Abstract
Purpose of Review
The field of neuroendocrine oncology has changed much since the time of Oberndorfer first described and coined the term carcinoid. The purpose of this review is to summarize recent findings and highlight clinically relevant updates in the management of NENs, particularly those that are practice changing.
Recent Findings
Neuroendocrine tumors (NETs) have replaced carcinoid tumor, for the most part. The classification of neuroendocrine neoplasms (NENs) improved, and the epidemiological understanding of this disease group also expanded with global collaborations and maturation of large tumor registries. Clarity in the utility of some NET biomarkers continues to be evolving. Knowledge of molecular drivers of tumorigenesis increases, and scientific/technological advancements lead the way to multiple drug approvals for the treatment of advanced NETs.
Summary
The incidence and prevalence of NENs continue to increase, and patients are living longer. Better understanding of molecular drivers and further understanding of the role of immunotherapy in NENs will further elevate the level of care and transform care for all patients with NENs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Siegfried Oberndorfer was credited with the introduction of the term carcinoid in 1907 [1] to describe their “cancer-like” nature, and Andre Gosset and Pierre Masson in 1914 were acknowledged to identify the endocrine nature of these tumors [2, 3]. Neuroendocrine neoplasms (NENs) are a group of epithelial neoplastic proliferation, with heterogenous spectrum ranging from indolent well-differentiated neuroendocrine tumors (NETs) to very aggressive poorly differentiated neuroendocrine carcinomas (NECs), originating from neuroendocrine cells that can exist anywhere in the body. Despite the diversity in tissue origin, all these tumors typically share common morphological and immunophenotypical features, including cellular function, growth pattern, and expression of neuroendocrine markers. More densely distributed in the gastrointestinal tract and bronchopulmonary systems, neuroendocrine cells are uncommon cells that function as part of both the nervous and endocrine systems. Characterized by amine and neuropeptide hormone production with dense vesicles, these neuroendocrine cells are specialized to receive neuronal inputs and consequentially release message peptides into circulation for regulation and modulation of cellular proliferation, growth, and development [4]. The neuroendocrine system includes the endocrine glands (pituitary, parathyroid, adrenal medulla), the endocrine islet tissue embedded within the glandular tissue (of thyroid and pancreas), and scattered cells in the exocrine parenchyma (of digestive and respiratory tracts) [5]. To appreciate the diversity of NEN spectrum, recall that lung carcinoid tumor, paraganglioma/pheochromocytoma, and medullary thyroid carcinoma, like the classically recognized carcinoid tumor of the small bowel, are all neoplasms originating from neuroendocrine cells [6, 7].
NENs are typically divided into indolent neuroendocrine tumors (NETs) and aggressive neuroendocrine carcinomas (NECs). The most common NENs are in the gastrointestinal and respiratory systems. Knowledge of molecular drivers of tumorigenesis increases, and scientific/technological advancements were added to the accuracy of molecular classification and led the way to multiple drug approvals for the treatment of advanced NENs. Once considered without treatment option and rare cancer groups managed with nihilistic approach, NENs are now manage in specialized NENs clinical programs or centers with focused research agendas. In this review, we will highlight the clinically relevant and impactful advancements in the past two decades, including classification, epidemiologic knowledge, and diagnostic and therapeutic options.
Classification
Progress has been made, but the classification of NENs remains complex and obfuscated by frequent debates and revisions. Foundational classification of NEN is based on the World Health Organization (WHO) nomenclature, and guideline development and translation into clinical practice are led by European organizations, particularly the European Neuroendocrine Tumor Society (ENETS). NEN was proposed to replace carcinoid tumor in the early 2000s, with incomplete penetration. Successful and functional transformation of terminology was symbolic in the USA with the current National Comprehensive Cancer Network (NCCN) [8] and North American Neuroendocrine Tumor Society (NANETS) [9], incorporating and recognizing treatment of adrenal NENs under NENs. Carcinoid tumor still defines certain NENs in the bronchopulmonary system, and healthcare providers still use carcinoid tumor when referring to indolent small bowel/intestine NETs. NENs are managed by different disease-focus specialty groups with their own classifications. Bronchopulmonary NENs (lung-NENs or L-NENs), usually managed by thoracic cancer specialists, are categorized as typical carcinoid tumor, atypical carcinoid tumor, small-cell lung carcinoma, and large-cell lung carcinoma [6, 10]. Gastrointestinal system NENs (GI-NENs) include pancreatic NENs (P-NENs) and extra-pancreatic such as small intestine NENs (SI-NENs). These NENs are frequently managed by gastrointestinal cancer specialists; they are categorized by either by embryonic origins of the primary sites (foregut, midgut, and hindgut) [11] or by histologic features [12]. More widely accepted, GI-NENs are classified by the World Health Organization (WHO) 2019 histological categories [12]: NETs grade 1 through grade 3, neuroendocrine carcinoma small-cell type (SCNEC) and large-cell type (LCNEC), mixed neuroendocrine–nonneuroendocrine neoplasm (MiNEN), and poorly differentiated neuroendocrine carcinoma (PDNEC).
Molecular classification, agnostic of primary site of disease, is not yet possible but strides toward better genomically and molecularly understanding, and classification has been made in the past two decades. Growing genomic evidence indicates that NETs and NECs are unrelated neoplasms. Seminal works presented in the past decade demonstrated distinct genomic differences are especially noted in NENs of the pancreas. For aggressive NECs, genetic mutations are noted in tumor protein-53 (TP53), retinoblastoma 1 (RB1), and less commonly in other carcinoma-related genes, such as retrovirus-associated DNA sequences isolated from Kirsten murine sarcoma viruses (KRAS), cyclin-dependent kinase inhibitor 2A (CDKN2A or p16), B cell lymphoma 2 (Bcl-2), and small molecules against decapentaplegic homolog 4 or deleted-in-pancreatic-cancer-4 (SMAD4/DPC4) [13, 14]. Defining mutations in indolent NETs are multiple endocrine type 1 (MEN), death-domain-associated protein (DAXX), and alpha-thalassemia/intellectual disability syndrome X-linked (ATRX) genes, which are completely absent in pancreatic NECs [15•]. Additional discoveries from genomic analysis of sporadic cases of pancreatic NETs (P-NETs) include frequent alteration of the adenine DNA glycosylase activity of 14 human MutY homolog (MUTYH), cell cycle checkpoint kinase 2 (CHEK2), and breast cancer type 2 (BRCA2). Overall, current genetic findings of P-NETs suggest four pathways: (1) DNA damage repair, (2) chromatin remodeling, (3) telomere maintenance, and (4) mechanistic target of rapamycin (mTOR) signaling activation [16]. Genomic comparisons between P-NETs and extra-pancreatic NETs suggest that there are more differences than similarities between them [17]. Achieved by different mechanisms and with different modulation effects, the mTOR pathway and cell cycle dysregulation remain the common features of both small intestine NETs (SI-NETs) and P-NETs [18]. Familial forms of SI-NETs have been recently discovered but segregated with different mutations in inositol polyphosphate multikinase (IPMK), 8-oxyguanine DNA glycosylase (OGG1), and MUTYH [17]. Conflicting reports of genomic changes in SI-NETS further confirm the low frequency of driver mutations and main chromosomal alterations [17, 19], and overall findings suggest the molecular landscape of SI-NETs appears to be characterized more by chromosomal alterations and gene methylation than by mutations. The first integrative analysis of cyclin-dependent kinase inhibitor 1B (CDKN1B) mutational status, copy and number alterations, and methylome analysis in 97 SI-NETs, Karpathakis et al. [20], proposed the existence of three molecular subtypes of SI-NETs: group 1, those characterized by chromosome 18 copy loss including all with CDKN1B mutation; group 2, those without specific mutations; and group 3, those harboring multiple copy gains at chromosome 4, 5, 14, and 20. These three groups display different methylation profiles and associate with different progression-free-survival after resection (not reach, 56 months, and 21 months, respectively) [20], where those SI-NETs with chromosome 14 copy gains being the worse [20, 21].
