Abstract
More than 50 % of untreated patients with celiac disease (CD) have bone loss detected by bone densitometry (dual-energy X-ray absorptiometry:DXA). Moreover, patients with CD are more likely to have osteoporosis and fragility fractures, especially of the distal radius. Although still controversial, we recommend DXA screening in all celiac disease patients, particularly in those with symptomatic CD at diagnosis and in those who present risk factors for fracture such as older age, menopausal status, previous fracture history, and familial hip fracture history. Bone microarchitecture, especially the trabecular network, may be deteriorated, explaining the higher fracture risk in these patients. Adequate calcium and vitamin D supplementation are also recommended to optimize bone recovery, especially during the first years of gluten free diet (GFD). If higher fracture risk persists after 1 or 2 years of GFD, specific osteoactive treatment may be necessary to improve bone health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: Celiac Disease
Celiac disease (CD) is a common autoimmune systemic disorder that affects up to 1 % of the population worldwide [1]. This enteropathy is triggered by dietary gluten (wheat, rye, and barley) and it is characterized by the presence of auto-antibodies resulting in a variety of intestinal and extra-intestinal manifestations [2]. While some symptoms are overt and easy to recognize, others may be subtle and silent resulting in a broad clinical presentation of CD. Some individuals may present with typical gastrointestinal symptoms, such as diarrhea, abdominal pain, distention, weight loss, and failure to thrive in children, whereas others may present with no gastrointestinal complaints, but exhibit iron deficiency anemia, low bone mineral density, elevated liver enzymes, unexpected weight loss, prolonged fatigue, or infertility [3•]. Moreover, some patients may be completely asymptomatic and detected only by serologic screening for associated conditions, such as dermatitis herpetiformis, autoimmune thyroid disease and type 1 diabetes, or first-degree relatives of patients with diagnosed CD [4]. The proportion of newly diagnosed patients with malabsorptive typical gastrointestinal symptoms has decreased over time and CD with ‘non-classical’ and even asymptomatic presentation is gaining prominence [5]. The current awareness of CD complications in combination with the advent of highly sensitive and specific serological tests has dramatically increased the identification of patients with this phenotype [5].
Diagnosis of CD is based on well-established criteria (positive CD serology tests and abnormal duodenal histology) [2]. If serology and histology are discordant, human leukocyte antigen (HLA) typing might be useful because HLA-DQ2 and HLA-DQ8 are present in almost all individuals with CD but only in 30 to 40 % of the general population, giving this test a high negative predictive value [2].
Currently, the only established treatment for the disease is a strict, lifelong gluten-free diet (GFD). Considerable interest exists in the development of non-dietary therapies. There are clinical trials that include new treatment approaches focused on modification of food products, enzymatic degradation or binding of gluten, inhibition of small intestinal permeability, inhibition of tissue transglutaminase, and modulation of the immune system [6].
Multifactorial Pathogenesis of Bone Damage
Bone compromise in CD has been extensively studied in the last 20 years. Metabolic bone diseases like low bone mass, osteoporosis, secondary hyperparathyroidism, and osteomalacia might be present in celiac patients, even in those without gastrointestinal complaints.
Both local and systemic mechanisms may play a role [7]. Calcium absorption is impaired due to mucosal atrophy; therefore, to avoid hypocalcemia, parathyroid hormone increases substantially (secondary hyperparathyroidism) and stimulates osteoclasts mediated bone degradation. Calcium is then obtained from the skeleton reservoir, but this high remodeling state can lead to osteopenia and osteoporosis, altering bone microstructure and increasing fracture risk. Concomitant hypogonadism can also affect bone metabolism [8]. Last, but not least, hypersecretion of proinflammatory cytokines like interleukin-1, interleukin-6, and tumor necrosis factor-alpha increased RANKL/OPG ratio, contribute to the increase in osteoclastic bone resorption [9]. This immunological pathogenesis may also include the potential role of autoimmune phenomena since tissue transglutaminase seems to be an extremely relevant enzyme also in bone mineralization [10].
Low Bone Mineral Density in Celiac Disease
The prevalence of low bone mineral density (BMD)—osteopenia and osteoporosis—measured by DXA among patients with CD is variable, reported to be from 38 to 72 % at diagnosis and 9 to 47 % in patients treated with a gluten-free diet [11]. Low BMD is more common in adults and is present even in patients asymptomatic at the time of diagnosis [11]. Severity of bone affectation depends on gender, age, pre or postmenopausal state, severity and duration of the disease and other concomitant diseases.
