Abstract
Purpose of Review
Approximately 15% of prostate cancer patients have lymph node metastases at the time of radical prostatectomy (RP). However, there is no universally accepted standard of care for these men. The options for treatment in this subset of patients range from observation to a combination of adjuvant androgen deprivation therapy (aADT) and radiation therapy (RT).
Recent Findings
A recent systematic review showed that there was no clear choice out of the options above to treat these patients. Studies have shown that patients treated with adjuvant radiation therapy have lower all-cause mortality when compared to patients treated with salvage radiation therapy.
Summary
In this review, we summarize treatment options for pathologic node-positive (pN1) patients and discuss the urgent need for robust clinical trials that includes observation as the control group to help establish a standard of care for treating patients with node-positive prostate cancer after RP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2022, prostate cancer is estimated to be the most common cancer diagnosed in men (27% of cancer diagnoses) in the USA and the second leading cause of cancer deaths in men (11% of cancer deaths) [1]. Although prostate cancer screening has been considered by many to be quite effective, available level 1 evidence supports the limited use of serum prostate-specific antigen (PSA) test in men ages 55 to 69 years old based on the principle of a shared decision [2]. Treatment of prostate cancer is usually guided by a risk stratification system which includes clinical T stage, serum PSA, grade group (Gleason score), and tumor volume on biopsy. Based on this model, clinically localized prostate cancer ranges from low- to high-risk [3]. The definitive treatment for prostate cancer such as radical prostatectomy (RP) or radiotherapy (RT) is recommended for patients with intermediate to high-risk prostate cancer [3].
Among patients with intermediate- and high-risk prostate cancer undergoing RP, simultaneous pelvic lymph node dissection (PLND) is generally recommended. Following PLND, approximately 15% have lymph node metastasis at the time of surgery [4]. Men who are diagnosed with lymph node invasion at the time of RP (pN1) have a higher cancer specific mortality when compared to men with nonmetastatic disease [5]. There is a plethora of treatment options for pN1 prostate cancer and include observation, androgen deprivation therapy (ADT), adjuvant radiotherapy (aRT), and a combination of aRT with limited ADT [6]. Notwithstanding, there is no clearly established standard of care for men with pN1 prostate cancer. Such uncertainty is due in large part to the lack of level 1 evidence comparing observation versus the commonly used treatment modalities.
Per NCCN (National Comprehensive Cancer Network) guideline, several management options are available in the setting of pN1 disease. ADT ± External Beam Radiation Therapy (EBRT) may be used as an initial treatment option for these patients. Another option involves observation of these patients and monitoring with serial PSAs. Using this management option, the decision to initiate treatment can be made on the basis of a detectable and rising PSA or PSA > 0.1 ng/mL. Considering this guideline statement, the treatment decision for pN1 consists of varying options and is ultimately left up to the discretion of the physician [7]. EUA guideline offers a similar perspective in that men with pN1 prostate cancer should be offered one of three options which include adjuvant ADT, adjuvant ADT with additional radiation therapy, or observation in men with \(\le\) 2 lymph nodes and a PSA < 0.1 ng/mL [8].
As for utilization of these varying treatment options, Touijer et al. published a comparative analysis of the different management approaches and found that of 1338 patients, 387 (28%) were observed, 676 (49%) received lifelong adjuvant androgen deprivation therapy, and 325 (23%) received adjuvant external beam radiation therapy (ERBT) and ADT [9].
In this review, we summarize the published data on the treatment outcomes of patients with pN1 prostate cancer. Furthermore, we advocate the need for level-one evidence on the therapeutic value of observation.
Observation
Outcomes of observation in men with pN1 prostate cancer have been analyzed primarily as single-center case series (Table 1).
However, there is one randomized clinical trial (RCTs) that included observation as the control. This trial compared observation to adjuvant ADT (aADT) by randomizing 98 patients 1:1. Follow-up included the regular assessment of PSA with subsequent salvage treatment on symptomatic progression or evidence of distant metastases. At a median follow-up of 7.1 years, there was a clinically significant difference in overall survival with death in 7 of 47 men treated with immediate ADT compared to 18 of 51 men who were observed (p = 0.02). This difference in overall survival and prostate cancer-specific survival remained significant with the longer follow-up of 11.9 years (HR 1.84 [1.01–3.34] and HR 4.09 [1.76–9.49], respectively). However, this study’s shortcomings include being under-powered (221 was the target accrual) and lacking central pathology review [10, 11]. In addition, this study was initiated in the pre-PSA era and accordingly, many patients in the observation arm likely have received delayed salvage treatments.
