Abstract
Purpose of Review
Skeletal metastasis involves the uncoupling of physiologic bone remodeling resulting in abnormal bone turnover and radical changes in bony architecture, density, and quality. Bone strength assessment and fracture risk prediction are critical in clinical treatment decision-making. This review focuses on bone tissue and structural mechanisms altered by osteolytic metastasis and the resulting changes to its material and mechanical behavior.
Recent Findings
Both organic and mineral phases of bone tissue are altered by osteolytic metastatic disease, with diminished bone quality evident at multiple length-scales. The mechanical performance of bone with osteolytic lesions is influenced by a combination of tissue-level and structural changes.
Summary
This review considers the effects of osteolytic metastasis on bone biomechanics demonstrating its negative impact at tissue and structural levels. Future studies need to assess the cumulative impact of cancer treatments on metastatically involved bone quality, and its utility in directing multimodal treatment planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone metastases frequently occur in patients with breast, lung, prostate, and renal cancers [1,2,3]. Bone metastases can lead to skeletal-related events (SREs) which include pathologic fractures, pain, compression syndromes of the nerve root or spinal cord, and metabolic disturbances [4, 5]. SREs increase mortality and significantly impact a patient’s quality of life, physical function, and health resource utilization [6, 7]. The risk of SREs is increased for all types of bone metastases which can present as osteoblastic (bone generating), osteolytic (bone destructive), or a mixture of the two [8]. Osteolytic metastases are more common and aggressive than osteoblastic metastases and have been associated with a higher incidence of pathologic fractures [9, 10]. Bone strength assessment and fracture risk prediction are critically important in guiding clinical treatment decisions aimed at preventing and/or lessening the burden of SREs, particularly as bone metastasis evolves to a more chronic disease state.
A literature search was performed to evaluate the current understanding of the effects of osteolytic metastatic disease on bone biomechanics. This review focuses on the bone tissue and structural mechanisms altered by pathology and the resulting changes to material and mechanical behavior. Moreover, it also considers research spanning from in vitro studies through preclinical analyses to clinical data.
Osteolytic Bone Quality and Biomechanics
Osteolytic bone metastases affect multiple length-scales including the whole bone, mesoscale, microscale, and nanoscale [46]. Due to bone’s hierarchical structure, the mechanical testing of bone at different physical scales is useful in isolating the origin of potential factors leading to decreased bone quality seen clinically (Table 1) [47].
Bone Matrix
Bone tissue is a composite material consisting of a combination of organic and mineral phases. Collagen fibers are the major components of the organic phase and hydroxyapatite crystals account for the majority of the mineral phase. Features within the organic phase which are used to assess bone quality include the structure and organization of collagen-I fibrils and the type and amount of collagen cross-links. The size of hydroxyapatite crystal deposits, degree of carbonation of the crystals, and the heterogeneity of mineral distribution are useful in describing the quality of the mineral phase.
Organic Phase
Collagen fibril organization, morphology, and packing contribute to the mechanical properties of bone [48]. The rectilinear array of collagen-I fibrils has been shown to contribute to the toughness of bone [49,50,51]. Collagen organization has also been shown to affect modulus and hardness [52, 53]. Osteolytic metastatic involvement has been shown to impact collagen organization in both trabecular and cortical bone, with increased collagen fibril disorganization associated with reduced hardness and modulus [18, 38,39,40]. While modifications in collagen fibril diameter have been associated with changes in intrafibrillar cross-linking, which in turn have been associated with changes in bone strength and post-yield properties [41,42,43], no significant differences have been seen between the collagen fibril diameter of osteolytic and healthy bone [38].
Type I collagen fibrils are stabilized in part by trivalent mature pyridinium cross-links: pyridinoline (pyr), deoxypyridinoline (dpyr), and pyrrole [11]. Unfolding of these collagen cross-links enables the bone to absorb extra energy without breaking [54]. Reductions in collagen cross-links have been correlated with a lowered bending strength and elastic modulus of bone [43]. Additionally, advanced glycation end products (AGEs) such as pentosidine form cross-links between collagen fibrils [55], reducing its ability to “unfold” [54]. An increase in pentosidine concentrations is associated with diminished bone ductility, toughness, and post-yield properties and may act as a marker for oxidative stress [56]. Human vertebrae with reduced compressive biomechanical properties have shown elevated non-enzymatic glycation and beta isomerization of type I collagen [57]. Recent studies have shown that osteolytic bone metastasis leads to an increase in pentosidine concentration and decrease in pyr and dpyr concentration and results in a bone with inferior cross-linking chemistry [11, 38]. An important feature of tumor tissue is its high glycolytic flow, producing dicarbonyl glyoxals and methyl glyoxals, causing tissue inflammation. Cancer cells protect themselves against these aldehydes by producing glyoxylases, increasing the production of AGEs [58]. In addition to glyoxylases, tumor cells also overproduce hydroxylation enzymes such as prolyl hydroxylase [13] and lysyl hydroxylase [59], generating reactive oxygen species (ROS) [60]. This can impact the cross-linkage pathway through the hydroxylation of collagen chain amino acids like proline and change the biochemistry as well as the mechanical behavior of bone. Literature has reported altered hydroxyproline-to-proline ratios, indicating the deterioration of the collagen cross-link chemistry and compromise in the mechanical properties of bone with osteolytic involvement [11, 38].
Mineral Phase
Numerous studies have highlighted the impact of metastatic disease on the mineral density and distribution of trabecular bone [19, 24, 61, 62]. A preclinical study examining the impact of metastasis on the mineral phase of vertebral bone tissue reported a slight increase in the tissue mineral homogeneity of osteolytic bone [16]. This increase in localized mineral homogeneity could lead to increased bone brittleness and fracture risk [44, 45]. Osteolytic bone has also been shown to reduce the tissue mineral content [16] which has a strong correlation to trabecular bone modulus and hardness [18].
Hydroxyapatite (HA) provides bone with its rigidity and changes in its chemistry can compromise the mechanical strength of the bone [14]. Previous studies have shown that metastasis can influence HA crystal composition and size and that these alterations can influence metastasis [14, 63]. He et al. reported a decrease in HA crystal size and quality in both tumor-involved and non-tumor-involved bone and suggested that the less mature HA crystal in non-tumor bone may further attract more tumor cells to bone [62]. Osteolytic bone metastases have been reported to increase the carbonation of the HA lattice and decrease the lattice strain [64]. Burke et al. showed that osteolytic bone metastasis leads to a higher carbonate-to-phosphate ratio and lower carbonate-to-matrix ratio [11], resulting in a bone vulnerable to fracture and susceptible to further tumor invasion. Further experiments by this group indicated that there was a reduced HA crystal width and lowered average mineral content in osteolytic bone, yielding a bone with lower modulus and hardness [16]. These changes in the crystal chemistry may be due to the overexpression of bone sialoproteins (BSP), the nucleation proteins responsible for initiating hydroxyapatite crystal mineralization [65]. BSP overexpression increases the number of nucleation sites and the number of mineral crystals, but lowers the size of these crystals due to spatial and ion constraints. As a result, tumor-involved bone has mineral crystals with smaller size, more carbonation, and inferior mechanical quality [16].
