Abstract
Purpose of Review
To review the pathophysiologic, epidemiologic, and clinical evidence for similarities and differences between migraine with and without aura.
Recent Findings
The ICHD-3 has recently refined the diagnostic criteria for aura to include positive symptomatology, which better differentiates aura from TIA. Although substantial evidence supports cortical spreading depression as the cause of visual aura, the role (if any) of CSD in headache pain is not well understood. Recent imaging evidence suggests a possible hypothalamic origin for a headache attack, but further research is needed. Migraine with aura is associated with a modest increase in the risk of ischemic stroke. The etiology for this association remains unclear. There is a paucity of evidence regarding treatments specifically aimed at the migraine with aura subtype, or whether migraine with vs without aura responds to treatment differently. Migraine with typical aura is therefore often treated similarly to migraine without aura. Lamotrigine, daily aspirin, and flunarizine have evidence for efficacy in prevention of migraine with aura, and magnesium, ketamine, furosemide, and single-pulse transcranial magnetic stimulation have evidence for use as acute treatments. Although triptans have traditionally been contraindicated in hemiplegic migraine and migraine with brainstem aura, this prohibition is being reconsidered in the face of evidence suggesting that use may be safe.
Summary
The debate as to whether migraine with and without aura are different entities is ongoing. In an era of sophisticated imaging, genetic advancement, and ongoing clinical trials, efforts to answer this question are likely to yield important and clinically meaningful results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine with aura is estimated to affect between 1/5 and 1/3 of people with migraine in the USA, an estimated 7.4–11.1 million people [1]. The dramatic neurologic accompaniments of migraine with aura initially appeared in the literature in 1873, but it took over 100 years for these symptoms to be recognized as the result of cortical spreading depression and associated oligemia, as first described by Leao [2]. The International Classification of Headache Disorders (ICHD) has differentiated between migraine with and without aura (formerly called classic and common migraine) since inception, citing the presence of spreading oligemia in migraine with aura and its absence in migraine without aura. Since that time, headache researchers and clinicians have wrestled with questions about whether these two types of migraine should be thought of as fundamentally different entities or as different manifestations of the same underlying pathophysiology. In this review, we will discuss the pathophysiologic, epidemiologic, and clinical evidence for similarities and differences, and consider the implications for management of patients with migraine with aura.
Defining Migraine with Aura
The ICHD recognizes that migraine aura and migrainous headache are related entities that do not always coincide [3]. The criteria reflect the current understanding that migraine is a neurological process of which headache is sometimes, but not always, a part. The presence of aura, with or without headache, is the defining feature of migraine with aura, while headache, migrainous or not, is not required for the diagnosis. In contrast, the definition of migraine without aura emphasizes headache characteristics and associated symptoms, i.e. migrainous headache. The neurological events of aura should be differentiated from commonly reported symptoms of prodrome, such as changes in mood or activity level, hunger/cravings, and yawning [4] or a postdrome such as fatigue, difficulty concentrating, and stiff neck [5].
The criteria for migraine with aura are listed in Table 1. Per the most recent classification, the aura symptom must have at least three of the six: spreading gradually over ≥ 5 min, two or more symptoms occur in succession, each individual aura symptom lasts 5–60 min, at least one aura symptom is unilateral, at least one aura symptom is positive, and the aura is accompanied, or followed within 60 min, by headache [3]. The prior ICHD-II definition did not include positive symptoms as one of the possible criteria. This element was added because field testing showed that the current criteria better distinguished between migraine aura and transient ischemic attacks [6•]. Out of the aura subtypes, visual aura is by far the most common. Indeed, it is unusual to encounter a patient with sensory, language, or motor aura who does not have a history of visual aura [7]. Much time has been spent on clinically distinguishing visual aura from other transient visual phenomenon. Validated clinical tools such as the visual aura rating scale have emphasized the key features which duration (5–60 min), gradual development (≥ 5 min), scotoma, zig-zag lines, and laterality as key features [8]. Descriptions of sensory aura, also defined as typical aura, classically manifest as a Jacksonian march that is unilateral, starts in the hand, progresses up the arm, and then affects the face and tongue.