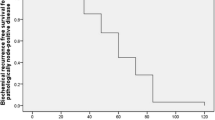
Since this RCT, several single-center analyses have been performed and reported survival outcomes in patients who had delayed initiation of ADT or other therapies. One such series followed 445 men with pN1 prostate cancer following RP with plans to offer salvage treatment (salvage ADT with or without salvage RT) to those with biochemical recurrence (BCR), defined as PSA > 0.1 with confirmatory rise. A 10-year OS of 60% and prostate cancer-specific survival of 72% was observed with Gleason grade > 7 and 3 + LN correlating with an increased risk of BCR [12].
For the remaining single-center observation studies, the observation protocols included an institutionally variable follow-up until BCR (PSA > 0.2 ng/mL) at which point salvage treatment such as ADT or RT was offered. A limitation of these single-center series was the lack of consistent reporting when and why salvage treatment was given while some studies did not report the indications. One such study is a retrospective review of 150 patients with pN1 disease who were followed with serum PSA and physical exam every 4–6 months in year one, every 6 months in years 2 and 3, and annually thereafter. BCR (defined as > 0.2) or symptomatic progression triggered radiographic evaluation (CT or MRI). 10-year OS and biochemical recurrence-free survival (bRFS) were 81% and 59%, respectively. The cohort consisted of most of the men with < 3 positive nodes and only 40% had Gleason > 8 prostate cancer [13].
A recent systematic review comparing 6 single center analyses demonstrated a BCR rate of 63% for all included patients, with cancer-specific survival (CSS) rates ranging from 78 to 72% at 5 to 10 years [6, 12,13,14,15,16]. The majority of these studies reported observation until BCR (defined at PSA > 0.2) at which point salvage therapy was offered (ADT, RT, or both depending on study). Like prior studies, a large proportion of the studies included patients with favorable characteristics, i.e., Gleason < 8 and 63% only had 1 positive node.
Most of the data supporting observation in the initial management of pN1 prostate cancer following RP is predominantly based on single-center analyses. There is a lack of level 1 evidence supporting the benefit of adjuvant therapy. Considering some of the data above, adjuvant therapy may not be necessary in patients with favorable characteristics including low-volume disease.
Adjuvant Androgen Deprivation Therapy
For the past 80 years, androgen deprivation therapy (ADT) has been the cornerstone of systemic treatment for prostate cancer [17]. ADT is typically performed through chemical castration, with the goal of achieving a total serum testosterone level of < 50 ng/dl [18]. Androgen plays many key roles in normal physiology and, therefore, ADT is associated with many adverse effects. These include decreased bone mineral density and muscle mass, increased insulin resistance, weight gain, decreased libido, gynecomastia, anemia, and fatigue [19]. More recently, ADT has been associated with an increased risk of cardiovascular events and cognitive impairment. Therefore, although ADT has shown survival benefit in pN1 patients [11], aADT in these men remains controversial (Table 2).
It should also be noted that some studies have shown no OS benefit for patients receiving aADT after RP. Wong et al. investigated men between 1991 and 1999 who had node-positive PCa after RP using the surveillance, epidemiology, and end results (SEER) database. In a cohort of 731 men, 209 of whom received ADT within 120 days after surgery, there was no statistically significant improvement in 10-year OS (HR: 0.95; 95% CI: 0.71 to 1.27) or in PCa-specific mortality (HR: 0.97; 95% CI, 0.56 to 1.68) in patients who received early ADT [20]. Touijer et al. reported survival outcomes for men with node-positive prostate cancer after RP between 1988 and 2010 treated with aADT versus observation. A total of 676 men treated with aADT were compared to 387 men who were observed. With a median follow up of 69 months, patients treated with aADT had no significant difference in OS when compared to men on observation (HR: 0.90, 95% CI: 0.65–1.25, p = 0.5). Patients on aADT had better CSS compared to the observation group (HR: 0.64, 95% CI: 0.43 to 0.95, p = 0.027); however, men treated with aADT had an increased risk of mortality from other causes (HR: 3.05, 95% CI: 1.45 to 6.40, p = 0.003) [9]. Park et al. showed similar results. Of a total of 40 patients with node positive disease, 18 patients received aADT for 2 years and 22 patients were observed. At 5 years PFS, CSS, and OS rates were similar in both groups [21].