Tissue-Level Mechanical Properties
The mechanical properties of bone can be measured at various length-scales using dynamic and quasi-static indentation testing. During indentation testing, tissue hardness and elastic modulus can be determined from force-displacement curves which are generated as the indenter loads and unloads the bone tissue. Microindentation (~ 5 to ~200 μm) and nanoindentation (~ 0.1 to ~ 10 μm) have been used to determine the hardness and modulus of bone tissue [66].
Nanoindentation has been used to characterize the hardness and modulus of metastatic lesions. A reduction in hardness and modulus has been demonstrated in metastatically involved human vertebral bone; however, this study did not distinguish between the osteoblastic and osteolytic natures of the samples [19]. Other metastatic bone models have suggested reduced bone tissue modulus with breast cancer involvement [67]. In contrast, nanoindentation performed on osteolytic metastatic rat vertebrae found no significant tissue-level differences between the hardness and modulus of osteolytic and healthy samples [18].
Indentation techniques have been used to determine fracture toughness; however, the accuracy of these methods may be overly simplified for use in bone [68, 69]. Notch tests or testing of cantilever beams has been used on cortical bone tissue to quantify fracture toughness [70, 71], but such testing has not been applied to bone impacted by osteolytic metastases. Opportunities exist to determine bone fracture toughness in trabecular bone and metastatically involved bone tissue through the creation and compression of micropillars of bone tissue (i.e., via ion beam milling) [72, 73]. Scratch tests could also be used to evaluate bone toughness on a microscale [74,75,76]. However, no such tests have yet been performed on osteolytic metastatic bone tissue.
Microdamage
Under normal physiology, microscopic tissue damage (microdamage formation) within bone tissue serves as a stimulant for bone remodeling. However, accumulation of unrepaired microdamage can be associated with clinical fracture susceptibility, especially fractures associated with age and osteolytic bone [77]. Deterioration of quality in osteolytic bone is evident when microdamage accumulation is visualized in the tissue (i.e., through histologic staining (i.e., calcein green) or micro-CT and/or backscatter electron imaging following barium sulfate staining). Accumulated microdamage negatively impacts the mechanical strength of bone, including reductions to elastic modulus and strength [17, 78]. Computational modeling has shown significantly higher stresses and strains in the damaged region of osteolytic vertebrae, which agrees with higher levels of accumulated microdamage [79] .
Structural Changes
At a macro level, skeletal metastasis affects the natural resorption cycle of bone. In osteolytic metastases, bone loss can be measured as a loss of trabecular architecture and through volumetric measurements of lesions within the bone tissue [9, 80,81,82]. Deviations from the healthy structure of bone tissue are associated with diminished mechanical integrity. Osteolytic defects have been shown to reduce the mechanical stability of bones; however, accurate quantification of the impact must consider more than bone loss (lesion size) alone [25, 29, 32, 83].
Architecture
To understand the effects of metastatic tumors on trabecular architecture, microcomputed tomography has been used to quantify morphological parameters of bone tissue in preclinical models. Stereological parameters including trabecular thickness, trabecular number, trabecular spacing, and trabecular bone volume have been used to quantify changes in architecture of bone in osteolytic murine models in the femurs and the spinal column [64, 84]. The architecture of osteolytic trabecular bone has been characterized by decreased trabecular number and thickness and increased trabecular spacing when compared with non-pathologic bone [18,19,20,21, 61, 64].
Mechanical Properties
At a macro level, mechanical testing is used to determine mechanical properties (stiffness, strength, rigidity) to better understand how disease and treatments affect mechanical stability. The mechanical strength of bones is affected by both material properties and architecture. In the context of mechanical testing, simulated defects in bone are often created to represent architectural changes caused by osteolytic disease [25,26,27, 33, 34, 85]. However, the lack of inclusion of tumor tissue and changes to tissue-level bone material properties in these models may limit their clinical relevance [33]. There are limited experimental studies that have tested mechanical performance of osteolytic disease in human tissue due to the inaccessibility of specimens [19, 22, 35]. Animal models of skeletal metastatic disease have been widely used in this context as they can incorporate both architectural and tissue material differences to better replicate osteolytic lesions when compared with simulated defects [18, 20, 30, 64, 84].
Catastrophic failure can present as varying fracture patterns depending on the loading scenario and bone specimen structure. Clinically, the presence of osteolytic metastasis in the spine has been associated with burst fracture patterns, but therapeutic treatments have lessened this type of catastrophic failure, with compression fracture patterns now more commonly observed [86,87,88]. Applied loading in experimental simulations (axial compression and bending, at differing loading rates) affects the resulting fracture location and type [89, 90]. In long bones, three-point bending methods are commonly used in osteoporosis to evaluate changes in mechanical properties. In osteolytic metastases, due to the focal nature of the lesions, long bones are more commonly tested in torsion [26].
Vertebral Testing
Axial compressive testing has been used to characterize vertebral structural integrity in the presence of osteolytic lesions in bone cores [19, 22], whole vertebrae [20, 23], and spinal motion segments [17, 18, 21]. All studies have found decreases in vertebral mechanical stability in the presence of metastatic disease (reduced stiffness, ultimate force, axial rigidity) [17,18,19,20,21,22,23]. Biomechanical testing performed through vertebral motion segments better represents physiological loading through the intervertebral discs and posterior elements, enabling representation of both burst and compression fracture patterns.
Researchers have observed correlations between stereological features and mechanical behavior of bone tissue with osteolytic lesions under compressive loads. In vertebrae, relations have been identified between both stiffness and strength with bone/tissue volume ratio, as well as between ultimate force and bone mineral density [15, 19]. However, bone tissue mineral density alone was not a strong indicator of macroscopic behavior [19]. Not surprisingly, osteolytic involvement has been reported to have a reduced vertebral trabecular bone volume, axial rigidity, stiffness, and failure force when compared with healthy controls [18].
