Abstract
Clinical practice guidelines universally recommend bone mineral density (BMD) screening to identify osteoporosis in women aged 65 years and older. Risk assessment is recommended to guide BMD screening in postmenopausal women under age 65. Insufficient data are available to inform standard ages to start and stop BMD screening in postmenopausal women. Based on longitudinal studies of incident osteoporosis and fracture in postmenopausal women, an initial BMD test should be ordered for all women aged 65, and the frequency of re-screening should be based on age and BMD T score (more frequent testing for older age and lower T score). Although clinical practice guidelines recommend BMD screening according to risk factors for fracture in postmenopausal women under age 65, no standard approach to risk assessment exists. Minimal evidence is available to guide osteoporosis screening in men, but some experts recommend initiation of BMD screening in men at age 70.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The past decade (2005–2015) has been an active period of progress in research on osteoporosis screening. This article reviews epidemiological issues in screening and highlights recent data on the use of bone mineral density (BMD) screening to identify osteoporosis in postmenopausal women and older men.
Key Components of the BMD Screening Program
The purpose of BMD screening is to identify a pre-symptomatic condition (osteoporosis) that can be treated to avoid morbidity and mortality from osteoporotic fractures [1]. The key components of a BMD screening program are as follows:
The Screened Population: Well Individuals
To meet the epidemiological criteria for a screened population, individuals who undergo BMD screening must be asymptomatic and without a history of fragility fracture (e.g., hip or clinical vertebral fracture), not taking pharmacologic treatment to prevent fractures, and without an identified secondary cause of osteoporosis [2].
Clinical Outcome: Major Osteoporotic Fracture
Fractures cause pain, immobility or impaired mobility, lost work days, and decreased quality of life and are associated with increased outpatient and inpatient costs that are especially high for hip fractures [3]. While both low-trauma and high-trauma fractures might be reduced by pharmacologic treatment in individuals with osteoporosis by BMD criteria or existing vertebral fracture [4], clinical trials have focused on agents to reduce “osteoporotic fractures” or “fragility fractures” associated with minimal trauma. No consensus exists regarding the specific fracture sites that should be considered “osteoporotic” or classified as fragility-related [5, 6]. Also, although lower BMD predicts fracture risk [7], most fractures in older adults occur in individuals who do not have osteoporosis by BMD criteria [8, 9]. In this article, we focus on the clinical outcome of “major osteoporotic fracture,” defined by the World Health Organization (WHO) to include clinical vertebral fractures and fractures at the hip, proximal humerus, or wrist [10]. Of these, hip and clinical vertebral fractures are the most clinically relevant fracture outcomes because of their associated high morbidity and mortality [11].
Target Condition of Screening: Osteoporosis by BMD Criteria
To define an appropriate target condition for BMD screening, the WHO developed diagnostic criteria for osteoporosis in 1994 based on the BMD T score (standard deviation from young normative BMD mean) at the lumbar spine and two sites at the hip (femoral neck and total hip) measured by dual energy x-ray absorptiometry (DXA) [12]. Osteoporosis was defined as a T score ≤−2.50 at any of the three sites, osteopenia as lowest T score between −2.50 and −1.00 (not inclusive) at any site, and normal BMD as T score ≥−1.00 at all sites [12].
The WHO described the T score cut point for osteoporosis as follows [12]:
“…all cut-off values are somewhat arbitrary, but a measured value of bone mineral more than 2.5 standard deviations below the mean for young healthy women at any site (spine, hip, mid-radius) identifies 30 % of all postmenopausal women as having osteoporosis, more than half of whom will have sustained a prior fracture of the proximal femur, spine, distal forearm, proximal humerus or pelvis.”
Despite the arbitrary and secular nature of the cut point, the clinical relevance of the −2.5 T score was later substantiated by multiple rigorous randomized, placebo-controlled trials demonstrating that treatment of osteoporosis by WHO diagnostic criteria reduced risk of clinical vertebral fractures and hip fractures, with less convincing evidence of reduction of fractures at other sites [13–18]. The most important working aspects of the WHO diagnostic criteria are as follows:
-
1.
The criteria apply to postmenopausal women and have been extrapolated to older men. Fracture risk cannot be accurately estimated by T scores measured in premenopausal women or young men, and those individuals are not candidates for screening and treatment within the general population.
-
2.
While densitometer manufacturers include BMD norms for both women and men, the International Osteoporosis Foundation [19] and the International Society for Clinical Densitometry [20] recommend that a uniform Caucasian (non-race-adjusted) female reference database should be used to calculate T scores for men of all ethnic groups. Some experts prefer to calculate T scores based on male norms, which results in a higher proportion of the male population being diagnosed as osteoporotic [21].
