Abstract
Purpose of review
Despite the accumulation of a significant amount of data on pediatric headache, few studies have been conducted on its occurrence in children under 7 years of age. Within primary headaches in this age, migraine especially, turns out to be a disorder affecting up to 4% of the general population. An underestimate of its true prevalence can be due to lack of specific diagnostic markers, the frequent difficulty of describing pain in childhood, and the necessity of reliable parents’ reports. Thus, migraine in children under 7 years of age represents an important challenge for clinicians. The objective of this manuscript is to provide a comprehensive review of epidemiologic, clinic, and therapeutic aspects of migraine in this age.
Recent findings
Current literature data show that migraine has some differences, especially in clinical and therapeutic terms, in this age group compared to subsequent ages. Furthermore, some evidences showing that an early onset of migraine may play an unfavorable role in its natural history, suggest an early identification and management of migraine in younger children. Moreover, we highlight the role that factors of prenatal and perinatal development can play in the predisposition and anticipation of migraine onset. Finally, open questions related to the several undefined features of migraine in this age are reported.
Summary
Migraine in this pediatric population is absolutely not rare, represents an importan clinical challenge and probably has a negative predictive role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is a common and crippling neurological disorder in pediatric population [1, 2], with limited description in children under 7 years of age [3•], although a fair group of subjects were included in old studies [4]. Nevertheless, few studies have reported careful description of clinical, prognostic, and therapeutic features of migraine under 7 years of age [5,6,7,8,9,9, 10•, 11,12,13,14,15,16,17]. In this age as well as in general population, some recent studies [18, 19] show an increased disability from primary headaches, and especially migraine. Thus, this evidence rises questions concerning clinical different phenotypes, new treatments, and prognosis in children. The new classification [20] does not provide any diagnostic criteria for migraine specifically referred to the pediatric population, except for the reduced duration of the attack from 4hours to 2 hours, while biological data shows that important changes happen in the maturation of the brain from newborn to the adolescence and then adult age [21, 22]. The rarity of studies on headaches in prescholar age probably depends on the difficulty that children experience to describe painful sensations, along with the “mythological” idea that primary headaches were typically well identified in scholar age children or adolescents only. This wrong assumption recalls the previous idea that migraine should affect only adult fertile woman [3•]. Furthermore, the lack of interest from pharmaceutical industry, the perception of being an uncommon and not life-threatening disorder, the prevailing interpretation of headache as secondary to a stressful life change or other conditions (fever, allergy, visual acuity defect), or refusal to go to kindergarten or school, as well as a mother’s fear to treat pharmacologically the child with migraine [3•, 23], have made difficult to promote clinical researches in very young children.
It is really surprising that recent Pubmed search results show just over a dozen studies on headaches in preschoolers compared to the thousands of papers published in the last 30 years on headache in school age children and adolescents [3•].
However, since studies on the maturation of the nervous system demonstrate that all anatomical and functional structures responsible for the expression and features of pain are already developed in infancy, is clear that a child under 7 years of age can suffer from almost all types of primary headache.
In this review, we focus on migraine considered as the primary headache most frequently responsible for emergency and pediatrics departments accesses in developmental age.
Epidemiology of Migraine in Children Under 7 Years of Age
Despite the rarity of epidemiological studies, primary headache in preschoolers is not numerical irrelevant, with a prevalence ranging from around 6 to 30% of the population in this age group [24]. In a Finnish retrospective study, the cumulative incidence of headache was 4.3% at 3 years and progressed to 21.9% at 5 years [25]. A prospective study on the headache in general population aged 0 to 5 years showed an overall frequency of 19.5%. Specifically, headache was highly frequent in 0.5%, quite frequent in 0.5% and 4.3%, and in infrequent 14.5% [26].
Considering the various types of headache, it has been reported a prevalence of migraine between 1.4 and 3.2%, chronic daily headache about 0.2%, while there are no data on episodic tension headache [24].
Interestingly, a prevalence of about 30% of secondary headache has been reported at the age of 7 years [25], followed by a progressive reduction of prevalence up to 10–15% at 50 years of age, and a further increasing in the elderly [27].
Since the risk of secondary headaches is increased in the preschool population, a high level of clinical vigilance is required especially under 6 years of age.
Mortimer et al. [28] showed that 12% of children under 5 years (12% males, 11% females), complained of almost one attack of headache monthly, with migraine ranging between 1 and 2% under 5 years and increased to 4.3% in males and 1.2% in females, between 5 and 7 years of age. Interestingly, in this study, the authors, although adopting different criteria (AD Hoc Committee, Valhquist and IHS criteria of the 1th IHS classification) to define the prevalence of migraine, did not found any important difference [28].
Abu-Arafeh and Russell [2] estimated a prevalence of migraine of 3.4%, 7.5%, and 3.5% at 5, 6, and 7 years of age respectively with a mild prevalence in males.
