Abstract
Purpose of Review
Osteogenesis imperfecta (OI) is a genetic bone disorder resulting in bone fragility. It has a heterogeneous phenotype which typically includes reduced bone mass, multiple fractures, deformity, and chronic disability. Bisphosphonate treatment remains the first-line medical management, but there is still debate on aspects of its effectiveness. This review summarizes current knowledge about long-term bisphosphonate use in OI with recommendations on clinical application.
Recent Findings
Bisphosphonates increase bone mineral density, most notably of the vertebrae, and reduce fracture risk in the pediatric OI population. Gains in strength and mobility, together with the permissive effect on orthopedic surgery (e.g., in combination with intramedullary rodding) and physiotherapy, have resulted in improved quality of life for those with OI.
Summary
As experience in its use continues, the risks and benefits of long-term bisphosphonate treatment in OI are slowly emerging. Patient registries containing data on genotype, phenotype, fractures, bisphosphonate treatment, orthopedic intervention, and functional outcomes are essential for systematic evaluation given the lack of large multi-centered randomized control trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteogenesis imperfecta (OI) is a genetic bone disorder with an estimated incidence of approximately 1:10,000 births. It is characterized by bone fragility but is associated with other clinical features including short stature, limb deformity, scoliosis, blue sclera, dentinogenesis imperfecta, hearing loss, hypermobility, wormian bones, and easy bruising [1]. OI is commonly caused by mutations in COL1A1 or COL1A2 in over 90% of cases causing defects in the helical domains of collagen type I protein or haploinsufficiency [2, 3].
OI remains a clinical diagnosis, as reflected in the original Sillence classification [4]. Advances in molecular genetic techniques have identified additional genes known to cause OI which has added to the complexity in classification. These include CRTAP, P3H1/LEPRE1, PPIB, FKBP10, SERPINH1, PLOD2, TMEM38B, BMP1, SEC24D, SPARC, P4HB, SP7/OSX, WNT1, SERPINF1, IFITM5, CREB3L1, PLS3, and LRP5 [5••]. A revised nomenclature is commonly used to categorize the OI type as established in the 2015 Nosology and Classification of Genetic Skeletal Disorders [6]. This categorizes the phenotype as non-deforming (type 1), perinatally lethal (type 2), progressively deforming (type 3), moderate severity (type 4), and OI with calcification of the interosseous membrane and/or hypertrophic callus (type 5). A hybrid classification of the causative gene together with the clinical phenotype should be used to avoid ambiguity. An example of a hybrid classification that also includes categorization by the underlying mechanism of disease and acknowledges variability in the phenotype despite the same mutation is provided by Trejo and Rauch [5••].
The holistic management of OI ideally involves a multidisciplinary team of medical, surgical, and allied health care professionals [1]. The aim of management is to improve motor function and quality of life by maximizing mobility and reducing fracture rate. Medical management primarily involves bisphosphonate therapy, and this has been the mainstay of treatment since the first case report described its effect in 1987 [7]. Despite 30 years of use, there are still a number of unanswered questions and conflicting evidence as to its efficacy [8••]. Areas of ongoing clinical investigation include (a) the dose and timing of treatment required to optimize bone health while minimizing side effects, (b) the role of oral vs. intravenous bisphosphonates, and (c) long-term bisphosphonate management in children and adults including outcomes following cessation of therapy and the concept of maintenance bisphosphonate therapy. This review aims to explore these areas further.
Bisphosphonates
Bisphosphonates are analogues of pyrophosphate that avidly bind to the surface of the bone. Their underlying structure comprises a carbon-phosphate-carbon backbone which makes them impervious to chemical hydrolysis [9]. They exert their effect by several mechanisms including direct inhibition of osteoclast precursor differentiation, osteoclast apoptosis, and inhibition of the mevalonate pathway [10]. Commonly used medications include the second-generation bisphosphonates, alendronate and pamidronate, which have amino-terminal groups. Third-generation bisphosphonates, namely risedronate and zoledronate, have a cyclic side chain resulting in improved anti-resorptive properties.
A systematic review from 2009 confirmed improvement in bone density in children with OI who were treated with bisphosphonates [11]. Not all studies included in that review showed reduction in fracture rates, improvement with pain, or increased quality of life with treatment. A more recent Cochrane review included 14 out of 21 trials (819 participants) to assess the effectiveness and safety of bisphosphonates in increasing bone mineral density, reducing fractures, and improving clinical function in children and adults with OI [8••]. Included studies were published between 2003 and 2013 [12,13,14, 15•, 16,17,18,19,20,21,22,23,24], and many of the questions raised in the initial systematic review were echoed in the follow-up review. Data describing growth, bone pain, fracture rate, or functional outcomes were incomplete, and studies were not sufficiently powered to assess these variables reliably. The benefits and adverse effects of bisphosphonates in OI will now be explored in further detail.
