiencing nausea [56]. In particular, the high abdominal and intrathoracic pressures during vomiting may result in further complications such as increased intracranial pressure [57]. In cases of depressed neurological status postoperative due to opioid treatment, the risk of aspiration may be elevated [56]. Fifty percent of the included patients experienced nausea and 39% vomiting with a significantly higher incidence of PONV in infratentorial surgical procedures. Risk factors for PONV were reported as infratentorial surgical procedures [56], female sex, and younger age due to heightened pain levels [56, 58]. Yang et al. revealed in their RCT in 2019 that the incidence of PONV was significantly lower in the group with scalp block compared to the group with local infiltration and the control group suggesting that a well-functioning scalp block may lead to less PONV due to less consumption of opioids [42]. Supporting this result, Chen et al. [33] found in their meta-analysis an odds ratio of 0.61 (95% CI 0.23, 1.67). Another systematic review and meta-analysis of Duda, conducted as well in 2022, including 22 RCTs, revealed a similar OR 0.65 (95% CI 0.43, 0.99; ̸2 = 20%) [32]. In summary, there is high-quality evidence that scalp blocks lead to less PONV.
Conclusion
In summary, nerve blocks prove to be effective in alleviating postoperative pain after craniotomy. Our findings demonstrate that scalp blocks contribute to lower pain levels and less opioid consumption in the first 48 h following surgery. Moreover, there is a significant decrease in patients suffering from PONV among patients who receive scalp block. Consequently, scalp blocks should be implemented in the multimodal pain therapy, particularly in patients with risk factors for heightened pain levels such as women and young people. We recommend employing regional anesthesia preoperatively, as it may result in lower amount of opioids used during surgery and a more favorable hemodynamic profile, ensuing less complications such as high pressure and intracranial hemorrhage.
Additional high-quality evidence is needed to investigate pain levels across various time periods, aiming to prevent the transition from acute to chronic PHC. Furthermore, adverse events other than PONV should be more broadly explored for an extensive understanding of the efficacy and safety of nerve blocks in neurosurgical procedures.
Data Availability
No datasets were generated or analyzed during the current study.
Code Availability
Not applicable.
Abbreviations
- IHS:
-
International Headache Society
- MAP:
-
Mean arterial pressure
- NRS:
-
Numeric Rating Scale
- NSAID:
-
Non-steroidal anti-inflammatory drugs
- PCA:
-
Patient-controlled analgesia
- PCH:
-
Postcraniotomy headache
- PONV:
-
Postoperative nausea and vomiting
- RCT:
-
Randomized controlled trial
- VAS:
-
Visual analog scale
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Subbarao BS, Fernández-de Thomas RJ, M Das J, Eapen BC. Postcraniotomy Headache. 2024 Jan 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 29493922
Haldar R, Kaushal A, Gupta D, Srivastava S, Singh PK. Pain following craniotomy: reassessment of the available options. Biomed Res Int. 2015;2015:509164. https://doi.org/10.1155/2015/509164. Epub 2015 Oct 1. PMID: 26495298; PMCID: PMC4606089.
Lamacraft G. The link between acute postoperative pain and chronic pain syndromes. Sout Afr J Anaesth Analg. 2012;18:45–50.
Flexman AM, Ng JL, Gelb AW. Acute and chronic pain following craniotomy. Curr Opin Anaesthesiol. 2010;23(5):551–7.
Mordhorst C, Latz B, Kerz T, Wisser G, Schmidt A, Schneider A, et al. Prospective assessment of postoperative pain after craniotomy. J Neurosurg Anesthesiol. 2010;22(3):202–6.
Hansen MS, Brennum J, Moltke FB, Dahl JB. Suboptimal pain treatment after craniotomy. Dan Med J. 2013;60(2):A4569.
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018 Jan;38(1):1–211. https://doi.org/10.1177/0333102417738202. PMID: 29368949.
Rocha-Filho PAS, Gherpelli JLD, de Siqueira JTT, Rabello GD. Post-craniotomy headache: characteristics, behaviour and effect on quality of life in patients operated for treatment of supratentorial intracranial aneurysms. Cephalalgia. 2008;28:41–8.
Kaur A, Selwa L, Fromes G, Ross DA. Persistent headache after supratentorial craniotomy. Neurosurgery. 2000;47(3):633–6.
De Benedittis G, Lorenzetti A, Migliore M, Spagnoli D, Tiberio F, Villani R. Postoperative pain in neurosurgery: a pilot study in brain surgery. Neurosurgery. 1996;38:466–70.
de Gray LC, Matta BF. Acute and chronic pain following craniotomy: a review. Anaesthesia. 2005;60(7):693–704.
