Abstract
Purpose of Review
Point of care ultrasound (POCUS) has played a role across almost every medical specialty. Although anesthesiologists have been using bedside ultrasound for nerve blocks and vascular access for many years now, there has been a recent push to incorporate whole-body POCUS into anesthesiologists’ training and daily practice. This article provides a brief overview of the indications, techniques for image acquisition, and general principles in interpreting basic images.
Recent Findings
Whole-body POCUS can provide quick diagnoses and impact clinical management across relevant pre-, intra-, and post-operative settings. Anesthesia providers need to understand different applications for POCUS, including focused cardiac ultrasound (FoCUS), lung ultrasound (LUS), gastric ultrasound, abdominopelvic ultrasound, and the use of ultrasound for airway management. Currently, there is no standard ultrasound curriculum for anesthesiology residents, and teaching methods include informal bedside teaching, structured expert demonstration, didactic lectures, and simulations. Model/simulation-based lecture series may be effective in teaching ultrasound to anesthesiology residents, and e-learning and traditional didactics are both equally effective in teaching POCUS applications such as LUS and focused assessment with sonography in trauma (FAST). Creating protocol-guided frameworks for POCUS, such as I-AIM (indication, acquisition, interpretation, medical decision making), can also ensure more consistent and reliable diagnoses and interpretations of findings.
Summary
Applications of POCUS should be focused, goal-oriented, easily learned, rapidly performable at bedside, accurate, and reliable. A variety of studies have shown this potential for POCUS in assessing cardiac, pulmonary, and intraabdominal pathologies, making it an emerging area of interest in medicine. The incorporation of POCUS into perioperative medicine provides an important tool to ensure continued improvement in coordinating care for patients in the perioperative period.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasonography is a safe, portable, relatively inexpensive, and easily accessible imaging modality that has been used for more than half a century by physicians for diagnostic and procedural purposes. Point of care ultrasound (POCUS), or the use of ultrasound that is brought to the patient and performed by the provider for evaluation, has played a role in almost every medical specialty [1••]. It has dramatically expanded in areas of critical care, surgery, and emergency medicine, as well as primary care and internal medicine.
In anesthesiology, bedside ultrasound has become a familiar tool in its use for vascular access and nerve blocks. More recently, however, increasing attention has been placed on incorporating whole-body POCUS into the daily practice of the modern anesthesiologist, not just for procedural guidance but as an adjunct to traditional diagnostic tools in the evaluation and management of patient care [2]. Anesthesiologists may benefit from the use of ultrasound in many settings, whether preoperatively to help assess a patient’s cardiac function or aspiration risk, to intraoperatively and postoperatively to assess for causes in sudden changes in hemodynamic or respiratory status (Table 1).
Whole-body POCUS curriculums have been successfully incorporated into anesthesiology training programs, with clinical examinations afterwards showing POCUS affecting clinical management at a rate of 76% and new pathology detection at 31% [3]. Accordingly, there has been a national push to incorporate whole-body ultrasound into pre-anesthetic evaluation and anesthesiology training [4] with some even calling for the start of bedside ultrasound training in medical school [5]. However, despite general consensus that POCUS is a valuable tool, there is limited and inadequate training among anesthesiology residents [6].
Several publications have advocated for the use and benefits of whole-body POCUS for anesthesiologists [6, 7] [2, 7, 8••], and detailed techniques and applications of bedside cardiac [9], lung [10, 11••,12••], abdominal [13, 14], gastric [15, 16], and airway [17, 18] ultrasound have been described for use in various specialties. However, to our knowledge, there is presently no comprehensive overview of the techniques and uses of perioperative POCUS for anesthesiologists. The purpose of this review is thus to provide an overview of the different applications of perioperative POCUS that can act as a primer for anesthesiologists and trainees.
General Principles
Basics of Ultrasound
Ultrasound is defined as high-frequency sound waves that are above what humans can hear, or more than 20.000 Hz (20 kHz) [1••]. The frequency of diagnostic ultrasound is in the millions of Hertz (MHz), with lower frequency probes usually being 2 to 5 MHz and higher frequency probes around 6 to 13 MHz [19]. In typical ultrasonography, transducers (or probes) are composed of multiple “crystals” that generate sound waves which return and produce a current, thus both transmitting and receiving the sound. These then produce multiple scan lines to compose an image that is refreshed many times per second to create moving images on the screen [1••].
The three most common probe types are linear, curvilinear, and phased array. Each probe has a different frequency, which determines resolution of image but is inversely related to depth of probe penetration. Linear probes have a high frequency, allowing for excellent resolution of superficial structures, but the low penetration does not allow visualization of deeper structures. Linear probes are thus best used for superficial structures, such as for vascular access or more detailed lung pleural evaluation. Curvilinear and phased array probes, in contrast, are lower frequency (e.g., 2–5 MHz) but have high penetration, allowing visualization of deeper structures, such as for abdominal and cardiac exams. The phased array has a smaller probe footprint than the curvilinear probe, thus making it easier to obtain adequate views between ribs when doing lung or cardiac exams.
Terminology
The echogenicity of tissue refers to how well ultrasound waves penetrate through the tissue relative to surrounding tissues. A structure can be hyperechoic (white on the screen, relatively not well penetrated by ultrasound), hypoechoic (gray), or anechoic (black). Ultrasound penetrates well through solid organs (e.g., liver and spleen) and fluid, but it does not penetrate well through bone or air. Fluid such as blood, urine, and ascites thus often appear completely anechoic. In contrast, bone will have a bright hyperechoic rim, although it will also appear black or anechoic on ultrasound beyond the rim because the ultrasound beam cannot penetrate bone and thus casts an acoustic shadow beyond the surface of the bone [19]. Ultrasound is subsequently more challenging and limited in its use in bony regions such as the skull and chest, as well as in areas of the abdomen where bowel gas may obscure the image.
