Abstract
Purpose of Review
Clinical decisions for (neo)adjuvant treatment in early breast cancer (eBC) have been based mostly on clinical factors over the last decades. We have reviewed development and validation of such assays in the HR + /HER2 eBC and discuss possible future directions in this field.
Recent Findings
Increasing knowledge about the biology of hormone-sensitive eBC, based on the precise and reproducible multigene expression analysis, has led to a significant change in the treatment pathways and reduction of overtreatment in particular by chemotherapy in HR + /HER2 eBC with up to 3 positive lymph nodes based on results from several retrospective-prospective trials used several genomic assays and in particular prospective trials (TAILORx, RxPonder, MINDACT, and ADAPT used OncotypeDX® and Mammaprint®).
Summary
Precise evaluation of tumor biology together with endocrine responsiveness assessment appears as promising tools for individualized treatment decisions together with clinical factors and menopausal status in early hormone-sensitive/HER2-negative breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hormone receptor positive breast cancer (HR + BC) is a highly heterogeneous disease. Due to substantial technical progress, the development of multigene expression assays (MGA) in early HR + breast cancer has been impelled. New gene expression assays have dramatically improved our understanding of breast cancer biology and enabled a development of novel multigene expression signatures prognostic and, to a degree, predictive for therapy response in early HR + BC. Although all these tools distinguish molecular subtypes in different ways due to various biostatistical approaches and use of different gene panels, none of them is based on a direct identification of gene mutations but on analysis of mRNA, in contrast to metastatic setting, where analyses of mutations in PI3K, ERBB2, BRCA1, BRCA2, PALB2, ESR1, FGFR2, and other genes are rather now ready for prime use in the clinical routine at different extent due to some promising results on response to targeted therapies [1, 2]. Conversely, only analysis of BRCA1 and BRCA2 mutations is of particular interest due to adjuvant olaparib approval in the early high-risk HR + /HER2 − BC [3].
Molecular Subtypes
Based on previous work by Perou et al., HR + /HER2 − BC has been subdivided into four major molecular subtypes by unsupervised clustering analysis, namely the most frequent luminal-A and luminal-B, HER2-enriched and very rare cases of basal-like subtype [4•, 5•]. Subsequent studies have shown substantially different mutational profile associated with these subtypes [6]. Several studies reported an enrichment of TP53 mutations and its association with aromatase inhibitor resistance, and less frequent mutations in PI3K and MAP3K1 genes in luminal-B vs. luminal-A tumors [6, 7].
Importantly, although mutational landscape of estrogen receptor positive (ER +) BC appears as relatively homogeneous in the primary disease, it becomes substantially more complex in the metastatic setting. In particular, an increased number of mutations in TP53, ERBBB2, and other genes has been observed after exposure to endocrine therapy (ET) [8].
In 2009, Parker et al. have proposed an use of standardized approach based on expression of 50 selected genes [9•]. This so-called PAM50 signature has been shown to be highly prognostic in several retrospective analyses in observational studies and clinical trials in early setting. The risk of relapse is relatively low in low-proliferating luminal-A disease, followed by luminal-B and HER2-enriched and basal-like subtypes in patients treated by ET alone [10,11,12]. Importantly, although the use of Ki-67 at different cut-off levels and/or progesterone receptor (PR) expression was significantly associated with molecular subtypes, the sensitivity and specificity were moderate [13, 14]. Furthermore, ET with tamoxifen seems to have a stronger efficacy in luminal-A cases defined by PAM50 compared to HR + disease identified by immunohistochemistry [10, 12]. Although this review focuses on the ER + /HER2 − disease, a substantial proportion (50–70%) of highly heterogeneous ER + /HER2 + tumors are allocated to luminal-A or luminal-B subtypes by PAM50 [15]. Remarkably, patients with luminal-A subtype have also the best prognosis following different chemotherapy/anti-HER2-based approaches in HR + /HER2 + disease despite a very low pCR rate [16]. Therefore, the need for such intensified approaches in luminal-A subtype appears at least questionable. However, until now this issue has never been prospectively addressed to challenge the current therapeutic algorithms. As stated above, PAM50 signatures seem to provide a similar prognostic value in the first-line setting in metastatic HR + /HER2 − as in early BC (eBC) [17, 18]. Moreover, the use of PAM50 to identify HER2-enriched subtype in HR + /HER2 − BC defined by immunohistochemistry appears to be predictive, for example for use of anti-HER2 drugs [17].
Multigene Prognostic Tests
In the last decades, several multigenic prognostic tests have been developed based on the same prognostically important pathways as those incorporated into the molecular subtypes mentioned above but using different statistic approaches. Most of these tests were developed with prognostic purposes in mind, including the Prosigna®/risk of recurrence (ROR), Endopredict®/Clin (EP/EPclin), MammaPrint®, Breast Cancer Index (BCI)®, and Genomic Grade®, while the OncotypeDX®/Recurrence Score was designed to focus on predictive power (chemotherapy vs. no chemotherapy in HR + disease). ROR and EP incorporate classical markers, including tumor size and nodal status which are considered independent prognostic markers, with the remaining tests evaluating biological information only. Despite these differences, most studies have shown a higher prognostic power of genomic signatures compared to immunohistochemical markers like proliferation index based on Ki-67 levels [19, 20]. Some [21], but not all studies [20, 22], have shown that prognostic impact of ER, PR, Ki-67, and HER2 expression analyzed within prognostic algorithms (e.g., IHC4) is similar to genomic signatures; however, therapeutical consequences remain unclear.
Moreover, these signatures differ in their prognostic power for early vs. late relapses, in particular regarding ER-responsive cluster (which is more important for late relapses) and proliferation cluster (which is critical for overall prognostic power and for early relapses in particular) [23, 24]. Given these differences, there is a significant re-classification of risk categories if several tests are applied on the same samples, despite generally similar prognostic information. Bartlett et al. have reported up to 60% discordance rate in risk classification when OncotypeDX, MammaPrint, IHC4, and Prosigna (PAM50) were used in the Optima trial [25].