Osteoporosis by BMD criteria is still the target condition for screening that is substantiated by the highest level of evidence [2]. The efficacy of pharmacologic treatment in patients selected on the basis of fracture risk scores calculated with or without BMD has not been tested in randomized controlled trials [22]. In 2014, the National Bone Health Alliance proposed an alternative definition of “osteoporosis” that included osteoporosis by BMD criteria as well as hip fracture and osteopenia-associated vertebral, proximal humerus, pelvis or some wrist fractures, or 10-year fracture risk estimations of ≥3 % for hip or 20 % for major osteoporotic fracture calculated using the FRAX fracture risk tool [23]. This alternative definition cannot be used in studies of screening because it combines the target condition for screening (osteoporosis by BMD criteria) with the clinical outcome that screening attempts to prevent (fracture). This leads to time-to-disease estimates that are not interpretable for the prevention of fracture. Other experts have recommended against expansion of the definition of osteoporosis unless further evidence-based research shows that the benefits of such an expansion outweigh the harms [24].
Intervention for Screen-Positive Patients: Pharmacologic Treatment to Prevent Fracture
The clinical efficacy of screening depends on treatment efficacy, i.e., a screening program can only be successful if available treatments effectively reduce clinically detectable disease. If effective treatments are not available, a test with 100 % accuracy is useless. For this reason, randomized controlled trials of treatment precede randomized trials of screening.
In 2002, BMD screening programs were given a Grade C evidence rating (evidence substantiates offering or providing this service for selected patients depending on individual circumstances) by the US Preventive Services Task Force after data from randomized controlled trials demonstrated fragility fracture reduction in individuals with osteoporosis by BMD criteria who received pharmacologic treatment [25]. While the WHO’s −2.50 T score cut point was in some sense an arbitrary cutoff, it proved to be a clinically relevant threshold for primary fracture prevention in subsequent randomized controlled trials of pharmacologic treatment. To date, reduction in clinical fracture events has only been demonstrated in RCTs in postmenopausal women with osteoporosis by WHO diagnostic criteria or with existing radiographic vertebral fractures or history of clinical vertebral fractures or in patients with recent hip fracture regardless of their T score level [13–18].
Despite the lack of direct RCT evidence demonstrating that BMD screening reduces fractures or mortality, the USPSTF concluded in 2011 that the net benefit of osteoporosis screening was at least moderate in women aged 65 and older and in younger postmenopausal women with fracture risk at least as high as a 65-year-old white woman who has no additional risk factors (grade B evidence) [26]. This approach has not been tested prospectively and is problematic because of the low level of accuracy of the USPSTF risk assessment approach to identify younger postmenopausal women who later develop osteoporosis or major fracture [27, 28] (see “Postmenopausal Women/Age to Start Osteoporosis Screening”).
Other Uses of BMD Testing
Osteoporosis screening is one of several uses of BMD testing. BMD testing may also be ordered to rule out osteoporosis in patients with secondary causes of BMD loss, for treatment monitoring or for surveillance after a major fragility fracture event. In the latter cases, patients who undergo BMD testing have a different risk of future fracture than the general population and thereby no longer qualify for a “screening” BMD test.
Postmenopausal Women
According to estimates from the National Health and Nutrition Examination Survey (NHANES) 2005–2008, the prevalence of osteoporosis at the femoral neck or lumbar spine ranges from 6.8 % in women aged 50 to 59 to 34.9 % in women aged 80 and older [29]. Among US women aged 65 and older, approximately 25.1 % have osteoporosis (BMD value at least 2.5 standard deviation units below the mean) and 52.3 % have low bone mass (BMD value between 1.0 and 2.5 standard deviation units below the mean) calculated using BMD norms for young non-Hispanic white females, age-adjusted to the 2010 Census Bureau estimates [30]. A meta-analysis of data from 12 cohort studies including 29,082 women reported that at the age of 65 years, women’s risk ratio for hip fractures increased by 2.88 (95 % CI 2.31, 3.59) for each SD decrease in BMD, and their risk of osteoporotic fractures (including hip, humeral or limb fractures and fractures of the spine, pelvis, ribs, distal forearm and forearm, clavicle, scapula or sternum) increased by 1.38 (95 % CI, 1.28, 1.48) per SD decrease in BMD [31, 32].
Age to Start Osteoporosis Screening
No standard age for starting BMD screening is recommended in clinical practice guidelines. Epidemiological data suggest that mass osteoporosis screening and treatment in postmenopausal women under age 60 is likely to be very inefficient. For example, the USPSTF estimated the number needed to screen to prevent one hip fracture would be more than 4000 for women aged 50–59 due to low osteoporosis prevalence and low fracture risk before age 60 [33]. A 2008 Cochrane review estimated that the number needed to treat (NNT) for alendronate to prevent the first hip fracture was nonestimable in postmenopausal women aged 50–54 and 943 for women aged 55–59, and the NNT to prevent the first vertebral fracture was 1111 for aged 50–54 and 556 for aged 55–59 [34]. A review of the cost-effectiveness literature concluded that treatment with bisphosphonates is likely to be cost-effective in populations aged 70 and older, but that “the younger the cohorts and the fewer risk factors they have, the less cost-effective treatment with a bisphosphonate is” [35].