Depending on the probe position relative to the subject, various planes are made by the ultrasound beam: sagittal (longitudinal), transverse (axial), coronal (frontal), or a combination (oblique). A window refers to what the probe is looking through, or the location fo the ultrasound probe. Together, a window and plane create a view to describe a specific image. Probes often have indicators on one side to help orient the operator to the plane of the screen, although the side the indicator corresponds to varies with ultrasound machines and should always be double checked by the operator. For instance, in general imaging, the indicator often corresponds to the left side, although traditionally in echocardiography it typically correlates to the right [1••]. Various terminology is also used to describe movement of the probe, including sliding (moving the probe to a different place on the body, or “window shopping”), tilting (a rocking motion that moves the cord towards or away the probe’s indicator, thus finding different structures in the same plane), rotating (turning the probe around its central axis), and angling (side-to-side movement that creates new imaging planes parallel to the original plane). Once a view is obtained, parameters such as gain (displayed brightness) and depth can be adjusted to optimize the image on the screen.
Applications of Perioperative Point-of-Care Ultrasound
Focused Cardiac Ultrasound (FoCUS)
Indication
The focused cardiac ultrasound (FoCUS) is a valuable point of care tool for anesthesiologists and, in the perioperative setting, is most often used to help evaluate potential causes of hemodynamic instability or signs of heart failure in patient (Table 2). Distinct from transthoracic echo, in which extensive training is needed to analyze and interpret images in unlimited clinical settings, FoCUS is a focused cardiac exam using ultrasound as an adjunct to recognize specific ultrasound signs that suggest a narrower list of potential diagnoses in specific clinical settings [20]. Multiple studies have shown the feasibility and success of incorporating FoCUS into pre-, intra-, and post-operative settings for both elective and emergency settings, providing important insight that can significantly alter patient management.
Information that can be quickly include biventricular function, gross valvular abnormalities, pericardial effusions, wall motion abnormalities suggestive of ischemia, and surrogates of a patient’s volume status including inferior vena cava (IVC) collapsibility and ventricular size. Multiple cases have been reported showing the value of bedside cardiac ultrasound in allowing fast diagnoses and changes in intraoperative management, for instance revealing left ventricle (LV) inferior wall akinesis despite no electrocardiogram (EKG) changes suggestive of acute ischemia in a patient with sudden and profound hypotension at the end of a case [21] or showing an underfilled LV in a patient with hypertrophic cardiomyopathy despite adequate central venous pressure (CVP) readings [22].
FoCUS also holds promise as a useful diagnostic modality for pre-operative cardiac assessment. In patients who present preoperatively with limited or no exercise tolerance and an unclear cardiac history, FoCUS allows a quick assessment of basic cardiac function to help decide whether further evaluation by a cardiologist or with cardiac testing is warranted. Gerlach et al. [23], for instance, described how the preoperative FoCUS to determine volume status in a patient with known aortic stenosis who was scheduled to undergo elective endoscopic surgery revealed the patient to have cardiac tamponade that was not appreciated by physical or history. While not intended to replace current tools for assessing cardiac function, ultrasound can augment traditional diagnostic tools and exams that often miss important cardiac diagnoses [24, 25]. For instance, 12-lead EKGs identify less than 10% of patients with left ventricular hypertrophy [26]. Kobal et al. [27] also showed that compared to board-certified cardiologists using physical exam alone, first year medical students with minimal training for FoCUS far outperformed them in diagnosing cardiovascular diagnoses (75% vs. 49% accuracy). Similar studies also support that even with limited training, bedside cardiac ultrasound allows residents to more accurately identify pathologies such as systolic dysfunction [28, 29] and right atrial pressures [30].
Acquisition
FoCUS uses three windows (parasternal, apical, and subcostal) to produce four views of the heart: parasternal long axis, parasternal short axis, apical four chamber, subcostal four chamber (Fig. 1). An additional subcostal view of the long-axis IVC is often included in the FoCUS exam to assist with evaluation of volume status. While techniques and applications of FoCUS are described in excellent detail by Zimmerman and colleagues [9], we will summarize them below.
Patient Position
Because the heart lies obliquely in the chest, surrounded by ribs and lungs which are naturally impenetrable by ultrasound waves, obtaining clear views can be challenging. Patients can be examined in the supine position, but the left lateral decubitus position is preferred for parasternal and apical views as they bring the heart’s structures closer to the chest wall. If a patient is not able to be placed in full left lateral decubitus, even placing towels or pillows under their right side to tilt them slightly to the left may be beneficial. Furthermore, abduction of the left arm (e.g., asking patients to raise their left arm and rest it behind their head) helps increase the intercostal space, allowing less interference from the ribs in obtaining an adequate view.
Probe Selection
A phased array probe is a good choice for this exam, as it is lower frequency and deeper penetration allows visualization of cardiac structures while maintain a small “footprint” to use intercostal windows. While curvilinear probes have similar frequency ranges, their slightly larger size is less amenable to obtaining adequate views in the intercostal windows, but they may be useful in the subcostal view.
Interpretation
Basic Cardiac Function
Long- and short-axis views can be used to make a crude estimate as to LV ejection fraction. To assess RV size and function, the subcostal four-chamber view is the preferred view. In this view, the RV should be smaller than the LV, and the apex primarily comprised of the LV. If the RV is enlarged, it will appear in similar size to the LV or may to contribute to the apex. A “D sign” or flattening of the intraventricular septum in the parasternal short axis view also suggests high RV pressure and volume overload. Ultrasound visualization of global and regional function also allow quick assessment of possible ischemia. Parasternal views of the LV can, in most instances, help identify regions of the LV that are hypokinetic or akinetic, as it uniquely allows assessment of movement of each of the 6 segments that represent myocardial territories perfused by each of the 3 main coronaries.
Severe Valvular Abnormalities
FoCUS allows for gross assessment of valvular function. The parasternal long-axis view allows a quick, qualitative evaluation of mitral valve function including potential prolapse and flail. The subcostal four-chamber view is the preferred view for assessing the function and structure of tricuspid valve. The aortic valve should be well visualized in the parasternal long axis. If the valve opens poorly and appears heavily calcified, stenosis should be suspected.