Lack of incorporation of specific histological subtypes, e.g., invasive lobular, mucinous, medullary, and other carcinomas, is a further limitation of these signatures. Some [26], but not all [27,28,29], retrospective studies have shown a limited prognostic impact of genomic signatures, and unclear predictive effect regarding survival impact from the chemotherapy addition to the ET impact e.g., in the invasive lobular carcinoma. Moreover, it remains unclear whether MGA have an additional prognostic effect in favorable histological subtypes as for example in tubular carcinoma [30, 31]. For these reasons, the use of MGA needs further prospective evaluation in patients with rare subtypes and in with male BC despite some promising data [32].
OncotypeDX®/Recurrence Score (Exact Science, Madison, USA) is the preferred MGA by the current NCCN breast cancer guidelines (2.2022) in all node-negative patients and in postmenopausal node-positive eBC, which is in line with the current ASCO guidelines [33]. This MGA has been released in 2004 [34•] and it provides a continuous recurrence score (RS) based on the expression of 21 genes. OncotypeDX is prognostic for distant relapse in the first 5–10 years in node-negative and node-positive disease, as shown by several prospective and retrospective trials [20, 35, 36•, 37•, 38]. Furthermore, it has some prognostic utility for late relapses [39]. This test was developed with focus on prediction of benefit from an adjuvant chemotherapy (six cycles of cyclophosphamide, methotrexate, fluorouracil, CMF) in addition to standard ET with tamoxifen using samples from the NSABP B-20 trial in patients with node-negative disease [36•, 40•]. Furthermore, the test was validated in node-positive postmenopausal patients in the SWOG 8814 trial [36•] which investigated six cycles of cyclophosphamide, doxorubicin, and fluorouracil in addition to tamoxifen. Both studies demonstrated most benefit from chemotherapy specifically in patients with a higher RS values (> 25–30), although this effect was more pronounced in younger patients in the NSABP B-20 trial [41]. Interestingly, a worse prognosis, compared to RS 0–11, but still no effect from the chemotherapy, was observed in tumors with an intermediate RS (11–25). This predictive effect was re-evaluated and confirmed in part in large prospective trials, in node-negative disease (Trial Assigning Individualized Options for Treatment, TailorX) and in patients with 1–3 positive lymph nodes (SWOG S1007/RxPonder).
The TailorX trial (NCT00310180) was performed in 10,273 mostly clinically low-risk patients with pT1-2, pN0 HR + /HER2 − eBC with RS 11–25 (n = 6711, 65%). Patients were randomized to chemotherapy followed by ET vs. ET alone mostly including tamoxifen in younger women, approximately 80%; only a few patients received ovarian suppression therapy with/without aromatase inhibitors, even in case of high clinical risk [37•]. All patients with RS 0–10 were treated with ET resulting in excellent survival [42•]; patients with RS > 25 were allocated to chemotherapy followed by ET. After 9 years of median follow-up, no significant outcome difference between both groups was observed, irrespective of clinical risk. However, a significant benefit regarding invasive disease-free survival (iDFS) and distant disease-free survival (dDFS) from a chemotherapy was seen in younger (premenopausal) patients with RS 16–25. In this group 5-year iDFS rates of 92% (RS 16–20) and 86.3% (RS 21–25) and 5-year dDFS rates of 98% and 93.2% were observed after ET, compared to 5-year iDFS 92.1% and 94.7% and 5-year dDFS of 98.1 and 96.4% after chemoendocrine therapy, respectively. In detail, 9-year iDFS benefit ranged between 9 and 6% and dDFS benefit was 1.6% and 6.4% in the RS 16–20 and RS 21–25 subgroups, respectively. In particular, improved dDFS was addressed to those with a higher clinical risk and 16–20 and/or aged 45–50 years within the critical subgroup by exploratory analysis [43•]. Collectively, these data indicate that 85% of women aged > 50 years and about 40–50% women aged ≤ 50 years with T1-2, node-negative HR + /HER2 − eBC appear not to be candidates for adjuvant chemotherapy.
Similar results were observed in the RxPonder trial (NCT01272037) [38] in 5083 patients with 1–3 positive lymph nodes and RS 0–25. After 6 years of median follow-up [44], no significant benefit from chemotherapy was observed in postmenopausal women (two-thirds of patients), and 5-year iDFS of approximately 91.3 (chemoendocrine treatment) and 91.9% (endocrine group) was observed in both groups, irrespective of RS which was clearly prognostic. In contrast, premenopausal patients (mostly treated with tamoxifen without ovarian suppression) had a modest, but significant benefit from chemotherapy use (2–3% regarding 5-year dDFS and 4–6% regarding 5-year iDFS) (5-year iDFS) was improved from 89 to 93.9%. This absolute benefit appeared to be lower in RS 0–13 and higher in the RS 14–25 group. One can speculate that ovarian suppression induced by (neo)adjuvant chemotherapy may be a reason for these results in younger patients. Unfortunately, only 15% of premenopausal patients received ovarian suppression therapy in the RxPonder trial despite a higher relapse risk. A recent update from this trial confirms a positive impact of period cessation on survival in both study arms, similarly to other trials in HR + /HER2 − disease [44]. In the explorative retrospective analysis, only patients with lobular histology and those aged > 50 years in the premenopausal group with RS < 26 derived no significant benefit from the CT addition to ET.
Other trials showed a similar (or even a higher) efficacy of ovarian suppression with or without tamoxifen vs. older chemotherapy regimens like CMF in patients with HR-positive disease [45, 46]. However, a lack of antihormonal treatment in the chemotherapy arms in some of these studies as well as inclusion of HER2-positive tumors prevents drawing definitive conclusions from these data sets. Moreover, recently published long-term results from the SOFT/TEXT trials underline the importance of addition of ovarian suppression to tamoxifen or even combination of aromatase inhibitors with ovarian suppression in patients with a higher relapse risk (defined by chemotherapy use in this analysis) [47]. Further studies also confirmed an importance of ovarian suppression in patients with a high clinical risk [48]. The ABCSG-12 trial showed an excellent 8-year survival at 97% in premenopausal patients with intermediate to high-risk HR + /HER2 − tumors (30% node-positive, only 5% treated with chemotherapy) treated by ET plus ovarian suppression in combination with zoledronic acid [49].