A German study on a sample of selected preschool children aged 5–7 years [29] showed that about 52.4% reported episodes of headache associated with abdominal pain (48.8%), while 3.6% had recurrent headaches with a male to female ratio of 10:1. Unfortunately, the distribution of headache type according to the age was not reported. Arruda et al. [1] in a study in a Brazilian pediatric population estimated in the groups under 6 years and up to 7 years, an overall prevalence of migraine with or without aura of 5.46%, chronic migraine of 1.79%, probable migraine up to 29.33%, infrequent tension episodic headache up to 3.01%, frequent tension episodic headache up to 2.37%, and probable tension headache up to 12.61% (also in this study, there are no distribution according age 0–7, but only < 6 and < 7 years old). Actually, there are no other epidemiological studies that explore the prevalence of the different headache types in preschoolers and in all the studies conducted in evolutive age, the distribution of migraine in the 0–7-year range is not reported. Main epidemiological data on migraine under 7 years are reported in Table 1.
In conclusion, from an epidemiological point of view, we can affirm that headache in preschoolers is not uncommon, migraine type headache is well represented, and even a chronic daily headache may be reported.
Reported Headache Distribution in Preschoolers’ Clinical Series
Only few clinical series aiming to describe both the primary headaches and the prevailing type of secondary headaches in preschoolers have been published [6, 7, 9, 13, 16, 30], although in 1880, a study on headache already included about 30% of patients aged below 7 years [4].
A brief review of the few studies conducted before the adoption of the 1st IHS classification (1988), highlighted that they were conducted on very small samples and furthermore, often including older subjects [31].
Until a few years ago, a unique study on chronic and/or recurrent headache in a large sample was available [30]. It was a retrospective one and involved 104 subjects whose headaches began before the seventh year of age. In this study, 75% of patients presented with a type of migraine (using pre-IHS criteria), 12% with a post-traumatic headache, 2% with tension headaches, 2% with psychogenic forms, 1% with not specified vascular headaches, and 9% with unclassifiable headaches. This large study in comparison with other studies brought important epidemiological data. Indeed, migraine is widely represented, while episodic and chronic tension headaches are quite rare, similarly to other forms of primary headaches, and secondary headaches are represented by post-traumatic headache only.
This study [30] had some methodological peculiarities because conducted on a sample of subjects observed by a neurologist before the completion of 10 years and whose headaches began before 7 years. Thus, the chosen sample selection could have been responsible for a bias consisting in an increased rate of headaches with greater persistence and intensity over the time.
The study by Chu and Shinnar [30] indeed showed some distortions in the prevalence and distribution of chronic and most frequently recurring headaches; moreover, they adopted diagnostic criteria pre-IHS classification, making more difficult the comparison with subsequent studies.
In the last 15 years have been published [6, 7, 9, 13, 15, 16] several studies reporting the different distribution of headaches subgroups. Migraine and tension headache were the most frequent [6, 7, 9, 13, 16], primary stabbing headache was more reported in comparison to later ages [7, 9], and the prevalence of non-classifiable headaches was not negligible, ranging from 9 to 25% [7, 13, 15, 16]. Moreover, in a study, we confirmed that even at this age, secondary headaches are frequent (about 26%) and could be dangerous [7]. Recent studies on headaches in preschoolers [17, 32, 33] showed that they are an increasing reason for emergency and pediatrics departments accesses, and related healthcare costs consequent to induced concerns in health professionals [33].
However, these first reports suggest that also in presence of red flags, the prevalence, in this subgroup of dangerous headaches, remains low [17].
Neuroanatomical and Functional Development of Nervous System Pathways and Neurotransmitters Involved in Migraine
In clinical practice, the term gestational age (GA) is computed in weeks of gestation (WG), starting from the first day of the woman’s last menstrual cycle, while conception takes place about two weeks after GA and defines the conceptional age (CA). Since in studies on embryo-fetal development is universally preferred the term GA, in this review, we have adopted GA and WG to define the developmental age of the embryo-fetal pathways involved in migraine.
Neurofunctional pathways involved in migraine can be recognized from 8 weeks of gestation (WG) with trigeminal free sensory nerve endings reaching the oral mucosa and then the facial epithelium. Vibratory sensory receptors, eliciting the sucking reflex, are identifiable in the lips at 12 WG. Neurochemical maturation involved in pain perception is characterized by appearance in dorsal horns of substance P (SP), acetylcholinesterase and enkephalin at 5–7 WG, prostaglandins, somatostatin and neuronal nitric oxide synthase from the 8 WG. Serotoninergic neurons are present in the dorsal raphe nucleus from 10 WG. Granular vesicles containing catecholamines in the neuronal bodies of the locus coeruleus are present at 11 WG and neuropeptides including enkephalin gain the brainstem nuclei at 11–12 WG. Neuropeptide Y, involved in the descending pain modulation pathway, is identifiable in spinal cord at 12 WG, and at 14 WG spinal cord cell differentiation in the dorsal horn is associated with the synthesis of GABA and glutamate, both characterized at this stage of development by an excitatory effect [34, 35].
The centromedian nucleus of thalamus differentiates from intralaminar nuclei between 10 and 14 WG. Thalamic nuclei are involved in sensory integration, behavioral state regulation, and connected to the limbic cortex (entorhinal and cingulate cortices) for emotional aspects of pain perception. The first neural connection between monoaminergic fibers originating from brainstem and subplate takes place at 16 WG [36]. The periaqueductal gray matter (PAG) of the midbrain is involved in the supraspinal modulation of primary nociceptive input. Serotoninergic and opioid receptors have been demonstrated by 22 WG with subsequent different changes in binding. Serotonin receptors show an important decrease of binding between fetal and neonatal age as well as between neonatal and adult age, while opioid receptor binding (3H-naloxone) remains relatively constant from fetal to neonatal life and increases slightly to adult life [37]. Thalamic projections to the cortical plate, formed at 23 WG, allow the fetus to feel pain, also if not yet myelinated [36]. Allodynia, hyperalgesia, and central sensitization (hypersensitivity) are active from the 24 WG in relation to behavioral pain expression that the extremely preterm newborn is already able to perform in case of stimulation near injured areas of the body. Myelination of nociceptive pathways to the brainstem and thalamus is completed by 36 WG, and thalamocortical connections are myelinated at 40 WG [36].