Volume Status
The parasternal long- and short-axis views of the LV can also help provide a gross assessment of volume status, with a highly collapsible central cavity with near obliteration of the end-systole cavity, suggestive of significant intravascular depletion. Conversely, if the intraventricular septum (IVS) appears flat between the two ventricles in the parasternal short axis view, suspect RV overload.
Although controversial, IVC collapsibility, which can be visualized and measured in the subcostal window, has been used to evaluate central volume status. When scanning for the IVC, it is important to keep the RA on the screen so that a long-axis view of the IVC can be seen as it enters the RA, in order to prevent mistaking the aorta as the IVC. Visualizing hepatic veins as they enter the IVC also confirms which vessel is being visualized.
Pericardial Effusions
The subcostal view allows the easiest and most reliable detection of pericardial effusions because it provides visualization of the most dependent portions of the heart. Asking the patient to inspire deeply can bring the heart closer to the probe and provide improved visualization. Pericardial effusions can be seen along the heart, separating the aorta from the pericardium. In contrast, pleural effusions will accumulate posterior to the descending aorta.
Lung Ultrasound (LUS)
Indication
The use of bedside lung ultrasound (LUS) to evaluate for pulmonary disease is not a novel technique and has been used in critical care since the early 1990s [31], followed by the field of emergency medicine and more recently in perioperative settings by anesthesiologists. LUS is a valuable, effective, and accurate goal-directed diagnostic technique for real-time assessment of respiratory symptoms and signs (Table 3). Because of high ultrasound reflectivity of the air-tissue interface, the air-filled lung cannot be directly visualized and ultrasound does not allow direct evaluation of the normal pulmonary parenchyma. Somewhat paradoxically, however, the acoustic limitations of ultrasound in normal, air-rich lungs provides a diagnostic advantage, as the use of LUS relies on recognition of signs, artifacts, and patterns associated with certain pathologies that are definite and easily recognized [12••]. LUS has been thus shown to be easily learned, accurate, and reproducible [11••] and can help determine the etiology of hypoxia in over 90% of cases [32]. It can be an extremely valuable tool for the anesthesiologist, allowing evaluation of causes of hypoxia as well as acute hemodynamic instability (e.g., tension pneumothorax) much faster than traditional diagnostic tools and imaging.
Acquisition
A thorough review of lung ultrasound technique is described elsewhere [10, 11••, 12••] but summarized below.
Probe Selection
A high-frequency linear probe allows visualization of up to around 4 cm, which is adequate to examine the superficial pleural line and lung parenchyma. Because it offers the highest resolution for examining abnormal pleural surfaces, it is the probe of choice for evaluating pneumothoraxes or edema.
Lower frequency probes can be used to evaluate deeper, under-pleural artifacts such as effusions [33]. Although the phased array probe’s small footprint may be advantageous in evaluating the anterior chest because it allows a view in small intercostal spaces, it examines only a tiny field of the pleural surface and is thus prone to causing missed, localized pathology. However, it is a good choice for gross, diffuse pathology such as pulmonary edema or large effusions. The curvilinear probe is a low-frequency probe with good penetration and thus ideal when scanning the pleural surface for general pathology. It also allows adequate views of the costophrenic angle, liver, and diaphragm when looking evaluating for effusions.
Patient Position
Generally, patients are examined in the supine position. Probes are placed on the anterior to assess for non-dependent pathologies such as a pneumothorax, as this is where air in the pleural space will accumulate in a supine patient [33]. If a patient is in a semi-sitting position, for instance because of respiratory distress, the least-dependent area would be the apical region, although this is challenging and less accessible for imaging because of the clavicles. In contrast, the probe is placed in the posterolateral area of the chest if looking for more dependent pathology, such as consolidation, effusion, or hemothorax.
Interpretation
As mentioned above, ultrasound energy is rapidly dissipated by air and thus does not allow direct evaluation of normal lung parenchyma, instead relying on recognition of common sonographic signs including lung sliding, A-lines, lung point, lung pulse, and B-lines (Fig. 2). These are described below in relation to common lung pathologies.
Normal Lung
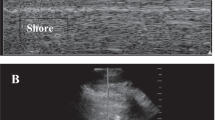
Normally, movement between visceral and parietal pleura results in a moving, shimmering pleural line known as lung sliding. Lung sliding at the parasternal areas rules out pneumothorax in the site of scanning with 100% negative predictive value [34, 35]. M-mode can be used to confirm a dynamic pleural line through distal artifacts in a granular pattern resembling sand on a beach, sometimes referred to as the “seashore sign”. In addition, hyperechoic, horizontal lines known as A-lines can be seen at regular intervals from the pleural line and represent reverberation artifacts in the air-filled lung. Together, A-lines and lung sliding represent an intact pleural line with normal content of air in the alveolar spaces (Fig. 2a).
Pneumothorax
A static pleural line suggests the absence of lung sliding, and in M-mode this is represented by a barcode appearance (Fig. 2b). Although the absence of lung sliding suggests possible pneumothorax, it is important to note that the lack of lung sliding and horizontal pleural movement can also be caused by adhesions, very low lung compliance, massive atelectasis, or in an apneic patient or main-stem intubation. Other signs like the lung pulse and B-lines, both described in more detail below, are artifacts which can only exist in the present of an intact visceral and parietal pleural, and thus their presence—even in the absence of lung sliding—rules out a pneumothorax at the scanned site [33, 34].
When this pattern suggests a pneumothorax (no lung sliding, lung pulse, or B-lines), the most definitive way to confirm the pneumothorax is to identify the lung point, or the dynamic transition point between normal, sliding lung and the absence of lung sliding. It is highly specific (98–100%) for diagnosing a pneumothorax [35, 36]. To find the lung point, the probe is gradually moved towards the lateral-inferior chest areas to find a point on the chest wall where there is re-visualization of a respiratory pattern (e.g., lung sliding) that is intermittently replaced by motionless pleura, corresponding to the edge of the intrapleural air layer. In M-mode, the lung point appears as an abrupt transition from a barcode appearance to the “seashore sign” (Fig. 2b).