Benefits of Bisphosphonates
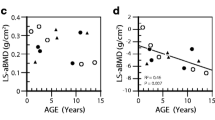
Bisphosphonates are an imperfect treatment for OI as they do not address the underlying issue of bone quality. There is no doubt, however, that bisphosphonate therapy increases bone mineral density in OI, particularly in growing children, as illustrated in the recent Cochrane review [8••]. Intravenous bisphosphonate treatment in the presence of ongoing growth enables improvement of vertebral compression fractures [25•] by bone modeling. This effect is time dependent so the longer the period of treatment/growth, the better the outcome in terms of normal or near-normal vertebral body dimensions [26]. Bisphosphonate use does not appear to alter the incidence of scoliosis but may slow its progression in severe forms of OI [27]. Improvements in mobility and functional outcome have also been described [25•]. A recent meta-analysis showed a 20% decrease in long-bone fractures in pediatric patients with OI treated with bisphosphonates [28] while another showed a trend to reduction that was not statistically significant [29]. As the underlying abnormal properties of OI bone are not altered with bisphosphonate therapy, ongoing fractures remain a challenge to manage [26]. Oral bisphosphonate treatment has not been associated with improvements in vertebral body morphology [15•] but has shown similar reduction in pediatric fractures compared to intravenous therapy [28], so its use may be limited to mild OI or maintenance of moderate OI in the absence of compression fractures.
The optimal dose, frequency, and duration of treatment for bisphosphonates in OI remain to be elucidated. The majority of data are on the use of intravenous pamidronate in OI with increasing data on zoledronate. The approach to treatment varies from center-to-center, dependent on the availability of medication and the experience of the treating physician. Our approach is to use intravenous pamidronate in children less than 2 years of age, switching to zoledronate in older children with moderate to severe OI. Other centers however use solely pamidronate or zoledronate. To date, there are no data to indicate that one form of intravenous bisphosphonate is superior to another. Not all children with OI require intravenous bisphosphonate therapy. At our center, we follow a highly conservative approach and consider using intravenous bisphosphonates in children with OI type III or children who have had two or more long-bone fractures per year or the presence of vertebral compression fractures. Other centers initiate bisphosphonate therapy in children with confirmed diagnoses of OI following a single major long-bone fracture (such as a femur fracture). The annual dose of pamidronate varies between 9 to 12 mg/kg/year, depending on the regimen used [30, 31]. Zoledronate is almost uniformly commenced at 0.05 mg/kg/dose six monthly. In bisphosphonate-naïve patients at our center, the first dose of zoledronate is reduced to 0.0125 mg/kg to decrease the likelihood of hypocalcemia and acute phase response [5••, 30]. The greatest increase in BMD, cortical thickness, and trabecular number occurs within the first 2–4 years of bisphosphonate therapy [26]. The vast majority of children with OI will therefore receive at least 2 years of intravenous bisphosphonate as above. Ongoing treatment is then titrated to clinical effect in terms of ongoing fracture history, bone pain, and serial bone mineral densitometry: if lumbar spine areal bone density z score falls within the range − 2 to 0, zoledronate is decreased from 0.05 to 0.025 mg/kg six monthly or pamidronate 1 mg/kg/dose 3–4 monthly. As the lumbar spine areal density z score improves further, then maintenance therapy continues at 0.025 mg/kg 12 monthly until growth is complete. Similar treatment strategies have been reported elsewhere [5••], but there is a paucity of data indicating that continuing treatment until growth ceases will limit fractures around the metaphyseal/growth plate site [31]. This site is at potentially higher risk of fracture as it is at the interface between treated and treatment-naïve bone (Fig. 1). Bisphosphonates have also been shown to be less effective for the treatment of adult OI patients compared to children [28, 32], therefore emphasizing the importance of optimal treatment during growth.