The presence of motor aura leads to the diagnosis of hemiplegic migraine. This distinction is in part secondary to the known rare genetic variants which correspond with familial hemiplegic migraine. Migraine with brainstem aura is perhaps the most controversial of the aura subtypes. Originally described as “basilar artery migraine” by Bickerstaff in 1961 secondary to the belief that there was a transient narrowing of the basilar artery, brainstem aura is characterized by at least two of the following fully reversible symptoms: dysarthria, vertigo, tinnitus, hypacusis, diplopia, ataxia not attributable to sensory deficit, and decreased level of consciousness [9]. Over the last 10 years, it has been argued that this may in fact not represent an independent disease entity that is different from migraine with typical aura, secondary to the overlap of many of these symptoms reported by patients with typical aura [10]. Field testing of the ICHD-3 also suggested that the criteria for brainstem aura should be more restrictive [11].
Pathophysiology of Aura and Headache Pain
The pathophysiology of visual aura is widely accepted to be cortical spreading depression, as first described by Leao in the rat [12]. CSD is initiated by a slowly propagating wave of depolarization in cortical neurons and glia, followed by hyperpolarization that moves across the cortex at a rate of 3–5 mm/min. It is accompanied by dramatic changes in ion homeostasis and neurotransmitter release [13]. Given the increased energy demands to restore homeostasis, this is quickly accompanied by a transient increase in cerebral blood flow [14, 15]. CSD has been demonstrated to occur in animal studies as well as in the human visual cortex in perfusion weighted and functional MRI studies [13, 16, 17••]. Although other types of aura (language, sensory, and brainstem) are not as well studied, evidence also points to CSD as their pathophysiology [18].
The connection between aura and the headache phase has several proposed mechanisms. One mechanism by which CSD may lead to the headache phase is by initiation of an inflammatory cascade and nociceptive substances via vascular dilation and constriction of pial vessels (which have nociceptive innervation by trigeminal afferents) and direct depolarization of nociceptive afferents through release of potassium [19, 20]. However, lack of evidence for blood-brain barrier disruption during migraine does not support the anticipated leakage and edema from neurogenic-like inflammation [21]. Furthermore, inhibitors of substances identified in the inflammatory cascade (such as substance P, neurokinin 1 or endothelin) have not prevented migraine headache in humans, although they have prevented CSD induced neurogenic dura mater inflammation in animal models [22,23,24,25]. CSD may also directly induce the trigeminal subnucleus caudalis via direct connections from layer 5 of the insula and primary somatosensory cortex [26]. Charles et al. argue that although there is strong evidence that CSD could cause pain, results from behavioral studies in awake rodents illustrate less convincing results—perhaps secondary to more limited models of pain—do not consistently show this [27].
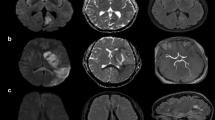
How migraine headache pain is initiated in those without aura is less well understood. One argument is that CSD occurs silently in those without aura (in subcortical regions, such as the hypothalamus), and that otherwise, the pathophysiology between migraine with and without aura does not substantially differ [28]. Evidence against this came from a modest-sized study (39 patients) in which tonabersat, a drug known to inhibit CSD in animal studies, significantly reduced the frequency of aura attacks but not migraine attacks without aura [29]. Further evidence that CSD may not always be coupled to migraine pain comes from the observation that calcitonin gene-related peptide (CGRP) is not elevated in live animal models of CSD, but only in slices of the neocortex [30,31,32]. Other proposed mechanisms for migraine without aura include shear-induced platelet aggregation in which platelets aggregate in narrowed vessels releasing local serotonin leading to nitric oxide formation and release of CGRP [25]. The anatomic origin of migraine headache pathophysiology has also been of interest with advances in imaging. One study proposed the hypothalamus as the new “generator” of migraine pain based on increased hypothalamic activity in fMRI in the 24 h prior to migraine pain (albeit this was done in only one patient) [33••]. Studies using advanced imaging techniques in a greater number of patients are needed to better elucidate such findings.
Risks Associated with Migraine with Aura
Epidemiologic studies show that migraine with aura is associated with an increased risk of cardiovascular outcomes. The best characterized of these is the increase in the risk of ischemic stroke. A recent meta-analysis found an OR of 1.56 (95% CI 1.30 to 1.87) for ischemic stroke in people with migraine with aura [34]. Older meta-analyses, which do not include a Swedish twin study published in 2017, showed roughly double the risk of ischemic stroke in people with migraine with aura [35]. The risk of ischemic stroke in people with migraine without aura is not increased, however, suggesting a pathophysiologic relationship between aura and the risk for stroke.
A history of migraine of any type has also been associated with an increased risk of cardiac events, including myocardial infarction (hazard ratio (HR) 1.39), angina/coronary revascularization procedures (HR 1.73), and all major cardiovascular disease (HR 1.50) [36]. A recent Danish population-based study suggests that this increased risk may also be driven by the migraine with aura subgroup (hazard ratio of 1.74 (95% CI 1.44 to 2.11) for migraine with aura and 1.22 (1.01 to 1.48) for migraine without aura) [37•].