Interstitial Syndrome and Edema
When the density of the lung tissue or air content changes, such as from exudate, transudate, collagen, or blood, the acoustic mismatch between the lung and surrounding tissues lowers and subsequently allows ultrasound beams to be repeatedly reflected at deeper zones. This causes artifacts known as B-lines, which are described as bright, hyperechoic, comet-tail signs that start at the pleural line and extend to the bottom of the ultrasound screen without fading (Fig. 2c). These artifacts obliterate normal A-line artifacts seen in lung and move with pleural siding [37]. While B-lines are often visualized in normal lung, three or more B-lines within the same intercostal space (one longitudinal scan) is considered a “positive B pattern” and suggests lung interstitial syndrome, with the number and diffusion of B line increases as fluid content increases [38].
If seen diffusely and homogenously across the anterior chest, cardiogenic pulmonary edema should be considered; in contrast, edema from acute lung injury or acute respiratory distress syndrome shows a more irregular pattern [12••]. B-lines may assist in the early detection of acute interstitial pulmonary edema, and they are highly sensitive for pulmonary edema but not specific, as B-lines may also represent changes in lung tissue from pathology such as pneumonia or pre-existing interstitial disease.
Atelectasis
The lung pulse refers to subtle, vertical movements of the pleura synchronous with cardiac beats, suggesting air in the lung but in a non-ventilated lung area, acting like a “bag full of air” receiving the transmitted “kicks” of the neighboring heart. For complete atelectasis, the lung pulse sign is reported to have sensitivity and specificity of 70–99% and 92–100%, respectively [39].
Consolidation
When the lung is highly fluid filled, it resembles the liver in echogenicity [12••]. In severe consolidation, a pleural effusion may be visualized at the lung base. Effusions are dependent and thus accumulate in the costophrenic angles, appearing as a hypoechoic “space” between the base of lung and diaphragm. A phased array probe can be used, allowing adequate penetration and depth to identify the liver, diaphragm, and lung bases, and placed in the posterolateral chest. Again, the probe marker should be directed cephalad.
Abdominopelvic Ultrasound
Indication
The focused assessment with sonography for trauma (FAST) is an application of POCUS that has been well-incorporated into the practice of emergency medicine, critical care, and surgery. Traditionally, the FAST exam is used in the setting of trauma to quickly identify free fluid suggestive of intraabdominal hemorrhage or free air suggestive of a ruptured viscus, as well as cardiac and lung views to look for pericardial or pleural effusions, respectively. Table 4 provides an overview of focused abdominopelvic ultrasound.
In the presence of intraabdominal bleeding in trauma and shock patients, FAST has proven to be extremely valuable tool, as in trauma and shock patients, the probability of death increases by approximately 1% for every 3 min that pass before treatment [40]. Studies have found that compared to abdominal CT scan, the sensitivity and specificity of FAST for detecting free fluid ranges from 64 to 98% and 86 to 100%, respectively [41, 42], and the average volume of fluid detectable by FAST ranging from 250 to 600 mL [43, 44].
For the anesthesiologist, similar views and concepts of the FAST exam can be used in the postoperative period for patients who decompensate after abdominal procedures, whether in the operating room, postoperative care unit, or intensive care unit. Using components of the FAST exam can help providers rapidly assess whether a patient’s evolving hemodynamic instability is due to intraabdominal hemorrhage or ruptured viscera. Furthermore, ultrasound allows not only fast identification of potentially life-threatening intraabdominal fluid but can also help guide the drainage of it, when applicable [45].
Acquisition
The components of the FAST most relevant for the anesthesiologist include three main ultrasound views that reveal spaces where fluid often accumulates in the abdomen and pelvis: (1) Right upper quadrant (RUQ) view to assess for fluid in the hepatorenal interface and subphrenic space, (2) left upper quadrant (LUQ) view to assess splenorenal interface and subphrenic space, and (3) pelvis view to assess the rectovesicular space and in female patients, the pouch of Douglas.
Patient Position
Patients are usually assessed in the supine position. To increase sensitivity of the RUQ and to some extent LUQ exam, patients can be placed in Trendelenburg in which gravity helps drive fluid up the pericolic gutters [46].
Probe Selection
A low-frequency probe, such as the curvilinear or phased array probes, is used to provide adequate tissue penetration.
Interpretation
Most relevant to the anesthesiologist is the use of the FAST views to assess for possible hemoperitoneum. The presence of anechoic fluid located in any potential space (hepatorenal, perisplenic, rectovesiular/pouch of Douglas) should raise concern for hemoperitoneum.
Given the tendency for fluid to collect in the RUQ, this view is usually obtained first. The RUQ view is both the most sensitive and easiest view for detecting hemoperitoneum [13]. In the absence of hemoperitoneum, the double density of the kidney is adjacent to the liver, with the absence of the potential hepatorenal space. In contrast, a positive scan would reveal anechoic (black) fluid pooling between the liver and kidney, creating a hepatorenal space. If a positive RUQ scan is found, no further abdominal imaging is necessary as hemoperitoneum has been confirmed. On the left side, the presence of the phrenicocolic ligament tends to direct free fluid to the subphrenic space rather than the splenorenal interface [13]. The space and identification of diaphragm can be challenging due to multiple artifacts. The kidney also sits higher on the left side than on the right, so structures are more cephalad and may require probe adjustments accordingly.
In the development of a hemoperitoneum, initial exams may be falsely negative as it takes time for fluid to collect. Sequential imaging is thus encouraged when there is a high suspicion for intraperitoneal fluid. Over time, blood that begins to coagulate may change from appearing anechoic to an iso- or hyperechoic.