Epidemiology
NENs are mostly sporadic in origin, but nearly 5% [11] can be associated with hereditary syndromes, such as multiple endocrine neoplasia type 1 and 2A (MEN-1 and MEN-2A) [22, 23], von Hippel–Lindau (VHL) disease [24], tuberous sclerosis type 2 (TSC-2 or Bourneville’s disease) [25], and neurofibromatosis type 1 (NF-1 or Von Recklinghausen’s disease) [26]. The hereditary NENs are characteristically multifocal, appear one to two decades earlier than sporadic NENs, and have different natural history of disease than expected sporadic counterpart [27]. In some circumstances, the risk of metastatic disease is low, and therefore, longer observation can be the preferred approach over early surgical intervention. Genetic screening and counseling for contributing hereditary etiologies should be particularly done in individuals diagnosed with adrenal cortical carcinoma, paraganglioma/pheochromocytoma, gastrinoma or multifocal pancreatic NETs, parathyroid adenoma or primary hyperparathyroidism before age 30, multiple parathyroid adenomas, recurrent primary hyperparathyroidism, and medullary thyroid cancer in the setting or multiglandular involvement with consideration for all patients age 40 or younger with lung, thymic, pancreatic, or gastric NETs [8].
With the uniformed application of the International Classification of Diseases for Oncology (ICD-O) [28] and with maturity of expanded tumor various registries [29•, 30,31,32,33], the classification of NENs is becoming more transparent and universal which in turn produce more accurate and consistent epidemiologic descriptions. Composite literature review to evaluate the global trends of incidence of NETs, Leoncini et al. [34] conclude an increase in the incidence of NENs as a worldwide phenomenon, affecting most anatomic sites and involving both low-grade (NETs) and high-grade (NECs). Notable increase in NEN incidence is found in Canada (5.86 per 100 000 from 2.46 per 100 000), the Netherlands (4.76 per 100 000 from 3.57 per 100 000), Norway (4.06 per 100 000 from 2.35 per 100 000), and Taiwan (1.51 per 100 000 from 0.30 per 100 000) [34]. Retrospective analyses of single-institution database and national tumor registries from Asia confirm increasing incidence of NENs but also suggest epidemiologic variations among different types of GI-NETs. Specifically, the rectum (> 55%) [35, 36] is the most common, and the small intestine (< 10%) [37, 38] is the least frequent primary sites of NETs among populations in Asian countries. Detailed understanding of the current epidemiological trends of NENs can be gleaned further from data from the US largest tumor registry program, Surveillance, Epidemiology, and End Results (SEER).
According to American Society of Clinical Oncology (ASCO) Cancer.Net website (https://www.cancer.net/cancer-types/neuroendocrine-tumors/statistics, AP accessed 09/29/2021), it is estimated that more than 12 000 people in the USA are diagnosed with NETs each year, and approximately, 175 000 people are living with this diagnosis. Adapted by various sources [29•, 39], these NENs made up less than 0.7% of all new neoplasms in the USA annually. NENs of the gastrointestinal system (GI-NENs), of bronchopulmonary/lung (L-NENs), and unknown primary were 61%, 25%, and 14%, respectively [11]. The distribution among GI-NENS were 33% small intestine (SI-NENs, including cecum), 30% rectum, 13% pancreas (P-NENs), 11% stomach, 8% appendiceal, and 5% colon [11]. The incidence of high-grade NENs is lower than those of low-grade NENs (10–20% vs. 80–90%) [40]. With continued updates in classification of NENs, these epidemiological data are evolving. Analyses of US SEER database (1973 to 2012) have noted a trend to increasing incidence among high-grade NENs or NECs (10.52 per 100 000 from 2.54 per 100 000, 4.1-fold increase) [34]. Consistent with its previous analysis in 2007 [41], the overall incidence and prevalence of NENs in the USA are steadily increasing [29•]. Dasari et al. [29•] report the increase of the annual age-adjusted incidence of NENs from 1.09 per 100,000 persons in 1973 to 6.98 per 100,000 persons in 2012, with the most dramatic rise in incidence was noted in patients 65 years or older with a more than eightfold rise to 25.3 per 100,000 persons. The increase in the incidence from 1973 to 2012 occurred across all primary sites, stages, and grades, with the highest incidences were GEP-NETs (3.56 per 100 000 persons) and lung NETs (1.49 per 100 000 persons) [29•]. Among grade groups, prevalence increases the most in grade 1 (G1) NETs, and among sites, prevalence was highest in the rectum, followed by the lung and small intestine [29•]. The age-, sex-, and race-adjusted 20-year limited duration prevalence for the US population for January 1, 2014, was estimated to be 171,321 [29•], which is significantly higher than the previously reported prevalence of 103,312 in 2004 [41].
The median OS time for patients with NENs is 9.3 years [29•], with statistically significant differences noted among different stages and sites of primary disease [29•]. Multivariate analyses of the population also reproducibly confirmed grade, age, stage, and site as independent predictors of survival [29•, 41]. Evaluating for 5-year mortality hazard rates, Dasari et al. [29•] found patients with G2 (HR, 1.76; 95% CI, 1.59–1.94) and G3 (HR, 5.26; 95% CI, 4.85–5.71) had worse OS than did those with G1. Among all NENs, localized stage had better median OS (> 30 years) compared with regional (10.2 years) and distant stage (12 months) [29•]. Additionally, NENs in the appendix (> 30 years) and rectum (24.6 years) had the best median OS among site groups, while the lung (5.5 years) and pancreas (3.6 years) had the worst median OS. Among distant indolent (G1/G2) NETs, best median OS is associated with the small intestine (SI-NETs, 8.58 years) compared to worse median OS associated with the pancreas (P-NETs, 5.0 years) and the lung (L-NETs, 2.0 years) [29•].