Computed tomography images can be used to calculate structural rigidity measures, which are dependent on both material modulus, cross-sectional area of bone, and material distribution. Imaging-based bending rigidity measures have been correlated to mechanical failure in biomechanical testing experiments [18, 31, 33, 61, 83]. Torsional biomechanical testing has been used to determine torsional rigidity and ultimate torque in vertebral bone cores with lytic lesions. Biomechanical measurements of yielding in torsion, in bending, and in tension were highly correlated (R2 > 0.9) with the corresponding imaging-derived rigidity measures, i.e., torsional, flexural, and axial rigidity, respectively [31].
Long Bone Testing
Torsional testing is most commonly used in evaluating the mechanical behavior of long bones with osteolytic involvement. Using this approach, femurs with osteolytic metastases have demonstrated reduced maximum torque and rigidity when compared with healthy controls in preclinical, simulated cadaveric, and computer models [26, 29, 31]. Torque and failure energy have been seen to have moderate correlation with BMD [30].
Loading to the femoral head is often applied to represent anatomical loading scenarios, yielding a combination of axial compression and bending in the femur. As expected, such studies have found decreased failure loads and stiffness in samples with osteolytic disease [22, 24,25,26,27]. Location of the lesion impacts the stiffness and ultimate strength measures [27, 28].
Computer Modeling
Finite element (FE) models, validated with in vitro experimental mechanical testing, have been utilized to better understand the impact of metastatic disease on bone stress and strain distribution. These models have been shown to accurately predict experimental results (apparent stiffness, ultimate strength) [17, 20, 22, 26, 32,33,34,35,36,37]; however, application to clinical datasets remains a challenge. While earlier parametric models were used to examine the impact of features, such as tumor size, location, material properties, and loading, on vertebral stress and strain patterns, more recent modeling has focused on specimen-specific image-based models. A notable limitation of modeling studies is neglecting the material properties of tumor and the effects of tumor or treatment on the material properties of the surrounding tissue. Validation of finite element analysis (FEA) has primarily been performed against ex vivo bone with voids created to mimic tumor shapes. Automated methods for segmentation of vertebrae and osteolytic disease from CT data facilitate generation of specimen-specific FE models [91,92,93,94]. Similar approaches have been taken in segmentation of vertebrae and metastatic disease in preclinical models based on micro-CT and micro-MRI data [21].
While continuum models have been generally created from clinical imaging, micro-CT-based models have been used to generate micro-FE models of vertebrae with metastatic disease. Such models have been shown to correlate strain with the generation of load-induced microdamage [17, 79] and suggested that microdamage may be generated at lower load strain levels in metastatically involved tissue. The current work has extended micro-FE modeling to represent post-yield behavior with the addition of cohesive elements—such work has demonstrated agreement with damage generated through in vitro mechanical testing in healthy and osteoblastic vertebrae [95, 96]. Further, this work has demonstrated that metastatic involvement affects the damage properties of bone tissue.
Clinical Biomechanics
Understanding the biomechanics of bone with metastatic involvement is important for clinical decision-making, considering treatment options, monitoring response to therapy, and disease progression. Many clinical factors have been identified that contribute to the instability of metastatically involved bone. The presence of existing fractures (consistent with patients without cancer) is a risk factor for future fracture [97]. In the bony spine, the malalignment of the spine (presence of scoliosis, kyphotic deformity, or vertebral subluxation or translation) also impacts risk [98]. Lung and liver tumors, older patient age, and higher pain levels have also been associated with increased risk of fracture [88, 97].
Clinical scoring tools have been used to make decision-making that involves combining of these many factors easier and more consistent. Scoring tools focus on determining the risk of instability in patients with skeletal metastases and can be used to triage patients deemed stable and direct interventions in those at risk of fracture or fracture progression, neurological compromise, or mechanical pain. A number of clinical scoring tools are used in the context of skeletal metastases including the Spinal Instability Neoplastic Score (SINS), Bilsky tumor grading in the spine, the Thoracolumbar Injury Classification and Severity Score (TLICS), and Mirels’ scoring system (long bones) [99,100,101]. SINS has been shown to have good intra- (0.886) and inter-rater (0.846) reproducibility [102, 103], although it lacks objectivity based on quantitative metrics. Defining spinal neoplastic-related instability and the introduction of SINS have led to improved uniform reporting within the spinal neoplastic literature; however, the prognostic value of SINS remains controversial [103].
CT-based structural rigidity analysis, calculated on transaxial CT images, has also been applied clinically in the identification of metastatically involved bone at risk of fracture. Prediction of the reduction in fracture risk based on CT-based structural rigidity at the lesion (> 35% in axial, bending, or torsional rigidities) has been shown to be better than Mirels’ scoring in predicting femoral impending pathologic fracture [104]. CT-based structural rigidity outcome measures applied to the metastatic spine have yielded 100% sensitivity, with 44 to 70% specificity, to predict fracture risk [105]. Volumetric assessments of tumor burden and dynamic quantification of bone density changes on CT imaging have also been shown to distinguish between those patients at risk of fracture and those who remain stable [106, 107]. Further complication in the bony spine is that many vertebral compression fractures will not require mechanical stabilization; they may be mechanically stable, with the presence of local healing showing a relationship with long-term stability [108].
Specimen-specific FEA presents an alternative to structural rigidity analysis that is potentially more sensitive to changes in tissue properties and loading conditions at the expense of greater complexity. Biomechanical models generated from FEA that quantify vertebral stability have been applied to clinical datasets with some success [107, 109,110,111], highlighting the ability of biomechanically based guidelines to yield quantitative metrics that may aid in clinical decision-making and intervention guidelines [22, 34, 112]. However, such approaches will require automated pipelines to realize clinical value. Current endeavors in the area of machine learning may facilitate this translation [113] with some recent work applied in the area of spinal metastases [94, 114, 115].
Treatment Effects
Treatments for skeletal bone metastases are designed to decrease pain, improve structural stability and mobility, and control tumor growth. Treatment decisions regarding metastatic spine disease are dependent on multiple factors including clinical symptoms, the presence of neurological deficits, tumor pathology, anticipated radiosensitivity, mechanical stability, the extent of disease, and the available therapeutic modalities. Treatments are often multimodal and may consist of systemic drugs (i.e., chemotherapeutics, Rank-L inhibitors, bisphosphonates), local treatments (i.e., radiotherapy, radiofrequency ablation), and structural stabilization techniques (i.e., vertebroplasty, kyphoplasty, open surgery, and hardware). The impact of such treatments on bone quality is critical in understanding their impact on mechanical stability.
Radiation therapy is commonly used for treatment of metastatic bone tumors; however, in the movement towards localized control with stereotactic body radiotherapy (SBRT), the incidence of post-treatment fractures has increased with post-SBRT vertebral compression fractures occurring in approximately 11% of patients [3, 116,117,118,119]. As such, the focal impact of SBRT on bone quality [120,121,122] must be considered in the context of treatment planning and patient selection.