Several studies have shown that treatment of CD induces an improvement in bone mineralization after starting GFD [12, 13]. Duerksen et al. evaluated changes in BMD, at baseline and follow-up in celiac seropositive cases and compared them with seronegative controls [14]. They included all patients aged 40 years or older, who had had at least two BMD measurements and initial serologic testing for CD, selected from the Manitoba database in Canada. The 43 seropositive cases had lower baseline spine and hip BMD compared with 233 seronegative controls of similar age and sex. There was a mean overall 10.8 % increase in spine BMD and 7.1 % increase in hip BMD compared with increases of 2.4 and 0.5 % in the seronegative controls. The mean interval between BMD testing was 2.4 ± 1.3 years in the seropositive group compared with 3.5 ± 1.5 years in the seronegative group (P = 0.003).
On the other hand, among the population of osteoporotic patients, serologic tests have shown a 3.4 % incidence of celiac disease compared with 1 % among the general population [15••]. So, CD must be taken into account in the diagnosis approach of secondary causes of osteoporosis. While the prevalence of CD among patients with low BMD is probably higher than that in the general population, routine screening for CD in all patients with low bone mass is not recommended. It should be targeted to higher risk cases such as severe osteoporosis or osteoporosis refractory to treatment and to those patients with vitamin D deficiency or hypocalciuria despite adequate supplementation.
Bone Microarchitecture in Celiac Disease
High-resolution peripheral quantitative computed tomography (HR-pQCT), which is a new non-invasive image method, permits three-dimensional exploration of bone microarchitectural characteristics measuring separately cortical and trabecular compartments, and giving a more profound insight into bone disease pathophysiology [16].
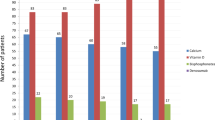
Using this new technique, we have been able to identify a significant deterioration of bone microarchitecture in peripheral bones in 31 premenopausal women with recently diagnosed CD [17••]. Patients were compared with a cohort of 22 healthy women of similar age and BMI, detecting a significant deterioration in most parameters evaluated. Patients—as expected—had low vitamin D levels, secondary hyperparathyroidism and high bone remodeling parameters. Trabecular bone, the area closest to the bone marrow, intimately related to blood vessels and the most metabolically active bone compartment, was the most affected, trabecular density being 26 % lower in celiac women than in the control group. The increased bone resorption biochemically evidenced in these patients produces thinned trabeculae with a subsequent decrease in their number, both phenomena leading to a more heterogeneous trabecular network (see Fig. 1). Notably, these features were greater in patients with symptomatic CD than in those with a subclinical phenotype.
These seminal features were also confirmed by Stein et al. who found abnormal bone microarchitecture in a group of 33 young women with CD [18]. Accordingly, they also found that CD patients had lower trabecular density and number leading to a more heterogeneous trabecular network. In addition, they also estimated lower bone strength in these patients via finite element analyses at both the distal tibia and radius.
Bone Fractures in Celiac Disease
Osteoporotic fractures are fractures occurring from a fall from standing height or less—low-energy fractures—and are associated with decreased bone resistance and increased fragility. They have a negative impact on the quality of life and independence of the patient and, in some cases like vertebral or hip fracture, they can even lead to higher mortality [19].
The first controlled study addressing the fracture risk in CD patients was published in 2000 by our group in Argentina showing that 25 % (45 of 165) of CD patients had 1–5 fractures compared with 8 % of age- and sex-matched controls [20]. The most common site of fractures was the wrist and the majority of them had occurred prior to diagnosis of CD. After this communication, the association between celiac disease and bone fractures has been examined in a number of epidemiological studies. It is difficult to analyze epidemiological data due to the great heterogeneity of the different study populations, study designs, and small sample sizes. Furthermore, most studies collect fracture data from personal interviews, self-administered questionnaires, records, discharge registers, general practice databases, etc. but no spine radiographs are done to diagnose vertebral fractures which are asymptomatic and therefore may be sub diagnosed in more than 50 % of the cases.