The pelvic exam can be obtained in two different planes, with the probe either oriented horizontally or longitudinally. Image quality is optimized with an adequately filled bladder. The rectum and/or uterus is visualized deep to the bladder. Just as in the upper quadrant views, free fluid is seen as anechoic fluid and detected posterior to the bladder in males or in the pouch of Douglas in females.
Gastric Ultrasound
Indication
Aspiration remains a rare but serious anesthetic complication, contributing to up to 9% of all anesthetic-related deaths [47, 48]. Gastric content is one of the main risks for aspirations, thus resulting in development of guidelines for preoperative fasting. The current guidelines by the American Society of Anesthesiologists, for instance, recommend a minimum of 2 h fasting for clears, 6 h for a light meal or nonhuman milk, and 8 or more hours after a full meal. However, these guidelines are intended for healthy patients undergoing elective procedures, not patients with comorbidities that affect gastric emptying or volume, including pregnancy, obesity, diabetes, reflux, trauma, or bowel obstructions, or potentially challenging airways [49]. Point-of-care gastric ultrasound has subsequently gained increasing attention as a diagnostic tool to help assess gastric content type and volume and thus aspiration risk in various settings, such as elective procedures where NPO guidelines are not followed or in which it is unknown, or in high-risk patients despite appropriate NPO guidelines (e.g., recent trauma, diabetes, chronic opioid use, active labor) [16]. Visualization of the gastric antrum without evidence of solid or fluid content and a low cross-sectional area may, for instance, reassure physicians to proceed with sedation or LMA in emergent cases where NPO guidelines are not clearly met but comorbidities and/or coagulopathies make regional or general endotracheal anesthesia undesirable. On the other hand, it could also lead providers to choose to intubate with an endotracheal (ETT) rather than provide sedation or use of a supraglottic airway in a diabetic patient with severe gastric delay who, despite having followed NPO guidelines, may still have significant amount of contents visualized in the stomach on ultrasound. Perlas and colleagues have proposed a detailed framework for using bedside gastric ultrasound in such perioperative settings [16]. Table 5 shows basic principles of gastric ultrasound.
Acquisition
The gastric antrum, located superficially (approximately 3–4 cm) is most amenable to ultrasound examination and accurately reflects the contents of the entire stomach [15]. With a sagittal scan in the epigastric region at the left subcostal margin and fanning past midline to the right subcostal region, the gastric antrum should be visualized as a hollow viscus with a prominent muscular wall, positioned between the left lobe of the liver and pancreas.
Patient Position
Patients may be positioned supine, semi-sitting, or in right lateral decubitus. The most reliable exam is obtained in the right-lateral decubitus position as contents will gravitate to the antrum in this position; an empty stomach cannot be based on a scan in the supine position alone [50].
Probe Selection
A low frequency, high penetration curvilinear probe is needed to identify relevant anatomic landmarks in adults. A linear, high-frequency probe may be used for children [16]. Probe positioning for various ultrasound exams is shown in Fig. 3.
Interpretation
Baseline gastric secretions and clear fluids (water, apple juice, black coffee) appear hypo- or anechoic. As gastric volume increases, the antrum becomes rounder and distended with thinner walls. Thicker fluids such as milk have increased echogenicity. After a solid meal, a “frosted glass” pattern may form due to food and air mixed with chewing and swallowing. This air/solid mixture creates multiple artifacts that may blur the posterior wall of the antrum and create a shadowing effect. Ultrasound can also show peristaltic gastric contractions which may suggest more recent oral intake.
Several studies have shown that the antral cross-sectional area (CSA) derived from sonography correlate with total volume of gastric volume [15] and can further define aspiration risk [51, 52]. The use of ultrasound and CSA to grade aspiration risk is more thoroughly described in a review by Van de Putte [16] and Perlas [15]. Although studies have shown these to be accurate and reliable [51, 52], as a relatively newer application of perioperative ultrasound, more studies are needed to better characterize the reliability as well as sensitivity and specificity for differentiating between different types of gastric content (e.g., empty, clear fluid, solids).
Airway Management
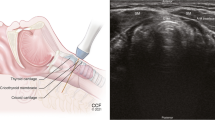
Endotracheal (ETT) Placement and Confirmation
Many proposed models of perioperative POCUS include the role of ultrasound for confirmation of ETT placement [2, 8••], either in real time imaging over the neck during intubation, or secondarily by detection of ventilation with signs of lung sliding or diaphragmatic movement. These studies have primarily been done for intubations in the emergency room rather than in the operating room, as the use of ultrasound for ETT confirmation would be most beneficial where capnography is not immediately available or noise prevents auscultation such as emergency room or pre-hospital settings.
Direct ultrasound confirmation of tracheal intubation is inferred from a single, hyperechoic air-mucosal interface (the trachea), whereas esophageal intubation creates two (both trachea and esophagus), or the “double tract sign.” This approach has shown comparable sensitivity and specificity to waveform capnography and clinical exam [53,54,55,56]. One meta-analysis that included 11 trials (n = 969 intubations) and reported both sensitivity and specificity of 98% [57]. Chou et al. also included cadaveric studies (n = 1656 intubations) with reported sensitivity and specificity of 93% and 97%, respectively [55]. Furthermore, because the patient’s lungs must be ventilated several times to confirm with capnography, transtracheal ultrasound allows for fast confirmation [53, 58, 59] and is as fast as auscultation alone, and faster than standard auscultation and capnography [60, 61].
Confirmation of ETT can also be done indirectly through identifying signs of lung ventilation including lung-sliding [62,63,64] and diaphragmatic motion through a subcostal view [65]. For secondary confirmation, bilateral assessment is important to avoid missing a mainstem intubation, and the patient cannot be spontaneously breathing. Table 6 summarizes basic principles of trancheal ultrasound.