No data are available on the benefit of osteoporosis treatment beginning at age 50–59 and continuing over three or four decades. Because of rapid rates of BMD loss and trabecular perforation during the perimenopausal transition, some experts have proposed antiresorptive treatment during early menopause [36], However, the long-term benefit of early therapy may be limited because of drug washout after discontinuation. Hormone therapy used in the early postmenopausal period does not confer fracture protection after discontinuation [37]. Similarly, withdrawal of alendronate leads to BMD declines within 2 years [38, 39]. Potential harms from early therapy must also be considered. Because younger postmenopausal women have lower immediate risk of fragility fractures, they are substantially more likely than postmenopausal women aged 60 and older to sustain harms that outweigh benefits from early treatment. Harms of screening include knowledge of low bone density that causes anxiety despite lack of symptoms [40]. Early treatment may lead to prolonged bisphosphonate use, which has been associated with osteonecrosis of the jaw [41, 42] and atypical femoral fractures [43, 44]. Finally, overtreating younger postmenopausal women when their fracture risk is low may leave them with few or no treatment options in their early 70s, when hip fractures start to increase exponentially [45]. This could potentially decrease the lifetime potential for net treatment benefit.
In the absence of definitive data on the optimal age to start BMD screening, clinical practice guidelines recommend consideration of BMD testing in postmenopausal women as young as 50 years, with risk factor assessment to guide the decision to order testing from age 50 to 64 [46, 47]. In its 2010 systematic review on osteoporosis screening, the USPSTF assessed studies of 21 externally validated clinical risk-assessment tools including 1 to more than 15 variables [48]. Most of the tools included age, weight or body mass index, and previous fracture. Risk tools to predict low BMD (area under the curve [AUC], 0.13 to 0.87) and fractures (AUC, 0.48 to 0.89) were evaluated; simple and complex instruments performed similarly. No tool demonstrated high AUC estimates in several studies. “Important methodological limitations of studies include nonrepresentative samples, cross-sectional rather than prospective data collection, inconsistent performance of the reference standard, and differences in performance measures across studies” [48]. A 2014 diagnostic accuracy analysis found that the Osteoporosis Self-assessment Tool (OST) and the Simple Calculated Osteoporosis Risk Estimate (SCORE) risk assessment tool had fair to poor diagnostic accuracy and that the US Preventive Services Task Force risk assessment strategy based on a fracture risk score had poor diagnostic accuracy to identify postmenopausal women aged 50 to 64 with incident osteoporosis by BMD criteria or major osteoporotic fracture over the subsequent 10 years [27, 28]. While the principle behind risk assessment to decide a screening test has face validity, a two-step process of risk assessment followed by BMD screening decision has not been tested prospectively, and there is no consensus regarding which risk factors or which risk tools to use for selection of candidates for BMD screening [49].
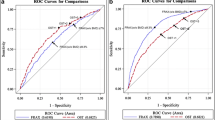
In a study of osteoporosis incidence in postmenopausal women aged 50 to 64 at baseline participating in the Women’s Health Initiative [50], tabulations of fracture events (Table 1) during study follow-up suggested that the lowest T scores within the osteopenia range (T score −2.49 to −2.00) were relatively infrequent but occurred across all age ranges of younger postmenopausal women. Development of osteoporosis by BMD criteria over 11 years of follow-up was rare in those who had baseline T scores >−1.50. The longitudinal results for this study (Fig. 1) also indicated that younger postmenopausal women with baseline T scores −2.49 to −2.00 transitioned to osteoporosis as rapidly as women aged 67 and older. These findings suggest that DXA testing has a role for some postmenopausal women across the age range of 50 to 64. However, evidence is lacking to inform a standard approach to selection of the best candidates for BMD screening and optimal timing of treatment in this age range.
A 2015 analysis documented a decrease in the BMD testing rate in commercially insured postmenopausal women aged 50 to 64 between 2006 and 2012, during a time period when Medicare reimbursement for DXA BMD testing declined significantly [51]. An estimated 667,982 DXA scans were performed for younger postmenopausal women in 2012, compared to an estimated 2,338,240 DXA tests performed in physician offices and hospitals for Medicare beneficiaries in 2009 [51, 52].
Osteoporosis Screening Intervals
Decisions regarding bone density screening intervals were initially based on machine precision specifications, i.e., the magnitude of the change in BMD that indicates real biological change, called the least significant change (LSC) [53]. A 2007 prospective observational study suggested that a second DXA BMD test up to 8 years after the first provided little additional fracture prediction in women aged 65 years and older [54]. A 2009 population-based study including 1008 women and 750 men aged 60 years and older at baseline estimated the time to development of osteoporosis or incident fragility fracture [55]. This study contributed important information regarding fracture risk stratification according to age and BMD T score; however, results were difficult to interpret with respect to osteoporosis screening because the pre-symptomatic condition of osteoporosis was combined with fragility fractures in the outcome measure.