The mechanism for this increase in risk is not known, but it is interesting that migraine with aura seems to be a more significant risk factor in younger people without traditional cardiac risk factors such as diabetes or hypertension. This could suggest that there is instead a common underlying genetic or physiologic difference that leads to both migraine aura and increased cardiovascular risk. Changes in the endothelium and hypercoagulability have both been proposed as potential mechanisms [38]. The best available evidence also supports a stronger association between brain white matter lesions and migraine with aura than for migraine without aura, possibly suggesting a role for microvascular abnormalities that increase the risk of both aura and stroke [39]. Another possible explanation is that migraine aura attacks themselves somehow increase the risk for cardiovascular events. This is somewhat supported by the finding that a recent diagnosis or onset of migraine is associated with a higher CVD risk than a remote diagnosis [37•]. One study also suggested that an increased frequency of attacks was associated with higher risk, although high frequency was defined as one attack per month or more. Regardless of the nature of the pathophysiologic link, it is clear that migraine with aura is associated with increased cardiovascular risks and that the association for migraine without aura is either less strong or absent. Thus, epidemiologic evidence supports a fundamental difference between the two entities.
Preventive Treatment of Migraine with Typical Aura
Treatments with evidence for efficacy in migraine with aura are summarized in Table 2. In a paper summarizing lessons learned from the tonabersat studies, Hauge et al. state that it is advisable to study migraine with and without aura separately, and recommend that the FDA “not accept a drug for the treatment of MA without specific studies focusing on this disorder” [40]. Although some treatments are tested specifically for migraine with aura, as summarized below, most studies of acute and preventative migraine treatments include both patients with migraine with aura and migraine without aura. When both migraine subtypes are included, it is unusual for treatment response to be reported as a function of migraine subtype. The degree to which migraine with aura responds to acute or preventive treatment differently from migraine without aura is therefore a sparsely studied topic. Despite this, the results of these trials are typically applied to both populations. In the search for clinical features that could help predict response to treatment, it is interesting that an obvious clinical marker—the presence or absence of aura—has largely been overlooked.
Based on the hypothesis that migraine aura is fundamentally a disorder of neuronal ionic gradients, anti-epileptic drugs are often suggested as preventive treatments. The little available evidence regarding response to AED treatment of migraine with vs without aura suggests that inhibition of CSD may be key to treatment efficacy. In rats, chronic daily administration of the AEDs topiramate and valproate, as well as propranolol, amitriptyline, and methysergide, decreased CSD frequency by 40–80%, in a dose-dependent fashion [41]. Several small open-label or pilot studies found that lamotrigine 50–300 mg daily (mean 100–170 daily) reduced aura frequency by 50% or more in 68–75% of patients [42, 43]. Yet, the 2012 AAN/AHS guidelines place lamotrigine in the category of medications that are established as ineffective for preventive treatment of migraine, not considering aura subtype [44]. Lamotrigine has been shown to suppress CSD in the rat brain [45]. Based on these findings, it may be that lamotrigine has a unique benefit for migraine aura via suppression of CSD. (It is also possible that any positive findings are due to typical placebo responses in open label studies.)
Contradicting this theory, a study of topiramate for the prevention of migraine with aura (n = 269) and migraine without aura (n = 542) showed that aura frequency reduced in parallel with reduction of overall migraine frequency in patients with migraine with aura, and overall headache frequency was reduced equally for migraine with and without aura [46]. Thus, this study did not support a uniquely benefit effect of topiramate for migraine with aura, despite evidence that topiramate also reduces CSD in the rat brain. Sodium valproate has often been suggested as a treatment for migraine with aura, but there are no studies examining this question and valproate does not inhibit CSD as strongly as lamotrigine [45]. Outside of the AEDs, one study of metoprolol that looked specifically at the frequency of aura attacks showed no benefit overall. Metoprolol was shown not to inhibit CSD in the rat brain [47].
In the absence of good evidence to support a different treatment course for migraine with aura, we typically follow the AAN/AHS treatment guidelines for migraine as a whole in these patients. [44]. In patients who have typical aura that is very bothersome, we often try treatments used more commonly in hemiplegic migraine or migraine with brainstem aura, such as verapamil or acetazolamide, in addition to lamotrigine. One author (RB) has anecdotally seen a reduction in migraine aura frequency in some patients treated with magnesium.