Meta-analyses suggest that CD is associated with increased risk of bone osteoporotic fractures [21, 22]. The first one was published in 2008 by Olmos et al. and evaluated a total of 20,955 CD patients with 1819 (8.7 %) fractures compared with 96,777 controls with 5955 (6.15 %) fractures (OR = 1.43; 95 % CI 1.15–1.78), thus describing a risk of fracture 43 % greater in CD patients [21]. As a limitation, the authors described the significant heterogeneity among the studies with six papers showing an increased prevalence of fractures while two others did not evidence significant differences with the control population (heterogeneity χ2 value of 47.06 (P < 0.00001).
More recently, Heikkilä et al. in a meta-analysis of case-control studies found that any bone fracture was almost twice as common in individuals with a clinically diagnosed celiac disease as in those without the disease (1.92 (1.29–2.84)) [22]. However, there was heterogeneity among the estimates and the study-specific associations varied from fractures being slightly more common in CD patients to fractures being over nine times as common in CD patients as in controls. In the meta-analyses of prospective studies, celiac disease at baseline was associated with a 30 % increase (1.30 [CI] 1.14, 1.50) in the risk of any fracture.
Moreno at al. analyzed the incidence and risk of peripheral fractures before and after diagnosis between a cohort of 265 patients who had been diagnosed with CD at least 5 years before study entry and a cohort of 530 age- and sex-matched controls who had been diagnosed with functional gastrointestinal disorders; they found that compared with the control group, the CD cohort showed significantly higher incidence rate and risk of first peripheral fracture before diagnosis in women [adjusted hazard ratio (HR) 1.78, 95 % CI 1.23–2.56, P < 0.002] and in men (HR 2.67, 95 % CI 1.37–5.22, P < 0.004) [23]. Fracture risk was significantly associated with the classic CD presentation with gastrointestinal symptoms (P < 0.003). In the time period after diagnosis, the risk of fractures was comparable between the CD cohort and controls in both sexes (HR 1.08, 95 % CI 0.55–2.10 for women; HR 1.57, 95 % CI 0.57–4.26 for men). In conclusion, fracture risk in CD seems to be related to the symptomatic clinical presentation and gender, being higher in symptomatic cases and in male patients [24].
However, further research would be needed to determine whether this association is specific to particular parts of the skeleton, and if asymptomatic celiac disease is also related to bone fractures.
How Can We Assess Bone Health in Celiac Disease Patients?
Clinical Risk Factors
At the medical interview, known risk factors for osteoporosis (smoking, excessive alcohol consumption, parent hip fracture history, and abnormal menstrual cycles) must be registered. History of fragility fractures, including the severity of trauma that produced the fracture and the site of the fracture, calcium intake, physical activity and sun exposure, concomitant known disorders affecting bone metabolism (thyroid disease, rheumatoid arthritis, primary hyperparathyroidism, renal insufficiency, etc.), consumption of medications potentially affecting bones as (such as corticosteroids) and clinical features related to CD should also be recorded along with the severity of symptoms at diagnosis, disease duration and later on, adherence to the gluten-free diet.
Areal Bone Density (DXA) and Biochemical Tests
There is no general agreement on the correct timing for bone densitometry scans in celiac patients. In 2003, the American Gastroenterological Association guidelines on osteoporosis in gastrointestinal disease suggested to perform bone densitometry scans in adults at the time of diagnosis of CD and after 1 year of GFD [25]. A Canadian Position Statement on evaluation and management of skeletal health in CD more recently suggested BMD measurement at diagnosis only in adults with classic CD or in those with risk factors such as menopause, older age, history of fragility fracture, vitamin D deficiency/insufficiency, and high titers of CD serological markers [26]. For asymptomatic or silent adults with CD, they recommended BMD evaluation after 1 year of GFD to allow stabilization of bone mineral density. The recommendations for follow-up were revaluation of BMD after 1 year of GFD in the presence of osteopenia/osteoporosis at diagnosis, and after 2 years in cases of normal bone mass.
In our personal opinion, every patient with celiac disease must have, if possible, a lumbar spine and femoral neck DXA scan at the time of diagnosis. Depending on that initial finding, a DXA must be repeated yearly during the first years if t-scores values are below −2 in any region. Biochemical evaluation of patients with bone compromise should include calcium, phosphorus, vitamin D, PTH, 24 h-calciuria, and bone turnover markers.