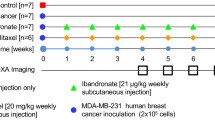
Mechanical and material properties of healthy and metastatically involved bone have also been assessed for treatments such as bisphosphonates [123,124,125,126,127,128], chemotherapeutics [129,130,131,132], photodynamic therapy (PDT) [15, 133], Rank-L inhibitors [134,135,136,137], and multimodal treatment combinations [138, 139]. Bisphosphonates and Rank-L inhibitors slow down bone turnover, leading to increased bone mineralization and slower osteolytic tumor growth. Clinically, bisphosphonates have been shown to reduce the risk of skeletal-related events in patients with bone metastases (relative risk (RR) = 0.85) and Rank-L inhibitors further reduce the risk compared with bisphosphonate treatment (RR = 0.78) [140]. Bisphosphonate use has been associated with osteonecrosis of the jaw, albeit rarely (0.5%), in breast cancer patients [140]. Atypical femur fracture has also been reported in patients with bone metastases undergoing antiresorptive therapies (denosumab (anti-Rank-L antibody) and bisphosphonates) at varying levels [141]. In a recent study, Ota et al. reported atypical femur fracture in 7.8% of breast cancer patients with bone metastasis who received antiresorptive agents (denosumab and/or bisphosphonates (zoledronic acid)) compared with no atypical fractures in those who did not receive antiresorptive agents [142]. The true incidence of atypical femur fracture among cancer patients on antiresorptive therapy is not currently known due to the lack of large studies [141]. PDT has shown increased apparent mechanical strength (40% increase) and bone mass (45% increase) in preclinical experiments with clinical trials needed to verify these findings [133]. Owing to the growing arsenal of treatments, there is a need to assess the impact of cancer treatments on bone quality in osteolytic bone at various length-scales to assist with multimodal treatment planning.
Conclusion
Osteolytic bone disease and associated treatments affect the material, mechanical, and structural properties of bone tissue. Bone quality assessment and fracture risk prediction are critical in determining the need for intervention and guiding multimodal treatment planning of osteolytic metastatic bone disease. Owing to the hierarchical structure of bone, it is essential to characterize the parameters that impact the mechanical integrity of metastatically involved bone at a nano, micro, meso, and whole-bone levels. No tissue or structural parameter alone has been able to completely explain the mechanical performance of bone with osteolytic lesions. An increased understanding of treatment options, including their biomechanical sequelae, can hopefully reduce the incidence of pathologic fractures in the metastatically involved skeleton, leading to reductions in health resource utilization and improvement in the quality of life for the growing number of patients with these lesions.
References
Janjan N. Bone metastases: approaches to management. Semin Oncol. 2001;28:28–34.
Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27:165–76.
Macedo F, Ladeira K, Pinho F, Saraiva N, Bonito N, Pinto L, et al. Bone metastases: an overview. Oncol Rev. 2017;11:321.
Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004;350:1655–64.
Lipton A, Theriault RL, Hortobagyi GN, Simeone J, Knight RD, Mellars K, et al. Pamidronate prevents skeletal complications and is effective palliative treatment in women with breast carcinoma and osteolytic bone metastases: long term follow-up of two randomized, placebo-controlled trials. Cancer. 2000;88:1082–90.
Hoefeler H, Duran I, Hechmati G, Rodriguez CG, Lüftner D, Ashcroft J, et al. Health resource utilization associated with skeletal-related events in patients with bone metastases: results from a multinational retrospective - prospective observational study - a cohort from 4 european countries. J Bone Oncol. 2014;3:40–8.
Hussain A, Lee RJ, Graff JN, Halabi S. The evolution and understanding of skeletal complication endpoints in clinical trials of tumors with metastasis to the bone. Crit Rev Oncol Hematol. 2019;139:108–16.
Vassiliou V, Kalogeropoulou C, Petsas T, Leotsinidis M, Kardamakis D. Clinical and radiological evaluation of patients with lytic, mixed and sclerotic bone metastases from solid tumors: is there a correlation between clinical status of patients and type of bone metastases? Clin Exp Metastasis. 2007;24:49–56.
O’Sullivan GJ. Imaging of bone metastasis: an update. World J Radiol. 2015;7:202.
Singh VA, Haseeb A, Alkubaisi AAHA. Incidence and outcome of bone metastatic disease at University Malaya Medical Centre. Singapore Med J. 2014;55:539–46.
Burke MV, Atkins A, Akens M, Willett TL, Whyne CM. Osteolytic and mixed cancer metastasis modulates collagen and mineral parameters within rat vertebral bone matrix. J Orthop Res. 2016;34:2126–36.
Fohr B, Dunstan CR, Seibel MJ. Markers of bone remodeling in metastatic bone disease. J Clin Endocrinol Metab. 2003;88:5059–75.
Gilkes DM, Chaturvedi P, Bajpai S, Wong CC, Wei H, Pitcairn S, et al. Collagen prolyl hydroxylases are essential for breast cancer metastasis. Cancer Res. 2013;73:3285–96.
Pathi SP, Lin DDW, Dorvee JR, Estroff LA, Fischbach C. Hydroxyapatite nanoparticle-containing scaffolds for the study of breast cancer bone metastasis. Biomaterials. 2011;32:5112–22.
Won E, Wise-Milestone L, Akens MK, Burch S, Yee AJM, Wilson BC, et al. Beyond bisphosphonates: photodynamic therapy structurally augments metastatically involved vertebrae and destroys tumor tissue. Breast Cancer Res Treat. 2010;124:111–9.
Burke M, Atkins A, Kiss A, Akens M, Yee A, Whyne C. The impact of metastasis on the mineral phase of vertebral bone tissue. J Mech Behav Biomed Mater. 2017;69:75–84.
Choudhari C, Chan K, Akens MK, Whyne CM. μFE models can represent microdamaged regions of healthy and metastatically involved whole vertebrae identified through histology and contrast enhanced μCT imaging. J Biomech. 2016;49:1103–10.
Burke M, Akens M, Kiss A, Willett T, Whyne C. Mechanical behavior of metastatic vertebrae are influenced by tissue architecture, mineral content, and organic feature alterations. J Orthop Res. 2018;36:3013–22.
Nazarian A, Von Stechow D, Zurakowski D, Müller R, Snyder BD. Bone volume fraction explains the variation in strength and stiffness of cancellous bone affected by metastatic cancer and osteoporosis. Calcif Tissue Int. 2008;83:368–79.