Findings are clear; both incidence and prevalence of NENs have phenomologically increased. The incidence increase is postulated to multiple attributable factors, including increased rate of imaging, improved imagining techniques, detection of early-stage disease, stage migration, and higher public awareness about NENs [11, 29•, 42], without any one definitive or clear causal factor. Among NENs, incidence congruently correlates with prevalence. Evidence reveal the overall survival (OS) rate for all NENs diagnosed in 2000–2004 period improved when compared to those diagnosed in 2009–2012 period [29•]. Patients with distant P-NETs experience the biggest improvement in OS [29•]. As will be discussed later, within the time period of 2009 to 2021, distant P-NET cohort also receives the most FDA-approved systemic therapy, compared to any other NENs. With more NENs being diagnosed, increased survival durations. and more available therapeutic options, researchers logically posit the attributing factors for the increasing incidence are also the same possible explanation for the increased prevalence of NENs.
Diagnosis
Biomarkers have tremendous value in clinical practice and medical industries such as biotechnology (both pharmaceutical and diagnostic), but there is significant confusion about the fundamental concepts. Biomarkers as molecular, histologic, radiologic, or physiologic characteristics are reproducibly and reliably measured as indicators of normal biological or pathogenic processes or responses to an exposure or intervention [43]. The diagnosis of NENs is made with tissue, and radiologic imaging is used to evaluate extend of disease (staging) and assess response to therapy, as well as to localize primary site of disease, while serologic biomarkers aid predicting disease course. Advances in diagnostic options include the development of NETest™ and functional imaging for NENs and have pave the way toward improved management of patients with NENs.
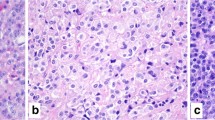
By immunochemistry, all NETs typically stain positive for synaptophysin or chromogranin, while NECs stain negative, while organ-specific immunochemical staining profile helps to delineate primary site origin. In addition to several genomic alterations such as TP53 and RB1, proliferative index using Ki67 and mitoses per high power field (HPF) are used in the current classification to distinguish NETs from NECs. Because of the heterogeneity of NENs, traditional biomarkers such as protein co-secretory product chromogranin-A (CgA) and urinary degradatory amine 5-hydroxyindoleacetic acid (5-HIAA) have limited value and applicability as predictive or prognostic markers [44]. To overcome the limitations of traditional biomarkers, the NET-related transcript-based evaluations test (NETest™) was developed. Tumor transcripts can be detected in the blood circulation and measured by quantitative reverse transcriptase polymerase chain reaction (qRT-PCR). NETest™ is a RNA-based multianalyte algorithmic assay compositely measuring 51 different biologically relevant transcripts involved in gastroenteropancreatic (GEP-NENs) proliferation, signaling, and secretion, as well as genes reported to have a defined association with tumor initiation and metastases [45, 46]. The assay gives a single readout; a cutoff score ≤ 40% to suggest stable disease, and ≥ 80% is considered NENs with high activity. Available data suggest that high activity levels for NETest™ are superior to traditional NEN biomarkers, for the diagnosis and prediction of disease natural history and therapeutic efficacy of somatostatin receptor-targeted therapy [47]. Despite available evidence, the optimal and uniformed application of NETest™ into clinical practice remains undetermined.
Expanding options in radiological techniques to workup clinical symptoms and signs have contributed to earlier and increased diagnoses of NENs. Computed tomography (CT) and magnetic resonance imaging (MRI) establish the foundation of anatomical characterization and evaluation of disease involvement and extent. Unlike anatomical or structural imaging, functional imaging is designed to physiologically examine and measure qualitatively and/or quantitatively changes in metabolism, blood flow, chemical or cellular composition, and receptor density. Using tracers or probes analogous to chemical compounds, like glucose or receptor binding ligands, bound to radioactive isotopes, functional imaging is vital in managing cancer patients.
Somotastatin receptor (SSR) scintigraphy using 111In-indium-pentetreotide, commonly known as octreoscan with or without single-photon emission computed tomography (SPECT), was the only available functional imaging modality for NENs for decades. Octreoscan has been used to localizing primary, staging, and predicting response to somatostatin analogs. Now positron emission tomography (PET) with 68 Ga-gallium-labeled-somatostatin analogs (SSAs such as DOTA0-Tyr3-octreotate [DOTA-TATE] or DOTA0-Phen1-Tyr3 octreotide [DOTA-TOC]), 18F-fluorodeoxyglucose-dihydroxyphenylalanine (18F-DOPA), and 11C-carbon-5-hydroxytryptophan (11C-5-HTP) is available to assist with evaluation and decision-making in the management of NENs. Because of the large variability and heterogeneity of NENs, from proliferation rate (Ki67), SSR subtype profile, and clinical aggressivity, no one radiologic modality is entirely effective, but these advanced functional imaging improve sensitivity and specificity of NEN detection to ~ 80–90% [48]. PET with radioactive-labeled somatostatin analog is available for commercial and clinical use, whereas the others (18F-DOPA and 11C-5-HTP) are only available to research centers. Comparison studies between 68 Ga-SSA-labeled-PET and standard imaging techniques (CT, octreoscan) have consistently demonstrated the superiority in the detection of NEN primary tumors and metastases. PET with 68 Ga-gallium-dotatate (Netspot™) in 2016 and later PET with 64Cu-copper-dotatate (Detectnet™) in 2020 have been approved for use in patients with somatostatin receptor positive NENs. For all practical purpose, except in limited resource healthcare systems, functional imaging with SSA-labeled-PET has replaced octreoscan for patients, because of their superior detection, therapeutic prediction, and increased access with FDA approval.
Therapy
The focus of the review on therapeutic advances will be systemic anti-neoplastic therapy for patients with advanced NENs, particularly GEP-NETs. Complete surgical resection remains closely associated with the chance for cure and durable disease control, among patients with localized and regional NENs. Among unresectable and metastatic NENs, expected outcomes and treatment options are considerably different between histologic grade and primary site.
Traditionally, advanced NECs are managed with cytotoxic systemic therapy, and management of NETs is limited to either observation or symptomatic control with somatostatin analogs (SSAs, octreotide long-acting release [LAR], or lanreotide depot). Robust randomized clinical studies in NENs were traditionally lacking, especially for cytotoxic systemic chemotherapy. For example, among patients with P-NETs, treatment with streptozocin-based combination chemotherapy [49, 50] was supported by results based on combined biochemical and radiologic response criteria not standardized response evaluation criteria in solid tumors (RECIST). Because it is cumbersome to administer and associated with moderate side effects, streptozocin usage has been essentially supplanted by temozolomide, an oral alkylating anti-neoplastic agent. While evidence suggests moderate activity in NETs in both small prospective and large retrospective studies [51,52,53], the adaptation of oral temozolomide plus capecitabine for patients with P-NETs was based largely on retrospective efficacy data [54] and without comparison to streptozocin-based regimens [55]. Among patients with extra-pulmonary NECs, such as small-cell or large-cell, cytotoxic treatment with platinum-based chemotherapy was supported by borrowed evidence from clinical studies for small-cell carcinoma of the lung (SCLC) [56,57,58]. Hence, for many decades, the management of NENs particularly for GEP-NENs had been either borrowed or based on limited clinical evidence.