Acute Treatment of Migraine with Aura
There is currently no acute treatment with good evidence for efficacy in shortening or reducing the severity of migraine aura itself. If cortical spreading depression is the preliminary step in initiating a migraine attack, it might be expected that abortive treatment during the aura phase could prevent subsequent headaches. Interestingly, studies of triptans given during the aura phase have instead been negative on balance. In one trial, 177 patients with migraine with aura were randomized to be treated with sumatriptan SQ 6 mg or placebo at onset of aura symptoms. The aura duration was 25 min in the treatment group vs 30 min in the placebo group, a difference that was not statistically significant. The proportion of patients who subsequently had a moderate or severe headache was also not different between groups [48]. Another randomized controlled trial of sumatriptan 200 mg vs placebo in 94 patients instructed to treat as soon as they were aware of a migraine with aura attack found that sumatriptan reduced the severity of the first migraine attack treated (63% of active vs 33% of placebo group responded). The severity of the second and third attacks treated was not reduced, however, which was partly attributed to a higher placebo value for these attacks [49]. In contrast, a four-way crossover open-label study of 19 patients found that treatment with sumatriptan 100 mg during aura prevented the development of the headache in 34 out of 38 attacks (89%), suggesting that this may still be an open research question [50]. Anecdotally, we find that some patients are in fact able to prevent or ameliorate their headaches by using their triptan or a strong non-steroidal anti-inflammatory drug (NSAID) during the aura phase. We often counsel patients to try treating a few attacks after onset of pain and then try treating during aura to see which strategy is more effective.
Neuronal N-methyl-d-aspartate (NMDA) receptors are involved in the initiation and propagation of CSD [51]. Ketamine and magnesium are NMDA receptor antagonists that have shown some promise in the acute treatment of aura [52]. Ketamine nasal spray 25 mg was tested in 11 patients with hemiplegic migraine. Of these, 5 reported shorter aura duration and 6 reported no response. Of the 5 patients who reported shortened neurologic symptoms, only 2 experienced benefit for the headache itself. In a randomized controlled trial of treatment for prolonged aura, with 18 participants completing the protocol, ketamine nasal spray 25 mg was compared to midazolam as an active control [53]. There was a non-statistically significant benefit on aura severity but not duration in the ketamine group compared to the midazolam group. Ketamine is actively being studied for the treatment of migraine without aura as well, with the clinicaltrials.gov website showing three active or recently completed trials. It is unclear whether aura will be assessed in these studies.
A placebo-controlled randomized trial of IV magnesium sulfate 1 mg infusion involving 60 patients showed that participants with migraine were more likely to respond than those with migraine without aura [54]. The subgroup of migraine without aura experienced improvement in only photophobia and phonophobia but not pain or nausea compared to placebo. The migraine with aura subgroup experienced relief of all symptoms including aura significantly more often than the placebo group. A similar randomized controlled trial comparing magnesium to metoclopramide and to placebo also showed benefit of magnesium in the migraine with aura subgroup alone [54].
The sTMS (single pulse Transcranial Magnetic Stimulation) device was initially developed for the acute treatment of migraine with aura. The single pulse of transcranial magnetic stimulation is designed to interrupt the wave of CSD during a migraine aura. In a randomized, sham-controlled trial including 164 patients, the 2-h pain-free response rates were 39% in the active group vs 22% in the sham group, giving a therapeutic gain of 17% (95% CI 3–31%; p = 0.0179) [55].
Three case reports suggest that furosemide (20 mg IV daily inpatient or 40 mg PO daily outpatient) may resolved prolonged aura or reduce the frequency of aura [56,57,58]. Anecdotally, we have occasionally tried this for patients with refractory complex aura symptoms with some benefit.
Treatment of Hemiplegic Migraine and Migraine with Brainstem Aura
Hemiplegic migraine and migraine with brainstem aura are often thought of as more severe migraine phenotypes when compared to migraine with typical aura. This is possibly due to the presence of more disabling symptoms, such as motor weakness, ataxia, alternation in consciousness, or vertigo. The classification also recognizes hemiplegic migraine as a more prolonged aura subtype, lasting up to 72 h. Traditionally, triptans and ergots have been avoided for these headache types due to concern about exacerbating or prolonging these disabling symptoms. The theory behind this prohibition has rested on the belief that triptans cause intracranial vasoconstriction and thus increase the risk for prolonged aura and migrainous infarction. More recent evidence has shown that triptans do not have significant intracranial vasocontrictive properties, however, and several large case series support reconsideration of this prohibition [59]. Taken together, the three reported case series include 89 patients with hemiplegic migraine and 80 with features of basilar migraine. These series found that treatment with triptans was well tolerated, with one case of hemiplegic aura being prolonged after a single dose of rizatriptan but with normal imaging [60,61,62]. Although these case series are not large enough to conclusively rule out increased risk associated with the use of triptans, it does seem that a broad prohibition may be overly cautious. If the underlying pathophysiology of migraine with aura is the same—i.e. cortical spreading depression—regardless of aura subtype, it is reasonable to expect that the treatment approach should also be similar.