Hardisty MR, Akens MK, Hojjat SP, Yee A, Whyne CM. Quantification of the effect of osteolytic metastases on bone strain within whole vertebrae using image registration. J Orthop Res. 2012;30:1032–9.
Hojjat SP, Foltz W, Wise-Milestone L, Whyne CM. Multimodal μcT/μMR based semiautomated segmentation of rat vertebrae affected by mixed osteolytic/osteoblastic metastases. Med Phys. 2012;39:2848–53.
Alexander GE, Gutierrez S, Nayak A, Palumbo BT, Cheong D, Letson GD, et al. Biomechanical model of a high risk impending pathologic fracture of the femur: lesion creation based on clinically implemented scoring systems. Clin Biomech. 2013;28:408–14.
Morton JJ, Bennison M, Lievers WB, Waldman SD, Pilkey AK. Failure behaviour of rat vertebrae determined through simultaneous compression testing and micro-CT imaging. J Mech Behav Biomed Mater. 2018;79:73–82.
Kaneko TS, Bell JS, Pejcic MR, Tehranzadeh J, Keyak JH. Mechanical properties, density and quantitative CT scan data of trabecular bone with and without metastases. J Biomech. 2004;37:523–30.
Lee T. Predicting failure load of the femur with simulated osteolytic defects using noninvasive imaging technique in a simplified load case. Ann Biomed Eng. 2007;35:642–50.
Mann KA, Lee J, Arrington SA, Damron TA, Allen MJ. Predicting distal femur bone strength in a murine model of tumor osteolysis. Clin Orthop Relat Res. 2008;466:1271–8.
Benca E, Reisinger A, Patsch JM, Hirtler L, Synek A, Stenicka S, et al. Effect of simulated metastatic lesions on the biomechanical behavior of the proximal femur. J Orthop Res. 2017;35:2407–14.
Tschirhart CE, Finkelstein JA, Whyne CM. Biomechanics of vertebral level, geometry, and transcortical tumors in the metastatic spine. J Biomech. 2007;40:46–54.
Entezari V, Basto PA, Vartanians V, Zurakowski D, Snyder BD, Nazarian A. Non-invasive assessment of failure torque in rat bones with simulated lytic lesions using computed tomography based structural rigidity analysis. J Biomech. 2011;44:552–6.
Arrington SA, Schoonmaker JE, Damron TA, Mann KA, Allen MJ. Temporal changes in bone mass and mechanical properties in a murine model of tumor osteolysis. Bone. 2006;38:359–67.
Hong J, Cabe GD, Tedrow JR, Hipp JA, Snyder BD. Failure of trabecular bone with simulated lytic defects can be predicted non-invasively by structural analysis. J Orthop Res. 2004;22:479–86.
Alkalay RN, Harrigan TP. Mechanical assessment of the effects of metastatic lytic defect on the structural response of human thoracolumbar spine. J Orthop Res. 2016;34:1808–19.
Oftadeh R, Karimi Z, Villa-Camacho J, Tanck E, Verdonschot N, Goebel R, et al. Curved beam computed tomography based structural rigidity analysis of bones with simulated lytic defect: a comparative study with finite element analysis. Sci Rep. 2016;6:1–12.
Derikx LC, van Aken JB, Janssen D, Snyers A, van der Linden YM, Verdonschot N, et al. The assessment of the risk of fracture in femora with metastatic lesions. J Bone Joint Surg Br. 2012;94-B:1135–42.
Anez-Bustillos L, Derikx LC, Verdonschot N, Calderon N, Zurakowski D, Snyder BD, et al. Finite element analysis and CT-based structural rigidity analysis to assess failure load in bones with simulated lytic defects. Bone. 2014;58:160–7.
Tanck E, van Aken JB, van der Linden YM, Schreuder HWWB, Binkowski M, Huizenga H, et al. Pathological fracture prediction in patients with metastatic lesions can be improved with quantitative computed tomography based computer models. Bone. 2009;45:777–83.
Mirzaei M, Zeinali A, Razmjoo A, Nazemi M. On prediction of the strength levels and failure patterns of human vertebrae using quantitative computed tomography (QCT)-based finite element method. J Biomech. 2009;42:1584–91.
Burke M, Golaraei A, Atkins A, Akens M, Barzda V, Whyne C. Collagen fibril organization within rat vertebral bone modified with metastatic involvement. J Struct Biol. 2017;199:153–64.
Sekita A, Matsugaki A, Ishimoto T, Nakano T. Synchronous disruption of anisotropic arrangement of the osteocyte network and collagen/apatite in melanoma bone metastasis. J Struct Biol. 2017;197:260–70.
Molla MS, Katti DR, Iswara J, Venkatesan R, Paulmurugan R, Katti KS. Prostate cancer phenotype influences bone mineralization at metastasis: a study using an in vitro prostate cancer metastasis testbed. JBMR Plus. 2020;4:e10256.
Saito M, Fujii K, Mori Y, Marumo K. Role of collagen enzymatic and glycation induced cross-links as a determinant of bone quality in spontaneously diabetic WBN/Kob rats. Osteoporos Int. 2006;17:1514–23.
Hernandez CJ, Tang SY, Baumbach BM, Hwu PB, Sakkee AN, Van Der Ham F, et al. Trabecular microfracture and the influence of pyridinium and non-enzymatic glycation-mediated collagen cross-links. Bone. 2005;37:825–32.
Oxlund H, Barckman M, Ørtoft G, Andreassen TT. Reduced concentrations of collagen cross-links are associated with reduced strength of bone. Bone. 1995;17:365–71.
Boskey AL, Spevak L, Weinstein RS. Spectroscopic markers of bone quality in alendronate-treated postmenopausal women. Osteoporos Int. 2009;20:793–800.
Renders GAP, Mulder L, van Ruijven LJ, Langenbach GEJ, van Eijden TMGJ. Mineral heterogeneity affects predictions of intratrabecular stress and strain. J Biomech. 2011;44:402–7.
Bailey S, Vashishth D. Mechanical characterization of bone: state of the art in experimental approaches - what types of experiments do people do and how does one interpret the results? Curr Osteoporos Rep. 2018;16:423–33.
Hernandez CJ, Keaveny TM. A biomechanical perspective on bone quality. Bone. 2006;39:1173–81.
Martin RB, Boardman DL. The effects of collagen fiber orientation, porosity, density, and mineralization on bovine cortical bone bending properties. J Biomech. 1993;26:1047–54.
Wang X, Shen X, Li X, Mauli AC. Age-related changes in the collagen network and toughness of bone. Bone. 2002;31:1–7.