Thus, in the last years, the increased awareness that from the first epochs of life early pain experiences are fully effective and could exert deleterious effects on the development of behavioral and emotional regulation has profoundly modified the management strategies especially in the neonatal intensive care units (NICU) [37]. In the early stage of development, neuropeptides and related receptors involved in migraine can even affect vital functions.
In newborn, an elevated circulating CGRP has been described in umbilical cord and infant blood in association with maternal and neonatal sepsis and shock, being then considered a reliable marker of inflammation and hemodynamic imbalance [38]. In early infancy, an important role of SP and its tachykinin neurokinin-1 receptor (NK1R) has been shown in the modulation of homeostatic function in brainstem, including regulation of respiratory rhythm generation, integration of cardiovascular control, modulation of the baroreceptor reflex, and mediation of the chemoreceptor reflex in response to hypoxia. Abnormalities in the SP neurokinin-1 receptor have been recently involved in sudden infant death syndrome [39].
Risk Profiles for Potential Subsequent Early Development of Migraine
Migraine onset in childhood could be related to both individual genetic and acquired determinants. Familiarity is a well-known risk factor for migraine, with a higher prevalence of migraine familiarity (70%) observed in comparison to episodic tension headache [7], while gender mainly influences the clinical phenomenology of migraine [40]. Exploring the individually acquired determinants, early exposure to pain experience could play an important role. Nociceptive neuronal circuits develop during embryonic and postnatal periods and, when excessive noxious stimuli are normally absent or rare, a normal neurofunctional development should be expected. Studies performed in animal [41] and human [42] have demonstrated that an immature organism excessively exposed to environmental stimuli or stress during a phase of rapid brain growth may be particularly sensitive to the effects of a dysfunctional pain processing, resulting in a detrimental effect on the developing dynamic pain connectome with permanent alteration of pain circuitry.
Early pain experiences characterize newborns admitted in Neonatal Level II and III Care Units owing to prematurity or perinatal adverse events. Prematurity, defined as a birth that occurs before 37 completed GW, involves 5 to 18% of births worldwide, with variable outcomes in terms of concomitant complications and developmental impairments. Prenatal and perinatal adverse events, mainly hypoxic, involve up to 8/1000 newborns, with variable degree of neonatal encephalopathy as well as multisystemic involvement. These complications might alter the programming of neurotransmitters and receptors expression, potentially leading to long-term effects [43]. Recent experimental findings show how even an intrauterine mild hypoperfusion can lead to an increase in glutamate release in adult rats along with a reduction in GABAergic levels, suggestive of hyperexcitability in the hind paw area of the sensorimotor cortex [44].
Newborn admitted in NICU are exposed to several persistent painful experiences varying from repeated heel lance to more invasive procedures as surgery and mechanical ventilation, and neonatal pain assessment techniques routinely available to neonatologists consist of behavioral observation and monitoring of physiological parameters.
In the neonatal period, sympathetic and even more markedly parasympathetic activities are very low in preterm newborns, compared to full-term. Parasympathetic activity is then characterized by a higher speed of recovery. Indeed, a study showed that autonomic nervous system maturation in preterm newborns has reached the level of full-term ones at 2 years of age [45]. The descending pain modulatory system (DPMS) comprises a network of cortical and subcortical brain regions that can facilitate or inhibit nociceptive afferent brain input via brainstem nuclei (bilateral anterior insula, anterior cingulate cortices, amygdala, rostroventromedial medulla (RVM), PAG). Alterations in DPMS connectivity influence pain perception [46]. Recently using functional MRI (fMRI), it has been demonstrated that in newborn infants, pain-related brain activity is similar to that observed in adults [47] and that infants with a more functionally connected DPMS, show a greater ability to regulate their pain experience and dampen the magnitude of their brain activity in response to incoming nociceptive input [48]. Activity of this descending pain-inhibitory system, with RVM pain responding “pronociceptive ON” cells and “antinociceptive OFF” cells, switches during persistent stimulation from a pain inhibitory to a pain facilitatory activity. This switch could explain how migraine headache can be generated and maintained also in the absence of a peripheral sensory input with consequent generation of allodynia. Altered nociceptive pathway has been considered responsible for a significantly earlier onset of pediatric migraine in patients who had been admitted in a NICU at birth in comparison to controls [49]. Thus, a possible effect of early alteration of pain circuitry plasticity, consisting in malfunctioning of descending inhibitory nociceptive pathways, increased activity of facilitatory nociceptive pathways, and altered neuronal synapses, could be a central hyperexcitability, corresponding to central sensitization, which is suspected to be involved in chronic headache [50]. Indeed, prevention, identification, and individualized treatment of pain are considered by neonatologists to be key elements of modern levels of care for prevention of future neurological and behavioral problems. Nowadays, although neonatal care protocols aim to prevent the at-risk newborns from being negatively affected by the consequence of detrimental response strategies to early life pain experiences, prenatal and perinatal insult during neuronal development are still having long-term impacts on the nervous system circuitry through neuronal plasticity.