A 2012 longitudinal study of 4957 women aged 67 and older at baseline tested a BMD screening interval defined as the estimated time for 10 % of women to transition from normal BMD or osteopenia to osteoporosis. Important aspects of the study with respect to clinical implementation included its large size, 15 years of concurrent imaging and fracture follow-up, and methodology that treated pharmacologic treatment and incident hip and spine fracture as competing risks rather than censoring criteria. The same authors documented time-to-fracture estimates according to baseline age groups of postmenopausal women aged 50 to 64 in an effort to separate age groups at lower and higher risk of major osteoporotic fracture [50].
A comparison of the cumulative incidence of osteoporosis in women aged 67 and older participating in the Study of Osteoporotic Fractures (SOF) vs. women aged 50 to 64 participating in the Women’s Health Initiative (WHI) from the latter two analyses is shown in Fig. 1 [50, 56••]. Figure 1 demonstrates that postmenopausal women aged 50 and older with baseline T scores between −2.49 and −2.00 may have a rapid transition to osteoporosis. Conversely, postmenopausal women with baseline T scores >−1.50 transition to osteoporosis much more slowly. For postmenopausal women aged 50 to 64 who undergo BMD testing and have baseline T scores >−1.50, the transition to osteoporosis is so slow that clinicians might consider deferring the next DXA test to age 65, the age at which routine BMD screening is recommended for all women.
While time-to-osteoporosis estimates are helpful, the timing of screening intervals is still a subjective decision in primary care practice. Results from the cited studies are only relevant for the screened population of well individuals, not patients with pre-existing fracture, treatment, or secondary causes of osteoporosis. The plots in Fig. 1 use a 10 % incidence threshold as the metric, i.e., the estimated time for 10 % of the T score group or age group to develop osteoporosis. A lower or higher threshold might be considered according to the patient’s baseline risk factors for fracture or because of the patient’s past history.
Age to Stop Osteoporosis Screening
An age to stop or decrease use of BMD testing has not been examined, and policy statements do not recommend cessation of screening at a specific age. In women aged 70 to 80 years at baseline, osteoporosis treatment is effective and mass BMD screening has been assessed as more cost-effective than no screening or screening only in women with at least one risk factor for fracture [13, 57–60]. Women aged 80 and older are less well studied because they are represented in smaller numbers in cohort studies of BMD and fracture. With increasing age, the rate of non-fracture death greatly outweighs fracture-related deaths, making BMD screening less likely to be beneficial.
Older Men
According to estimates from the NHANES 2005–2008 [29], the prevalence of osteoporosis at the femoral neck or lumbar spine ranges from 3.4 % in men aged 50 to 59 to 10.9 % in men aged 80 and older [29]. Among US men aged 65 and older, approximately 5.7 % have osteoporosis (BMD value at least 2.5 standard deviation units below the mean) and 44.2 % have low bone mass (BMD value between 1.0 and 2.5 standard deviation units below the mean) calculated using BMD norms for young non-Hispanic white females, age-adjusted to the 2010 Census Bureau estimates [30]. A meta-analysis of data from 12 cohort studies including 9891 men reported that at the age of 65 years, men’s risk ratio for hip fractures increased by 2.94 (95 % CI, 2.02, 4.27) for each SD decrease in BMD, and their risk of osteoporotic fractures (including hip, humeral or limb fractures and fractures of the spine, pelvis, ribs, distal forearm and forearm, clavicle, scapula or sternum) increased by 1.41 (95 % CI, 1.33, 1.51) per SD decrease in BMD [31, 32].
Osteoporosis and Fracture Risk in Men
A 1998 prospective study of a Dutch cohort of 7046 individuals (2778 men) aged 55 years and older suggested that the risk of hip fracture in men and women is similar at the same femoral neck absolute bone density level [61], but a 2006 analysis found that men aged 65 and older had a lower risk of fracture at every T score of hip BMD compared to same-aged women [62]. On average, men have higher BMD than age-matched women throughout life, and their rate of BMD loss in older age is slower than that for women [63]. As a result, fewer men develop osteoporosis, and fragility fractures occur less often in men than in women.
Despite lower overall fracture incidence, men have greater morbidity and mortality associated with hip fractures compared to women. Men are more likely than women to die within 1 year after a hip fracture [64]. Almost one third of men with hip fractures have subsequent fractures (of any type) during their remaining lifetime [65]. After a hip fracture, most new fractures occur in relatively younger men within 5 years, whereas most aged 75 and older die before experiencing a new fracture [65]. Fractures at typical osteoporotic sites are associated with increased mortality across all age groups of women and men, particularly in men [66–71].
