Abstract
Purpose of Review
The development of carcinoid heart disease (CHD) is a fibrotic complication of neuroendocrine neoplasms (NEN) which is associated with a poor prognosis. This review aims to summarise the clinical features, investigations and management of this condition.
Recent Findings
CHD can affect up to 50% of NET patients with carcinoid syndrome. However, it is often not screened for appropriately and recognised late when patients become symptomatic. A screening strategy with biomarkers and multimodality imaging is necessary for early recognition. Management by an experienced multidisciplinary team with appropriate medical therapeutic strategies and where indicated surgical intervention is needed to optimise clinical outcomes.
Summary
CHD is a poor prognostic factor, but recently, outcomes have improved due to the multidisciplinary approach and centralised care of CHD-NET patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasms (NENs) are relatively rare tumours with an annual age-adjusted incidence of 6.98 per 100,000 persons [1]. They represent a heterogeneous group of neoplasms that arise from neuroendocrine cells of the diffuse endocrine system, and the most common sites of origin are the gastrointestinal and bronchopulmonary system [1, 2]. Although they are considered rare, their incidence is rising [1]. These neoplasms are often associated with fibrosis which may occur at local or distant sites [3, 4]. Even though this association has been known for a long time, the pathophysiology of fibrogenesis in NENs remains poorly understood [4]. Carcinoid heart disease (CHD) is a relatively common fibrotic complication of NENs which is characterised by the development of plaque-like, fibrous endocardial thickening affecting the heart valves (mainly of the right heart) [5, 6]. It may affect up to 40% (and in recent years around 20%) of patients with carcinoid syndrome (typically defined as the triad of flushing, diarrhoea and bronchospasm) that develops due to the effects of serotonin and the release of biogenic amines and other peptides by the tumour into the systemic circulation [5, 7]. The development of CHD is a poor prognostic feature and is associated with substantial morbidity and mortality [8, 9]. In this review article, we provide a comprehensive overview of the pathophysiology, clinical and epidemiological characteristics, relevant biomarkers and imaging modalities, as well as management strategies for CHD.
Pathophysiology
The pathogenesis of fibrosis in NENs has not been completely delineated, and little progress has been made in recent decades to better understand the underlying mechanisms of fibrogenesis. It is generally thought that NEN-associated fibrosis is due to the effects of serotonin, growth factors and other peptides secreted by the neuroendocrine tumour cells, but these factors do not act independently of each other, and pathway crosstalk is important in the pathophysiology of the fibrotic process (Fig. 1) [3•].
Schematic representation of our current understanding of the pathophysiology of fibrosis in NETs. Several factors within the tumour microenvironment play a role in fibrogenesis and are known to interact with each other. The pathway cross talk largely accounts for the complexity of the process, and the difficulty in establishing effective antifibrotic therapies
Serotonin appears to play a central role in the development of CHD [3•]. This is supported by several experimental animal studies and a combination of prospective and retrospective clinical studies which are summarised in another review article by our group [3•]. Further evidence for the role of serotoninergic pathways in the development of CHD comes from the elucidation of the pathophysiology of drug-induced valvular heart disease. Antimigraine ergot alkaloid agents (ergotamine and methysergide), appetite suppressants (fenfluramine and dexfenfluramine) and ergot-derived dopamine agonists used for the treatment of Parkinson disease and restless leg syndrome (pergolide and cabergoline) have been associated with the development of mainly left-sided valvular abnormalities that closely resemble carcinoid-related valvulopathies, thereby raising suspicion for a common pathophysiologic mechanism with CHD [3, 10,11,12,13,14,15,16]. All the implicated drugs (or their metabolites) have been shown to have high affinity for and to be partial or full agonists of the 5-HT receptor subtype 5-HT2B (5-HT2B R). 5-HT2B R agonists can mediate fibroblast mitogenesis in vitro, suggesting that circulating serotonin may directly stimulate the proliferation of valve interstitial cells and induce heart valve fibroplasia [17, 18]. The 5-HT2B R also mediates important trophic functions in cardiovascular morphogenesis [19, 20]. There is also some evidence that serotoninergic pathways may induce oxidative stress which can promote the development of fibrosis in heart valves [21, 22].
TGFβ is a downstream mediator of serotonin and major driver of fibrosis [23] which has also been implicated in the development of CHD [3•]. Clinicopathological investigation of human carcinoid and normal valve cusps using immunohistochemical techniques demonstrated that staining for the latent form of TGF-β1 (LAP TGF-β1) and alpha smooth muscle actin (a marker of activated myofibroblasts) was more prominent in carcinoid compared with control valves. Conceivably, the greater amounts of LAP TGF-β1 found in carcinoid cusps compared with controls are likely to reflect upregulation of TGF-β because of serotonin [24].