Given the inconsistency of the data in support of aADT and its long-term side-effects, aADT is not routinely used. Patients with more aggressive pathology findings (i.e., multiple positive nodes) may benefit the most from aADT.
Adjuvant RT and ADT
Another treatment regimen frequently utilized in treating pN1 prostate cancer patients is the combination therapy in which both adjuvant androgen deprivation therapy (aADT) and adjuvant radiation therapy (aRT) are employed. Radiation therapy is typically applied to the whole pelvis. Radiation therapy is rarely used as a single modality to treat this subset of patients. Multiple retrospective studies have demonstrated an overall survival difference of definitive radiotherapy in combination with ADT when compared to adjuvant ADT alone in patients with node-positive prostate cancer after radical prostatectomy (Table 3) [22, 23, 24•, 25, 26].
Zagars et al. demonstrated that the 10-year overall survival for patients treated with combination therapy was 67% versus 46% for those treated with just ADT. In addition, this group also showed the 10-year recurrence-free survival for the combination therapy was approximately 80% when compared to 25% for the ADT group [23]. Guo et al. also showed an improved OS benefit (HR: 0.74; p = 0.008) and dramatic improvement in CSS (HR: 0.40; p = 0.000) in pN1 prostate cancer patients treated with adjuvant RT in combination with ADT. These authors acknowledged the heterogeneity of this subset of patients as the patient disease burden was a strong predictor of the treatment success [24•].
Notwithstanding, it is important to highlight that the data described above was collected retrospectively. Prospective data and more importantly randomized trials are lacking on this subject of aRT and ADT in men with pN1 disease. Consequently, the approach to pN1 prostate cancer using aRT and ADT varies among centers and providers. As aforementioned, a carefully designed clinical trial that includes the control group of observation followed by salvage radiotherapy with ADT is clearly needed to assess the benefit of aRT combined with ADT. Indeed, as recently demonstrated with the use radiation in men with high-risk features following RP, radiating all men with pN1 disease without level 1 evidence may result in significant overtreatment.
Salvage Radiation Therapy
In addition to the adjuvant treatments, salvage radiation therapy (sRT) is another option that must be included in discussing outcomes of pN1 prostate cancer patients. The outcome of this treatment modality has mainly been studied in comparison to adjuvant radiation therapy. Tilki et al. reported that patients with pN1 prostate cancer that were treated with adjuvant radiation after RP had better biochemical recurrence-free (BCR-free) and metastasis-free survival (MFS) rates than patients treated with no treatment or sRT. In this study, the 4-year MFS was 82.5% in the no treatment/sRT group vs 91.8% in the adjuvant radiation therapy group [27]. Next, Tikil et al. observed that patients treated with aRT vs early sRT had lower all-cause mortality (ACM), and this reduction in ACM increased with each subsequent positive lymph node. At a median follow-up of 7 years, they found that men with four or more positive lymph nodes had a statistically significant reduction in ACM when compared to sRT [28••]. This study highlights the potential importance of considering the number of positive lymph nodes in the pathological specimen when deciding between aRT and sRT.