The ADAPT trial (NCT01779206) conducted by the West German Study Group (WSG) has applied another approach by combining OncotypeDX® with early proliferation response to a short course of standard preoperative ET in patients with enhanced clinical risk and HR + /HER2 − eBC. All patients with an intermediate RS of 12–25, 0–3 positive lymph nodes, and a low post-endocrine Ki-67 proliferation index after 2–4 weeks of preoperative ET (≤ 10% by central pathology, defined as endocrine therapy responders) as well as those with pN0-1 with RS 0–11 (n = 2290) were treated by standard ET alone. In contrast, all RS 12–25 patients with a high post-endocrine Ki-67 (endocrine non-responders) were allocated to (neo)adjuvant chemotherapy together with all patients with RS > 25 or a very high clinical risk (e.g., N2-3 disease). An excellent 5-year iDFS at 94% was observed in all patients with RS 0–11 (all treated by ET) compared to 93% in RS 12–25/endocrine responders (including those with premenopausal status) thus reaching non-inferiority threshold between both groups [50]. Of note, iDFS rate in RS 0–11 arm confirmed previous results from the prospective PlanB trial which omitted chemotherapy in patients with pN0-1 clinical high-risk HR + /HER2 − eBC. Importantly, there were no survival differences between RS 0–15, RS 16–20, and RS 21–25 subgroups in younger patients irrespective of nodal status. For example 5-year iDFS of 92% was observed in younger N0 patients with RS 16–25 and ET response treated by ET alone, which is very similar to the reported outcomes in this critical group after chemoendocrine therapy in the TailorX trial [37•] by an indirect cross-trial comparison, which has to be interpreted with caution. Young patients with N0-1 tumors without ET response and RS 12–25 had a significantly worse iDFS of 89.5%, in spite of chemotherapy which was given, in particular driven by node-positive patients. Moreover, the whole group of younger N1 patients treated by ET alone with RS 0–25 (selected by ET response in the RS 12–25 group) had 5-year dDFS of 95%, also very similar to the RxPonder premenopausal cohort. Remarkably, ET response was observed twice more often in postmenopausal vs. premenopausal patients, with almost 80% cases with a low post-endocrine Ki-67 levels among older women with RS 12–25, similarly to other reports [51]. These results could be potentially explained by the use of aromatase inhibitors (few postmenopausal patients treated with tamoxifen) and/or different intrinsic biology between premenopausal and postmenopausal women with a higher endocrine sensitivity in older women due to a higher expression of ER-related genes. Substantial rate of endocrine sensitivity was also observed in the RS > 25 patients [52]. Importantly prognostic impact of ET response was clearly observed in the whole study, irrespective of age/menopausal status, and was driven in particular by cases with baseline Ki-67 > 10%.
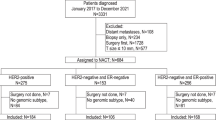
OncotypeDX® has also been shown to be highly predictive for pathological complete response (pCR) after neoadjuvant chemotherapy (NACT) in the high-risk cohort in the ADAPT trial [53]. A total of 864 patients in total were treated with NACT; pCR rate in the RS > 25 compared to RS ≤ 25 group was 16% vs. 8%, in line with results from previous smaller trials. Interestingly, pCR rate was also significantly higher in patients with RS > 25 and in endocrine non-responders (21%) vs. those with post-endocrine Ki-67 levels ≤ 10% (6%). Therefore, evaluation of endocrine sensitivity by Ki-67 measurement after a short course of preoperative ET appears to be a promising factor for patient selection for (neo)adjuvant chemotherapy or ET-based approach particularly in premenopausal women with RS < 26 and/or in future in some postmenopausal and premenopausal women with RS > 26 (currently under investigation in the prospective WSG-ADAPTCycle trial (NCT04055493)).
Higher sensitivity of tumors with a lower RS (and more favorable, hormone-sensitive biology) has also been confirmed by the adjuvant NSABP B-14 trial investigating adjuvant tamoxifen vs. placebo. Here, patients with a lower RS derived most benefit from tamoxifen, although interaction test had a borderline significance. ESR1 expression by reverse transcription polymerase chain reaction (RT-PCR) was highly associated with an absolute gain in outcome from the adjuvant tamoxifen [54]. Moreover, this effect has been confirmed by the neoadjuvant Trans-NEOS trial showing a higher clinical response after 6 months of neoadjuvant letrozol in postmenopausal patients with RS ≤ 18 vs. RS > 30 [55].
Expression levels of estrogen-related genes may be crucial not only for benefit assessment from ET, but also for late relapse risk. In pooled analysis of the NSAB B-14 and B-28 trials, RS has been shown to be significantly associated with late relapse risk, but only in case of a high expression of estrogen receptors [39]. OncotypeDX® is available as a centralized test, performed only in a single lab in the clinical trial setting; however, Lee et al. published a set of 179 genes assessed by next-generation sequencing and which was associated with a strong prognostic impact and a high concordance with RS testing in HR + /HER2 − eBC [56].
Measurement of endocrine-related but not proliferation-related pathway (SET 2,3 signature) appears critical for assessment of both prognosis and even benefit from chemotherapy dose intensification as shown recently at the ASCO 2022 from the retrospective analysis of the CALGB 9744 trial. Further data are also needed for definition of standard methods regarding endocrine sensitivity [57].