Zimmermann EA, Busse B, Ritchie RO. The fracture mechanics of human bone: influence of disease and treatment. Bonekey Rep. 2015;4:743.
Launey ME, Buehler MJ, Ritchie RO. On the mechanistic origins of toughness in bone. Annu Rev Mater Res. 2010;40:25–53.
Zysset PK, Edward Guo X, Edward Hoffler C, Moore KE, Goldstein SA. Elastic modulus and hardness of cortical and trabecular bone lamellae measured by nanoindentation in the human femur. J Biomech. 1999;32:1005–12.
Lau ML, Lau KT, Yao Yeo YD, Au Yeung CT, Lee JH. Measurement of bovine bone properties through surface indentation technique. Mater Manuf Process. 2010;25:324–8.
Kawamura M, Masaki C, Shibata Y, Kondo Y, Mukaibo T, Miyazaki T, et al. Pentosidine correlates with nanomechanical properties of human jaw bone. J Mech Behav Biomed Mater. 2019;98:20–5.
Burton B, Gaspar A, Josey D, Tupy J, Grynpas MD, Willett TL. Bone embrittlement and collagen modifications due to high-dose gamma-irradiation sterilization. Bone. 2014;61:71–81.
Viguet-Carrin S, Garnero P, Delmas PD. The role of collagen in bone strength. Osteoporos Int. 2006;17:319–36.
Viguet-Carrin S, Roux JP, Arlot ME, Merabet Z, Leeming DJ, Byrjalsen I, et al. Contribution of the advanced glycation end product pentosidine and of maturation of type I collagen to compressive biomechanical properties of human lumbar vertebrae. Bone. 2006;39:1073–9.
Nass N, Ignatov A, Andreas L, Weißenborn C, Kalinski T, Sel S. Accumulation of the advanced glycation end product carboxymethyl lysine in breast cancer is positively associated with estrogen receptor expression and unfavorable prognosis in estrogen receptor-negative cases. Histochem Cell Biol. 2017;147:625–34.
Chen Y, Terajima M, Yang Y, Sun L, Ahn YH, Pankova D, et al. Lysyl hydroxylase 2 induces a collagen cross-link switch in tumor stroma. J Clin Invest. 2015;125:1147–62.
Storz P. Reactive oxygen species in tumor progression. Front Biosci. 2005;10:1881–96.
Wise-Milestone L, Akens MK, Rosol TJ, Hojjat SP, Grynpas MD, Whyne CM. Evaluating the effects of mixed osteolytic/osteoblastic metastasis on vertebral bone quality in a new rat model. J Orthop Res. 2012;30:817–23.
He F, Chiou AE, Loh HC, Lynch M, Seo BR, Song YH, et al. Multiscale characterization of the mineral phase at skeletal sites of breast cancer metastasis. Proc Natl Acad Sci USA. 2017;114(40):10542–7.
Zhu W, Wang M, Fu Y, Castro NJ, Fu SW, Zhang LG. Engineering a biomimetic three-dimensional nanostructured bone model for breast cancer bone metastasis study. Acta Biomater. 2015;14:164–74.
Bi X, Sterling JA, Merkel AR, Perrien DS, Nyman JS, Mahadevan-Jansen A. Prostate cancer metastases alter bone mineral and matrix composition independent of effects on bone architecture in mice - a quantitative study using microCT and raman spectroscopy. Bone. 2013;56:454–60.
Ibrahim T, Leong I, Sanchez-Sweatman O, Khokha R, Sodek J, Tenenbaum HC, et al. Expression of bone sialoprotein and osteopontin in breast cancer bone metastases. Clin Exp Metastasis. 2000;18:253–60.
Nyman JS, Granke M, Singleton RC, Pharr GM. Tissue-level mechanical properties of bone contributing to fracture risk. Curr Osteoporos Rep. 2016;14:138–50.
Richert L, Keller L, Wagner Q, Bornert F, Gros C, Bahi S, et al. Nanoscale stiffness distribution in bone metastasis. World J Nano Sci Eng. 2015;05:219–28.
Mullins LP, Bruzzi MS, McHugh PE. Measurement of the microstructural fracture toughness of cortical bone using indentation fracture. J Biomech. 2007;40:3285–8.
Kruzic JJ, Kim DK, Koester KJ, Ritchie RO. Indentation techniques for evaluating the fracture toughness of biomaterials and hard tissues. J Mech Behav Biomed Mater. 2009;2:384–95.
Ural A, Vashishth D. Cohesive finite element modeling of age-related toughness loss in human cortical bone. J Biomech. 2006;39:2974–82.
Morais JJL, de Moura MFSF, Pereira FAM, Xavier J, Dourado N, Dias MIR, et al. The double cantilever beam test applied to mode I fracture characterization of cortical bone tissue. J Mech Behav Biomed Mater. 2010;3:446–53.
Tertuliano OA, Greer JR. The nanocomposite nature of bone drives its strength and damage resistance. Nat Mater. 2016;15:1195–202.
Schwiedrzik J, Raghavan R, Bürki A, Lenader V, Wolfram U, Michler J, et al. In situ micropillar compression reveals superior strength and ductility but an absence of damage in lamellar bone. Nat Mater. 2014;13:740–7.
Kataruka A, Mendu K, Okeoghene O, Puthuvelil J, Akono AT. Microscopic assessment of bone toughness using scratch tests. Bone Reports. 2017;6:17–25.
Mendu K, Kataruka A, Puthuvelil J, Akono AT. Fragility assessment of bovine cortical bone using scratch tests. J Vis Exp. 2017;2017(129):56488.
Islam A, Neil Dong X, Wang X. Mechanistic modeling of a nanoscratch test for determination of in situ toughness of bone. J Mech Behav Biomed Mater. 2012;5:156–64.
Chapurlat RD, Delmas PD. Bone microdamage: a clinical perspective. Osteoporos Int. 2009;20:1299–308.
Diab T, Vashishth D. Effects of damage morphology on cortical bone fragility. Bone. 2005;37:96–102.
Atkins A, Burke M, Samiezadeh S, Akens MK, Hardisty M, Whyne CM. Elevated microdamage spatially correlates with stress in metastatic vertebrae. Ann Biomed Eng. 2019;47:980–9.
Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 2011;2011:1–12.
Hamaoka T, Madewell JE, Podoloff DA, Hortobagyi GN, Ueno NT. Bone imaging in metastatic breast cancer. J Clin Oncol. 2004;22:2942–53.
Heindel W, Gübitz R, Vieth V, Weckesser M, Schober O, Schäfers M. The diagnostic imaging of bone metastases. Dtsch Arztebl Int. 2014;111:741–7.