Neurovegetative system during child development can be characterized by a functional dysregulation, as well described in case of high autonomic arousal related to sympathetic activity and concomitant conversion symptoms [51]. Thus, an imbalance of DPMS neuroregulation, related to a reduced adrenergic activation and persistent reduced action of adrenergic modulation and NPY on trigeminovascular system, could predispose, in preschool migraines, to a heightened pain experience and presence of symptoms attributable to the activation of the parasympathetic trigeminal reflex. The locus coeruleus (LC) is one of the major sources of noradrenaline to the dorsal horn of the spinal cord and neocortex and might be the key nucleus involved in such an autonomic control dysfunction. The hypothesis of a relative noradrenergic reduced activity in predisposition to chronic pain development has been experimentally sustained [52].
In adult migraineurs, several studies ascertained, during headache-free intervals, an imbalance between sympathetic and parasympathetic tone, characterized by a complex pattern ranging from sympathetic hypofunction and parasympathetic hyper-function [53, 54] to the opposite, with sympathetic hyper-function and a parasympathetic hypofunction [55]. An asymmetry in brain autonomic control has also been demonstrated in adults in response to pain, with a predominant parasympathetic activation in left-side migraineurs and a predominantly sympathetic function in right-side migraineurs [56]. Thus, an autonomic dysfunction could in some children to be responsible for a predisposition to manifest a different symptomatologic profile.
Clinical Features of Migraine
The current 3rd IHS classification [20] establishes diagnostic criteria specifically aimed at adult age, with the only “pain duration” reduced from 4 to 2 h in developmental age.
The restrictive use of these diagnostic criteria means that only subjects satisfying them could be included migraine studies. However, many studies have shown a low sensitivity of ongoing IHS criteria for a right migraine diagnosis in children with consequent epidemiological underestimation [15].
These difficulties appear to be even more evident in preschool age as evidenced by an important recent Italian study [15] which underlines how with the current criteria about 30% of children under 6 remain unclassifiable and 30% is classified as probable migraine.
A criteria modification, specifically excluding the migraine attack duration and introducing the positive familiarity, increased migraine diagnosis and reduced the unclassifiable headaches to 8.5% of children under 6 years.
A recent Korean study [16] confirmed the aroused criticisms on the 3rd IHS criteria adoption in preschoolers, finding unclassifiable recurrent headaches in more than 60% and probable migraine in 12% of patients.
A lower duration of migraine attacks, even less than 1 h, has been described in preschoolers in comparison with older children. Torriero et al. [15] reported that 70.7% of preschoolers had painful attacks lasting less than 1 h. The easy occurrence of naps in youngers has been considered as a potential determinant for the shorter duration of migraine attacks [14]. In follow-up studies, a gradual increase in the duration of attacks has been observed [9, 10, 57, 58•].
The frequency of attacks is generally lower than at later ages [9,10,11, 14, 59]. Attacks are often severe in intensity. The pain site is predominantly bilateral compared to adulthood, but without significant differences compared to children aged more than 7 years. The few literature studies show that vomiting tends to be more frequent at this age, while photo and phonophobia are prevalent in elders [9, 11, 59, 60]. The attack topography may vary in the same subject in the course of the time from frontal or occipital to bitemporal [10•, 58•].
A Finnish study [10•] also reported that the triggers of the attacks vary in the same subject over the years, suggesting a possible specific age vulnerability [10•\]. Raieli et al. [14] have recently observed in the pediatric migraine population both the presence of allodynia and cranial autonomic symptoms (CAS), as conjunctival injection, lacrimation, rhinorrhea, etc., and among them also a curious condition like the red ear syndrome, correlated with juvenile migraine [61].
An interesting observation is that both the allodynia and the CAS may already be present in younger children with migraine, without significant different prevalence compared to the subsequent ages [14]. On the other hand, this study showed an increased prevalence of allodynia which, after reaching the post-pubertal age, settled on values similar to those described in adults [58•].
These data may suggest that increased allodynia may be secondary to sensitization due to repeated attacks over several years, and expression of a worsening migraine. Instead, CAS may already be a clinical marker of migraine in a subgroup of children, whose presence predicts the persistence of attacks in adulthood [58•]. These observations, if confirmed in larger and non-selected populations, may suggest early intervention strategies.
The familiarity for migraine is very high in this group, ranging from 75 to 90% of children [9, 14, 15], and it has been suggested as a diagnostic criterion [15]. Moreover, recent data suggest the association of familiarity with early onset of migraine, especially when one or both parents are migraineurs [62] and migraine appears earlier in these children than their affected parents [63].
The few existing studies in preschoolers often report incomplete and non-homogeneous information on clinical features of migraine and the variable prevalence of symptoms could be related to the different median age considered [3•].
Therefore, more prospective studies on larger population are necessary, aiming to obtain more careful description of the migraine attacks and to better understand similarities and differences between age groups.