Both improved understanding of molecular drivers for NENs and supported by results from robust randomized clinical studies lead the way to multiple systemic treatment options. Interestingly, the most dramatic expansion of FDA-approved therapeutic options is for patients with GEP-NETs. Thematically, three molecular targets postulated to drive tumorigenesis, somatostatin receptor, vascular endothelial growth factor (VEGF), and mechanistic target of rapamycin (mTOR) were the focus of drug development for GEP-NETs. Table 1 summarizes outcomes from these pivotal studies.
Nearly 80% of NETs express somatostatin receptors [59]. Because SSAs octreotide and lanreotide bind to somatostatin receptors on the tumor cells, these modified long-acting analogs of endogenous somatostatin are highly effective in inhibiting the release of serotonin and other vasoactive substances. Symptom functional NETs and carcinoid syndrome such as flushing and diarrhea are significantly improved in over 80% with SSAs [60]. Turning the focus of targeting somatostatin receptors for tumor control, two pivotal randomized phase 3 studies with SSAs have demonstrated improved time-to-tumor progression (TTP) with octreotide LAR (14.3 vs. 6.0 months, hazard ratio [HR] = 0.34; 95% CI, 0.20 to 0.59) [61•] and prolonged progression-free survival (PFS) with lanreotide depot (median not reached vs. 18.0 months, HR = 0.47; 95% CI, 0.30 to 0.73) [62•], when compared with placebo. Peptide receptor radioligand therapy (PRRT) has been widely used in European centers to treat advanced somatostatin receptor positive NETs, but no prospective randomized clinical studies were done to detect true outcomes. NETTER-1 was a multicenter randomized phase 3 study, designed to evaluate PFS between treatment with lutetium 177Lu-dotatate, a radiolabeled SSA along with 30 mg octreotide LAR compared to control with 60 mg octreotide LAR, in patients with somatostatin receptor positive advanced SI-NETs. Treatment with lutetium 177Lu-dotatate results in statistically significant improved median PFS when compared to control arm (median not reached vs. 8.5 months; HR = 0.21; 95% CI, 0.13 to 0.32) [63•]. In 2018, the FDA-approved lutetium 177Lu-dotatate was for all patients with GEP-NETs, based largely from the results of NETTER-1 [63•] and the subset analysis (n = 360) of 1214 patients treated at ERASMUS Medical Center [64].
NETs, characterized by a high vascular supply and a strong expression of vascular endothelial growth factor A (VEGF-A), are attractive indication for targeted drug development of anti-angiogenic therapy. Bevacizumab, a monoclonal antibody (MAb) given intravenously, inhibits VEGF-A to slow the growth of new blood vessels. Conceptually, bevacizumab is a great choice for drug development in NETs, targeting angiogenesis. Despite initial demonstration of activity in phase 2 study [65], larger phase 3 randomized study comparing bevacizumab plus octreotide LAR to bevacizumab plus interferon in patients with L-NETs and SI-NETs failed to demonstrate superior efficacy over the control arm [66]. Several small-molecule tyrosine kinase inhibitors (TKIs) that target angiogenic VEGF receptor (VEGFR), including sorafenib [67], sunitinib [68], pazopanib [69], lenvatinib [70], and carbozantinib [71] have been evaluated in phase 2 studies for patients with either P-NETs or SI-NETs. All of these agents demonstrated moderate anti-tumor activity, with more activity seen among patients with P-NETs compared to those with SI-NETs (overall response rate [ORR] 2–16% vs. 9–44%). In the latest non-randomized, phase 2 study of VEGF/VEGFR targeted therapy (TALENT trial), 111 patients with advanced GEP-NETS treated with lenvatinib had ORR 29.9% (95% CI, 21.6 to 39.6); ORRs were 44.2% among P-NET and 16.4% among GI-NET [70]. At present, only sunitinib went on to phase 3 registrational study involving 171 patients with P-NETs. Results demonstrated a prolonged median PFS for those treated with sunitinib compare placebo (11.4 months vs. 5.5 months; HR = 0.42; 95% CI, 0.26 to 0.66) [72•]. Sunitinib, being FDA-approved, is the only targeted therapy against angiogenesis to treat patients with P-NETs. Results from surufatinib in advanced neuroendocrine tumor for pancreatic (SANET-p) [73•] and extra-pancreatic (SANET-ep) [74•] further confirm the role of small-molecule inhibitors of angiogenesis in treating patients with GEP-NETs. Among patients with extra-pancreatic NETs, median PFS was superior with surufatinib compared to placebo (9.2 months vs. 3.8 months; HR = 0.33; 95% CI, 0.22 to 0.50) [74•]. Similar benefit in median PFS was found among patients with P-NETs treated with surufatinib compared to placebo (10.9 months vs. 3.7 months; HR = 0.49; 95% CI, 0.32 to 0.76) [73•]. Surufatinib results have been submitted for consideration of FDA approval.
Through interacting with several proteins to form multiprotein complexes, mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2), mTOR regulates key cell functions involved in cell survival, proliferation, and metabolism [75]. Two important observations support the importance of mTOR pathways in the tumorigenesis of NETs. Firstly, pathogenic mutations of genes associated with hereditary syndromes predisposing NETs encode for proteins that lie upstream from mTOR. Loss of function due to inactivating mutations of neurofibromatosis type 1 (NF-1) and tuberous sclerosis (TSC1 and TSC2) genes leads to mTOR activation in NET patients [76]. The second observation came from genomic analysis of sporadic pancreatic NETs, identifying somatic mutations in genes [15•] and components of genes [77] involved in the mTOR pathway. Targeting mTOR pathway for drug development in NETs has proven to be very successful. Everolimus, an oral mTOR inhibitor, was evaluated in four clinical studies, the RAD-001 (everolimus) In Advanced Neuroendocrine Tumor (RADIANT) studies. RADIANT-1 evaluated two doses of everolimus (5 mg and 10 mg) plus octreotide LAR in 150 patients with SI- and P-NETs, demonstrating 20% overall response rate (ORR) and 15.0 months PFS [78]. RADIANT-2 evaluated the combination of everolimus (10 mg) plus octreotide LAR compared to octreotide LAR alone in 429 patients with SI-NETs. Primary endpoint of RADIANT-2 (median PFS) did not reach statistical significance (16.4 months vs. 11.3 months; HR = 0.77; 95% CI, 0.59 to 1.00) [79]. RADIANT-3 showed treatment with everolimus prolonged median PFS in patients with advanced P-NETs when compared to placebo (11.0 months vs. 4.6 months; HR = 0.35; 95% CI 0.27 to 0.45) [80•]. RADIANT-4 demonstrated treatment with everolimus improved median PFS in patients with advanced gastrointestinal (GI)-NETs and L-NETs when compared to placebo arm (14.0 months vs. 5.5 months; HR = 0.39; 95% CI 0.28 to 0.54) [81•]. Results collected from all four RADIANT studies were successful in obtaining FDA approval of everolimus for patients with advanced P-NETs and GI- and L-NETs.