Whealan K, Kwak D, Tedrow JR, Inoue K, Snyder BD. Noninvasive imaging predicts failure load of the spine with simulated osteolytic defects. J Bone Jt Surgery. 2000;326–328:811–4.
Hojjat S-PP, Whyne CM. Automated quantitative microstructural analysis of metastatically involved vertebrae: effects of stereologic model and spatial resolution. Med Eng Phys. 2011;33:188–94.
Alkalay RN. Effect of the metastatic defect on the structural response and failure process of human vertebrae: an experimental study. Clin Biomech. 2015;30:121–8.
Skrinskas T, Clemons M, Freedman O, Weller I, Whyne CM. Automated CT-based analysis to detect changes in the prevalence of lytic bone metastases from breast cancer. Clin Exp Metastasis. 2009;26:97–103.
Hill ME, Richards MA, Gregory WM, Smith P, Rubens RD. Spinal cord compression in breast cancer: a review of 70 cases. Br J Cancer. 1993;68:969–73.
Cunha MVR, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012;84:343–9.
Whyne CM, Hu SS, Lotz JC. Burst fracture in the metastatically involved spine: development, validation, and parametric analysis of a three- dimensional poroelastic finite-element model. Spine (Phila Pa 1976). 2003;28:652–60.
Tschirhart CE, Nagpurkar A, Whyne CM. Effects of tumor location, shape and surface serration on burst fracture risk in the metastatic spine. J Biomech. 2004;37:653–60.
Campbell JQ, Petrella AJ. Automated finite element modeling of the lumbar spine: using a statistical shape model to generate a virtual population of models. J Biomech. 2016;49:2593–9.
Hardisty M, Gordon L, Agarwal P, Skrinskas T, Whyne C. Quantitative characterization of metastatic disease in the spine. Part I. Semiautomated segmentation using atlas-based deformable registration and the level set method. Med Phys. 2007;34:3127–34.
Whyne C, Hardisty M, Wu F, Skrinskas T, Clemons M, Gordon L, et al. Quantitative characterization of metastatic disease in the spine. Part II. Histogram-based analyses. Med Phys. 2007;34:3279–85.
Klein G, Martel A, Sahgal A, Whyne C. Hardisty M. In: Cai Y, Wang L, Audette M, Zheng G, Li S, editors. Computational methods and clinical applications for spine imaging: metastatic vertebrae segmentation for use in a clinical pipeline. Shenzhen, China: Springer; 2019. p. 15–28.
Clement A. Image based and biomechanical characterization of osteoblastic vertebral metastases [master’s dissertation]. Toronto: [Toronto, ON]: University of Toronto; 2019.
Samiezadeh S, Ebrahimi H, Tong F, Whyne C. A computational model of the post-yield response of vertebral bone using zero-thickness cohesive elements. Poster presented at: Orthopaedic Research Society Annual Meeting. United States: San Diego; 2017 Mar 20.
Boehling NS, Grosshans DR, Allen PK, McAleer MF, Burton AW, Azeem S, et al. Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases: clinical article. J Neurosurg Spine. 2012;16:379–86.
Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability Neoplastic score. J Clin Oncol. 2013;31:3426–31.
Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13:324–8.
Fisher CG, Dipaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the spine oncology study group. Spine (Phila Pa 1976). 2010;35:1221–9.
Joaquim AF, Fernandes YB, Cavalcante RAC, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976). 2011;36:33–6.
Fourney DR, Frangou EM, Ryken TC, DiPaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score: an analysis of reliability and validity from the Spine Oncology Study Group. J Clin Oncol. 2011;29:3072–7.
Versteeg AL, Verlaan JJ, Sahgal A, Mendel E, Quraishi NA, Fourney DR, et al. The spinal instability neoplastic score: impact on oncologic decision-making. Spine (Phila Pa 1976). 2016;41:S231–7.
Damron TA, Nazarian A, Entezari V, Brown C, Grant W, Calderon N, et al. CT-based structural rigidity analysis is more accurate than Mirels scoring for fracture prediction in metastatic femoral lesions. Clin Orthop Relat Res. 2016;474:643–51.
Snyder BD, Cordio MA, Nazarian A, Kwak SD, Chang DJ, Entezari V, et al. Noninvasive prediction of fracture risk in patients with metastatic cancer to the spine. Clin Cancer Res. 2009;15:7676–83.
Thibault I, Whyne CM, Zhou S, Campbell M, Atenafu EG, Myrehaug S, et al. Volume of lytic vertebral body metastatic disease quantified using computed tomography - based image segmentation predicts fracture risk after spine stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2017;97:75–81.
Hoff B, Toole M, Yablon C, Ross B, Luker G, VanPoznak C, et al. Potential for early fracture risk assessment in patients with metastatic bone disease using parametric response mapping of CT images. Tomography. 2015;1:98–104.
Hardisty M, Wright T, Campbell M, Burke M, Atenafu E, Cawricz M, et al. CT based quantitative measures of the stability of fractured metastatically involved vertebrae treated with spine stereotactic body radiotherapy. Clin Exp Metastasis. 2020;37(5):575–84.
Sternheim A, Giladi O, Gortzak Y, Drexler M, Salai M, Trabelsi N, et al. Pathological fracture risk assessment in patients with femoral metastases using CT-based finite element methods. A retrospective clinical study. Bone. 2018;110:215–20.
Janssen S, Paulino Pereira N, Meijs T, Bredella M, Ferrone M, van Dijk C, et al. Predicting pathological fracture in femoral metastases using a clinical CT scan based algorithm: a case-control study. J Orthop Sci. 2018;23:394–402.
Eggermont F, van der Wal G, Westhoff P, Laar A, de Jong M, Rozema T, et al. Patient-specific finite element computer models improve fracture risk assessments in cancer patients with femoral bone metastases compared to clinical guidelines. Bone. 2020;130:115101.
Roth SE, Mousavi P, Finkelstein J, Chow E, Kreder H, Whyne CM. Metastatic burst fracture risk prediction using biomechanically based equations. Clin Orthop Relat Res. 2004;419:83–90.
Galbusera F, Casaroli G, Bassani T. Artificial intelligence and machine learning in spine research. JOR SPINE. 2019;2:e1044.
Ramos JS, Nogueira-Barbosa MH, Watanabe CYV, Traina AJM. B Growth: an efficient approach for the segmentation of vertebral compression fractures in magnetic resonance imaging. Proc ACM Symp Appl Comput. 2019;(Part F1477):220–7.