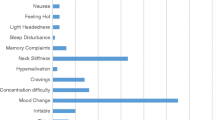
The main clinical features described in studies on children under 7 years, adopting the IHS criteria, are reported in Table 2.
Therapy of Migraine in Preschoolers
Since recent findings on migraine model in rats show that prophylactic drugs (Valproic Acid and Topiramate) present different effects in relation to age [64], and topiramate and amitriptyline, with documented prophylactic efficacy in adults, are comparable to placebo in developmental age [65], a therapeutic setting in adults cannot be translated tout court in childhood. Moreover, symptomatic or prophylactic pharmacological trials of migraine in younger children have not been published yet.
The suggested management is actually based on experts’ opinion only and points the use of NSAID and Paracetamol in symptomatic treatment for painful attacks, associated with anti-emetic agents when nausea and vomiting are very disabling [3•]. A study showed good and well-tolerated responses to assumption of triptans in a small population of migraineurs children (10 children), including children below 7 years age [66], without specifying the age ranges considered and the relative response rates to the treatment. Some authors underline that prophylactic treatment is not often needed. Nevertheless, in presence of more than 4 attacks/months, longer duration of attacks, or severe impact on child and family’s quality of life, the use of prophylactic drugs may be suggested [3•]. No randomized trials are available on the treatment of children under the age of 7, but pizotifen, cyproheptadine, propranolol, and amitriptyline were suggested for prophylactic treatment [3•].
It is common opinion that in younger children, these therapies have a good safety profile and may be useful. In this subgroup of migraineurs, non-pharmacologic treatments as regular meals, rest, good sleep, avoidance of factors triggering or aggravating the attacks, are usually suggested.
A study comparing migraineurs under 6 years to children aged more than 6, and aiming to evaluate the efficacy of non-pharmacologic strategies (avoidance of dietary triggers, excessive exposure to sun, and good sleep hygiene), evaluating attack frequency reduction from 50 to 75% [12].
The response was higher in younger population. The authors interpreted these results as related to shorter duration of the disease until the start of treatment as well as a lower frequency in this population [12].
Certainly, in general opinion, the non-pharmacologic option should be considered the first therapeutic step in treating younger children.
Follow-up of Preschoolers with Migraine
Since migraine is a long-life disease with temporal intermittent course, the analysis of impact on quality of life and therapeutic strategy must be taken this into account. The fear about the temporal course of their migraine seems be more relevant in children than in their parents or pediatricians [23]. Surely the sooner onset of disease poses major questions about the future of younger children, along with their families, who see the prospect of a long-lasting suffering. However, if clinical studies on migraine are rare in preschoolers, the prospective follow-up researches are more rare, both in relation to the temporal course of migraine in school-age children and adolescents and to its clinical course in adulthood.
In 2000, Hernandez et al. [57] studied a pediatric migraine population (284 children), including 69 children below 6 years, of whom 181 children (50 under 6 years) were followed for a period ranging from 2 to 10 years. The follow-up showed that in the whole sample, only 11.7% had an unfavorable evolution. The pediatric migraineurs below 6 years had 4.2 times more risk of an unfavorable evolution than older group. However, limits of the study were that children were classified following Prensky’s criteria (not IHS criteria), the follow-up did not distinguish the stable or reduced migraine within the favorable outcome group and the full remission group, and moreover the follow-up covered a limited range of years (2–10 years) [57].
The first prospective study on pediatric population under 7 years monitored 25 children for a mean duration of 4.2 years (range 2.8 to 6.6 years), but only 5 children were classified migraineurs with the 2004 2nd IHS criteria and only 1 had also persistent headache at follow-up [8]. Early somatic symptoms and psychiatric comorbidity were more present in children with persistent headache, but more children had tension or not classified headache and the clinical subgroups were small.
Another study [9] showed that 39 migraineurs under 6 years, after a follow-up ranging from 0.5 to 10 years (mean 3.5 ± 2.7 years SD), had remission in 13%, improvement in 36%, and stability or worsening in 51%. In summary, migraineurs had a poorer prognosis than other primary headaches (tension type and idiopathic stabbing headache), and vomiting during attacks had a negative predictive factor for headache persistence.
An original study [10•] compared a population of children with migraine and tension-type headache in at 6 and 13 years of age. Results showed that 38% of children with tension-headache changed in migraine, 32% migraineurs changed in tension-type headache, and 15% become headache free. Moreover, some clinical features and trigger factors changed during the 7-year follow-up. The power of this study was based on a prospective model, the unselected population, a larger sample, and the age homogeneous population (only children 6 years old), while its limits were the short-term follow-up (7 years) and a dropout superior to 50%.
We [58•] recently showed in the first long-term follow-up study (mean 17 ys, range 15–23 years) that 75% of migraineurs below 6 years of age had a migraine persistence. Pain clinical features could change over time in the same subject. The suspected prognostic negative factors were cranial autonomic symptoms and allodynia. There are no other prospective studies on younger migraineurs followed before 7 year of age. A recent study [67] showed that the early onset of migraine (cut-off 7 years) was associated with more frequent attacks in a sample of adults (median follow-up, 18.2 years), supporting the hypothesis that early onset of migraine is associated with persistence and poorer prognosis. However, the larger range of follow-up was limited by a retrospective assessment of age at onset of migraine, a possible bias of sample selection, and a transversal instead of longitudinal assessment of the increased frequency, considering the floating course of migraine.