Treatment and Recommendations
After starting GFD, systemic inflammation decreases, the intestinal mucosa heals progressively, and gastrointestinal absorption is re-established. Consequently, bone resorption decreases and calcium and vitamin D go to the hungry skeleton and remineralize it. This process can be evidenced by the increase in DXA bone mineral density and ultimately, by the decrease in fracture risk [24]. Patients showed a significant decrease in bone resorption parameters and PTH values, and a significant increase in calcium and vitamin D serum concentrations after GFD, along with a considerable increase in mineralization in all regions evaluated by DXA. Although with some controversy, more recent studies have suggested a long-term normalization of the rate of fractures in patients with strict adherence to the treatment [19, 20]. Although normalization of bone mass is unlikely in adult CD, significant remineralization of axial and peripheral skeleton has been demonstrated in several studies. However, reducing the risk of fracture does not solely depend on increasing bone mass and mineral density. Other risk factors, such as structural alteration of bones with impairment of the mechanical quality (stiffness of cortical bones), deterioration of body mass, fat and muscle compartments, and neuromuscular dysfunction, also contribute to bone weakness and falls in CD patients [13]. In this context, improving muscle mass and function, nutritional status, and bone architecture through long-term GFD treatment may reduce the overall risk of fractures in CD patients [24].
It is crucial to allow enough supplementation of calcium and vitamin D to accompany this bone restoration process [7]. Calcium daily intake should range from 1000 to 1500 mg per day, in two or more divided intakes of dairy products. If the patient is not able or willing to fulfill the required intake through the diet, calcium supplements can be given. Vitamin D role is essential for the optimum absorption of calcium through the intestine [25]. The endocrine society clinical practice guideline recommends serum levels of around 30 ng/ml [27]. This can be obtained from regular sun exposure or by supplementation with the different available presentations. Muscle mass is strongly associated with bone health, fracture, and falls. Regular physical activity should be firmly recommended to help achieve the maximum recovery of bone health [28].
As with all secondary causes of osteoporosis, the first line of treatment is the specific secondary cause. However, if after 1 or 2 years of GFD with correct supplementation of calcium and vitamin D, the patient continues with osteoporosis and high risk of fracture, adding a specific osteoactive treatment must be considered. Each patient should be thoroughly evaluated to decide which treatment is the most appropriate: oral or intravenous bisphosphonates, teriparatide or denosumab.
Conclusion
Diagnosing celiac disease can be very rewarding in clinical practice because of the change in quality of life a patient may experience after adopting the correct treatment. Due to the high prevalence of low bone mass and the higher risk of fracture associated with this disease, bone health is a very important aspect of the CD patient approach. To allow for optimum recovery of bone through GFD, we recommend first a profound initial assessment of the degree of bone compromise with DXA scans and lab tests. After the initial evaluation, supplementation with calcium and vitamin D is crucial to achieve the maximum benefits of GFD. If the patient continues with high risk of fracture, osteoactive treatment should be considered. Future studies will answer some pending questions regarding normalization of fracture risk and bone microarchitecture after long treatment with GFD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ludvigsson J, Leffler D, Bai JC, Biagi F, Fasano A, Green P, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43–52.
Ludvigsson J, Bai JC, Biagi F, Card TR, Ciacci C, Ciclitira PJ, et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut. 2014;63:1210–28.
Pintos Sanchez M, Premysl B, Verdu E, Bai JC. Extraintestinal manifestations of celiac disease. Dig Dis. 2015;33:147–54. Clear summary of all extraintestinal manifestations of celiac disease including bone health.
Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357(17):1731–43.
Rampertab SD, Pooran N, Brar P, et al. Trends in the presentation of celiac disease. Am J Med. 2006;119:355.e9–e14.
Plugis NM, Khosla C. Therapeutic approaches for celiac disease. Best Pract Res Clin Gastroenterol. 2015;29:503–21.
Corazza G, Di Stefano M, Mauriño E, Bai JC. Bones in coeliac disease: diagnosis and treatment. Best Pract Res Clin Gastroenterol. 2005;19:453–65.
Xing Y, Morgan SL. Celiac disease and metabolic bone disease. J Clin Densitom: Assess Manag Musculoskelet Health. 2013;16(4):439–44.