Current Clinical Trials in pN1 Disease
A clinical trial currently investigating aRT in pN1 prostate cancer patients is NCT04134260 (“Testing the Addition of the Drug Apalutamide to the Usual Hormone Therapy and Radiation Therapy After Surgery for Prostate Cancer”). This trial compares the therapeutic effect of the addition of apalutamide, an androgen receptor inhibitor, to ADT and radiation therapy versus adjuvant ADT + aRT. One criticism of this trial is that observation alone (followed by salvage radiation on failure) is not evaluated. This treatment modality is frequently used in the care of pN1 prostate cancer patients. Given that observation has not been studied rigorously in a prospective nature, the standard of care for pN1 prostate cancer patients will continue to be complex with multiple options. We propose that a study is needed to evaluate the effectiveness of observation followed by salvage therapy upon disease progression. In such a study, patients with pN1 disease would receive adjuvant ADT plus aRT versus observation followed by sRT plus ADT upon disease progression. Our group is in the process of designing such a trial.
Conclusion
The detection of nodal metastasis at the time of radical prostatectomy is not a rare event. While there are a few existing and ongoing studies comparing different treatment modalities in this subset of prostate cancer patients, there is no uniformly accepted standard of treatment for these patients. Consequently, the treatment regimens for this group remain highly variable across institutions and surgeons. Importantly, there is no solid level-one evidence supporting the role of adjuvant radiotherapy combined with ADT. A randomized trial on adjuvant radiotherapy combined with ADT in which the control group is observation is needed to start systematically establishing the standard of care in men with pN1 prostate cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA: a cancer journal for clinicians. 2022;72(1):7–33.
Carter HB, Albertsen Peter C, Barry Michael J, et al. Early detection of prostate cancer: AUA guideline. J Urol. 2013;190:419–26.
Eastham James A, Auffenberg Gregory B, Barocas Daniel A, et al. Clinically localized prostate cancer: AUA/ASTRO guideline, Part I: introduction, risk assessment, staging, and risk-based management. J Urol. 2022;208:10–8.
Abdollah F, Suardi N, Gallina A, Bianchi M, Tutolo M, Passoni N, Fossati N, Sun M, dell’Oglio P, Salonia A, Karakiewicz PI, Rigatti P, Montorsi F, Briganti A. Extended pelvic lymph node dissection in prostate cancer: a 20-year audit in a single center. Ann Oncol. 2013;24(6):1459–66. https://doi.org/10.1093/annonc/mdt120.
Bernstein Adrien N, Shoag Jonathan E, Golan R, et al. Contemporary incidence and outcomes of prostate cancer lymph node metastases. J Urol. 2018;199:1510–7.
Marra G, Valerio M, Heidegger I, Tsaur I, Mathieu R, Ceci F, Ploussard G, van den Bergh RCN, Kretschmer A, Thibault C, Ost P, Tilki D, Kasivisvanathan V, Moschini M, Sanchez-Salas R, Gontero P, Karnes RJ, Montorsi F, Gandaglia G; EAU-YAU prostate cancer working party. Management of patients with node-positive prostate cancer at radical prostatectomy and pelvic lymph node dissection: a systematic review. Eur Urol Oncol. 2020;3(5):565–581. https://doi.org/10.1016/j.euo.2020.08.005.
National Comprehensive Cancer Network. Prostate Cancer (Version 1.2023). https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed Oct. 20, 2022.
EAU (European Association of Urology) Guidelines. Prostate Cancer. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP_SIOG-Guidelines-on-Prostate-Cancer-2022_2022-04-25-063938_yfos.pdf. Accessed Oct. 20, 2022.
Touijer KA, Karnes RJ, Passoni N, et al. Survival outcomes of men with lymph node-positive prostate cancer after radical prostatectomy: a comparative analysis of different postoperative management strategies. Eur Urol. 2018;73(6):890–6.
Messing EM, Manola J, Sarosdy M, Wilding G, Crawford ED, Trump D. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med. 1999;341(24):1781–8. https://doi.org/10.1056/NEJM199912093412401.
Messing EM, Manola J, Yao J, et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006;7(6):472–9.
Touijer KA, Mazzola CR, Sjoberg DD, Scardino PT, Eastham JA. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol. 2014;65(1):20–5. https://doi.org/10.1016/j.eururo.2013.03.053.
Dorin RP, Lieskovsky G, Fairey AS, Cai J, Daneshmand S. Outcomes after radical prostatectomy for patients with clinical stages T1–T2 prostate cancer with pathologically positive lymph nodes in the prostate-specific antigen era. Urol Oncol. 2013;31(8):1441–7.