With multiple approved systemic therapeutic options, ranging from cytotoxic chemotherapy, targeted small molecules targeting VEGF/VEGFR and mTOR and PRRT, sequencing of systemic therapy requires continued elucidation. Because streptozocin-based chemotherapy is still foundationally used in many parts of Europe to treat advanced P-NETs, further understanding on the efficacy of this combination compared to presently approved everolimus is needed. Efficacy and safety of frontline everolimus versus combination cytotoxic chemotherapy streptozocin and 5-flurouracil (STZ-5FU) in patients with advanced P-NETs are being evaluated in ongoing phase 3 randomized study (SEQTOR trial, ClinicalTrials.gov identifier, NCT02246127). The results are anticipated to provide further clarification on the role of combination chemotherapy versus oral targeted therapy for this patient cohort. Furthermore, studies such as SEQTOR are keys to studying patients who have a longer life expectancy and whose quality of life can be altered by the sequence of treatment.
The combination of scientific and technological advances and regulatory government reforms and incentives, along with robust commercial incentives, has come together in a perfect storm, fueling the momentous era of drug developments. Tremendous scientific advancements and accessibility of next-generation sequencing (NSG) have paved the way to genomic characterization of many neoplastic processes, identification of novel oncogenic targets, and the development of new targeted therapies. Concurrently, reforms in orphan disease designation and expedited drug approval processes by FDA regulatory agency have revolutionarily brought forth many novel and targeted cancer therapy in the past two decades. Representative of this paradigm shift in cancer treatment and drug development are two momentous transformations: (1) immunotherapies and (2) tissue/tumor-agnostic treatments.
Tumor can escape the immune surveillance by several possible mechanisms, but the most commonly targeted is to reverse the cancer inhibition of adaptive immunity by blocking T cell checkpoint pathways. Clinical studies with monoclonal antibodies (MAbs) developed to inhibit the CTLA-4 checkpoint molecule or to inhibit the interaction between PD-1 checkpoint and its ligands (PD-L1 and PD-L2) have led to many FDA-approved cancer therapy in many different cancers. Table 2 summarizes clinical studies that have been done with immunotherapy in patients with GEP-NETs. MAbs blocking PD-1, such as spartalizumab or pembrolizumab, have resulted in modest ORR, ranging 4–12% [82,83,84]. Combination therapy of MAbs blocking PD-1 and CTLA-4, nivolumab plus ipilimumab, has demonstrated slightly higher ORR, 25–33% [85, 86]. Early studies demonstrated encouraging activity of immunotherapies, and plans to further confirm their anti-neoplastic activity in patients with indolent NETs are continuing.
The FDA made a landmark decision to create a new category of cancer therapy, tissue/tumor-agnostic drugs in 2017. Being highly selective for specific molecular alterations, tissue/tumor-agnostic drugs are active against multiple different subtypes of oncogene-addicted cancers. Three drugs of this new tumor-agnostic therapeutic class, pembrolizumab for patients with solid tumors with microsatellite instability-high (MSI-H) or deficient mismatch repair (dMMR), larotrectinib for patients with solid tumors with activating neurotrophic TRK (NTRK) gene fusions, and entrectinib for patients with solid tumors with activating NTRK gene fusions and patients with non-small-cell lung cancer (NSCLC) with activating fusion anaplastic lymphoma kinase (ALK) or mutation of the proto-oncogene tyrosine protein kinase 1 (ROS-1), have received FDA approval in 2017, 2018, and 2019, respectively. Pembrolizumab is anti-PD-1 MAb given intravenously, and larotrectinib and entrectinib are oral small-molecule inhibitors of pan-tropomyosin receptor tyrosine kinase (pan-TRK). These approved tumor-agonistic drugs further add to the therapeutic armamentarium for specific patients with NENs.
As understanding for molecular drivers of tumorigenesis of NENs continues to expand, the development of targeted therapy for NENs will no doubt continue. As this paper is being written, the FDA approved belzutifan, an orally available hypoxia-inducible factor inhibitor, for the cancers associated with von Hippel–Lindau (VHL) disease. In an ongoing registrational phase 2 study, belzutifan demonstrated ORR 83% among 12 patients with advanced P-NETs [87].
Summary and Conclusion
A combination of scientific advances, improved disease classification, and better molecular and epidemiologic understandings of NENs, along with successes in targeted drug developments in GEP-NETs, has all culminate in transforming the clinical practices and management of patients with NENs. Accessible NGS has identified meaningful biomarkers and molecular drivers of NENs. Uniformed WHO classification of NENs and the maturation of large tumor registries lead to the discovery of a worldwide phenomological occurrence, where both incidence and prevalence of NENs have been steadily increasing. At present, patients with GEP-NETs have five FDA-approved therapy for advanced disease, along with two functional imaging options to assess specifically for somatostatin receptor positive disease. The field of neuroendocrine oncology has changed a lot in the past 20 years, and patients with NENs have options and hope, and their cancer is no longer a misomer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Oberndorfer S. Karzinoide tumoren des dunndarms. 1907. 1:426-432
Gosset A, Masson P. Tumeurs endocrines de l’appendice. Presse Med. 25:237–240.
Modlin IM, Shapiro MD, Kidd M. Siegfried Oberndorfer: origins and perspectives of carcinoid tumors. Hum Pathol. 2004;35(12):1440–51. https://doi.org/10.1016/j.humpath.2004.09.018.
Keener J, Sneyd J. Neuroendocrine cells. In: Keener J, Sneyd J, eds. Mathematical Physiology. Vol 8/1. Interdisciplinary Applied Mathematics. Springer New York; 2009:385–426. https://doi.org/10.1007/978-0-387-75847-3_9
Kaltsas GA, Besser GM, Grossman AB. The diagnosis and medical management of advanced neuroendocrine tumors. Endocr Rev. 2004;25(3):458–511. https://doi.org/10.1210/er.2003-0014.
Metovic J, Barella M, Bianchi F, et al. Morphologic and molecular classification of lung neuroendocrine neoplasms. Virchows Arch Int J Pathol. 2021;478(1):5–19. https://doi.org/10.1007/s00428-020-03015-z.
Strosberg JR. Update on the management of unusual neuroendocrine tumors: pheochromocytoma and paraganglioma, medullary thyroid cancer and adrenocortical carcinoma. Semin Oncol. 2013;40(1):120–33. https://doi.org/10.1053/j.seminoncol.2012.11.009.
Shah MH, Goldner WS, Halfdanarson TR, et al. NCCN guidelines insights: neuroendocrine and adrenal tumors version 2 2018. J Natl Compr Canc Netw. 2018;16(6):693–702.
Fishbein L, Del Rivero J, Else T, et al. The North American Neuroendocrine Tumor Society Consensus Guidelines for Surveillance and Management of Metastatic and/or Unresectable Pheochromocytoma and Paraganglioma. Pancreas. 2021;50(4):469–93. https://doi.org/10.1097/MPA.0000000000001792.