• Bello C, Andereggen L, Luedi MM, Beilstein CM. Postcraniotomy headache: etiologies and treatments. Curr Pain Headache Rep. 2022;26:357–64. A recent overview of ethiologies and treatment strategsie in postcraniotomie headache.
Vacas S, Van de Wiele B. Designing a pain management protocol for craniotomy: a narrative review and consideration of promising practices. Surg Neurol Int. 2017;8:291.
Luedi MM, Schober P, Hammoud B, Andereggen L, Hoenemann C, Doll D. Preoperative pressure pain threshold is associated with postoperative pain in short-stay anorectal surgery: a prospective observational study. Anesth Analg. 2021;132(3):656–62.
Braun M, Bello C, Riva T, Hönemann C, Doll D, Urman RD, Luedi MM. Quantitative Sensory Testing to Predict Postoperative Pain. Curr Pain Headache Rep. 2021 Jan 14;25(1):3. https://doi.org/10.1007/s11916-020-00920-5. PMID: 33443676; PMCID: PMC7808998.
Irefin SA, Schubert A, Bloomfield EL, DeBoer GE, Mascha EJ, Ebrahim ZY. The effect of craniotomy location on postoperative pain and nausea. J Anesth. 2003;17(4):227–31.
Basali A, Mascha EJ, Kalfas I, Schubert A. Relation between perioperative hypertension and intracranial hemorrhage after craniotomy. Anesthesiology. 2000;93(1):48–54.
Rigamonti A, Garavaglia MM, Ma K, Crescini C, Mistry N, Thorpe K, et al. Effect of bilateral scalp nerve blocks on postoperative pain and discharge times in patients undergoing supratentorial craniotomy and general anesthesia: a randomized-controlled trial. Can J Anaesth. 2020;67(4):452–61.
Galvin IM, Levy R, Day AG, Gilron I. Pharmacological interventions for the prevention of acute postoperative pain in adults following brain surgery. Cochrane Database Syst Rev. 2019 Nov 21;2019(11):CD011931. https://doi.org/10.1002/14651858.CD011931.pub2. PMID: 31747720; PMCID: PMC6867906.
Ban VS, Bhoja R, McDonagh DL. Multimodal analgesia for craniotomy. Curr Opin Anaesthesiol. 2019;32(5):592–9.
• Baumann L, Bello C, Filipovic MG, Urman RD, Luedi MM, Andereggen L. Acute pain and development of opioid use disorder: patient risk factors. Curr Pain Headache Rep. 2023;27:437–44. A recent overview of patient-derived risk factors for developing postoperative opioid dependency.
•• Mestdagh FP, Lavand’homme PM, Pirard G, Joshi GP, Sauter AR, Van de Velde M, et al. Pain management after elective craniotomy: a systematic review with procedure-specific postoperative pain management (PROSPECT) recommendations. Eur J Anaesthesiol. 2023;40(10):747–57. Relevant PROSPECT guideline for analgesia after elective craniotomy.
Dean C, Papangelou A. How I do it: scalp blocks for the neuroanesthesiologist. ASRA News 2021;46. https://doi.org/10.52211/asra110121.067
Sola C, Dadure C, Choquet O, Capdevila X. Nerve blocks of the face In: NYSORA. https://www.nysora.com/techniques/head-and-neck-blocks/nerve-blocks-face/#toc_CONCLUSION. Accessed on 11 January 2024.
Muse IO, Straker T. A comprehensive review of regional anesthesia for head and neck surgery. Journal of Head & Neck Anesthesia. 5(2):p e33. May 2021. https://doi.org/10.1097/HN9.0000000000000033
Potters JW, Klimek M. Local anesthetics for brain tumor resection: current perspectives. Local Reg Anesth. 2018;11:1–8.
Kemp WJ 3rd, Tubbs RS, Cohen-Gadol AA. The innervation of the scalp: a comprehensive review including anatomy, pathology, and neurosurgical correlates. Surg Neurol Int. 2011;2:178.
Novitch M, Hyatali FS, Jeha G, Motejunas M, Bonneval L, Pankaj T, et al. Regional techniques for head and neck surgical procedures. Best Pract Res Clin Anaesthesiol. 2019;33(4):377–86.