Wrist x-ray following multiple cycles of intravenous bisphosphonate therapy. a Immediately prior to fracture, “<” indicating sclerotic metaphyseal bands from treatment. b The same wrist immediately after a distal radial fracture, “>” indicating the position of fracture at the boundary of one of the sclerotic bands
Adverse Effects of Bisphosphonates
Multiple reports on the adverse effects of bisphosphonates have been published [1, 5••, 33]. Typical effects following initial treatment include an acute phase response (fever, headache, vomiting, arthralgia, myalgia) and hypocalcemia which are less likely on subsequent doses. These side effects are less marked with oral bisphosphonates and can be minimized for intravenous bisphosphonates by reducing the initial dose [30]. Oral bisphosphonates have been associated with increased gastrointestinal discomfort compared to intravenous preparations, even when patients are instructed to drink large volumes of water and refrain from lying down following administration [34]. Fortunately, early reports of oral agents potentially causing esophageal adenocarcinoma remain unproven [35].
There are many other reported side effects that are rare but need to be considered when managing patients on bisphosphonates. These include ocular inflammation (iritis, episcleritis, conjunctivitis), rash, urticaria, mucositis, hepatitis, atrial fibrillation, and psychosis [34]. Atrial fibrillation (AF) was not associated with oral alendronate in a meta-analysis of placebo-controlled clinical trials [36], but a larger meta-analysis of oral and intravenous bisphosphonates showed a significantly increased risk of AF-requiring hospitalization [37]. Zoledronate has also been associated with acute tubular necrosis in adults following a single dose [38]. Care should be given when administering to those with impaired renal function and appropriate dose reduction should always be considered in the context of renal impairment [39]. Although case reports and observational cohort studies can identify possible uncommon adverse effects, it should be remembered that this does not confirm a true causal relationship. Ultimately, bisphosphonates should be prescribed through specialized clinics by clinicians with experience in their administration.
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) has received a lot of attention over recent years and warrants further discussion. BRONJ is defined as exposed mandibular/maxillary bone that does not heal within 8 weeks of appropriate treatment in a patient with a history of bisphosphonate exposure (in the absence of craniofacial radiation therapy) [40•]. The pathogenic mechanisms of BRONJ are still being elucidated, but risk factors include duration of bisphosphonate treatment, intravenous administration, dental procedures (extraction/surgery), dental trauma/prosthesis, and an underlying diagnosis of cancer [41]. BRONJ has not been described in the pediatric population to date [42], but most centers practice a conservative approach from a dental perspective. This includes a pre-treatment dental assessment, regular dental surveillance, and postponement of bisphosphonate treatment until dental surgical sites (e.g., post-extraction sites) have healed [40•].
Bisphosphonates have been shown to cause delayed tooth development and eruption in animal models [43]. The timing of dental development in OI patients was recently investigated and treatment-naïve patients had advanced dental development compared to controls [44]. They also had faster resorption of their deciduous teeth. OI patients treated with bisphosphonates had a relative delay in dental development compared to treatment-naïve patients that made them indistinguishable from controls [44]. Delayed healing of osteotomy sites, but not fracture sites, also occurs in the context of bisphosphonate treatment in children with OI [45]. It is therefore prudent to delay routine bisphosphonate treatment until sufficient post-surgical healing has taken place. The exact time for healing can vary from patient to patient but is nominally 4 months [46]. This can be monitored clinically with serial x-rays to show sufficient callus formation and disappearance of the osteotomy line. Delayed healing is more likely to be associated with intraoperative use of a power saw rather than an osteotome [46].
Atypical femoral subtrochanteric/diaphyseal fractures are uncommon but have been described in adult patients treated with long-term bisphosphonates for osteoporosis as well as adults who have not received bisphosphonate therapy [34, 47]. Case reports have also cited atypical fractures in children with OI [48]. One such possible example is exemplified in Fig. 2; however, considerable controversy remains as to whether atypical femur fractures in children with OI are due to the underlying disease or to bisphosphonate therapy. A recent retrospective study looking at 116 femur fractures in 119 children with OI showed atypical fractures were more closely associated with the severity of OI rather than to bisphosphonate treatment history [49•]. It is important to note that atypical femoral fractures have been defined according to the following specific criteria: minimal trauma, a transverse fracture line, originating at the lateral cortex, non-comminuted, and with localized periosteal/endosteal thickening at the fracture site [47]. Additional features that suggest atypical femur fracture, but are not required for formal diagnosis, include prodromal pain, generalized increase in cortical thickness of femoral diaphysis, bilateral femoral diaphysis fractures, and delayed fracture healing. Many of these features are present in treatment-naïve OI patients, so the question remains as to what constitutes an atypical fracture in OI?