The MINDACT trial in 6693 patients (NCT00433589) has examined the 70-gene signature (MammaPrint®, Agendia, NV, continuous score with low and high-risk categories) vs. clinical factors by Adjuvant!Online 8.0 in the context of the adjuvant chemotherapy decision-making by a randomization design [58•, 59•]. This trial has been based on the first promising results obtained with the 70-gene signature indicating very low recurrence rates in untreated patients [60]. Enrolled were patients with pN0-1, mostly HR + disease (n = 1497 with HR + /HER2 − eBC) and discrepant risk assessment results, i.e., a high clinical risk (approximate definition in node-negative BC as G1 tumors and tumor size > 3 cm, G2 and tumor size > 2 cm, and G3 disease and tumor size > 1 cm or node-positive disease) and a low genomic risk or vice versa. Patients were randomized to receive adjuvant chemotherapy or no chemotherapy (mostly ET alone in around 90% of patients with HR + /HER2 − disease). A total of 75% of patients with luminal BC were determined as genomically low risk. After 9 years of follow-up, an excellent 5-year distant metastasis free survival (DMFS) at 95.1% (within a non-inferiority boundary) in clinically high/genomically low-risk group is treated by ET alone. However, a positive effect on 9-year DMFS of 5% was observed which was attributed to chemotherapy administration in patients aged ≤ 50 years in contrast to 0.2% in older women [59•]. Unfortunately, also in this trial a very low rate of ovarian suppression was used in young patients and therefore, it remains unclear whether this benefit was due to chemotherapy-induced ovarian suppression. Patients with an ultra low MammaPrint® result (18% of luminal cases) had an excellent distant metastasis free interval (DMFI) rate of 97% with only 14% of patients treated with adjuvant chemotherapy and further 16% patients without any systemic treatment. Only a positive lymph node status was significantly associated with worse DMFI in this sub-collective [61]. Moreover, an additional 80-gene tool, Bluepint, provides molecular subtyping (luminal, basal, HER2) and can be used to supplement prognostic multigene index by MammaPrint®. Blueprint has been shown to re-classify about 50% of luminal-B cancers to the genomically luminal-A group with similar survival outcomes in the MINDACT trial [62]. Both tests are available as a decentralized NGS-based testing [63].
MammaPrint® has also shown a predictive impact on NACT response with a significantly higher pCR rate in patients with genomic high-risk compared to those with a low-risk disease [64]. Moreover, the highest pCR rate was observed in patients with HR + /HER2 − disease who were classified as basal by Blueprint [65].
MammaPrint® has also been evaluated in the NSABP-42 trial as a predictor for efficacy of letrozole therapy prolonged beyond 5 years in postmenopausal women [66]. Patients with low risk by MammaPrint derived more benefit from a longer ET than high-risk patients and, interestingly, this extended treatment was not associated with reduced risk of late relapse.
Data from all randomized trials clearly indicate an additional prognostic impact of clinical markers (nodal status, tumor size, and others) supplementing genomic markers, what may be important for assessment of absolute relapse risk and predicting benefit from different treatments [67]. Nevertheless, there is a lack of predictive impact regarding chemotherapy use [68] particularly in postmenopausal patients.
Breast Cancer Index® (BCI, Biotheranostics) classifies tumors into low-risk and high-risk categories by combining proliferation (Molecular Grade Index, MGI) and estrogen-related genes (HOXB13/IL17BR ratio, H/I), and it is highly predictive for early-risk and late-risk relapse in different cohorts. The use of BCI as a predictive tool for patient selection for a longer ET has been initially demonstrated in smaller retrospective studies, namely MA-17 (letrozole following tamoxifen) [69] and aTTom (10 vs. 5 years of tamoxifen) [70] in node-positive disease. Unfortunately, this effect was less conclusive in two larger validation cohorts. For instance, although BCI was associated with a significant benefit from a longer aromatase inhibitor treatment (10 years vs. 7.5 years of overall duration) in the IDEAL trial [71], this effect could not have been confirmed by the abovementioned NSABP B-42 trial investigating longer (years 5–10) therapy with letrozole after previous aromatase inhibitors or tamoxifen in postmenopausal women [72]. Nevertheless, the use of BCI for treatment decisions regarding the use of a longer ET is recommended by the current ASCO guidelines [33].
Prosigna® and EPclin® are another two genomic signatures recommended by NCCN guidelines (version 2.2022) as prognostic assays that incorporate clinical markers into the prognostic tool. Prosigna® (Veracyte, CA), based on the expression of 50 genes (plus eight reference genes, PAM50), provides a continuous risk of recurrence score (ROR, ranging from 0 to 100) adjusted for proliferation and tumor size. ROR is calculated with different cutoffs for node-negative and node-positive HR + /HER2 − disease together with molecular PAM50 subtype (luminal-A/-B, HER2-enriched, basal-like). This test has been shown to be strongly prognostic in different retrospective-prospective studies in postmenopausal women with 0–3 positive lymph nodes [11, 73], as well as in the early and late relapse settings [74]. There are also some data in premenopausal women showing a strong prognostic impact in untreated and in chemotherapy-treated patients, as well as a higher efficacy of chemotherapy in basal-like and luminal-B subtypes [75]. Currently ongoing OPTIMA trial (ISRCTN42400492), which at the time of writing this manuscript has randomized 3180 out of planned 5000 patients, investigates Prosigna regarding its clinical impact (CT followed by ET vs. Prosigna®-directed treatment).
Endopredict (Myriad Genetics, UT) is based on the expression of eight genes (plus three reference genes) classifying tumors into low-risk and high-risk categories and combines a continuous genomic score with tumor size and nodal status (EPclin). This combined score has shown a very strong prognostic effect in different postmenopausal retrospective-prospective cohorts, untreated and treated with chemotherapy, and for both early and late relapse [19, 24]. Although no prospective trials addressing the chemotherapy benefit are available so far, Sestak et al. showed a stronger chemotherapy effect in the EPclin high-risk but not in the EPclin low-risk cohort by an indirect comparison of outcomes from the TransATAC, ABCSG-6, and ABCSG-8 trials (treated with ET only) vs. GEICAM 2003–02/9906 trial (treated with chemotherapy + ET) in postmenopausal patients (no comparison was possible in premenopausal women) [76]. In postmenopausal patients with 1–3 positive lymph nodes, a higher percentage of high-risk patients was identified by the genomic signature in the EPclin than in OncotypeDx® and MammaPrint® tools due to inclusion of nodal status into the EPclin which could be taken into account if adopted in the clinical routine.
There are only a few studies comparing prognostic impact of different genomic assays. The largest retrospective study, TransATAC, was performed by Sestak et al. in the postmenopausal, ET only treated cohort with 0–3 positive lymph nodes. In that study, ROR, EPclin, and BCI provided an additional prognostic information to clinical markers, immunocytochemistry score (IHC4: ER, PR, HER2, Ki-67), and RS (particularly in node-negative patients) [77]. However, clinical impact of these findings appears unclear due to a missing prospective data on chemotherapy use in case of high-risk patients identified by these assays.