Open Questions
If up to 2005 only very few studies [5, 6] specifically pointed on migraine under 7 years, the next clinical epidemiological and follow-up studies on preschool migraineurs demonstrate clearly that migraine in this pediatric population is absolutely not rare. Thus, migraine in preschoolers can represent an important clinical challenge and probably has a negative predictive role for its persistence in later ages.
However, several questions remain open owing to the few available studies and their frequent methodological problems.
More studies are based on retrospectively collected data, mainly from parents’ interview, almost all are on selected clinical population, frequently with incomplete descriptions of the clinical features, the follow-up studies present important drop-out and are based on small groups, and the management of migraine is generally poorly described.
Biological factors attributable to early painful experiences can enhance a predisposition to migraine based on a genetic background [48, 54, 68]. Nevertheless, their specific role on clinical, prognostic, and therapeutic dimensions of migraine, across the different ages, are not been well defined.
Also, the bio psycho-social dimension should be better considered and integrated with the more recent biological evidences [69].
Clinical evidence suggests that migraine in this age may present several differences in comparison to school age children and adolescents.
However, these differences have not been well clarified, except for the duration of the attacks and probably their frequency. There are not data about features of aura or other clinical important characteristics, e.g., allodynia. Obviously, many difficulties come from the age of children that make difficult to collect reliable clinical reports and from the absence of neurophysiological and neuroimaging investigations related to strict ethical limits. We believe that usual pharmacological and non-pharmacological therapeutic strategies are efficacious in this age like in the more aged patients, but no specific studies are available yet. Multicentric studies can help to answer to these questions.
The follow-up studies are usually brief, or retrospective, based on small and heterogeneous samples with important drop-out at follow-up, not analyzing more stages of the migraine temporal course, and with possible confounding factors influencing the prognosis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arruda MA, Guidetti V, Galli F, Albuquerque RC, Bigal ME. Primary headaches in childhood: a population-based study. Cephalalgia. 2010;30:1056–64.
Abu-Arafeh I, Russell G. Prevalence of headache and migraine in schoolchildren. BMJ. 1994;309:765–9.
Abu-Arafeh I, Howells R. Primary headaches in children under the age of 7 years. Curr Pain Headache Rep. 2014;18:401–8. This article is the first and only review describing preschoolar primary headaches.
Warner JF. Recurrent headaches in children and associated pathological conditions. BMJ. 1879;2:889–90.
Lahat E, Barr J, Barzilai A, Cohen H, Berkovitch M. Visual evoked potentials in the diagnosis of headache before 5 years of age. Eur J Pediatr. 1999;158:892–5.
Balottin U, Nicoli F, Pitillo G, Ferrari Ginevra O, Borgatti R, Lanzi G. Migraine and tension headache in children under 6 years of age. Eur J Pain. 2004;8:307–14.
Raieli V, Eliseo M, Pandolfi E, La Vecchia M, La Franca G, Puma D, et al. Recurrent and chronic headaches in children below 6 years of age. J Headache Pain. 2005;6:135–42.
Balottin U, Termine C, Vicoli F. Idiopathic headache in children under six years of age: a follow-up study. Headache. 2005;45:705–15.
Battistella PA, Fiumana E, Binelli M, Bertossi E, Battista P, Perakis E, et al. Primary headaches in preschool age children: clinical study and follow-up in 163 patients. Cephalalgia. 2006;26:162–71.
Virtanen R, Aromaa M, Rautava P, Metsähonkala L, Anttila P, Helenius H, et al. Changing headache from preschool age to puberty. A controlled study. Cephalalgia. 2007;27:294–303. This original prospective study compares migraine and tension-type headache in an unselected population of children assessed at 6 and 13 years of age. Moreover, it describes the changing clinical features and trigger factors during the 7 years follow-up.
Eidlitz-Markus T, Gorali O, Haimi-Cohen Y, Zeharia A. Symptoms of migraine in the paediatric population by age group. Cephalalgia. 2008;28:1259–63.
Eidlitz-Markus T, Haimi-Cohen Y, Steier D, Zeharia A. Effectiveness of nonpharmacologic treatment for migraine in young children. Headache. 2010;50:219–23.
Ramdas S, Prasad M, Abu-Arefeh I. Primary headache disorders in children under 7 years of age. Scott Med J. 2013;58:26–9.
Raieli V, Pitino R, Giordano G, Spitalieri C, Consolo F, Puma D, et al. Migraine in a pediatric population: a clinical study in children younger than 7 years of age. Dev Med Child Neurol. 2015;57:585–8.
Torriero R, Capuano A, Mariani R, Frusciante R, Tarantino S, Papetti L, et al. Diagnosis of primary headache in children younger than 6 years: a clinical challenge. Cephalalgia. 2017;37:947–54.
Kang BS, Lee J, Choi JH, Kwon HH, Kang JW. Clinical manifestations of headache in children younger than 7 years. Korean J Pediatr. 2018;61:355–61.
Correnti E, Drago F, Messina LM, Rocchitelli L, D’Aiuto F, Vanadia F, et al. Headaches in preschoolers: are red flags predictive of positive neuroimaging in emergency department? SF J Headache Pain. 2018;1:1–5.