Lung Isolation
Observing lung sliding has also been utilized to assist with confirmation of lung isolation in several studies. Although one lung ventilation is typically assessed by direct visualization of tube placement by flexible bronchoscopy, Saporito et al. [66] (n = 51) demonstrated that ultrasound and bronchoscopy yielded identical results with the exception of one case with inadequate windows for ultrasound assessment. Ultrasound has also been shown to be superior to clinical exam alone [67, 68]. In a study by Ramsingh et al. [68], single-lumen ETTs were placed into either the trachea, right mainstem, or left mainstem under bronchoscopic guidance (n = 42), and blinded assessors determined tube position either with ultrasound or auscultation. The authors found that the use of ultrasound had a sensitivity and specificity of 93% and 96%, respectively, compared to 66% and 59% for auscultation. Alvarez-Diaz et al. [67] similarly found sensitivity and specificity of US to be 98% and 53%, superior to 85% and 41% with clinical assessment alone.
Additional Airway Uses
As anesthesiologists become more trained in whole-body ultrasound, POCUS of the airway may continue to develop. It has been suggested ultrasound can provide a non-invasive version of the Cormack-Lehane classification as it has been shown to have a significant correlation between ultrasound evaluation and the epiglottis and vocal cords distance and may supplement current noninvasive modalities of pre-anesthetic airway assessment, such as the Mallampati Classification [69]. However, evidence for the ability to predict a difficult airway is inconsistent [70, 71]. Ultrasound may be useful to evaluate pathology affecting airway management such as laryngeal stenosis or cysts [17]. Using ultrasound to measure the width of the base of tongue has also been shown to predict severity of obstructive sleep apnea (OSA) [72]. Ultrasound can also be of use intraoperatively to perform airway nerve blocks, locate the cricothyroid membrane for emergency tracheostomy [73] and predict appropriate diameter for ETT through measurement of subglottic diameter [74]. Postoperatively, it can also be used to assess for subglottic edema [18], for instance in a patient with increasing postoperative distress. The use of POCUS for these and other topics in airway management is described more thoroughly by Kristensen [17] and Votruba and colleagues [18].
Conclusion
Applications of POCUS should be focused, goal-oriented, easily learned, rapidly performable at bedside, accurate, and reliable. As reviewed above, a variety of studies have shown this potential for POCUS in assessing cardiac, pulmonary, and intraabdominal pathologies, making it an emerging area of interest in medicine. The incorporation of point-of-care ultrasound into perioperative medicine is an important advancement in the field of anesthesiology, providing us with an important adjunct and tool to ensure our continued improvement in coordinating care for patients in the perioperative period.
Critical to the effective and safe use of this powerful diagnostic tool is, however, proper training. User dependence is an important limitation of the use of POCUS by anesthesiologists, with concerns that image misinterpretation may result in incorrect assessment or treatment. As ultrasound is likely the most operator-dependent of all imaging modalities [75], the limited training for POCUS among anesthesiology trainees must be addressed. Currently, there is no standard ultrasound curriculum for anesthesiology residents, and teaching methods vary from informal bedside teaching, structured expert demonstration, didactic lectures, and simulations [76]. Further barriers to training may include limited time and comfort of educators themselves with the recently emerging applications of POCUS. However, many have started sharing their experiences with pilot curriculums in anesthesiology trainees, providing insight to help other programs create their own curriculums. For instance, groups have found that model/simulation-based lecture series are likely to be more effective in teaching ultrasound to anesthesiology residents [77], and that e-learning and traditional didactics are both equally effective in teaching POCUS applications such as LUS and FAST [78, 79]. Creating protocol-guided frameworks for POCUS, such as I-AIM (indication, acquisition, interpretation, medical decision making), can also ensure more consistent and reliable diagnoses and interpretations of findings [16, 75] and should thus be further developed and widely taught. Standardized, national curriculums or workshops that expose anesthesiologists of all levels to these would be beneficial.
Abbreviations
- POCUS:
-
Point of care ultrasound
- MHz:
-
Millions of Hertz
- FoCUS:
-
Focused cardiac ultrasound
- IVC:
-
Inferior vena cava
- LV:
-
Left ventricle
- EKG:
-
Electrocardiogram
- CVP:
-
Central venous pressure
- RV:
-
Right ventricle
- LUS:
-
Lung ultrasound
- FAST:
-
Focused assessment with sonography for trauma
- RUQ:
-
Right upper quadrant
- LUQ:
-
Left upper quadrant
- CSA:
-
Cross-sectional area
- OSA:
-
Obstructive sleep apnea
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–57 (excellent review of point-of-care ultrasonography).
Mahmood F, Matyal R, Skubas N, Montealegre-Gallegos M, Swaminathan M, Denault A, et al. Perioperative ultrasound training in anesthesiology: a call to action. Anesth Analg. 2016;122(6):1794–804.
Ramsingh D, Rinehart J, Kain Z, Strom S, Canales C, Alexander B, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology. 2015;123(3):670–82.
Nomura T, Watanabe I. Pre-anesthetic whole body point-of-care ultrasonography. Masui. 2017;66(5):522–9.
Kobal SL, Lior Y, Ben-Sasson A, Liel-Cohen N, Galante O, Fuchs L. The feasibility and efficacy of implementing a focused cardiac ultrasound course into a medical school curriculum. BMC Med Educ. 2017;17(1):94.
Conlin F, Roy Connelly N, Raghunathan K, Friderici J, Schwabauer A. Focused transthoracic cardiac ultrasound: a survey of training practices. J Cardiothorac Vasc Anesth. 2016;30(1):102–6.
Haskins SCV, Ansara M, Garvin S. Perioperative point-of-care ultrasound for the anesthesiologist. Journal of Anesthesia and Perioperative Medicine. 2018;5(2):92–6.
•• Deshpande R, Ramsingh D. Perioperative point of care ultrasound in ambulatory anesthesia: thinking beyond nerve blocks. Curr Opin Anaesthesiol. 2017;30(6):663–9 (excellent review of point-of-care ultrasonography).