Evidence for Pharmacologic Treatment Efficacy in Men
Treatment with oral bisphosphonates is effective in reducing risk of incident radiographic vertebral fractures in RCTs up to 3 years in length conducted in men aged 30s to 80s, about half of whom had existing radiographic vertebral fracture and many of whom had osteoporosis by BMD criteria at baseline [72–78]. A 2012 randomized controlled trial of older men with osteoporosis treated with zoledronic acid demonstrated significant reduction in the primary endpoint of radiographic vertebral fracture [79••]. However, no RCT has demonstrated prevention of clinical fractures in men with or without osteoporosis at baseline.
The optimal T score cut point for treatment is uncertain for older men, but data from Ensrud et al. suggest that older men with T scores ≤−2.50 calculated using BMD norms for young white women may be most likely to benefit from pharmacologic treatment to reduce fracture [80••].
Lack of a BMD Screening Protocol in Men
No standard BMD screening schedule exists for men, but several subspecialty organizations have offered recommendations based on expert opinion. Based on literature reviews by expert panels, the National Osteoporosis Foundation [46] and International Society for Clinical Densitometry [81] supported BMD screening in all men aged 70 and older and in men aged 50 to 69 with clinical risk factors for fracture. The American College of Physicians recommended that osteoporosis risk factors be evaluated in men aged 50 to 69 to determine whether DXA testing should be considered [82, 83]. They listed important osteoporosis risk factors in men to be age (>70 years), low body weight (body mass index <20 to 25 kg/m2), weight loss, physical inactivity, corticosteroid use, androgen deprivation therapy, and previous fragility fracture. Studies are needed to compare performance of strategies to identify older men who are candidates for osteoporosis screening.
Conclusions
The state of the art of BMD screening has been strengthened by new data published since 2005. Despite a number of studies of risk assessment tools to select postmenopausal women under age 65 for osteoporosis screening, no standard approach has been tested prospectively. The very low fracture risk in women aged 50 to 54 argues against frequent screening in this age range. Clinical guidelines universally recommend routine BMD screening in women aged 65 and older, and recent data suggest that women with baseline T scores ≤−1.50 can benefit from more frequent BMD screening than women with T scores >−1.50. Minimal evidence exists to inform BMD screening in older men, and studies are needed to compare the performance of potential strategies to select individuals for osteoporosis screening in this population.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R. Diagnosis and screening. Evidence-based medicine: how to practice and teach EBM. 2nd ed. New York: Harcourt; 2000. p. 261.
Gourlay ML, Preisser JS, Lui LY, Cauley JA, Ensrud KE. BMD screening in older women: initial measurement and testing interval. J Bone Mineral Res Off J Am Soc Bone Mineral Res. 2012;27(4):743–6. doi:10.1002/jbmr.1585.
Burge R, Dawson-Hughes B, Solomon D, Wong J, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75.
Mackey DC, Black DM, Bauer DC, McCloskey EV, Eastell R, Mesenbrink P, et al. Effects of antiresorptive treatment on nonvertebral fracture outcomes. J Bone Miner Res. 2011;26(10):2411–8. doi:10.1002/jbmr.446.
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2005;16 Suppl 2:S3-7. doi:10.1007/s00198-004-1702-6
Sanchez-Riera L, Wilson N, Kamalaraj N, Nolla JM, Kok C, Li Y, et al. Osteoporosis and fragility fractures. Best Pract Res Clin Rheumatol. 2010;24(6):793–810. doi:10.1016/j.berh.2010.10.003.
Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–9.
Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA, et al. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab. 2005;90(5):2787–93. doi:10.1210/jc.2004-1568.
Stone K, Seeley D, Lui L, Cauley J, Ensrud K, Browner W, et al. BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res. 2003;18:1947–54.
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E. FRAX and its applications to clinical practice. Bone. 2009;44(5):734–43. doi:10.1016/j.bone.2009.01.373.
Ensrud KE. Epidemiology of fracture risk with advancing age. J Gerontol A Biol Sci Med Sci. 2013;68(10):1236–42. doi:10.1093/gerona/glt092.
Wilks DC, Winwood K, Gilliver SF, Kwiet A, Chatfield M, Michaelis I, et al. Bone mass and geometry of the tibia and the radius of master sprinters, middle and long distance runners, race-walkers and sedentary control participants: a pQCT study. Bone. 2009;45(1):91–7. doi:10.1016/j.bone.2009.03.660.
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;1:CD001155. doi:10.1002/14651858.CD001155.pub2.
Wells G, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;1:CD004523.
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357(18):1799–809. doi:10.1056/NEJMoa074941.
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282(7):637–45.
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19):1434–41. doi:10.1056/NEJM200105103441904.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–65. doi:10.1056/NEJMoa0809493.
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8(1-2):136. doi:10.1007/s11657-013-0136-1.
Watts NB, Leslie WD, Foldes AJ, Miller PD. 2013 International Society for Clinical Densitometry Position Development Conference: Task Force on Normative Databases. J Clin Densitometry Off J Int Soc Clin Densitometry. 2013;16(4):472–81. doi:10.1016/j.jocd.2013.08.001.