X-ray showing a femoral fracture in a 17-year-old boy with OI receiving 6 monthly zoledronate for 8 years. Note the lateral origin of the fracture and the cortical thickening at the fracture line “<”, raising the question whether this is an atypical femur fracture due to bisphosphonate use. A recent publication in children with OI suggests such fractures may be more closely related to the severity of the OI than the bisphosphonate history [5••]
Cyclical intravenous bisphosphate therapy creates sclerotic metaphyseal bands parallel to the growth plate and can readily be visualized on x-ray (Fig. 1). Formation of stress risers from orthopedic hardware or bisphosphonate treatment can also contribute to fracture risk [50] (Fig. 3). These areas create stress risers due to the close approximation of the bone with differing densities [50]. The clinician must remain mindful about the long-term effects of bone suppression from continued bisphosphonate use and should consider titrating medication dose/frequency to achieve the best outcomes in both the short and long term. Given the lack of data on optimal treatment regimen, and the heterogeneity of OI, patients will continue to be treated case by case. Once bisphosphonate treatment is ceased entirely, there is negligible effect on any new bone that is produced following further growth and remodeling [51]. It is therefore advised to have children with OI on a long-term maintenance dose of bisphosphonate although the best medication, dose, and frequency remain uncertain.
Right femur x-ray showing a Fassier-Duval rod in a 1-year-old girl with OI treated with intravenous pamidronate. Note the healing fracture involving the mid-diaphysis. b She outgrew the rod by 8 years of age and sustained a stress fracture (c) at the proximal end of the original rod necessitating a femoral osteotomy and new Fassier-Duval rod with femoral neck fixation. d Sufficient healing was evident 4 months later and bisphosphonate therapy was recommenced. e The fracture site was still evident at 9 years of age, 1 year post fracture. f Complete radiological resolution occurred by 2 years post fracture
Bisphosphonates persist in the bone matrix for years after therapy is discontinued, so there have been concerns raised regarding fetal bisphosphonate exposure. A recent review of 65 pregnancies showed decreased gestational age, decreased birth weight, hypocalcemia, and hyperphosphatemia were associated with bisphosphonate use before or during pregnancy [52]. Importantly, no study to date has identified any increased incidence in birth defects or long-term adverse effects [52]. Bisphosphonates are contraindicated during pregnancy, and we routinely ensure a negative pregnancy test in all females of reproductive age before each bisphosphonate dose. Females should be counseled about the issues surrounding this aspect of bisphosphonate treatment, and the above risks need to be weighed against the benefits of ongoing bisphosphonate treatment in OI women of childbearing age.
Summary
Bisphosphonates have been used in OI for the last 30 years and have been shown to effectively increase bone mineral density, particularly the spine, with a small but significant improvement in reducing fracture risk, particularly in the pediatric OI population [26, 28]. The positive impact on strength and mobility and the permissive effect on orthopedic surgery (e.g., intramedullary rods) and physiotherapy have resulted in improved quality of life for those with OI [53]. The potential side effects of bisphosphonates are well described, and treatment outcomes need to be monitored by experienced physicians. The clinical heterogeneity of OI, lack of consensus of treatment strategies, and small population size contribute to the difficulty in assessing the effectiveness of bisphosphonate treatment; nevertheless, the evidence is clear that intravenous (but not oral) bisphosphonates prevent vertebral fractures and foster reshaping of previously fractured vertebrae in OI—this is one of the most compelling reasons to support their use in this setting. National and international patient registries containing data on genotype, phenotype, treatment, fractures, and functional outcomes are essential for systematic evaluation given the lack of large multi-centered randomized control trials. Bisphosphonate therapy remains only one aspect of OI management, and improvements in function require a combination of medical, surgical, physical, and rehabilitation therapy [1].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Biggin A, Munns CF. Osteogenesis imperfecta: diagnosis and treatment. Curr Osteoporos Rep. 2014;12(3):279–88.
Byers PH. Etiology of osteogenesis imperfecta: an overview of biochemical and molecular genetic analyses. Connect Tissue Res. 1995;31(4):257–9.
Forlino A, Marini JC. Osteogenesis imperfecta. Lancet. 2016;387(10028):1657–71.
Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979;16(2):101–16.
•• Trejo P, Rauch F. Osteogenesis imperfecta in children and adolescents-new developments in diagnosis and treatment. Osteoporos Int. 2016;27(12):3427–37. A recent review of the diagnosis and management of OI in children including new approaches to treatment.
Bonafe L, et al. Nosology and classification of genetic skeletal disorders: 2015 revision. Am J Med Genet A. 2015;167A(12):2869–92.