Zimmerman JM, Coker BJ. The nuts and bolts of performing focused cardiovascular ultrasound (FoCUS). Anesth Analg. 2017;124(3):753–60.
Sera M. Point-of-care lung ultrasound. Masui. 2017;66(5):493–502.
•• Goffi A, Kruisselbrink R, Volpicelli G. The sound of air: point-of-care lung ultrasound in perioperative medicine. Can J Anaesth. 2018;65(4):399–416 (excellent review of point-of-care ultrasonography).
•• Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014;12:25 (excellent review of lung ultrasound).
Pace J, Arntfield R. Focused assessment with sonography in trauma: a review of concepts and considerations for anesthesiology. Can J Anaesth. 2018;65(4):360–70.
Manson WC, Kirksey M, Boublik J, Wu CL, Haskins SC. Focused assessment with sonography in trauma (FAST) for the regional anesthesiologist and pain specialist. Reg Anesth Pain Med. 2019;44(5):540–8.
Perlas A, Davis L, Khan M, Mitsakakis N, Chan VW. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg. 2011;113(1):93–7.
Perlas A, Van de Putte P, Van Houwe P, Chan VW. I-AIM framework for point-of-care gastric ultrasound. Br J Anaesth. 2016;116(1):7–11.
Kristensen MS. Ultrasonography in the management of the airway. Acta Anaesthesiol Scand. 2011;55(10):1155–73.
Votruba J, Zemanova P, Lambert L, Vesela MM. The role of airway and endobronchial ultrasound in perioperative medicine. Biomed Res Int. 2015;2015:754626.
Ihnatsenka B, Boezaart AP. Ultrasound: basic understanding and learning the language. Int J Shoulder Surg. 2010;4(3):55–62.
Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26(6):567–81.
Augoustides JG, Hosalkar HH, Savino JS. Utility of transthoracic echocardiography in diagnosis and treatment of cardiogenic shock during noncardiac surgery. J Clin Anesth. 2005;17(6):488–9.
Ferguson EA, Paech MJ, Veltman MG. Hypertrophic cardiomyopathy and caesarean section: intraoperative use of transthoracic echocardiography. Int J Obstet Anesth. 2006;15(4):311–6.
Gerlach RM, Saha TK, Allard RV, Tanzola RC. Unrecognized tamponade diagnosed pre-induction by focused echocardiography. Can J Anaesth. 2013;60(8):803–7.
McGee S, Abernethy WB 3rd, Simel DL. The rational clinical examination. Is this patient hypovolemic? JAMA. 1999;281(11):1022–9.
Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007;297(16):1810–8.
Levy D, Labib SB, Anderson KM, Christiansen JC, Kannel WB, Castelli WP. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation. 1990;81(3):815–20.
Kobal SL, Trento L, Baharami S, Tolstrup K, Naqvi TZ, Cercek B, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002–6.
Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319–24.
Panoulas VF, Daigeler AL, Malaweera AS, Lota AS, Baskaran D, Rahman S, et al. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging. 2013;14(4):323–30.
Brennan JM, Blair JE, Goonewardena S, Ronan A, Shah D, Vasaiwala S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–6.
Lichtenstein D, Axler O. Intensive use of general ultrasound in the intensive care unit. Prospective study of 150 consecutive patients. Intensive Care Med. 1993;19(6):353–5.
Lichtenstein DA, Meziere GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134(1):117–25.
Volpicelli G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011;37(2):224–32.
Lichtenstein DA. Ultrasound in the management of thoracic disease. Crit Care Med. 2007;35(5 Suppl):S250–61.
Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding Chest. 1995;108(5):1345–8.
Lichtenstein D, Meziere G, Biderman P, Gepner A. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25(4):383–8.
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–91.
Volpicelli G, Caramello V, Cardinale L, Mussa A, Bar F, Frascisco MF. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008;26(5):585–91.
Lichtenstein DA, Lascols N, Prin S, Meziere G. The “lung pulse”: an early ultrasound sign of complete atelectasis. Intensive Care Med. 2003;29(12):2187–92.
Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma. 2002;52(3):420–5.
Korner M, Krotz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current role of emergency US in patients with major trauma. Radiographics. 2008;28(1):225–42.
Akdemir HU, Caliskan F, Kati C, Baydin A. The blunt abdominal trauma bedside ultrasonography comparison with trauma severity scores and computerized tomography. J Coll Physicians Surg Pak. 2019;29(7):621–5.
Branney SW, Wolfe RE, Moore EE, Albert NP, Heinig M, Mestek M, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39(2):375–80.
Paajanen H, Lahti P, Nordback I. Sensitivity of transabdominal ultrasonography in detection of intraperitoneal fluid in humans. Eur Radiol. 1999;9(7):1423–5.
Sharma A, Bhattarai P, Sharma A. eFAST for the diagnosis of a perioperative complication during percutaneous nephrolithotomy. Crit Ultrasound J. 2018;10(1):7.
Abrams BJ, Sukumvanich P, Seibel R, Moscati R, Jehle D. Ultrasound for the detection of intraperitoneal fluid: the role of Trendelenburg positioning. Am J Emerg Med. 1999;17(2):117–20.
Shime N, Ono A, Chihara E, Tanaka Y. Current status of pulmonary aspiration associated with general anesthesia: a nationwide survey in Japan. Masui. 2005;54(10):1177–85.
Lienhart A, Auroy Y, Pequignot F, Benhamou D, Warszawski J, Bovet M, et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105(6):1087–97.
Anesthesiologists ASo. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. Anesthesiology. 2017;126(3):376–93.
Carp H, Jayaram A, Stoll M. Ultrasound examination of the stomach contents of parturients. Anesth Analg. 1992;74(5):683–7.
Bouvet L, Mazoit JX, Chassard D, Allaouchiche B, Boselli E, Benhamou D. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume. Anesthesiology. 2011;114(5):1086–92.
Perlas A, Mitsakakis N, Liu L, Cino M, Haldipur N, Davis L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination. Anesth Analg. 2013;116(2):357–63.