Fornari C, Pedreira S, Niveloni S, González D, Diez R, Vázquez H, et al. Pre- and post-treatment serum levels of cytokines IL-1β, IL-6, and IL-1 receptor antagonist in celiac disease. Are they related to the associated osteopenia? Am J Gastroenterol. 1998;93(3):413–8.
Sugai E, Cherñasky A, Pedreira S, Smecuol E, Vázquez H, Mazure R, et al. Bone specific antibodies in sera from patients with celiac disease. Characterization and implications in osteoporosis. J Clin Inmmunol. 2002;22:353–62.
Larussa T, Suraci E, Nazionale I, et al. Bone mineralization in celiac disease. Gastroenterol Res Pract 2012:1980–25.
González D, Mazure R, Mautalen C, Vazquez H, Bai JC. Body composition and bone mineral density in untreated and treated patients with celiac disease. Bone. 1995;16:231–4.
Ferretti J, Mazure R, Tanoue P, et al. Analysis of the structure and strength of bones inceliac disease patients. Am J Gastroenterol. 2003;98:382–90.
Duerksen DR, Leslie WD. Longitudinal evaluation of bone mineral density and body composition in patients with positive celiac serology. J Clin Densitom: Assess Skelet Health. 2011;14(4):478–83.
Rios LP, Khan A, Sultan M, McAssey K, Fouda MA, Armstrong D. Canadian. Approach to diagnosing celiac disease in patients with low bone mineral density or fragility fractures. Multidisciplinary task force report. Can Fam Phys. 2013;59:1055–61. Practical and useful clinical guideline for bone approach in CD patients.
Boutroy S, Bouxsein M, Munoz F, Delmas P. In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab. 2005;90:6508–15.
Zanchetta MB, Costa F, Longobardi V, Longarini G, Mazure RM, Moreno ML, et al. Significant bone microarchitecture impairment in premenopausal women with active celiac disease. Bone. 2015;76:149–57. First evidence of an important bone microarchitecture impairment in premenopausal women with CD at diagnosis.
Stein EM, Rogers H, Leib A, McMahon DJ, Young P, Nishiyama K, et al. Abnormal skeletal strength and microarchitecture in women with celiac disease. J Clin Endocrinol Metab. 2015;100:2347–53.
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32(5):468–73.
Vasquez H, Mazure R, Gonzalez D, Flores D, Pedreira S, Niveloni S, et al. Risk of fractures in celiac disease patients: a cross-sectional, case–control study. Am J Gastroenterol. 2000;95:183–9.
Olmos M, Antelo M, Vazquez H, Smecuol E, Mauriño E, Bai JC. Systematic review and meta-analysis of observational studies on the prevalence of fractures in coeliac disease. Dig Liver Dis. 2008;40:46–53.
Heikkilä K, Pearce J, Mäki M, Kaukinen K. Celiac disease and bone fractures: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(1):25–3.
Moreno ML, Vazquez H, Mazure R, Smecuol E, Niveloni S, Pedreira S, et al. Stratification of bone fracture risk in patients with celiac disease. Clin Gastroenterol Hepatol. 2004;2:127–34.
Pinto Sánchez MI, Mohaidle A, Baistrocchi A, et al. Risk of fracture in celiac disease: gender, dietary compliance, or both? World J Gastroenterol. 2011;17:3035–42.
American Gastroenterological Association. American gastroenterological association medical position statement: guidelines on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003;124:791–4.
Fouda MA, Khan AA, Sultan MS, Rios LP, McAssey K, Armstrong D. Evaluation and management of skeletal health in celiac disease: position statement. Can J Gastroenterol. 2012;26:819–29.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Endocrine Society. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Edwards MH, Dennison EM, Aihie Sayer A, Fielding R. Cooper C osteoporosis and sarcopenia in older age. Bone. 2015;80:126–30.
Acknowledgments
We thank Susana Carballo for editing the English language of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
María Belén Zanchetta, Vanesa Longobardi, and Julio César Bai declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All studies by authors involving animal and/or human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Additional information
This article is part of the Topical Collection on Secondary Causes of Osteoporosis
Rights and permissions
About this article
Cite this article
Zanchetta, M.B., Longobardi, V. & Bai, J.C. Bone and Celiac Disease. Curr Osteoporos Rep 14, 43–48 (2016). https://doi.org/10.1007/s11914-016-0304-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-016-0304-5