Devogelaer JP, et al. Radiological manifestations of bisphosphonate treatment with APD in a child suffering from osteogenesis imperfecta. Skelet Radiol. 1987;16(5):360–3.
•• Dwan K, et al. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev. 2016;10:CD005088. A Cochrane review of 14 trials (819 participants) to assess the effectiveness and safety of bisphosphonates in increasing bone mineral density, reducing fractures and improving clinical function in children and adults with OI.
Watts NB. Treatment of osteoporosis with bisphosphonates. Endocrinol Metab Clin N Am. 1998;27(2):419–39.
Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc Mayo Clin. 2008;83(9):1032–45.
Castillo H, Samson-Fang L. Effects of bisphosphonates in children with osteogenesis imperfecta: an AACPDM systematic review. Dev Med Child Neurol. 2009;51(1):17–29.
Adami S, et al. Intravenous neridronate in adults with osteogenesis imperfecta. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2003;18(1):126–30.
Barros ER, et al. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab: JPEM. 2012;25(5–6):485–91.
Bishop N, et al. A randomized, controlled dose-ranging study of risedronate in children with moderate and severe osteogenesis imperfecta. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2010;25(1):32–40.
• Bishop N, et al. Risedronate in children with osteogenesis imperfecta: a randomised, double-blind, placebo-controlled trial. The Lancet. 2013; Reported that oral risedronate increased areal BMD and reduced risk of first and recurrent clinical fractures in children with OI.
Chevrel G, et al. Effects of oral alendronate on BMD in adult patients with osteogenesis imperfecta: a 3-year randomized placebo-controlled trial. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2006;21(2):300–6.
DiMeglio LA, Peacock M. Two-year clinical trial of oral alendronate versus intravenous pamidronate in children with osteogenesis imperfecta. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2006;21(1):132–40.
Gatti D, et al. Intravenous neridronate in children with osteogenesis imperfecta: a randomized controlled study. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2005;20(5):758–63.
Letocha AD, et al. Controlled trial of pamidronate in children with types III and IV osteogenesis imperfecta confirms vertebral gains but not short-term functional improvement. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2005;20(6):977–86.
Rauch F, et al. Risedronate in the treatment of mild pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Bone Mineral Res: Off J Am Soc Bone Mineral Res. 2009;24(7):1282–9.
Sakkers R, et al. Skeletal effects and functional outcome with olpadronate in children with osteogenesis imperfecta: a 2-year randomised placebo-controlled study. Lancet. 2004;363(9419):1427–31.
Seikaly MG, et al. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop. 2005;25(6):786–91.
Senthilnathan S, Walker E, Bishop NJ. Two doses of pamidronate in infants with osteogenesis imperfecta. Arch Dis Child. 2008;93(5):398–400.
Ward LM, et al. Alendronate for the treatment of pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Clin Endocrinol Metab. 2011;96(2):355–64.
• Alcausin MB, et al. Intravenous pamidronate treatment in children with moderate-to-severe osteogenesis imperfecta started under three years of age. Horm Res Paediatr. 2013;79(6):333–40. Reported that pamidronate started under three years of age improved bone density, reduced fracture frequency and resulted in attainment of motor milestones at an earlier age.
Palomo T, et al. Intravenous bisphosphonate therapy of young children with osteogenesis imperfecta: skeletal findings during follow up throughout the growing years. J Bone Miner Res. 2015;30(12):2150–7.
Sato A, et al. Scoliosis in osteogenesis imperfecta caused by COL1A1/COL1A2 mutations—genotype-phenotype correlations and effect of bisphosphonate treatment. Bone. 2016;86:53–7.
Shi CG, Zhang Y, Yuan W. Efficacy of bisphosphonates on bone mineral density and fracture rate in patients with osteogenesis imperfecta: a systematic review and meta-analysis. Am J Ther. 2016;23(3):e894–904.
Hald JD, et al. Bisphosphonates for the prevention of fractures in osteogenesis imperfecta: meta-analysis of placebo-controlled trials. J Bone Miner Res. 2015;30(5):929–33.
Munns CF, et al. Acute phase response and mineral status following low dose intravenous zoledronic acid in children. Bone. 2007;41(3):366–70.
Brizola E, Shapiro JR. Bisphosphonate treatment of children and adults with osteogenesis imperfecta: unanswered questions. Calcif Tissue Int. 2015;97(2):101–3.