Thomas VK, Paul C, Rajeev PC, Palatty BU. Reliability of ultrasonography in confirming endotracheal tube placement in an emergency setting. Indian J Crit Care Med. 2017;21(5):257–61.
Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49(1):75–80.
Chou EH, Dickman E, Tsou PY, Tessaro M, Tsai YM, Ma MH, et al. Ultrasonography for confirmation of endotracheal tube placement: a systematic review and meta-analysis. Resuscitation. 2015;90:97–103.
Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the confirmation of endotracheal tube intubation: a systematic review and meta-analysis. Ann Emerg Med. 2018;72(6):627–36.
Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anaesth. 2015;62(4):413–23.
Hoffmann B, Gullett JP, Hill HF, Fuller D, Westergaard MC, Hosek WT, et al. Bedside ultrasound of the neck confirms endotracheal tube position in emergency intubations. Ultraschall Med. 2014;35(5):451–8.
Saglam C, Unluer EE, Karagoz A. Confirmation of endotracheal tube position during resuscitation by bedside ultrasonography. Am J Emerg Med. 2013;31(1):248–50.
Pfeiffer P, Rudolph SS, Borglum J, Isbye DL. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand. 2011;55(10):1190–5.
Pfeiffer P, Bache S, Isbye DL, Rudolph SS, Rovsing L, Borglum J. Verification of endotracheal intubation in obese patients - temporal comparison of ultrasound vs. auscultation and capnography. Acta Anaesthesiol Scand. 2012;56(5):571–6.
Chun R, Kirkpatrick AW, Sirois M, Sargasyn AE, Melton S, Hamilton DR, et al. Where’s the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med. 2004;19(4):366–9.
Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13(3):239–44.
Lyon M, Walton P, Bhalla V, Shiver SA. Ultrasound detection of the sliding lung sign by prehospital critical care providers. Am J Emerg Med. 2012;30(3):485–8.
Hosseini JS, Talebian MT, Ghafari MH, Eslami V. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci. 2013;3(2):113–7.
Saporito A, Lo Piccolo A, Franceschini D, Tomasetti R, Anselmi L. Thoracic ultrasound confirmation of correct lung exclusion before one-lung ventilation during thoracic surgery. J Ultrasound. 2013;16(4):195–9.
Alvarez-Diaz N, Amador-Garcia I, Fuentes-Hernandez M, Dorta-Guerra R. Comparison between transthoracic lung ultrasound and a clinical method in confirming the position of double-lumen tube in thoracic anaesthesia. A pilot study. Rev Esp Anestesiol Reanim. 2015;62(6):305–12.
Ramsingh D, Frank E, Haughton R, Schilling J, Gimenez KM, Banh E, et al. Auscultation versus point-of-care ultrasound to determine endotracheal versus bronchial intubation: a diagnostic accuracy study. Anesthesiology. 2016;124(5):1012–20.
Gupta D, Srirajakalidindi A, Ittiara B, Apple L, Toshniwal G, Haber H. Ultrasonographic modification of Cormack Lehane classification for pre-anesthetic airway assessment. Middle East J Anaesthesiol. 2012;21(6):835–42.
Komatsu R, Sengupta P, Wadhwa A, Akca O, Sessler DI, Ezri T, et al. Ultrasound quantification of anterior soft tissue thickness fails to predict difficult laryngoscopy in obese patients. Anaesth Intensive Care. 2007;35(1):32–7.
Ezri T, Gewurtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58(11):1111–4.
Lahav Y, Rosenzweig E, Heyman Z, Doljansky J, Green A, Dagan Y. Tongue base ultrasound: a diagnostic tool for predicting obstructive sleep apnea. Ann Otol Rhinol Laryngol. 2009;118(3):179–84.
Nicholls SE, Sweeney TW, Ferre RM, Strout TD. Bedside sonography by emergency physicians for the rapid identification of landmarks relevant to cricothyrotomy. Am J Emerg Med. 2008;26(8):852–6.
Lakhal K, Delplace X, Cottier JP, Tranquart F, Sauvagnac X, Mercier C, et al. The feasibility of ultrasound to assess subglottic diameter. Anesth Analg. 2007;104(3):611–4.
Brandli L. Benefits of protocol-driven ultrasound exams. Radiol Manage. 2007;29(4):56–9.
Mok D, Schwarz SKW, Rondi K. Point-of-care ultrasonography in Canadian anesthesiology residency programs: a national survey of program directors. Can J Anaesth. 2017;64(10):1023–36.
Ramsingh D, Alexander B, Le K, Williams W, Canales C, Cannesson M. Comparison of the didactic lecture with the simulation/model approach for the teaching of a novel perioperative ultrasound curriculum to anesthesiology residents. J Clin Anesth. 2014;26(6):443–54.
Haskins SC, Feldman D, Fields KG, Kirksey MA, Lien CA, Luu TH, et al. Teaching a point-of-care ultrasound curriculum to anesthesiology trainees with traditional didactic lectures or an online E-learning platform: a pilot study. J Educ Perioper Med. 2018;20(3):E624.
Edrich T, Stopfkuchen-Evans M, Scheiermann P, Heim M, Chan W, Stone MB, et al. A comparison of web-based with traditional classroom-based training of lung ultrasound for the exclusion of pneumothorax. Anesth Analg. 2016;123(1):123–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Linda Li, R. Jason Yong, and Richard D. Urman declare no conflict of interest. Alan Kaye is a Section Editor for Current Headache and Pain Reports. He has not been involved in the editorial handling of this manuscript. Dr. Kaye is also a speaker for Merck.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Li, L., Yong, R.J., Kaye, A.D. et al. Perioperative Point of Care Ultrasound (POCUS) for Anesthesiologists: an Overview. Curr Pain Headache Rep 24, 20 (2020). https://doi.org/10.1007/s11916-020-0847-0
Published:
DOI: https://doi.org/10.1007/s11916-020-0847-0