Straube A, Andreou A. Primary headaches during lifespan. J Headache Pain. 2019;20:35. https://doi.org/10.1186/s10194-019-0985-0.
GBD 2016 Headache Collaborators, Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–76.
Headache Classification Subcommittee of the International Headache Society. The International Classification of headache disorders. 3nd edition. Cephalalgia. 2018;38:1–211.
Jernigan TL, Baaré WF, Stiles J, Madsen KS. Postnatal brain development: structural imaging of dynamic neurodevelopmental processes. Prog Brain Res. 2011;189:77–92.
Stiles J, Jernigan TL. The basics of brain development. Neuropsychol Rev. 2010;20:327–48.
Raieli V, Compagno A, Pandolfi E, La Vecchia M, Puma D, La Franca G, et al. Headache: what do children and mothers expect from pediatricians? Headache. 2010;50:290–300.
Sillanpaa M. The classification of migraine of headache. In: Guidetti V, Russell G, Sillanpaa M, Winner P, editors. Headache and migraine in childhood and adolescence. London: Martin Dunitz; 2002. p. 275–85.
Sillanpaa M. Prevalence of migraine and other headache in Finnish children starting school. Headache. 1976;15:288–90.
Sillanpaa M, Piekkala P, Kero P. Prevalence of headache at preschool age in an unselected child population. Cephalalgia. 1991;11:239–42.
Do TP, Remmers A, Schytz HW, Schankin C, Nelson SE, Obermann M, et al. Red and orange flags for secondary headaches in clinical practice SNNOOP10 list. Neurology. 2019;92:134–44.
Mortimer MJ, Kay J, Jaron A. Childhood migraine in general practice: clinical features and characteristics. Cephalalgia. 1992;12:238–43.
OstKirken G, Andler F, Hammer F, Pöhler KD, Snyder-Schendel E, Werner NK, et al. Prevalences of primary headaches symptoms at school-entry: a population-based epidemiological survey of preschool children in Germany. J Headache Pain. 2006;7:331–40.
Chu ML, Shinnar S. Headaches in children younger than 7 years of age. Arch Neurol. 1992;49:79–82.
Barlow CF. Migraine in the infant and toddler. J Child Neurol. 1994;9:92–4.
Cavestro C, Montrucchio F, Benci P, Pompilio D, Mandrino S, Cencio PG, et al. Headache prevalence and related symptoms, family history, and treatment habits in a representative population of children in Alba, Italy. Pediatr Neurol. 2014;51:348–53.
Vetri L, Messina LM, Drago F, D’Aiuto F, Vanadia F, Brighina F, et al. Are pediatric headaches in the emergency department increasing? An Italian experience. Funct Neurol. 2019;34:188-195.
Glover V, Fisk NM. Fetal pain: implications for research and practice. Br J Obstet Gynaecol. 1999;106:881–6.
Ken WS, Ashwell, Jürgen KMF, et al. Development of the central nervous system. In: The Human Nervous System (Third Edition); 2012. p. 31–79.
Derbyshire SW. Fetal pain: do we know enough to do the right thing? Reprod Health Matters. 2008;16:117–26.
American Academy of Pediatrics, Canadian Paediatric Society. Prevention and management of pain and stress in the neonate. Paediatrics. 2000;105:454–61.
Parida SK, Schneider DB, Stoss TD, Pauly TH, McGillis JP. Elevated circulating calcitonin gene-related peptide in umbilical cord and infant blood associated with maternal and neonatal sepsis and shock. Pediatr Res. 1998;43:276–82.
Bright FM, Vink R, Byard RW, Duncan JR, Krous HF, Paterson DS. Abnormalities in substance P neurokinin-1 receptor binding in key brainstem nuclei in sudden infant death syndrome related to prematurity and sex. PLoS One. 2017;20:e0184958. https://doi.org/10.1371/journal.pone.0184958.
Slater S, Crawford MJ, Kabbouche MA, LeCates SL, Cherney S, Vaughan P, et al. Effects of gender and age on paediatric headache. Cephalalgia. 2009;29:969–73.
Lidow MS. Long-term effects of neonatal pain on nociceptive systems. Pain. 2002;99:377–83.
Walker SM. Biological and neurodevelopmental implications of neonatal pain. Clin Perinatol. 2013;40:471–91.
Herlenius E, Lagercrantz H. Development of neurotransmitter systems during critical periods. Exp Neurol. 2004;190:S8–21.
Coq JO, Delcour M, Ogawa Y, Peyronnet J, Castets F, Turle-Lorenzo N, et al. Mild intrauterine hypoperfusion leads to lumbar and cortical hyperexcitability, spasticity, and muscle dysfunctions in rats: implications for prematurity. Front Neurol. 2018;15(9):423. https://doi.org/10.3389/fneur.2018.00423.
De Rogalski Landrot I, Roche F, Pichot V, Teyssier G, Gaspoz JM, Barthelemy JC, et al. Autonomic nervous system activity in premature and full-term infants from theoretical term to 7 years. Auton Neurosci. 2007;136:105–9.
Ploner M, Lee MC, Wiech K, Bingel U, Tracey I. Prestimulus functional connectivity determines pain perception in humans. PNAS. 2010;107:355–60.
Goksan S, Hartley C, Emery F, Cockrill N, Poorun R, Moultrie F, et al. fMRI reveals neural activity overlap between adult and infant pain. eLife. 2015;4:e06356. https://doi.org/10.7554/eLife.08663.