Rindi G, Inzani F. Neuroendocrine neoplasm update: toward universal nomenclature. Endocr Relat Cancer. 2020;27(6):R211–8. https://doi.org/10.1530/ERC-20-0036.
Fernandez CJ, Agarwal M, Pottakkat B, Haroon NN, George AS, Pappachan JM. Gastroenteropancreatic neuroendocrine neoplasms: a clinical snapshot. World J Gastrointest Surg. 2021;13(3):231–55. https://doi.org/10.4240/wjgs.v13.i3.231.
Assarzadegan N, Montgomery E. What is new in the 2019 World Health Organization (WHO) classification of tumors of the digestive system: review of selected updates on neuroendocrine neoplasms, appendiceal tumors, and molecular testing. Arch Pathol Lab Med. 2021;145(6):664–77. https://doi.org/10.5858/arpa.2019-0665-RA.
Konukiewitz B, Schlitter AM, Jesinghaus M, et al. Somatostatin receptor expression related to TP53 and RB1 alterations in pancreatic and extrapancreatic neuroendocrine neoplasms with a Ki67-index above 20. Mod Pathol Off J U S Can Acad Pathol Inc. 2017;30(4):587–98.
Yachida S, Vakiani E, White CM, et al. Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2012;36(2):173–84. https://doi.org/10.1097/PAS.0b013e3182417d36
• Jiao Y, Shi C, Edil BH, et al. DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science. 2011;331(6021):1199–203. https://doi.org/10.1126/science.1200609. This is important because it is one of the few original data on molecular tumorigenesis of pancreatic NETs.
Australian Pancreatic Cancer Genome Initiative, Scarpa A, Chang DK, et al. Whole-genome landscape of pancreatic neuroendocrine tumours. Nature. 2017;543(7643):65–71. https://doi.org/10.1038/nature21063 This is important review on molecular landscape of small intestine NETs.
Scarpa A. The landscape of molecular alterations in pancreatic and small intestinal neuroendocrine tumours. Ann Endocrinol. 2019;80(3):153–8. https://doi.org/10.1016/j.ando.2019.04.010.
Mafficini A, Scarpa A. Genetics and epigenetics of gastroenteropancreatic neuroendocrine neoplasms. Endocr Rev. 2019;40(2):506–36. https://doi.org/10.1210/er.2018-00160.
Cunningham JL, Díaz de Ståhl T, Sjöblom T, Westin G, Dumanski JP, Janson ET. Common pathogenetic mechanism involving human chromosome 18 in familial and sporadic ileal carcinoid tumors. Genes Chromosomes Cancer. 2011;50(2):82–94. https://doi.org/10.1002/gcc.20834.
Karpathakis A, Dibra H, Pipinikas C, et al. Prognostic impact of novel molecular subtypes of small intestinal neuroendocrine tumor. Clin Cancer Res. 2016;22(1):250–8. https://doi.org/10.1158/1078-0432.CCR-15-0373.
Andersson E, Swärd C, Stenman G, Ahlman H, Nilsson O. High-resolution genomic profiling reveals gain of chromosome 14 as a predictor of poor outcome in ileal carcinoids. Endocr Relat Cancer. 2009;16(3):953–66. https://doi.org/10.1677/ERC-09-0052.
Marx SJ. Molecular genetics of multiple endocrine neoplasia types 1 and 2. Nat Rev Cancer. 2005;5(5):367–75. https://doi.org/10.1038/nrc1610.
Donis-Keller H, Dou S, Chi D, et al. Mutations in the RET proto-oncogene are associated with MEN 2A and FMTC. Hum Mol Genet. 1993;2(7):851–6. https://doi.org/10.1093/hmg/2.7.851.
Varshney N, Kebede AA, Owusu-Dapaah H, Lather J, Kaushik M, Bhullar JS. A Review of Von Hippel-Lindau syndrome. J Kidney Cancer VHL. 2017;4(3):20–9. https://doi.org/10.15586/jkcvhl.2017.88.
Larson AM, Hedgire SS, Deshpande V, et al. Pancreatic neuroendocrine tumors in patients with tuberous sclerosis complex. Clin Genet. 2012;82(6):558–63. https://doi.org/10.1111/j.1399-0004.2011.01805.x.
Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44(2):81–8. https://doi.org/10.1136/jmg.2006.045906.
Geurts JL. Inherited syndromes involving pancreatic neuroendocrine tumors. J Gastrointest Oncol. 2020;11(3):559–66. https://doi.org/10.21037/jgo.2020.03.09.
Fritz A. International Classification of Diseases for Oncology: ICD-O (Ed 3). World Health Organization; 2000. This is important because it is the largest reporting of epidemiologic study
• Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335. https://doi.org/10.1001/jamaoncol.2017.0589. This is important because it is the large USA population analysis leading to robust epidemiological understanding of NETs.
Hallet J, Law CHL, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes: neuroendocrine tumor epidemiology. Cancer. 2015;121(4):589–97. https://doi.org/10.1002/cncr.29099.
Ellis L, Shale MJ, Coleman MP. Carcinoid tumors of the gastrointestinal tract: trends in incidence in England since 1971. Am J Gastroenterol. 2010;105(12):2563–9. https://doi.org/10.1038/ajg.2010.341.
Korse CM, Taal BG, van Velthuysen MLF. Visser O 2013 Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer Oxf Engl. 1990;49(8):1975–83. https://doi.org/10.1016/j.ejca.2012.12.022.
Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113(10):2655–64. https://doi.org/10.1002/cncr.23883.
Leoncini E, Boffetta P, Shafir M, Aleksovska K, Boccia S, Rindi G. Increased incidence trend of low-grade and high-grade neuroendocrine neoplasms. Endocrine. 2017;58(2):368–79. https://doi.org/10.1007/s12020-017-1273-x.
Lim CH, Lee IS, Jun BY, et al. Incidence and clinical characteristics of gastroenteropancreatic neuroendocrine tumor in Korea: a single-center experience. Korean J Intern Med. 2017;32(3):452–8. https://doi.org/10.3904/kjim.2015.232.
JNETS Project Study Group, Masui T, Ito T, Komoto I, Uemoto S. Recent epidemiology of patients with gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NEN) in Japan: a population-based study. BMC Cancer. 2020;20(1):1104. https://doi.org/10.1186/s12885-020-07581-y.
Fan JH, Zhang YQ, Shi SS, et al. A nation-wide retrospective epidemiological study of gastroenteropancreatic neuroendocrine neoplasms in china. Oncotarget. 2017;8(42):71699–708. https://doi.org/10.18632/oncotarget.17599.
Cho MY, Kim JM, Sohn JH, et al. Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000–2009: multicenter study. Cancer Res Treat. 2012;44(3):157–65. https://doi.org/10.4143/crt.2012.44.3.157.
Chauhan A, Yu Q, Ray N, et al. Global burden of neuroendocrine tumors and changing incidence in Kentucky. Oncotarget. 2018;9(27):19245–54. https://doi.org/10.18632/oncotarget.24983.