Hemiplegic migraine is known to be associated with three genes that affect the function of neuronal sodium channels, calcium channels, or sodium/potassium ATPase. Based on this, preventive medications that affect ionic gradients via function of sodium or calcium channels, or other mechanisms, have been suggested as being particularly helpful for hemiplegic migraine. These include the calcium channel blockers verapamil and flunarizine, the carbonic anhydrase inhibitor acetazolamide, and antiepileptics such as topiramate, valproate, lamotrigine, and gabapentin. Of these, flunarazine has the best quality evidence, as described above. Single case reports or small case series also support the use of verapamil, acetazolamide, and lamotrigine for prevention [63•]. There is also one case report of successful use of oral acetazolamide as an acute treatment for hemiplegic migraine aura [63•].
Other Treatment Implications of Migraine with Aura
Aspirin
The role of aspirin in the management of migraine with aura is uncertain. In the past, many providers started a daily baby aspirin in patients with migraine with aura in the hopes of mitigating the increased risk of stroke. Aspirin has never been formally studied for this purpose in the migraine with aura population, which tends to be younger and have fewer traditional cardiovascular risk factors than the population in which aspirin is typically used for primary prevention. There is preliminary evidence to suggest that further study is needed before making this a standard practice. An exploratory subgroup analysis of the Nurses Health Study II by Kurth et al. showed that women who had migraine with aura and were in the aspirin group had a higher risk of stroke than the group not treated with aspirin [64]. One open research question is whether a therapeutically induced reduction in frequency of migraine aura attacks reduces the stroke risk. Aspirin has been evaluated as a preventive treatment for migraine aura. An observational case series of 49 patients with migraine with aura who were treated with ASA 80 mg daily found that aura frequency was reduced in 39 of the 42 cases available for follow-up (93%) [65]. Aura completely disappeared in 20 (48%). A retrospective chart review including 203 Italian patients with migraine with aura found that 88.4% of patients treated with aspirin up to 300 mg daily responded, compared to 59.3% of patients who were treated with other preventive agents [66]. Response is not defined in the paper. Whether daily aspirin is beneficial for patients with migraine aura needs further study.
Combined Hormonal Contraceptives
The relationship between migraine aura and increased risk for stroke has resulted in several guidelines recommending against the use of combined hormonal contraceptives (CHCs) in women with migraine with aura [67]. Exogenous estrogen at historically commonly used doses has been shown to increase the risk of stroke, and there is concern that the combined effects of migraine with aura and estrogen result in a risk of stroke that outweighs the benefits of CHCs. There have been suggestions that these guidelines should be revised to reflect a possible decrease in CHC-associated stroke risk with modern, lower estrogen exposure CHCs [68]. A recent systematic review found insufficient evidence to guide such a revision, however [69].
In the absence of good-quality evidence, it is reasonable to continue avoiding combined hormonal contraceptives as first-line contraceptive treatments for women with migraine with aura. An individualized assessment of other cardiovascular risk factors is warranted in most cases, however. There are many situations in which it may be reasonable to use CHCs, including medical conditions that benefit from hormonal regulation, bothersome side effects from progesterone only formulations, or lack of reliable or effective contraceptive alternatives.
Conclusions
The debate as to whether migraine with and without aura are different entities is ongoing. Although there is strong evidence to support CSD as the underlying cause of migraine with aura, there is substantially less certainty that silent CSD is the underlying cause of migraine without aura. Recent limited imaging data suggests alternative generators and increasingly sophisticated imaging modalities may provide further insight. The preponderance of evidence suggests that there are important epidemiologic differences between migraine with and without aura. The pathophysiologic or genetic reasons for this are unknown. Treatments aimed at suppressing CSD are more specifically effective in migraine with aura, but there is little evidence regarding possible differential efficacy in treatments with other mechanisms. In the absence of evidence specific to migraine with aura, treatment options are thus typically shared between the two migraine subtypes. Recent advances in imaging and genetic techniques may be helpful in delineating the possible differences between the two subtypes of migraine. Further clinical studies examining differences in treatment responses between migraine with vs without aura may also be fruitful.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Buse DC, Loder EW, Gorman JA, Stewart WF, Reed ML, Fanning KM, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53(8):1278–99.