Current ASCO guidelines [33] recommend the use of all five genomic signatures for clinical use in postmenopausal patients with ER + /HER2 − breast cancer and 0–3 positive lymph nodes, as well as Oncotype DX for use in premenopausal node-negative breast cancer. However, the use of these assays in premenopausal patients with 1–3 positive lymph nodes is not recommended due to inconclusive results from the prospective trials. A prospective trial comparing chemotherapy vs. ovarian suppression in combination with aromatase inhibitors is currently planned by the Southwest Oncology Group in patients with premenopausal node-negative disease with RS 16–25 and in node-positive women with RS 0–25. West German Study Group trial ADAPTcycle (NCT04055493) is currently investigating aromatase inhibitors in combination with ribociclib vs. chemotherapy in a similar group of patients, but with recommendation to focus patient recruitment on endocrine non-responders and to treat all endocrine responders (with low post-endocrine Ki-67 ≤ 10% or low baseline proliferation in combination with high expression of hormone receptors in patients without preoperative endocrine therapy) with 0–3 positive lymph nodes and RS 0–25 by endocrine therapy alone (in combination with ovarian suppression if high clinical risk). This trial additionally enrolls patients with unclear chemotherapy benefit, namely those with N2-3 status and favorable biology or endocrine responders with N0-1 and RS > 25.
Currently presented negative results on lack of positive predictive effect of high Genomic Grade Index regarding chemotherapy survival impact in a phase III Unicancer ASTER 70 s trial (NCT00156405) in older patients with HR + /HER2 − [78], despite its strong prognostic impact [79], underline an urgent need for prospective well-powered trials addressing optimal use of genomic signatures.
Furthermore, other ongoing prospective trials focus on possible de-escalation of radiotherapy in patients with low genomic risk, like DEBRA trial (NCT04852887), which randomizes patients 50–70 years old, with node-negative T1 HR + /HER2 − disease and RS < 18 to radiotherapy vs. not after breast conserving therapy, due to low local relapse rates observed in low genomic risk group by several trials [80]. Similar trials are ongoing for low risk by Prosigna assay. Their results have to be compared to the currently resented very low local relapse rates in endocrine-treated patients with stage I HR + /HER2, luminal-A by IHC (ER ≥ 1%, PR > 20% KI-67 ≤ 13, 25%) disease and > 55 years old and omission of radiotherapy [31].
Further prospective trials may also address an interesting question of omission or reduction of ET duration in node-negative patients with very low genomic risk.
Conclusion
The use of validated genomic assays significantly changed treatment landscape in early HR + /HER2 − BC, particularly in postmenopausal patients with 0–3 positive lymph nodes, and led to a considerable decrease in chemotherapy use without a negative impact on survival. The use of these tests, especially in combination with assessment of endocrine response, clinical-pathological factors, and histology, seems to be very promising for guiding adjuvant treatment—also in premenopausal women or in patients with moderately increased genomic risk (Fig. 1). Future trials could address the impact of somatic and/or germline genomic aberrations, which can be measured beside or instead of commercially available genomic signatures (capturing phenotype only). Such research could lead to a more personalized treatment in early ER + /HER2 − disease by providing a precise biological information based on genomic assays and/or immunohistochemical markers. Currently, only germline BRCA1/2 mutation in patients with a very high clinical risk appears to be clinically relevant due to availability of olaparib as a treatment option [3]. However, mutations within TP53 gene, highly associated with ET-resistance and a high genomic risk [81], and ERBB2 mutation, associated with promising response rates after anti HER2-treatment in the metastatic setting [82, 83], may be able to refine treatment options in clinically challenging group of patients with a high genomic risk and poor prognosis despite chemotherapy use. Furthermore, prognostic and predictive impact of genomic signatures may be re-evaluated in the context of novel prognostic markers like circulating tumor DNA, which has been currently shown to be strongly associated with late relapse risk in HR + /HER2 − [84] and led to significant reduction of chemotherapy use with similar survival results in other tumor types [85].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
André F, Gonçalves A, Filleron T, et al. Abstract GS1–10: Clinical utility of molecular tumor profiling: results from the randomized trial SAFIR02-BREAST. Cancer Res. 2022;82:GS1-10-GS11-10.
André F, Ciruelos E, Rubovszky G, et al. Alpelisib for PIK3CA-mutated, hormone receptor–positive advanced breast cancer. N Engl J Med. 2019;380:1929–40.
Tutt ANJ, Garber JE, Kaufman B, et al. Adjuvant olaparib for patients with BRCA1- or BRCA2-mutated breast cancer. N Engl J Med. 2021;384:2394–405.
• Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52. Both papers provide basis for understanding of molecular heterogeneity of breast cancer
• Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci. 2001;98:10869–74. Both papers provide basis for understanding of molecular heterogeneity of breast cancer
Koboldt DC, Fulton RS, McLellan MD, et al. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70.
Ellis MJ, Ding L, Shen D, et al. Whole-genome analysis informs breast cancer response to aromatase inhibition. Nature. 2012;486:353–60.
Razavi P, Chang MT, Xu G, et al. The genomic landscape of endocrine-resistant advanced breast cancers. Cancer Cell. 2018;34:427-438.e426.
• Parker JS, Mullins M, Cheang MCU, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009;27:1160–7. This study creates a link between molecular subtypes, discovered by clustering methods and clinically applicable PAM50-signature, based on gene expression analysis on paraffine-embeded fixed tissue
Lundgren C, Bendahl P-O, Church SE, et al. PAM50 subtyping and ROR score add long-term prognostic information in premenopausal breast cancer patients. npj Breast Cancer. 2022;8:61.
Gnant M, Filipits M, Greil R, et al. Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 Risk of Recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol. 2014;25:339–45.
Nielsen TO, Parker JS, Leung S, et al. A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor–positive breast cancer. Clin Cancer Res. 2010;16:5222–32.
Prat A, Cheang MCU, Martín M, et al. Prognostic significance of progesterone receptor–positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31:203–9.