Nanayakkara D, Manawaratne R, Sampath H, Vadysinghe A, Peiris R. Supraorbital nerve exits: positional variations and localization relative to surgical landmarks. Anat Cell Biol. 2018 Mar;51(1):19–24. https://doi.org/10.5115/acb.2018.51.1.19. Epub 2018 Mar 28. PMID: 29644106; PMCID: PMC5890013.
Barre SM, Adhikary SD. Acute pain management protocol for cranial procedures. In First Aid Perioperative Ultrasound: Acute Pain Manual for Surgical Procedures. Springer International Publishing. 2023. p. 261–290. https://doi.org/10.1007/978-3-031-21291-8_17
Levin M. Nerve blocks in the treatment of headache. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics. 2010;7:197–203.
• Duda T, Lannon M, Gandhi P, Martyniuk A, Farrokhyar F, Sharma S. Systematic review and meta-analysis of randomized controlled trials for scalp block in craniotomy. Neurosurgery. 2023;93:4–23. Comprehensive systematic review about the value of periprocedural scalp blocks in craniotomy.
Chen Y, Ni J, Li X, Zhou J, Chen G. Scalp block for postoperative pain after craniotomy: a meta-analysis of randomized control trials. Front Surg. 2022 Sep 26;9:1018511. https://doi.org/10.3389/fsurg.2022.1018511. PMID: 36225222; PMCID: PMC9550001.
Kulikov A, Tere V, Sergi PG, Pugliese F, Lubnin A, Bilotta F. Preoperative versus postoperative scalp block combined with incision line infiltration for pain control after supratentorial craniotomy. Clin J Pain. 2021;37(3):194–8.
Luo M, Zhao X, Deng M, Hu Y, Yang X, Mei Z, et al. Scalp nerve block, local anesthetic infiltration, and postoperative pain after craniotomy: a systematic review and network meta-analysis of randomized trials. J Neurosurg Anesthesiol. 2023;35(4):361–74.
Akcil EF, Dilmen O, Vehid H, Ibisoglu L, Tunali Y. Which one is more effective for analgesia in infratentorial craniotomy? The scalp block or local anesthetic infiltration. Clinical Neurology Neurosurgery. 2017;154:98–103.
Can BO, Bilgin H. Effects of scalp block with bupivacaine versus levobupivacaine on haemodynamic response to head pinning and comparative efficacies in postoperative analgesia: a randomized controlled trial. J Int Med Res. 2017;45(2):439–50.
Carella M, Tran G, Bonhomme VL, Franssen C. Influence of levobupivacaine regional scalp block on hemodynamic stability, intra- and postoperative opioid consumption in supratentorial craniotomies: a randomized controlled trial. Anesth Analg. 2021 Feb 1;132(2):500–511. https://doi.org/10.1213/ANE.0000000000005230. PMID: 33060491.
Gazoni FM, Pouratian N, Nemergut EC. Effect of ropivacaine skull block on perioperative outcomes in patients with supratentorial brain tumors and comparison with remifentanil: a pilot study. J Neurosurg. 2008;109(1):44–9.
Hussien ABM, Saleh ZT, Al attar HAS, Nasr YM. Preoperative regional scalp block versus intraoperative intravenous fentanyl for attenuating intraoperative surgical stress response to supratentorial craniotomy in adult patients under general anaesthesia. Int J Res Pharm Sci. 2020;11:6996–7004.
Tuchina L, Somboonviboon W, Supbornsug K, Worathongchai S, Limutaitip S. Bupivacaine scalp nerve block: hemodynamic response during craniotomy, intraoperative and post-operative analgesia. Asian Biomedicine. 2010;4:243–51.
Yang X, Ma J, Li K, Chen L, Dong R, Lu Y, et al. A comparison of effects of scalp nerve block and local anesthetic infiltration on inflammatory response, hemodynamic response, and postoperative pain in patients undergoing craniotomy for cerebral aneurysms: a randomized controlled trial. BMC Anesthesiol. 2019;19(1):91.
Yang Y, Ou M, Zhou H, Tan L, Hu Y, Li Y, et al. Effect of scalp nerve block with ropivacaine on postoperative pain in patients undergoing craniotomy: a randomized, double blinded study. Sci Rep. 2020;10(1):2529.
Wang L, Cai H, Wang Y, Liu J, Chen T, Liu J, et al. Enhanced recovery after elective craniotomy: a randomized controlled trial. J Clin Anesth. 2022;76: 110575.