Marom R, et al. Pharmacological and biological therapeutic strategies for osteogenesis imperfecta. Am J Med Genet C Semin Med Genet. 2016;172(4):367–83.
Tanvetyanon T, Stiff PJ. Management of the adverse effects associated with intravenous bisphosphonates. Ann Oncol: Off J Eur Soc Med Oncol/ESMO. 2006;17(6):897–907.
Italian Society of Osteoporosis, M.M, et al. Safety profile of drugs used in the treatment of osteoporosis: a systematical review of the literature. Reumatismo. 2013;65(4):143–66.
Sun K, et al. Bisphosphonate treatment and risk of esophageal cancer: a meta-analysis of observational studies. Osteoporos Int. 2013;24(1):279–86.
Barrett-Connor E, et al. Alendronate and atrial fibrillation: a meta-analysis of randomized placebo-controlled clinical trials. Osteoporosis Int. 2012;23:233–45.
Sharma A, et al. Risk of serious atrial fibrillation and stroke with use of bisphosphonates. Chest. 2013;144(4):1311–22.
Yachoui R. Early onset acute tubular necrosis following single infusion of zoledronate. Clin Cases Miner Bone Metab. 2016;13(2):154–6.
Ott SM. Pharmacology of bisphosphonates in patients with chronic kidney disease. Semin Dial. 2015;28(4):363–9.
• Bhatt RN, Hibbert SA, Munns CF. The use of bisphosphonates in children: review of the literature and guidelines for dental management. Aust Dent J. 2014;59(1):9–19. Reports the pediatric uses and adverse effects of bisphosphonates and provides recommendations on the dental management of children receiving bisphosphonates.
Bejhed, R.S., M. Kharazmi, and Hallberg, Identification of risk factors for bisphosphonate-associated atypical femoral fractures and osteonecrosis of the jaw in a pharmacovigilance database. Ann Pharmacother, 2016. 50(8): 616–624.
Hennedige AA, et al. Systematic review on the incidence of bisphosphonate related osteonecrosis of the jaw in children diagnosed with osteogenesis imperfecta. J Oral Maxillofac Res. 2013;4(4):e1.
Bradaschia-Correa V, Massa LF, Arana-Chavez VE. Effects of alendronate on tooth eruption and molar root formation in young growing rats. Cell Tissue Res. 2007;330(3):475–85.
Vuorimies I, et al. Timing of dental development in osteogenesis imperfecta patients with and without bisphosphonate treatment. Bone. 2017;94:29–33.
Munns CF, et al. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Mineral Res: Off J Am Soc Bone Min Res. 2004;19(11):1779–86.
Anam EA, et al. Osteotomy healing in children with osteogenesis imperfecta receiving bisphosphonate treatment. J Bone Miner Res. 2015;30(8):1362–8.
Shane E, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1–23.
Vasanwala RF, et al. Recurrent proximal femur fractures in a teenager with osteogenesis imperfecta on continuous bisphosphonate therapy: are we overtreating? J Bone Miner Res. 2016;31(7):1449–54.
• Trejo P, et al. Diaphyseal femur fractures in osteogenesis imperfecta: characteristics and relationship with bisphosphonate treatment. J Bone Miner Res. 2016; A recent retrospective study looking at 116 femur fractures in 119 children with OI showed atypical fractures were more closely associated with the severity of OI rather than to bisphosphonate treatment history.
Biggin A, et al. Fracture during intravenous bisphosphonate treatment in a child with osteogenesis imperfecta: an argument for a more frequent, low-dose treatment regimen. Horm Res Paediatr. 2014;81(3):204–10.
Rauch F, et al. Long-bone changes after pamidronate discontinuation in children and adolescents with osteogenesis imperfecta. Bone. 2007;40(4):821–7.
Green SB, Pappas AL. Effects of maternal bisphosphonate use on fetal and neonatal outcomes. Am J Health Syst Pharm. 2014;71(23):2029–36.
Ashby E, et al. Functional outcome of humeral rodding in children with osteogenesis imperfecta. J Pediatr Orthop. 2016; https://doi.org/10.1097/BPO.0000000000000729.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Andrew Biggin and Craig Munns report participating in drug trials sponsored by Novartis. Dr. Munns has received funding for trials from Novartis.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatrics
Rights and permissions
About this article
Cite this article
Biggin, A., Munns, C.F. Long-Term Bisphosphonate Therapy in Osteogenesis Imperfecta. Curr Osteoporos Rep 15, 412–418 (2017). https://doi.org/10.1007/s11914-017-0401-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-017-0401-0