Cheang MCU, Chia SK, Voduc D, et al. Ki67 Index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
Prat A, Carey LA, Adamo B et al. Molecular features and survival outcomes of the intrinsic subtypes within HER2-positive breast cancer. JNCI: J Natl Cancer Inst. 2014;106:dju152.
Harbeck N, Nitz U, Christgen M, et al. LBA13 Predictive impact of biomarkers on pCR and survival after de-escalated neoadjuvant T-DM1 with or without endocrine therapy (ET) vs. trastuzumab+ET in HER2+/HR+ early breast cancer: WSG ADAPT TP trial. Ann Oncol. 2021;32:S1285.
Prat A, Cheang MU, Galván P, et al. PRognostic value of intrinsic subtypes in hormone receptor–positive metastatic breast cancer treated with letrozole with or without lapatinib. JAMA Oncol. 2016;2:1287–94.
Prat A, Chaudhury A, Solovieff N, et al. Correlative biomarker analysis of intrinsic subtypes and efficacy across the MONALEESA phase III studies. J Clin Oncol. 2021;39:1458–67.
Filipits M, Rudas M, Jakesz R, et al. A new molecular predictor of distant recurrence in ER-positive, HER2-negative breast cancer adds independent information to conventional clinical risk factors. Clin Cancer Res. 2011;17:6012–20.
Nitz U, Gluz O, Christgen M, et al. Reducing chemotherapy use in clinically high-risk, genomically low-risk pN0 and pN1 early breast cancer patients: five-year data from the prospective, randomised phase 3 West German Study Group (WSG) PlanB trial. Breast Cancer Res Treat. 2017;165:573–83.
Cuzick J, Dowsett M, Pineda S, et al. Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the genomic health recurrence score in early breast cancer. J Clin Oncol. 2011;29:4273–8.
Gluz O, Liedtke C, Huober J, et al. Comparison of prognostic and predictive impact of genomic or central grade and immunohistochemical subtypes or IHC4 in HR+/HER2- early breast cancer: WSG-AGO EC-Doc Trial. Ann Oncol. 2016;27:1035–40.
Dowsett M, Sestak I, Buus R, et al. Estrogen receptor expression in 21-gene recurrence score predicts increased late recurrence for estrogen-positive/HER2-negative breast cancer. Clin Cancer Res. 2015;21:2763–70.
Dubsky P, Brase JC, Jakesz R, et al. The EndoPredict score provides prognostic information on late distant metastases in ER+/HER2- breast cancer patients. Br J Cancer. 2013;109:2959–64.
Bartlett JMS, Bayani J, Marshall A et al. Comparing breast cancer multiparameter tests in the OPTIMA prelim trial: no test is more equal than the others. J Natl Cancer Inst. 2016;108:djw050.
Christgen M, Gluz O, Harbeck N, et al. Differential impact of prognostic parameters in hormone receptor–positive lobular breast cancer. Cancer. 2020;126:4847–58.
Weiser R, Polychronopoulou E, Hatch SS, et al. Adjuvant chemotherapy in patients with invasive lobular carcinoma and use of the 21-gene recurrence score: a National Cancer Database analysis. Cancer. 2022;128:1738–47.
Makower D, Qin J, Lin J, et al. The 21-gene recurrence score in early non-ductal breast cancer: a National Cancer Database analysis. npj Breast Cancer. 2022;8:4.
Nunes R, Sella T, Treuner K, et al. Prognostic utility of Breast Cancer Index to stratify distant recurrence risk in invasive lobular carcinoma. Clin Cancer Res. 2021;27:5688–96.
Wang J, He Z-Y, Dong Y et al. The distribution and outcomes of the 21-gene recurrence score in T1-T2N0 estrogen receptor-positive breast cancer with different histologic subtypes. Front Genet. 2018;9:638.
Turashvili G, Brogi E, Morrow M, et al. The 21-gene recurrence score in special histologic subtypes of breast cancer with favorable prognosis. Breast Cancer Res Treat. 2017;165:65–76.
Wang F, Reid S, Zheng W, et al. Sex disparity observed for oncotype DX breast recurrence score in predicting mortality among patients with early stage ER-positive breast cancer. Clin Cancer Res: Off J Am Assoc Cancer Res. 2020;26:101–9.
Andre F, Ismaila N, Allison KH, et al. Biomarkers for adjuvant endocrine and chemotherapy in early-stage breast cancer: ASCO guideline update. J Clin Oncol. 2022;40:1816–37.
• Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26. This study was of particular importance due to strong prognostic significance of OncotypeDX in node-negative hormone-sensitive BC, which was shown retrospectively on tumor tissue from a prospective trial
Dowsett M, Cuzick J, Wale C, et al. Prediction of risk of distant recurrence using the 21-gene recurrence score in node-negative and node-positive postmenopausal patients with breast cancer treated with anastrozole or tamoxifen: a TransATAC study. J Clin Oncol. 2010;28:1829–34.
• Albain KS, Barlow WE, Shak S, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11:55. This manuscript has confirmed prognostic and predictive impact of Oncotype DX regarding chemotherapy use in postmenopausal node-positive breast cancer
• Sparano JA, Gray RJ, Makower DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379:111–21. This large study confirmed finding from retrospective analysis on lack of chemotherapy benefit in node-negative HR+/HER2- breast cancer and Recurrence Score 11-25 in patients older than 50 years. No chemotherapy benefit was observed in younger patients in Recurrence Score <16-20.
Kalinsky K, Barlow WE, Gralow JR, et al. 21-gene assay to inform chemotherapy benefit in node-positive breast cancer. New Engl J Med. 2021;385:2336–47 This very important study has shown no adjuvant chemoendocrine therapy benefit over endocrine therapy alone in postmenopausal patients with 1-3 positive lymph nodes and Recurrence Score 0-25. Moderate but significant chemotherapy effect was observed in premenopausal patients, if compared with tamoxifen alone in most patients.
Wolmark N, Mamounas EP, Baehner FL, et al. Prognostic impact of the combination of recurrence score and quantitative estrogen receptor expression (ESR1) on predicting late distant recurrence risk in estrogen receptor–positive breast cancer after 5 years of tamoxifen: results from NRG Oncology/National Surgical Adjuvant Breast and Bowel Project B-28 and B-14. J Clin Oncol. 2016;34:2350–8.