Ayoub C, Girard F, Boudreault D, Chouinard P, Ruel M, Moumdjian R. A comparison between scalp nerve block and morphine for transitional analgesia after remifentanil-based anesthesia in neurosurgery. Anesth Analg. 2006 Nov;103(5):1237–40. https://doi.org/10.1213/01.ane.0000244319.51957.9f. PMID: 17056961.
Bala I, Gupta B, Bhardwaj N, Ghai B, Khosla VK. Effect of scalp block on postoperative pain relief in craniotomy patients. Anaesth Intensive Care. 2006;34(2):224–7.
Nguyen A, Girard F, Boudreault D, Fugere F, Ruel M, Moumdjian R, et al. Scalp nerve blocks decrease the severity of pain after craniotomy. Anesth Analg. 2001;93(5):1272–6.
Hwang J-Y, Bang J-S, Oh C-W, Joo J-D, Park S-J, Do S-H, et al. Effect of scalp blocks with levobupivacaine on recovery profiles after craniotomy for aneurysm clipping: a randomized, double-blind, and controlled study. World Neurosurg. 2015;83:108–13.
Chaki T, Sugino S, Janicki PK, Ishioka Y, Hatakeyama Y, Hayase T, Kaneuchi-Yamashita M, Kohri N, Yamakage M. Efficacy and safety of a lidocaine and ropivacaine mixture for scalp nerve block and local infiltration anesthesia in patients undergoing awake craniotomy. J Neurosurg Anesthesiol. 2016 Jan;28(1):1–5. https://doi.org/10.1097/ANA.0000000000000149. PMID: 25493926.
Skutuliene J, Banevicius G, Bilskiene D, Macas A. The effect of scalp block or local wound infiltration versus systemic analgesia on post-craniotomy pain relief. Acta Neurochir (Wien). 2022;164(5):1375–9.
Gaudray E, N’Guyen C, Martin E, Lyochon A, Dagain A, Bordes J, et al. Efficacy of scalp nerve blocks using ropivacaine 0,75% associated with intravenous dexamethasone for postoperative pain relief in craniotomies. Clin Neurol Neurosurg. 2020;197:106125.
Luedi MM, Singh SK, Mosley JC, Hassan ISA, Hatami M, Gumin J, et al. Dexamethasone-mediated oncogenicity in vitro and in an animal model of glioblastoma. J Neurosurg. 2018;129(6):1446–55.
Stachtari C, Stergiouda Z, Koraki E, Sifaki F, Bagntasarian S, Chatzopoulos S. Dexmedetomidine as an adjuvant to scalp block in patients undergoing elective craniotomy: A prospective randomized controlled trial. Clin Neurol Neurosurg. 2023 Apr;227:107669. https://doi.org/10.1016/j.clineuro.2023.107669. Epub 2023 Mar 11. PMID: 36924695.
McNicholas E, Bilotta F, Titi L, Chandler J, Rosa G, Koh A. Transient facial nerve palsy after auriculotemporal nerve block in awake craniotomy patients. Cases Anesthesia Analgesia. 2014;2:0–3.
Sung CH, Tsuang FY, Shih CC, Chang JL, Liao MH, Yang YW, et al. Scalp block is associated with improved recurrence profiles in patients undergoing primary glioma resection surgery. J Neurosurg Anesthesiol. 2021;33(3):239–46.
Fabling JM, Gan TJ, Guy J, Borel CO, el-Moalem HE, Warner DS. Postoperative nausea and vomiting. A retrospective analysis in patients undergoing elective craniotomy. J Neurosurg Anesthesiol. 1997;9(4):308–12.
Jangra K, Kumari K, Panda NB, Samagh N, Luthra A. Postoperative nausea and vomiting in neurosurgical patients: current concepts and management. Neurol India. 2018;66:1117–23.
Gan TJ, Belani KG, Bergese S, Chung F, Diemunsch P, Habib AS, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2020;131(2):411–48.
Funding
None.
Author information
Authors and Affiliations
Contributions
Andrea Stieger, Carolina S. Romero, Lukas Andereggen, Daniel Heisenberg, Richard D. Urman, and Markus M. Luedi conducted literature searches, wrote the article, and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
Richard D. Urman is a Section Editor for the journal. Richard D. Urman fees/funding from AcelRx and Merck. The other authors report no conflicts of interest. No funding was involved.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Ethics Approval
As a review article, ethical approval is not required by Swiss law. This review article complies with ethical standards.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stieger, A., Romero, C.S., Andereggen, L. et al. Nerve Blocks for Craniotomy. Curr Pain Headache Rep 28, 307–313 (2024). https://doi.org/10.1007/s11916-024-01236-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-024-01236-4