Pavel M, Öberg K, Falconi M, et al. Gastroenteropancreatic neuroendocrine neoplasms: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol. 2020;31(7):844–60. https://doi.org/10.1016/j.annonc.2020.03.304.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063–72. https://doi.org/10.1200/JCO.2007.15.4377.
Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing but NET: a review of neuroendocrine tumors and carcinomas. Neoplasia. 2017;19(12):991–1002. https://doi.org/10.1016/j.neo.2017.09.002.
FDA-NIH Biomarker Working Group. BEST (biomarkers, endpoints, and other tools) resource. Food and Drug Administration (US); 2016. Accessed October 3, 2021. http://www.ncbi.nlm.nih.gov/books/NBK326791/
Oberg K, Modlin IM, De Herder W, et al. Consensus on biomarkers for neuroendocrine tumour disease. Lancet Oncol. 2015;16(9):e435–46. https://doi.org/10.1016/S1470-2045(15)00186-2.
Kidd M, Drozdov I, Modlin I. Blood and tissue neuroendocrine tumor gene cluster analysis correlate, define hallmarks and predict disease status. Endocr Relat Cancer. 2015;22(4):561–75. https://doi.org/10.1530/ERC-15-0092.
Modlin IM, Drozdov I, Kidd M. Gut neuroendocrine tumor blood qPCR fingerprint assay: characteristics and reproducibility. Clin Chem Lab Med. 2014;52(3):419–29. https://doi.org/10.1515/cclm-2013-0496.
Öberg K, Califano A, Strosberg JR, et al. A meta-analysis of the accuracy of a neuroendocrine tumor mRNA genomic biomarker (NETest) in blood. Ann Oncol Off J Eur Soc Med Oncol. 2020;31(2):202–12. https://doi.org/10.1016/j.annonc.2019.11.003.
Bodei L, Sundin A, Kidd M, Prasad V, Modlin IM. The status of neuroendocrine tumor imaging: from darkness to light? Neuroendocrinol. 2014;101(1):1–17. https://doi.org/10.1159/000367850.
Moertel CG, Hanley JA, Johnson LA. Streptozocin alone compared with streptozocin plus fluorouracil in the treatment of advanced islet-cell carcinoma. N Engl J Med. 1980;303(21):1189–94. https://doi.org/10.1056/NEJM198011203032101.
Moertel CG, Lefkopoulo M, Lipsitz S, Hahn RG, Klaassen D. Streptozocin–doxorubicin, streptozocin–fluorouracil, or chlorozotocin in the treatment of advanced islet-cell carcinoma. N Engl J Med. 1992;326(8):519–23. https://doi.org/10.1056/NEJM199202203260804.
Kulke MH, Stuart K, Enzinger PC, et al. Phase II study of temozolomide and thalidomide in patients with metastatic neuroendocrine tumors. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(3):401–6. https://doi.org/10.1200/JCO.2005.03.6046.
Chan JA, Stuart K, Earle CC, et al. Prospective study of bevacizumab plus temozolomide in patients with advanced neuroendocrine tumors. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(24):2963–8. https://doi.org/10.1200/JCO.2011.40.3147.
Kulke MH, Hornick JL, Frauenhoffer C, et al. O6-methylguanine DNA methyltransferase deficiency and response to temozolomide-based therapy in patients with neuroendocrine tumors. Clin Cancer Res Off J Am Assoc Cancer Res. 2009;15(1):338–45. https://doi.org/10.1158/1078-0432.CCR-08-1476.
Cives M, Ghayouri M, Morse B, et al. Analysis of potential response predictors to capecitabine/temozolomide in metastatic pancreatic neuroendocrine tumors. Endocr Relat Cancer. 2016;23(9):759–67. https://doi.org/10.1530/ERC-16-0147.
Kunz PL, Catalano PJ, Nimeiri H, et al. 2018 A randomized study of temozolomide or temozolomide and capecitabine in patients with advanced pancreatic neuroendocrine tumors: a trial of the ECOG-ACRIN Cancer Research Group (E2211). J Clin Oncol. 2018;36(15_supp):4004–4004. https://doi.org/10.1200/JCO.2018.36.15_suppl.4004.
Roth BJ, Johnson DH, Einhorn LH, et al. Randomized study of cyclophosphamide, doxorubicin, and vincristine versus etoposide and cisplatin versus alternation of these two regimens in extensive small-cell lung cancer: a phase III trial of the Southeastern Cancer Study Group. J Clin Oncol Off J Am Soc Clin Oncol. 1992;10(2):282–91. https://doi.org/10.1200/JCO.1992.10.2.282.
Fukuoka M, Furuse K, Saijo N, et al. Randomized trial of cyclophosphamide, doxorubicin, and vincristine versus cisplatin and etoposide versus alternation of these regimens in small-cell lung cancer. J Natl Cancer Inst. 1991;83(12):855–61. https://doi.org/10.1093/jnci/83.12.855.
Sundstrøm S, Bremnes RM, Kaasa S, et al. Cisplatin and etoposide regimen is superior to cyclophosphamide, epirubicin, and vincristine regimen in small-cell lung cancer: results from a randomized phase III trial with 5 years’ follow-up. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20(24):4665–72. https://doi.org/10.1200/JCO.2002.12.111.
Reubi JC, Kvols LK, Waser B, et al. Detection of somatostatin receptors in surgical and percutaneous needle biopsy samples of carcinoids and islet cell carcinomas. Cancer Res. 1990;50(18):5969–77.
Kvols LK, Moertel CG, Óconnell MJ, Schutt AJ, Rubin J, Hahn RG. Treatment of the malignant carcinoid syndrome Evaluation of a long-acting somatostatin analogue. N Engl J Med. 1986;315(11):663–6. https://doi.org/10.1056/NEJM198609113151102.
• Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID study group. J Clin Oncol. 2009;27(28):4656–63. https://doi.org/10.1200/JCO.2009.22.8510. The same pivotal and practice changing trials.
• Caplin ME, Pavel M, Ćwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33. https://doi.org/10.1056/NEJMoa1316158. The same pivotal and practice changing trials.
• Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35. https://doi.org/10.1056/NEJMoa1607427. The same pivotal and practice changing trials.
Kwekkeboom DJ, de Herder WW, Kam BL, et al. Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(13):2124–30. https://doi.org/10.1200/JCO.2007.15.2553.
Yao JC, Phan A, Hoff PM, et al. Targeting vascular endothelial growth factor in advanced carcinoid tumor: a random assignment phase II study of depot octreotide with bevacizumab and pegylated interferon alpha-2b. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(8):1316–23. https://doi.org/10.1200/JCO.2007.13.6374.
Yao JC, Guthrie KA, Moran C, et al. Phase III prospective randomized comparison trial of depot octreotide plus interferon alfa-2b versus depot octreotide plus bevacizumab in patients with advanced carcinoid tumors: SWOG S0518. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35(15):1695–703. https://doi.org/10.1200/JCO.2016.70.4072.