• Paik S, Tang G, Steven S, Chungyeul K, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–34. First retrospective analysis, based on the data from a prospective trial, which shows a chemotherapy benefit in the N0 situation, which was addressed only to patients with high Recurrence Score >30.
Geyer CE, Tang G, Mamounas EP, et al. 21-Gene assay as predictor of chemotherapy benefit in HER2-negative breast cancer. npj Breast Cancer. 2018;4:37.
• Sparano JA, Gray RJ, Makower DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373:2005–14. TAILORx study results provide a basis for daily use of OncotypeDX as a most validated test for chemotherapy decisions in early node-negative HR+/HER2- breast cancer, in particular with regard to clinical risk
• Sparano JA, Gray RJ, Ravdin PM, et al. Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N Engl J Med. 2019;380:2395–405. TAILORx study results provide a basis for daily use of OncotypeDX as a most validated test for chemotherapy decisions in early node-negative HR+/HER2- breast cancer, in particular with regard to clinical risk
Kalinsky KM, Barlow WE, Gralow JR, et al. Cancer Research. 2022;82:GS2-07-GS02-07.
Kaufmann M, Jonat W, Blamey R, et al. Survival analyses from the ZEBRA study: goserelin (Zoladex™) versus CMF in premenopausal women with node-positive breast cancer. Eur J Cancer. 2003;39:1711–7.
Schmid P, Untch M, Kossé V, et al. Leuprorelin acetate every-3-months depot versus cyclophosphamide, methotrexate, and fluorouracil as adjuvant treatment in premenopausal patients with node-positive breast cancer: the TABLE study. J Clin Oncol. 2007;25:2509–15.
Regan MM, Francis PA, Pagani O, et al. Absolute improvements in freedom from distant recurrence with adjuvant endocrine therapies for premenopausal women with hormone receptor-positive (HR+) HER2-negative breast cancer (BC): results from TEXT and SOFT. J Clin Oncol. 2018;36:503–503.
Kim H-A, Lee JW, Nam SJ, et al. Adding ovarian suppression to tamoxifen for premenopausal breast cancer: a randomized phase III trial. J Clin Oncol. 2020;38:434–43.
Gnant M, Mlineritsch B, Stoeger H, et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol. 2015;26:313–20.
Nitz UA, Gluz O, Kümmel S et al. Endocrine therapy response and 21-gene expression assay for therapy guidance in HR+/HER2– early breast cancer. J Clin Oncol. 2022;40: 2557–2567.
DeCensi A, Guerrieri-Gonzaga A, Gandini S, et al. Prognostic significance of Ki-67 labeling index after short-term presurgical tamoxifen in women with ER-positive breast cancer. Ann Oncol. 2011;22:582–7.
Gluz O, Nitz U, Christgen M, et al. Prognostic impact of recurrence score, endocrine response and clinical-pathological factors in high-risk luminal breast cancer: results from the WSG-ADAPT HR+/HER2- chemotherapy trial. J Clin Oncol. 2021;39:504–504.
Kuemmel S, Gluz O, Nitz U, et al. Abstract GS4–03: neoadjuvant nab-paclitaxel weekly versus dose-dense paclitaxel followed by dose-dense EC in high risk HR+/HER2- early BC by: Results from the neoadjuvant part of ADAPT HR+/HER2- trial. Cancer Res. 2021;81:GS4-03-GS04-03.
Kim C, Tang G, Pogue-Geile KL, et al. Estrogen receptor (ESR1) mRNA expression and benefit from tamoxifen in the treatment and prevention of estrogen receptor–positive breast cancer. J Clin Oncol. 2011;29:4160–7.
Iwata H, Masuda N, Yamamoto Y, et al. Validation of the 21-gene test as a predictor of clinical response to neoadjuvant hormonal therapy for ER+, HER2-negative breast cancer: the TransNEOS study. Breast Cancer Res Treat. 2019;173:123–33.
Lee H-B, Lee SB, Kim M, et al. Development and validation of a next-generation sequencing–based multigene assay to predict the prognosis of estrogen receptor–positive, HER2-negative breast cancer. Clin Cancer Res. 2020;26:6513–22.
Metzger O, Ballman KV, Campbell J, et al. Measurement of endocrine activity (SET2,3) related to prognosis and prediction of benefit from dose-dense (DD) chemotherapy in estrogen receptor-positive (ER+) cancer: CALGB 9741 (Alliance). J Clin Oncol. 2022;40:505–505.
• Cardoso F, van’t Veer LJ, Bogaerts J, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. New Engl J Med. 2016;375:717–29. Both publications of the MINDACT trial result have a huge clinical importance together with the TailorX, RxPonder, and ADAPT results, in particular in view of different outcomes after chemoendocrine therapy in younger vs. older patients
• Piccart M, van’t Veer LJ, Poncet C, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 2021;22:476–88. Both publications of the MINDACT trial result have a huge clinical importance together with the TailorX, RxPonder, and ADAPT results, in particular in view of different outcomes after chemoendocrine therapy in younger vs. older patients
van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–6.
Lopes Cardozo JMN, Drukker CA, Rutgers EJT, et al. Outcome of patients with an ultralow-risk 70-gene signature in the MINDACT trial. J Clin Oncol. 2022;40:1335–45.
Viale G, de Snoo FA, Slaets L, et al. Immunohistochemical versus molecular (BluePrint and MammaPrint) subtyping of breast carcinoma. Outcome results from the EORTC 10041/BIG 3–04 MINDACT trial. Breast Cancer Res Treat. 2018;167:123–31.
Mittempergher L, Delahaye LJMJ, Witteveen AT, et al. MammaPrint and BluePrint molecular diagnostics using targeted RNA next-generation sequencing technology. J Mol Diagn. 2019;21:808–23.
Whitworth P, Pellicane JV Jr, Baron P, et al. Abstract PD9–01: 5-year outcomes in the NBRST trial: preoperative MammaPrint and BluePrint breast cancer subtype is associated with neoadjuvant treatment response and survival. Cancer Res. 2021;81:PD9-01-PD09-01.