Tfelt-Hansen PC. History of migraine with aura and cortical spreading depression from 1941 and onwards. Cephalalgia. 2010;30(7):780–92.
Olesen J. International classification of headache disorders. Lancet Neurol. 2018;17:396–7.
Blau JN. Migraine prodromes separated from the aura: complete migraine. Br Med J. 1980;281(6241):658–60.
Giffin NJ, Lipton RB, Silberstein SD, Olesen J, Goadsby PJ. The migraine postdrome: an electronic diary study. Neurology. 2016;87(3):309–13.
• Lebedeva ER, Gurary NM, Gilev DV, Olesen J. Prospective testing of ICHD-3 beta diagnostic criteria for migraine with aura and migraine with typical aura in patients with transient ischemic attacks. Cephalalgia. 2018;38(3):561–7 A study showing that the revised migraine with aura criteria better differentiate migraine aura from TIA.
Russell MB, Rasmussen BK, Fenger K, Olesen J. Migraine without aura and migraine with aura are distinct clinical entities: a study of four hundred and eighty-four male and female migraineurs from the general population. Cephalalgia. 1996;16(4):239–45.
Eriksen MK, Thomsen LL, Olesen J. The Visual Aura Rating Scale (VARS) for migraine aura diagnosis. Cephalalgia. 2005;25(10):801–10.
Bickerstaff ER. Impairment of consciousness in migraine. Lancet. 1961;2(7211):1057–9.
Kirchmann M, Thomsen LL, Olesen J. Basilar-type migraine: clinical, epidemiologic, and genetic features. Neurology. 2006;66(6):880–6.
Li D, Christensen AF, Olesen J. Field-testing of the ICHD-3 beta/proposed ICD-11 diagnostic criteria for migraine with aura. Cephalalgia. 2015;35(9):748–56.
Leao AA. Spreading depression of activity in the cerebral cortex. J Neurophysiol. 1944;7(6).
Sugaya E, Takato M, Noda Y. Neuronal and glial activity during spreading depression in cerebral cortex of cat. J Neurophysiol. 1975;38(4):822–41.
Shinohara M, Dollinger B, Brown G, Rapoport S, Sokoloff L. Cerebral glucose utilization: local changes during and after recovery from spreading cortical depression. Science. 1979;203(4376):188–90.
Busija DW, Bari F, Domoki F, Horiguchi T, Shimizu K. Mechanisms involved in the cerebrovascular dilator effects of cortical spreading depression. Prog Neurobiol. 2008;86(4):379–95.
Cutrer FM, Sorensen AG, Weisskoff RM, Ostergaard L, Sanchez del Rio M, Lee EJ, et al. Perfusion-weighted imaging defects during spontaneous migrainous aura. Ann Neurol. 1998;43(1):25–31.
•• Hadjikhani N, Sanchez Del Rio M, Wu O, Schwartz D, Bakker D, Fischl B, et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci U S A. 2001;98(8):4687–92 Imaging study showing that migraine aura is caused by cortical spreading depression.
Richter F, Lehmenkuhler A. Cortical spreading depression (CSD): a neurophysiological correlate of migraine aura. Schmerz. 2008;22(5):544–6 8-50.
Moskowitz MA. Neurogenic inflammation in the pathophysiology and treatment of migraine. Neurology. 1993;43(6 Suppl 3):S16–20.
Zhang X, Levy D, Kainz V, Noseda R, Jakubowski M, Burstein R. Activation of central trigeminovascular neurons by cortical spreading depression. Ann Neurol. 2011;69(5):855–65.
Hougaard A, Amin FM, Christensen CE, Younis S, Wolfram F, Cramer SP, et al. Increased brainstem perfusion, but no blood-brain barrier disruption, during attacks of migraine with aura. Brain. 2017;140(6):1633–42.
May A, Goadsby PJ. Substance P receptor antagonists in the therapy of migraine. Expert Opin Investig Drugs. 2001;10(4):673–8.
Goldstein DJ, Offen WW, Klein EG, Phebus LA, Hipskind P, Johnson KW, et al. Lanepitant, an NK-1 antagonist, in migraine prevention. Cephalalgia. 2001;21(2):102–6.