Mandel P, Kriegmair MC, Bogdan K, et al. Association between lymph node counts and oncological outcomes in lymph node positive prostate cancer. (2405–4569 (Electronic)).
Palapattu GS, Allaf ME, Trock BJ, Epstein JI, Walsh PC. Prostate specific antigen progression in men with lymph node metastases following radical prostatectomy: results of long-term followup. J Urol. 2004;172(5 Pt 1):1860–4. https://doi.org/10.1097/01.ju.0000139886.25848.4a.
Fleischmann A, Schobinger S, Schumacher M, Thalmann GN, Studer UE. Survival in surgically treated, nodal positive prostate cancer patients is predicted by histopathological characteristics of the primary tumor and its lymph node metastases. Prostate. 2009;69(4):352–62. https://doi.org/10.1002/pros.20889.
Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972;22(4):232–40.
Breul J, Lundström E, Purcea D, et al. Efficacy of testosterone suppression with sustained-release triptorelin in advanced prostate cancer. Adv Ther. 2017;34(2):513–23.
Nguyen PL, Alibhai SM, Basaria S, et al. Adverse effects of androgen deprivation therapy and strategies to mitigate them. Eur Urol. 2015;67(5):825–36.
Wong YN, Freedland S, Egleston B, Hudes G, Schwartz JS, Armstrong K. Role of androgen deprivation therapy for node-positive prostate cancer. J Clin Oncol. 2009;27(1):100–5.
Park S, Kim SC, Kim W, Song C, Ahn H. Impact of adjuvant androgen-deprivation therapy on disease progression in patients with node-positive prostate cancer. Korean J Urol. 2011;52(11):741–5.
Broughman JR, Chen RC. Management of node-positive and oligometastatic prostate cancer. Semin Radiat Oncol. 2017;27:79–86.
Zagars GK, Pollack A, von Eschenbach AC. Addition of radiation therapy to androgen ablation improves outcome for subclinically node-positive prostate cancer. Urology. 2001;58:233–9.
• Guo L, Zhu Z, Zhang X. Adding radiotherapy to androgen deprivation therapy in men with node-positive prostate cancer after radical prostatectomy: a meta-analysis. Medicine. 2020;99(10). This study highlights that the addition of adjuvant radiation therapy to a regimen of adjuvant androgen deprivation therapy may be associated with improved overall survival and cancer specific survival.
Lin CC, Gray PJ, Jemal A, Efstathiou JA. Androgen deprivation with or without radiation therapy for clinically node-positive prostate cancer. JNCI: J Nat Cancer Inst. 2015;107:djv119.
Rusthoven CG, Carlson JA, Waxweiler TV, Raben D, Dewitt PE, Crawford ED, Maroni PD, Kavanagh BD. The impact of definitive local therapy for lymph node-positive prostate cancer: a population-based study. Int J Radiat Oncol Biol Phys. 2014;88(5):1064–73. https://doi.org/10.1016/j.ijrobp.2014.01.008.
Tilki D, Preisser F, Tennstedt P, Tober P, Mandel P, Schlomm T, Steuber T, Huland H, Schwarz R, Petersen C, Graefen M, Ahyai S. Adjuvant radiation therapy is associated with better oncological outcome compared with salvage radiation therapy in patients with pN1 prostate cancer treated with radical prostatectomy. BJU Int. 2017;119(5):717–23. https://doi.org/10.1111/bju.13679.
•• Tilki D, Chen MH, Wu J, Huland H, Graefen M, D'Amico AV. Adjuvant versus early salvage radiation therapy after radical prostatectomy for pN1 prostate cancer and the risk of death. J Clin Oncol. 2022;40(20):2186–2192. https://doi.org/10.1200/JCO.21.02800. This article compares adjuvant radiation therapy to salvage radiation therapy and reports decreased all cause mortality with the use of adjuvant radiation therapy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hayden, C., Rahman, S., Lokeshwar, S. et al. Management of Pathologic Node-Positive Prostate Cancer following Radical Prostatectomy. Curr Oncol Rep 25, 729–734 (2023). https://doi.org/10.1007/s11912-023-01420-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-023-01420-6