Whitworth P, Beitsch P, Mislowsky A, et al. Chemosensitivity and endocrine sensitivity in clinical luminal breast cancer patients in the prospective Neoadjuvant Breast Registry Symphony Trial (NBRST) predicted by molecular subtyping. Ann Surg Oncol. 2017;24:669–75.
Rastogi P, Bandos H, Lucas PC, et al. Utility of the 70-gene MammaPrint assay for prediction of benefit from extended letrozole therapy (ELT) in the NRG Oncology/NSABP B-42 trial. J Clin Oncol. 2021;39:502–502.
Sparano JA, Crager MR, Tang G, et al. Development and validation of a tool integrating the 21-gene recurrence score and clinical-pathological features to individualize prognosis and prediction of chemotherapy benefit in early breast cancer. J Clin Oncol. 2021;39:557–64.
Tang G, Cuzick J, Costantino JP, et al. Risk of recurrence and chemotherapy benefit for patients with node-negative, estrogen receptor–positive breast cancer: recurrence score alone and integrated with pathologic and clinical factors. J Clin Oncol. 2011;29:4365–72.
Sgroi DC, Carney E, Zarrella E, et al. Prediction of late disease recurrence and extended adjuvant letrozole benefit by the HOXB13/IL17BR biomarker. J Natl Cancer Inst. 2013;105:1036–42.
Bartlett JMS, Sgroi DC, Treuner K, et al. Breast Cancer Index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the Adjuvant Tamoxifen-To Offer More? (aTTom) trial. Ann Oncol : Off J Eur Soc Med Oncol. 2019;30:1776–83.
Noordhoek I, Treuner K, Putter H, et al. Breast Cancer Index predicts extended endocrine benefit to individualize selection of patients with HR+ early-stage breast cancer for 10 years of endocrine therapy. Clin Cancer Res. 2021;27:311–9.
Mamounas EP, Bandos H, Rastogi P, et al. Breast Cancer Index (BCI) and prediction of benefit from extended aromatase inhibitor (AI) therapy (tx) in HR+ breast cancer: NRG oncology/NSABP B-42. J Clin Oncol. 2021;39:501–501.
Lænkholm A-V, Jensen M-B, Eriksen JO, et al. PAM50 risk of recurrence score predicts 10-year distant recurrence in a comprehensive Danish cohort of postmenopausal women allocated to 5 years of endocrine therapy for hormone receptor–positive early breast cancer. J Clin Oncol. 2018;36:735–40.
Sestak I, Cuzick J, Dowsett M, et al. Prediction of late distant recurrence after 5 years of endocrine treatment: a combined analysis of patients from the Austrian Breast and Colorectal Cancer Study group 8 and arimidex, tamoxifen alone or in combination randomized trials using the PAM50 Risk of Recurrence Score. J Clin Oncol. 2015;33:916–22.
Jensen MB, Lænkholm AV, Nielsen TO, et al. The Prosigna gene expression assay and responsiveness to adjuvant cyclophosphamide-based chemotherapy in premenopausal high-risk patients with breast cancer. Breast Cancer Res. 2018;20:79.
Sestak I, Martín M, Dubsky P, et al. Prediction of chemotherapy benefit by EndoPredict in patients with breast cancer who received adjuvant endocrine therapy plus chemotherapy or endocrine therapy alone. Breast Cancer Res Treat. 2019;176:377–86.
Sestak I, Buus R, Cuzick J, et al. Comparison of the performance of 6 prognostic signatures for estrogen receptor–positive breast cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018;4:545–53.
Brain E, Viansone AA, Bourbouloux E, et al. Final results from a phase III randomized clinical trial of adjuvant endocrine therapy ± chemotherapy in women ≥ 70 years old with ER+ HER2- breast cancer and a high genomic grade index: the Unicancer ASTER 70s trial. J Clin Oncol. 2022;40:500–500.
Ignatiadis M, Azim HA Jr, Desmedt C, et al. The genomic grade assay compared with Ki67 to determine risk of distant breast cancer recurrence. JAMA Oncol. 2016;2:217–24.
Mamounas EP, Tang G, Fisher B et al. Association between the 21-gene recurrence score assay and risk of locoregional recurrence in node-negative, estrogen receptor-positive breast cancer: results from NSABP B-14 and NSABP B-20. J Clin Oncol. 2010;28:1677–1683.
Grote I, Bartels S, Kandt L, et al. TP53 mutations are associated with primary endocrine resistance in luminal early breast cancer. Cancer Med. 2021;10:8581–94.
Ma CX, Luo J, Freedman RA, et al. The phase II MutHER study of neratinib alone and in combination with fulvestrant in HER2-mutated, non-amplified metastatic breast cancer. Clin Cancer Res. 2022;28:1258–67.
Jhaveri K, Park H, Waisman J, et al. Abstract GS4–10: Neratinib + fulvestrant + trastuzumab for hormone receptor-positive, HER2-mutant metastatic breast cancer and neratinib + trastuzumab for triple-negative disease: latest updates from the SUMMIT trial. Cancer Res. 2022;82:GS4-10-GS14-10.
Lipsyc-Sharf M, Bruin ECd, Santos K et al. Circulating tumor DNA and late recurrence in high-risk hormone receptor–positive, human epidermal growth factor receptor 2–negative breast cancer. J Clin Oncol. 2022;40:2408–2419.
Tie J, Cohen JD, Lahouel K et al. Circulating tumor DNA analysis guiding adjuvant therapy in stage II colon cancer. New Engl J Med. 2022;386:2261–2272.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
OG received travel support from Roche and personal fees from Celgene, AstraZeneca, Roche, Pfizer, Novartis, Lilly, Pierre Fabre, Nanostring, MSD, Seagen, Gilead, Molecular Health, and Genomic Health/Exact Sciences. MG received travel support from Daiichi-Sankyo and personal fees from AstraZeneca.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gluz, O., Graeser, M. Molecular Profiling in Early ER + Breast Cancer to Aid Systemic Therapy Decisions. Curr Oncol Rep 25, 491–500 (2023). https://doi.org/10.1007/s11912-023-01377-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-023-01377-6