Richy F, Gourlay ML, Garrett J, Hanson L, Reginster JY. Osteoporosis prevalence in men varies by the normative reference. J Clin Densitom. 2004;7(2):127–33.
Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD. FRAX((R)) with and without bone mineral density. Calcif Tissue Int. 2012;90(1):1–13. doi:10.1007/s00223-011-9544-7.
Siris ES, Adler R, Bilezikian J, Bolognese M, Dawson-Hughes B, Favus MJ et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2014;25(5):1439-43. doi:10.1007/s00198-014-2655-z.
Schousboe JT, Ensrud KE. Diagnostic criteria for osteoporosis should not be expanded. Lancet Diabetes Endocrinol. 2015;3(4):236–8. doi:10.1016/S2213-8587(15)00050-9.
Screening for osteoporosis in postmenopausal women: recommendations and rationale. Annals of internal medicine. 2002;137(6):526-8.
Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154(5):356-64. Doi: 10.1059/0003-4819-154-5-201103010-00307.
Crandall CJ, Larson J, Gourlay ML, Donaldson MG, Lacroix A, Cauley JA, et al. Osteoporosis screening in postmenopausal women 50-64 years-old: comparison of U.S. Preventive Services Task Force Strategy and two traditional strategies in the Women's Health Initiative. J Bone Mineral Res Off J Am Soc Bone Mineral Res. 2014. doi:10.1002/jbmr.2174.
Crandall CJ, Larson JC, Watts NB, Gourlay ML, Donaldson MG, LaCroix A, et al. Comparison of fracture risk prediction by the US Preventive Services Task Force strategy and two alternative strategies in women 50-64 years old in the Women's Health Initiative. J Clin Endocrinol Metab. 2014;99(12):4514–22. doi:10.1210/jc.2014-2332.
Looker AC, Melton 3rd LJ, Borrud LG, Shepherd JA. Lumbar spine bone mineral density in US adults: demographic patterns and relationship with femur neck skeletal status. Osteoporos Int. 2012;23(4):1351–60. doi:10.1007/s00198-011-1693-z.
Looker AC, Frenk SM. Percentage of adults aged 65 and over with osteoporosis or low bone mass at the femur neck or lumbar spine: United States, 2005–2010. National Center for Health Statistics. August 2015. Available from: http://www.cdc.gov/nchs/data/hestat/osteoporsis/osteoporosis2005_2010.htm
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20(7):1185–94. doi:10.1359/JBMR.050304.
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int. 2001;12(5):417–27. doi:10.1007/s001980170112.
Nelson H, Helfand M, Woolf S, Allan J. Screening for postmenopausal osteoporosis: a review of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2002;137:529–41.
Wells G, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;1:CD001155.
Fleurence RL, Iglesias CP, Johnson JM. The cost effectiveness of bisphosphonates for the prevention and treatment of osteoporosis: a structured review of the literature. Pharmacoeconomics. 2007;25(11):913–33.
Zaidi M, Turner CH, Canalis E, Pacifici R, Sun L, Iqbal J, et al. Bone loss or lost bone: rationale and recommendations for the diagnosis and treatment of early postmenopausal bone loss. Curr Osteoporos Rep. 2009;7(4):118–26.
Castelo-Branco C, Davila J, Perello MF, Peguero A, Ros C, Martinez-Serrano MJ, et al. Long-term effect of hormone therapy on bone in early menopause: vertebral fractures after 20 years. Climacteric. 2014;17(4):336–41. doi:10.3109/13697137.2013.871511.
Ravn P, Weiss SR, Rodriguez-Portales JA, McClung MR, Wasnich RD, Gilchrist NL, et al. Alendronate in early postmenopausal women: effects on bone mass during long-term treatment and after withdrawal. Alendronate Osteoporosis Prevention Study Group. J Clin Endocrinol Metab. 2000;85(4):1492–7. doi:10.1210/jcem.85.4.6549.
Ravn P, Bidstrup M, Wasnich RD, Davis JW, McClung MR, Balske A, et al. Alendronate and estrogen-progestin in the long-term prevention of bone loss: four-year results from the early postmenopausal intervention cohort study. A randomized, controlled trial. Ann Intern Med. 1999;131(12):935–42.
Cummings SR. A 55-year-old woman with osteopenia. JAMA. 2006;296(21):2601–10. doi:10.1001/jama.296.21.2601.
Woo SB, Hellstein JW, Kalmar JR. Narrative [corrected] review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144(10):753–61.
Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, et al. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg. 2008;66(6):1320–1. doi:10.1016/j.joms.2008.01.054. author reply 1-2.
Odvina CV, Levy S, Rao S, Zerwekh JE, Rao DS. Unusual mid-shaft fractures during long-term bisphosphonate therapy. Clin Endocrinol (Oxford). 2010;72(2):161–8. doi:10.1111/j.1365-2265.2009.03581.x.