Hobday TJ, Rubin J, Holen K, et al. MC044h, a phase II trial of sorafenib in patients (pts) with metastatic neuroendocrine tumors (NET): a phase II consortium (P2C) study. J Clin Oncol. 2007;25(18_suppl):4504–4504. https://doi.org/10.1200/jco.2007.25.18_suppl.4504.
Kulke MH, Lenz HJ, Meropol NJ, et al. Activity of sunitinib in patients with advanced neuroendocrine tumors. J Clin Oncol. 2008;26(20):3403–10. https://doi.org/10.1200/JCO.2007.15.9020.
Phan AT, Halperin DM, Chan JA, et al. Pazopanib and depot octreotide in advanced, well-differentiated neuroendocrine tumours: a multicentre, single-group, phase 2 study. Lancet Oncol. 2015;16(6):695–703. https://doi.org/10.1016/S1470-2045(15)70136-1.
Capdevila J, Fazio N, Lopez C, et al. Lenvatinib in patients with advanced grade 1/2 pancreatic and gastrointestinal neuroendocrine tumors: results of the phase II TALENT trial (GETNE1509). J Clin Oncol Off J Am Soc Clin Oncol. 2021;39(20):2304–12. https://doi.org/10.1200/JCO.20.03368.
Chan JA, Faris JE, Murphy JE, et al. Phase trial of cabozantinib in patients with carcinoid and pancreatic neuroendocrine tumors. J Clin Oncol. 2017;35(4_supp):228–228. https://doi.org/10.1200/JCO.2017.35.4_suppl.228.
• Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):501–13. https://doi.org/10.1056/NEJMoa1003825. The same pivotal and practice changing trials.
• Xu J, Shen L, Bai C, et al. Surufatinib in advanced pancreatic neuroendocrine tumours (SANET-p): a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21(11):1489–99. https://doi.org/10.1016/S1470-2045(20)30493-9. The same pivotal and practice changing trials.
• Xu J, Shen L, Zhou Z, et al. Surufatinib in advanced extrapancreatic neuroendocrine tumours (SANET-ep): a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21(11):1500–12. https://doi.org/10.1016/S1470-2045(20)30496-4. The same pivotal and practice changing trials.
Zoncu R, Efeyan A, Sabatini DM. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol. 2011;12(1):21–35. https://doi.org/10.1038/nrm3025.
Chan J, Kulke M. Targeting the mTOR signaling pathway in neuroendocrine tumors. Curr Treat Options Oncol. 2014;15(3):365–79. https://doi.org/10.1007/s11864-014-0294-4.
Kasajima A, Pavel M, Darb-Esfahani S, et al. mTOR expression and activity patterns in gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer. 2011;18(1):181–92. https://doi.org/10.1677/ERC-10-0126.
Yao JC, Phan AT, Chang DZ, et al. Efficacy of RAD001 (everolimus) and octreotide LAR in advanced low- to intermediate-grade neuroendocrine tumors: results of a phase II study. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(26):4311–8. https://doi.org/10.1200/JCO.2008.16.7858.
Pavel ME, Hainsworth JD, Baudin E, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet Lond Engl. 2011;378(9808):2005–12. https://doi.org/10.1016/S0140-6736(11)61742-X.
• Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514–23. https://doi.org/10.1056/NEJMoa1009290. The same pivotal and practice changing trials.
• Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet Lond Engl. 2016;387(10022):968–77. https://doi.org/10.1016/S0140-6736(15)00817-X. The same pivotal and practice changing trials.
Yao JC, Strosberg J, Fazio N, et al. Spartalizumab in metastatic, well/poorly-differentiated neuroendocrine neoplasms. Endocr Relat Cancer. Published online January 1, 2021:ERC-20–0382.R1. https://doi.org/10.1530/ERC-20-0382
Strosberg J, Mizuno N, Doi T, et al. Efficacy and safety of pembrolizumab in previously treated advanced neuroendocrine tumors: results from the phase II KEYNOTE-158 study. Clin Cancer Res Off J Am Assoc Cancer Res. 2020;26(9):2124–30. https://doi.org/10.1158/1078-0432.CCR-19-3014.
Mehnert JM, Bergsland E, O’Neil BH, et al. Pembrolizumab for the treatment of programmed death-ligand 1-positive advanced carcinoid or pancreatic neuroendocrine tumors: results from the KEYNOTE-028 study. Cancer. 2020;126(13):3021–30. https://doi.org/10.1002/cncr.32883.
Klein O, Kee D, Markman B, et al. Immunotherapy of ipilimumab and nivolumab in patients with advanced neuroendocrine tumors: a subgroup analysis of the CA209-538 clinical trial for rare cancers. Clin Cancer Res Off J Am Assoc Cancer Res. 2020;26(17):4454–9. https://doi.org/10.1158/1078-0432.CCR-20-0621.
Patel SP, Othus M, Chae YK, et al. A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART SWOG 1609) in patients with nonpancreatic neuroendocrine tumors. Clin Cancer Res Off J Am Assoc Cancer Res. 2020;26(10):2290–6. https://doi.org/10.1158/1078-0432.CCR-19-3356.
Srinivasan R, Donskov F, Iliopoulos O, et al. Phase 2 study of belzutifan (MK-6482), an oral hypoxia-inducible factor 2α (HIF-2α) inhibitor, for Von Hippel-Lindau (VHL) disease-associated clear cell renal cell carcinoma (ccRCC). J Clin Oncol. 2021;39(15_suppl):4555–4555. https://doi.org/10.1200/JCO.2021.39.15_suppl.4555.
Hörsch D, Ezziddin S, Haug A, et al. Effectiveness and side-effects of peptide receptor radionuclide therapy for neuroendocrine neoplasms in Germany: a multi-institutional registry study with prospective follow-up. Eur J Cancer Oxf Engl. 1990;2016(58):41–51. https://doi.org/10.1016/j.ejca.2016.01.009.
Brabander T, van der Zwan WA, Teunissen JJM, et al. Long-term efficacy, survival, and safety of [177Lu-DOTA0, Tyr3]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin Cancer Res Off J Am Assoc Cancer Res. 2017;23(16):4617–24. https://doi.org/10.1158/1078-0432.CCR-16-2743.
Sun W, Lipsitz S, Catalano P, Mailliard JA, Haller DG. Phase II/III study of doxorubicin with fluorouracil compared with streptozocin with fluorouracil or dacarbazine in the treatment of advanced carcinoid tumors: eastern cooperative oncology group study E1281. J Clin Oncol. 2005;23(22):4897–904. https://doi.org/10.1200/JCO.2005.03.616.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
Emma N. Rizen declares that she has no conflict of interest. Alexandria T. Phan has received compensation for service as a consultant from Roche Diagnostics, and has received speaker's honoraria from Ipsen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Neuroendocrine Neoplasms
Rights and permissions
About this article
Cite this article
Rizen, E.N., Phan, A.T. Neuroendocrine Tumors: a Relevant Clinical Update. Curr Oncol Rep 24, 703–714 (2022). https://doi.org/10.1007/s11912-022-01217-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01217-z