May A, Gijsman HJ, Wallnofer A, Jones R, Diener HC, Ferrari MD. Endothelin antagonist bosentan blocks neurogenic inflammation, but is not effective in aborting migraine attacks. Pain. 1996;67(2–3):375–8.
Borgdorff P. Arguments against the role of cortical spreading depression in migraine. Neurol Res. 2018;40(3):173–81.
Brennan KC, Pietrobon D. A systems neuroscience approach to migraine. Neuron. 2018;97(5):1004–21.
Charles AC, Baca SM. Cortical spreading depression and migraine. Nat Rev Neurol. 2013;9(11):637–44.
Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol. 2013;75:365–91.
Hauge AW, Asghar MS, Schytz HW, Christensen K, Olesen J. Effects of tonabersat on migraine with aura: a randomised, double-blind, placebo-controlled crossover study. Lancet Neurol. 2009;8(8):718–23.
Tozzi A, de Iure A, Di Filippo M, Costa C, Caproni S, Pisani A, et al. Critical role of calcitonin gene-related peptide receptors in cortical spreading depression. Proc Natl Acad Sci U S A. 2012;109(46):18985–90.
Piper RD, Edvinsson L, Ekman R, Lambert GA. Cortical spreading depression does not result in the release of calcitonin gene-related peptide into the external jugular vein of the cat: relevance to human migraine. Cephalalgia. 1993;13(3):180–3 discussion 49.
Ebersberger A, Schaible HG, Averbeck B, Richter F. Is there a correlation between spreading depression, neurogenic inflammation, and nociception that might cause migraine headache? Ann Neurol. 2001;49(1):7–13.
•• Schulte LH, May A. The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain. 2016;139(Pt 7):1987–93 Study showing that the hypothalamus is involved in generation of a migraine attack.
Mahmoud AN, Mentias A, Elgendy AY, Qazi A, Barakat AF, Saad M, et al. Migraine and the risk of cardiovascular and cerebrovascular events: a meta-analysis of 16 cohort studies including 1 152 407 subjects. BMJ Open. 2018;8(3):e020498.
Lantz M, Sieurin J, Sjolander A, Waldenlind E, Sjostrand C, Wirdefeldt K. Migraine and risk of stroke: a national population-based twin study. Brain. 2017;140(10):2653–62.
Kurth T, Winter AC, Eliassen AH, Dushkes R, Mukamal KJ, Rimm EB, et al. Migraine and risk of cardiovascular disease in women: prospective cohort study. BMJ. 2016;353:i2610.
• Adelborg K, Szepligeti SK, Holland-Bill L, Ehrenstein V, Horvath-Puho E, Henderson VW, et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. BMJ. 2018;360:k96 Observational study showing increased risk of cardiovascular disease in migraine with aura.
Tietjen GE, Collins SA. Hypercoagulability and migraine. Headache. 2018;58(1):173–83.
Bashir A, Lipton RB, Ashina S, Ashina M. Migraine and structural changes in the brain: a systematic review and meta-analysis. Neurology. 2013;81(14):1260–8.
Hauge AW, Hougaard A, Olesen J. On the methodology of drug trials in migraine with aura. Cephalalgia. 2010;30(9):1041–8.
Ayata C, Jin H, Kudo C, Dalkara T, Moskowitz MA. Suppression of cortical spreading depression in migraine prophylaxis. Ann Neurol. 2006;59(4):652–61.
Lampl C, Katsarava Z, Diener HC, Limmroth V. Lamotrigine reduces migraine aura and migraine attacks in patients with migraine with aura. J Neurol Neurosurg Psychiatry. 2005;76(12):1730–2.
Pascual J, Caminero AB, Mateos V, Roig C, Leira R, Garcia-Monco C, et al. Preventing disturbing migraine aura with lamotrigine: an open study. Headache. 2004;44(10):1024–8.
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the quality standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337–45.
Bogdanov VB, Multon S, Chauvel V, Bogdanova OV, Prodanov D, Makarchuk MY, et al. Migraine preventive drugs differentially affect cortical spreading depression in rat. Neurobiol Dis. 2011;41(2):430–5.
Reuter U, Del Rio MS, Diener HC, Allais G, Davies B, Gendolla A, et al. Migraines with and without aura and their response to preventive therapy with topiramate. Cephalalgia. 2010;30(5):543–51.
Alemdar M, Akman O, Selekler H, Komsuoglu S, Ates N. Does metoprolol inhibit the cortical spreading depression? Acute effects of systematic metropol on CSD in rats. Cephalalgia. 2007;27(9):1010–3.