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294–301. doi:10.1210/jc.2004-0952.
Banks E, Reeves GK, Beral V, Balkwill A, Liu B, Roddam A. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis. PLoS Med. 2009;6(11):e1000181. doi:10.1371/journal.pmed.1000181.
Runhaar J, Schiphof D, van Meer B, Reijman M, Bierma-Zeinstra SM, Oei EH. How to define subregional osteoarthritis progression using semi-quantitative MRI Osteoarthritis Knee Score (MOAKS). Osteoarthr Cartil. 2014;22(10):1533–6. doi:10.1016/j.joca.2014.06.022.
Baim S, Binkley N, Bilezikian J, Kendler D, Hans D, Lewiecki E, et al. Official Positions of the International Society for Clinical Densitometry and Executive Summary of the 2007 ISCD Position Development Conference. J Clin Densitom. 2008;11:75–91.
Nelson H, Haney E, Dana T, Bougatsos C, Chou R. Screening for osteoporosis: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2010;153:1–13.
Schousboe JT, Gourlay ML. Comparative effectiveness and cost-effectiveness of strategies to screen for osteoporosis in postmenopausal women. Ann Intern Med. 2011;155(11):788–9. doi:10.1059/0003-4819-155-11-201112060-00012.
Gourlay ML, Overman RA, Fine JP, Ensrud KE, Crandall CJ, Gass ML, et al. Baseline age and time to major fracture in younger postmenopausal women. Menopause. 2014. doi:10.1097/GME.0000000000000356.
Overman RA, Farley JF, Curtis JR, Zhang J, Gourlay ML, Deal CL. DXA utilization between 2006 and 2012 in commercially insured younger postmenopausal women. J Clin Densitometry Off J Int Soc Clin Densitometry. 2015;18(2):145–9. doi:10.1016/j.jocd.2015.01.005.
Zhang J, Delzell E, Zhao H, Laster AJ, Saag KG, Kilgore ML, et al. Central DXA utilization shifts from office-based to hospital-based settings among medicare beneficiaries in the wake of reimbursement changes. J Bone Mineral Res Off J Am Soc Bone Mineral Res. 2012;27(4):858–64. doi:10.1002/jbmr.1534.
Bonnick S, Johnston CJ, Kleerekoper M, Lindsay R, Miller P, Sherwood L, et al. Importance of precision in bone density measurements. J Clin Densitom. 2001;4:105–10.
Hillier T, Stone K, Bauer D, Rizzo J, Pedula K, Cauley J, et al. Evaluating the value of repeat bone mineral density measurement and prediction of fractures in older women. Arch Intern Med. 2007;167:155–60.
Frost S, Nguyen N, Center J, Eisman J, Nguyen T. Timing of repeat BMD measurements: development of an absolute risk-based prognostic model. J Bone Miner Res. 2009;24:1800–7.
Gourlay ML, Fine JP, Preisser JS, May RC, Li C, Lui LY, et al. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366(3):225–33. doi:10.1056/NEJMoa1107142. This competing risk analysis estimated the time to incident osteoporosis by BMD criteria for women aged 67 and older followed for up to 15 years in the Study of Osteoporotic Fractures. The time for 10% of women with baseline T-scores > -1.50 to transition to osteoporosis was approximately 17 years. The corresponding time intervals for women with baseline T-scores -1.50 to -1.99 and -2.00 to -2.49 were 5 years and 1 year respectively.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures Fracture Intervention Trial Research Group. Lancet. 1996;348(9041):1535–41.
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344(5):333–40. doi:10.1056/NEJM200102013440503.
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C. Meta-analyses of therapies for postmenopausal osteoporosis. IX: Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002;23(4):570–8.
Schott A, Ganne C, Hans D, Monnier G, Gauchoux R, Krieg M, et al. Which screening strategy using BMD measurements would be most cost effective for hip fracture prevention in elderly women? A decision analysis based on a Markov model. Osteoporos Int. 2007;18:143–51.
De Laet CE, Van Hout BA, Burger H, Weel AE, Hofman A, Pols HA. Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res. 1998;13(10):1587–93. doi:10.1359/jbmr.1998.13.10.1587.
Cummings SR, Cawthon PM, Ensrud KE, Cauley JA, Fink HA, Orwoll ES. BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res. 2006;21(10):1550–6. doi:10.1359/jbmr.060708.
Berger C, Langsetmo L, Joseph L, Hanley DA, Davison KS, Josse R, et al. Change in bone mineral density as a function of age in women and men and association with the use of antiresorptive agents. CMAJ. 2008;178(13):1660–8. doi:10.1503/cmaj.071416.
Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007;17(7):514–9. doi:10.1016/j.annepidem.2006.12.004.
von Friesendorff M, McGuigan FE, Besjakov J, Akesson K. Hip fracture in men-survival and subsequent fractures: a cohort study with 22-year follow-up. J Am Geriatr Soc. 2011;59(5):806–13. doi:10.1111/j.1532-5415.2011.03399.x.