Jakubicek R, Chmelik J, Jan J, Ourednicek P, Lambert L, Gavelli G. Learning–based vertebra localization and labeling in 3D CT data of possibly incomplete and pathological spines. Comput Methods Programs Biomed. 2020;183:105081.
Rose PS, Laufer I, Boland PJ, Hanover A, Bilsky MH, Yamada J, et al. Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol. 2009;27:5075–9.
Loi M, Nuyttens JJ, Desideri I, Greto D, Livi L. Single-fraction radiotherapy (SFRT) for bone metastases: patient selection and perspectives. Cancer Manag Res. 2019;11:9397–408.
Faruqi S, Tseng C-LL, Whyne C, Alghamdi M, Wilson J, Myrehaug S, et al. Vertebral compression fracture after spine stereotactic body radiation therapy: a review of the pathophysiology and risk factors. Clin Neurosurg. 2018;83:314–22.
Sprave T, Verma V, Förster R, Schlampp I, Hees K, Bruckner T, et al. Local response and pathologic fractures following stereotactic body radiotherapy versus three-dimensional conformal radiotherapy for spinal metastases - a randomized controlled trial. BMC Cancer. 2018;18:4777–8.
Wernle JD, Damron TA, Allen MJ, Mann KA. Local irradiation alters bone morphology and increases bone fragility in a mouse model. J Biomech. 2010;43:2738–46.
Soares PBF, Soares CJ, Limirio PHJO, de Jesus RNR, Dechichi P, Spin-Neto R, et al. Effect of ionizing radiation after-therapy interval on bone: histomorphometric and biomechanical characteristics. Clin Oral Investig. 2019;23:2785–93.
Ehresman J, Schilling A, Pennington Z, Gui C, Chen X, Lubelski D, et al. A novel MRI-based score assessing trabecular bone quality to predict vertebral compression fractures in patients with spinal metastasis. J Neurosurg Spine. 2020;32:499–506.
Savaridas T, Wallace RJ, Dawson S, Simpson AHRW. Effect of ibandronate on bending strength and toughness of rodent cortical bone: possible implications for fracture prevention. Bone Jt Res. 2015;4:99–104.
Tang SY, Allen MR, Phipps R, Burr DB, Vashishth D. Changes in non-enzymatic glycation and its association with altered mechanical properties following 1-year treatment with risedronate or alendronate. Osteoporos Int. 2009;20:887–94.
Acevedo C, Bale H, Gludovatz B, Wat A, Tang SY, Wang M, et al. Alendronate treatment alters bone tissues at multiple structural levels in healthy canine cortical bone. Bone. 2015;81:352–63.
Allen MR, Gineyts E, Leeming DJ, Burr DB, Delmas PD. Bisphosphonates alter trabecular bone collagen cross-linking and isomerization in beagle dog vertebra. Osteoporos Int. 2008;19:329–37.
Jin A, Cobb J, Hansen U, Bhattacharya R, Reinhard C, Vo N, et al. The effect of long-term bisphosphonate therapy on trabecular bone strength and microcrack density. Bone Jt Res. 2017;6:602–9.
Pazianas M, van der Geest S, Miller P. Bisphosphonates and bone quality. Bonekey Rep. 2014;3:529.
Pelker RR, Friedlaender GE, Panjabi MM, Markham T, Hausman M, Doganis AC, et al. Chemotherapy-induced alterations in the biomechanics of rat bone. J Orthop Res. 1985;3:91–5.
Quach JM, Askmyr M, Jovic T, Baker EK, Walsh NC, Harrison SJ, et al. Myelosuppressive therapies significantly increase pro-inflammatory cytokines and directly cause bone loss. J Bone Miner Res. 2015;30:886–97.
Hall TJ, Jeker H, Schaueblin M. Taxol inhibits osteoclastic bone resorption. Calcif Tissue Int. 1995;57:463–5.
Chung YS, Kang HC, Lee T. Comparative effects of ibandronate and paclitaxel on immunocompetent bone metastasis model. Yonsei Med J. 2015;56:1643–50.
Won E, Akens MK, Hardisty MR, Burch S, Bisland SK, Yee AJM, et al. Effects of photodynamic therapy on the structural integrity of vertebral bone. Spine (Phila Pa 1976). 2010;35:272–7.
Iolascon G, Napolano R, Gioia M, Moretti A, Riccio I, Gimigliano F. The contribution of cortical and trabecular tissues to bone strength: Insights from denosumab studies. Clin Cases Miner Bone Metab. 2013;10:47–51.
Castellano D, Sepulveda JM, García-Escobar I, Rodriguez-Antolín A, Sundlöv A, Cortes-Funes H. The role of RANK-ligand inhibition in cancer: the story of denosumab. Oncologist. 2011;16:136–45.
Dougall WC, Holen I, González SE. Targeting RANKL in metastasis. Bonekey Rep. 2014;3:519.
Dempster DW, Lambing CL, Kostenuik PJ, Grauer A. Role of RANK ligand and denosumab, a targeted RANK ligand inhibitor, in bone health and osteoporosis: a review of preclinical and clinical data. Clin Ther. 2012;34:521–36.
Lo VCK, Akens MK, Wise-Milestone L, Yee AJM, Wilson BC, Whyne CM. The benefits of photodynamic therapy on vertebral bone are maintained and enhanced by combination treatment with bisphosphonates and radiation therapy. J Orthop Res. 2013;31:1398–405.
Arrington SA, Damron TA, Mann KA, Allen MJ. Concurrent administration of zoledronic acid and irradiation leads to improved bone density, biomechanical strength, and microarchitecture in a mouse model of tumor-induced osteolysis. J Surg Oncol. 2007;97:284–90.
O’Carrigan B, Wong MHF, Willson ML, Stockler MR, Pavlakis N, Goodwin A. Bisphosphonates and other bone agents for breast cancer. Cochrane Database Syst Rev. 2017;10:CD003474.
Lockwood M, Banderudrappagari R, Suva LJ, Makhoul I. Atypical femoral fractures from bisphosphonate in cancer patients – review. J Bone Oncol. 2019;18:100259.
Ota S, Inoue R, Shiozaki T, Yamamoto Y, Hashimoto N, Takeda O, et al. Atypical femoral fracture after receiving antiresorptive drugs in breast cancer patients with bone metastasis. Breast Cancer. 2017;24:601–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
I, Cari Whyne, on behalf of all authors, declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Biomechanics
Rights and permissions
About this article
Cite this article
Whyne, C.M., Ferguson, D., Clement, A. et al. Biomechanical Properties of Metastatically Involved Osteolytic Bone. Curr Osteoporos Rep 18, 705–715 (2020). https://doi.org/10.1007/s11914-020-00633-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00633-z