Goksan S, Baxter L, Moultrie F, Duff E, Hathway G, Hartley C, et al. The influence of the descending pain modulatory system on infant pain-related brain activity. Elife. 2018;11:7. https://doi.org/10.7554/eLife.37125.
Maneyapanda SB, Venkatasubramanian A. Relationship between significant perinatal events and migraine severity. Pediatrics. 2005;116:555–8.
Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926.
Kozlowska K, Palmer DM, Brown KJ, McLean L, Scher S, Gevirtz R, et al. Reduction of autonomic regulation in children and adolescents with conversion disorders. Psychosom Med. 2015;77:356–70.
Patel R, Qu C, Jennifer Y, Xie JY, Porreca F, Dickenson AH. Selective deficiencies in descending inhibitory modulation in neuropathic rats: implications for enhancing noradrenergic tone. Pain. 2018;159:1887–99.
Gotoh F, Komatsumoto S, Araki N, Gomi S. Noradrenergic nervous activity in migraine. Arch Neurol. 1984;41:951–5.
Benjelloun H, Birouk N, Slaoui I, Coghlan L. Autonomic profile of patients with migraine. Neurophysiol Clin. 2005;35:127–34.
Havanka-Kanniainen H, Tolonen U, Myllyla VV. Autonomic dysfunction in adult migraineurs. Headache. 1986;26:425–30.
Avnon Y, Nitzan M, Sprecher E, Rogowski Z, Yarnitsky D. Autonomic asymmetry in migraine augmented parasympathetic activation in left unilateral migraineurs. Brain. 2004;127:2099–108.
Hernandez-Latorre MA, Roig M. Natural history of migraine in childhood. Cephalalgia. 2000;20:573–9.
Marchese F, Rocchitelli L., Messina LM, Mangano GD, Nardello R, Vanadia F, Mangano S, Brighina F, Raieli V. Migraine in children under 6 years of age: a long-term follow-up study. Eur J. Paed Neurol. 2020; 27:67–71. This article is the first long term follow study in migrainous children under 7 years of age. Main findings are that early onset of migraine, familiarity of migraine and cranial autonomic symptoms are probable risk factors for persistence of migraine in adulthood.
Eidlitz-Markus T, Zeharia A. Symptoms and clinical parameters of pediatric and adolescent migraine, by gender -a retrospective cohort study. J Headache Pain. 2017;80. https://doi.org/10.1186/s10194-017-0789-z.
Eidlitz-Markus T, Haimi-Cohen Y, Zeharia A. Vomiting and migraine-related clinical parameters in pediatric migraine. Headache. 2017;57:899–907.
Raieli V, Compagno A, Brighina F, La Franca G, Puma D, Ragusa D, et al. Prevalence of red ear syndrome in the juvenile primary headaches. Cephalalgia. 2011;4:597–602.
Eidlitz-Markus T, Haimi-Cohen Y, Zeharia A. Association of age at onset of migraine with family history of migraine in children attending a pediatric headache clinic: a retrospective cohort study. Cephalalgia. 2015;35:722–7.
Eidlitz-Markus T, Zeharia A. Younger age of migraine onset in children than their parents: a retrospective cohort study. J Child Neurol. 2018;33:92–7.
Huang P, Kuo PH, Lee MT, Chiou LC, Fan PC. Age-dependent anti-migraine effects of valproic acid and topiramate in rats. Front Pharmacol. 2018;25(9):1095. https://doi.org/10.3389/fphar.2018.01095.
Powers SW, Coffey CS, Chamberlin LA, Ecklund DJ, Klingner EA, Yankey JW, et al. Trial of amitriptyline, topiramate, and placebo for pediatric migraine. N Engl J Med. 2017;12(376):115–24.
Hershey AD, Powers SW, Le Cates S, Bentti AL. Effectiveness of nasal sumatriptan in 5- to 12-year-old children. Headache. 2001;41:693–7.
Asuni C, Manchia M, Deidda A, Stochino ME, Cherchi A, del Zompo M. Mixture analysis of age at onset in migraine without aura: evidence for three subgroups. Headache. 2010;50:1313–9.
Guidetti V, Ottaviano S, Pagliarini M. Childhood headache risk: warning signs and symptoms present during the first six months of life. Cephalalgia. 1984;4:236–42.
Guidetti V, Cerutti R, Faedda N, Natalucci G. Migraine in childhood: an organic, biobehavioral, or psychosomatic disorder. Neurol Sci. 2019;40:93–8.
Author information
Authors and Affiliations
Contributions
Vincenzo Raieli conceived the review, Ettore Piro performed especially the section “Neuroanatomical and functional development of nervous system pathways and neurotransmitters involved in migraine,” Vincenzo Raieli and Antonina D’Amico performed the literature search and data analysis, and Vincenzo Raieli and Ettore Piro wrote the first draft of the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent Form
Not applicable
Ethics Approval
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Childhood and Adolescent Headache
Rights and permissions
About this article
Cite this article
Raieli, V., D’Amico, A. & Piro, E. Migraine in Children Under 7 Years of Age: a Review. Curr Pain Headache Rep 24, 79 (2020). https://doi.org/10.1007/s11916-020-00912-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-020-00912-5