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90. doi:10.1059/0003-4819-152-6-201003160-00008.
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int. 2011;22(9):2439–48. doi:10.1007/s00198-010-1480-2.
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–21. doi:10.1001/jama.2009.50.
Robbins JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the cardiovascular health study. J Am Geriatr Soc. 2006;54(12):1885–91. doi:10.1111/j.1532-5415.2006.00985.x.
Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10(1):73–8.
Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82(8):1147–50.
Orwoll E, Ettinger M, Weiss S, Miller P, Kendler D, Graham J, et al. Alendronate for the treatment of osteoporosis in men. N Engl J Med. 2000;343(9):604–10. doi:10.1056/NEJM200008313430902.
Ringe JD, Faber H, Dorst A. Alendronate treatment of established primary osteoporosis in men: results of a 2-year prospective study. J Clin Endocrinol Metab. 2001;86(11):5252–5.
Ringe JD, Dorst A, Faber H, Ibach K. Alendronate treatment of established primary osteoporosis in men: 3-year results of a prospective, comparative, two-arm study. Rheumatol Int. 2004;24(2):110–3. doi:10.1007/s00296-003-0388-y.
Sawka AM, Papaioannou A, Adachi JD, Gafni A, Hanley DA, Thabane L. Does alendronate reduce the risk of fracture in men? A meta-analysis incorporating prior knowledge of anti-fracture efficacy in women. BMC Musculoskelet Disord. 2005;6:39. doi:10.1186/1471-2474-6-39.
Ringe JD, Farahmand P, Faber H, Dorst A. Sustained efficacy of risedronate in men with primary and secondary osteoporosis: results of a 2-year study. Rheumatol Int. 2009;29(3):311–5. doi:10.1007/s00296-008-0689-2.
Ringe JD, Faber H, Farahmand P, Dorst A. Efficacy of risedronate in men with primary and secondary osteoporosis: results of a 1-year study. Rheumatol Int. 2006;26(5):427–31. doi:10.1007/s00296-005-0004-4.
Boonen S, Orwoll ES, Wenderoth D, Stoner KJ, Eusebio R, Delmas PD. Once-weekly risedronate in men with osteoporosis: results of a 2-year, placebo-controlled, double-blind, multicenter study. J Bone Miner Res. 2009;24(4):719–25. doi:10.1359/jbmr.081214.
Boonen S, Reginster JY, Kaufman JM, Lippuner K, Zanchetta J, Langdahl B, et al. Fracture risk and zoledronic acid therapy in men with osteoporosis. N Engl J Med. 2012;367(18):1714–23. doi:10.1056/NEJMoa1204061. This randomized clinical trial demonstrated significant reduction of radiographic vertebral fracture in older men with osteoporosis treated with zoledronic acid. This was the first clinical trial of men that used fracture as the primary endpoint.
Ensrud KE, Taylor BC, Peters KW, Gourlay ML, Donaldson MG, Leslie WD, et al. Implications of expanding indications for drug treatment to prevent fracture in older men in United States: cross sectional and longitudinal analysis of prospective cohort study. BMJ. 2014;349:g4120. doi:10.1136/bmj.g4120. This observational study demonstrated that different choices of the definition of osteoporosis in men had major effects on the proportion of men identified as candidates for antifracture treatment. The prevalence of hip and major osteoporotic fracture by each definition suggested that men with osteoporosis by WHO diagnostic criteria are most likely to benefit from treatment.
Lewiecki E, Gordon C, Baim S, Leonard M, Bishop N, Bianchi M, et al. International Society for Clinical Densitometry 2007 adult and pediatric official positions. Bone. 2008;43:1115–21.
Liu H, Paige NM, Goldzweig CL, Wong E, Zhou A, Suttorp MJ, et al. Screening for osteoporosis in men: a systematic review for an American College of Physicians guideline. Ann Intern Med. 2008;148(9):685–701.
Qaseem A, Snow V, Shekelle P, Hopkins Jr R, Forciea MA, Owens DK. Screening for osteoporosis in men: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(9):680–4.
Acknowledgments
We acknowledge Anne Looker PhD and Steven M. Frenk for providing data in NCHS Health E-Stat that was important for our discussion of osteoporosis in men.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
ᅟ
Conflict of Interest
Dr. Gourlay is supported by Grant Number R01 AG046294 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the funding agency.
Dr. Overman and Dr. Ensrud have nothing to disclose.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Epidemiology and Pathophysiology
Rights and permissions
About this article
Cite this article
Gourlay, M.L., Overman, R.A. & Ensrud, K.E. Bone Density Screening and Re-screening in Postmenopausal Women and Older Men. Curr Osteoporos Rep 13, 390–398 (2015). https://doi.org/10.1007/s11914-015-0289-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-015-0289-5