Bates D, Ashford E, Dawson R, Ensink FB, Gilhus NE, Olesen J, et al. Subcutaneous sumatriptan during the migraine aura. Sumatriptan Aura Study Group. Neurology. 1994;44(9):1587–92.
Banerjee M, Findley LJ. Sumatriptan in the treatment of acute migraine with aura. Cephalalgia. 1992;12(1):39–44.
Aurora SK, Barrodale PM, McDonald SA, Jakubowski M, Burstein R. Revisiting the efficacy of sumatriptan therapy during the aura phase of migraine. Headache. 2009;49(7):1001–4.
Bu F, Du R, Li Y, Quinn JP, Wang M. NR2A contributes to genesis and propagation of cortical spreading depression in rats. Sci Rep. 2016;6:23576.
Kaube H, Herzog J, Kaufer T, Dichgans M, Diener HC. Aura in some patients with familial hemiplegic migraine can be stopped by intranasal ketamine. Neurology. 2000;55(1):139–41.
Afridi SK, Giffin NJ, Kaube H, Goadsby PJ. A randomized controlled trial of intranasal ketamine in migraine with prolonged aura. Neurology. 2013;80(7):642–7.
Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015;55(1):3–20.
Lipton RB, Dodick DW, Silberstein SD, Saper JR, Aurora SK, Pearlman SH, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9(4):373–80.
Rozen TD. Treatment of a prolonged migrainous aura with intravenous furosemide. Neurology. 2000;55(5):732–3.
de Almeida RF, Leao IA, Gomes JB, da Silva AA Jr, Teixeira AL. Migraine with persistent visual aura: response to furosemide. Clinics (Sao Paulo). 2009;64(4):375–6.
Lim J, Jo KD, Lee MK, Jang W. Persistent negative visual aura in migraine without headache: a case report. J Med Case Rep. 2014;8:61.
Amin FM, Asghar MS, Ravneberg JW, de Koning PJ, Larsson HB, Olesen J, et al. The effect of sumatriptan on cephalic arteries: a 3T MR-angiography study in healthy volunteers. Cephalalgia. 2013;33(12):1009–16.
Artto V, Nissila M, Wessman M, Palotie A, Farkkila M, Kallela M. Treatment of hemiplegic migraine with triptans. Eur J Neurol. 2007;14(9):1053–6.
Klapper J, Mathew N, Nett R. Triptans in the treatment of basilar migraine and migraine with prolonged aura. Headache. 2001;41(10):981–4.
Mathew PG, Krel R, Buddhdev B, Ansari H, Joshi SG, Spinner WD, et al. A retrospective analysis of triptan and the use for basilar and hemiplegic migraine. Headache. 2016;56:841–8.
• Pelzer N, Stam AH, Haan J, Ferrari MD, Terwindt GM. Familial and sporadic hemiplegic migraine: diagnosis and treatment. Curr Treat Options Neurol. 2013;15(1):13–27 Comprehensive review of management of hemiplegic migraine.
Kurth T, Diener HC, Buring JE. Migraine and cardiovascular disease in women and the role of aspirin: subgroup analyses in the Women’s Health Study. Cephalalgia. 2011;31(10):1106–15.
Turk WE, Uiterwijk A, Pasmans R, Meys V, Ayata C, Koehler PJ. Aspirin prophylaxis for migraine with aura: an observational case series. Eur Neurol. 2017;78(5–6):287–9.
Anoaica MB, Anoaica PG, Popescu F. Acetylsalicylic acid in migraine with aura prevention - a retrospective study. Curr Health Sci J. 2014;40(2):126–8.
CDC. US Medical Eligibility Criteria (US MEC) for contraceptive use. In: Services HaH, editor. 2017.
Calhoun AH, Gill N. Presenting a new, non-hormonally mediated cyclic headache in women: end-menstrual migraine. Headache. 2017;57(1):17–20.
Sheikh HU, Pavlovic J, Loder E, Burch R. Risk of stroke associated with use of estrogen containing contraceptives in women with migraine: a systematic review. Headache. 2018;58(1):5–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Angeliki Vgontzas and Rebecca Burch declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Episodic Migraine
Rights and permissions
About this article
Cite this article
Vgontzas, A., Burch, R. Episodic Migraine With and Without Aura: Key Differences and Implications for Pathophysiology, Management, and Assessing Risks. Curr Pain Headache Rep 22, 78 (2018). https://doi.org/10.1007/s11916-018-0735-z
Published:
DOI: https://doi.org/10.1007/s11916-018-0735-z