Further research is needed into the pathophysiology of CHD in order to gain a better understanding of the underlying processes, and this will be of critical importance for the development of targeted antifibrotic therapies for valvular fibrosis.
Epidemiology and Prognosis
Estimates of CHD prevalence and incidence among patients with carcinoid syndrome vary widely at 3–65% and 3–42%, respectively, but generally tend to be lower in recent studies [5, 25, 26]. This may be due to the increased use of somatostatin analogues and their effect on circulating serotonin levels [25]. Most cases of CHD are associated with small-bowel NENs (72%), followed by lung (4%), large bowel (4%), pancreatic (1%), appendiceal (1%) and ovarian neoplasms (1–3%), while in 18% the primary site is unknown [27]. A recent study from the Mayo clinic showed that CHD is rare in patients with bronchopulmonary NENs (<1%). In that series of 185 patients diagnosed with lung NENs who had also undergone echocardiographic evaluation, CHD was associated with the presence of liver metastases, and left-sided valve involvement was only seen in the presence of a patent foramen ovale (PFO) [28]. This indicates that primary bronchopulmonary NENs do not usually secrete sufficient fibrogenic substances to induce left-sided valvular changes in the absence of metastatic disease or intracardiac shunts and question the need for regular surveillance in such cases [28].
The development of CHD is associated with increased morbidity and mortality [5]. A study from the Mayo clinic which was published in 1993 showed a 3-year survival of 31% in patients with CHD compared with 68% for patients without valvular involvement [27]. A mean overall survival of 3.8 years has been reported in patients with CHD [5] with a relatively wide range in different publications (11 months–6.5 years) [26], and the severity of CHD determines prognosis [29]. The prognostic significance of 5-hydroxyindoleacetic acid (5-HIAA) levels in the progression of CHD has been shown in several studies [26, 29,30,31]. In addition, higher 5-HIAA levels are associated with increased odds of death [26].
The prognosis of patients with CHD has improved in recent decades which is probably due to improvements in medical and surgical therapeutic strategies, cardiac imaging technologies and the multidisciplinary approach for the management of CHD [8, 32]. A retrospective study from the Mayo clinic of 200 patients with CHD showed that the median survival improved from 1.5 years in the 1980s to 4.4 years in the late 1990s, which the authors attributed most probably to the introduction of valve replacement surgery [9]. In addition, a recent multicentre study from 8 ENETS Centres of Excellence which has been published in abstract form showed that in 136 patients with midgut NENs diagnosed with CHD between 2008 and 2018, the median survival was 2.4 years (95% CI, 1.6–2.9 years). The univariate analysis demonstrated that prognosis was significantly influenced by valve replacement (HR 0.39, 95% CI 0.24–0.62) and high N-terminal pro B-type natriuretic peptide (NT-proBNP) levels (>3 times the upper limit of normal) at the time of CHD diagnosis (HR 1.89 95% CI 1.04–3.43) [33•]. At multivariate analysis, valve replacement remained statistically significant as a prognostic factor (HR 0.30, 95% CI 0.16, 0.57) [33•].
Diagnosis
Presentation and Clinical Assessment
Cardiac symptoms are often subtle until CHD becomes advanced [32•]. This often results in a delay in the diagnosis of CHD [5]. Typically, symptoms include those of right-sided heart failure characterised by fatigue, peripheral oedema and exertional dyspnoea and eventually, cardiac cachexia may develop with progressive CHD. Left-sided heart failure may occur in about 10% of cases [5]. Physical examination lacks sensitivity in detecting valvular pathology and should not be relied upon for the diagnosis of CHD [32•]. Jugular vein distension and v waves due to tricuspid regurgitation may be present. Peripheral oedema, hepatomegaly and ascites may relate to right-sided heart failure. A systolic murmur (tricuspid regurgitation/pulmonary stenosis) and early diastolic murmur (pulmonary regurgitation) may be heard on auscultation [34]. Electrocardiography (ECG) is normal in 50% of cases or may reveal non-specific changes, such as low-voltage QRS complexes and right bundle branch block [5].
Biomarkers
5-HIAA
5-HIAA is a metabolite of serotonin which is usually measured in a 24-h urine sample or in plasma and provides a measure of the functionality of the tumour [35]. Multiple studies have shown that 5-HIAA levels are higher in patients with CHD (median urinary 5-HIAA levels 266-1,381 μmol/24h) than without (67.5–575 μmol/24h) [26, 36,37,38,39]. In addition, higher levels of 5-HIAA are associated with progression of CHD [30, 31] and increased mortality (7% with every 100 nmol/L increase) [26]. Bhattacharyya et al. showed that urinary 5-HIAA levels greater than 300 μmol/24h are associated with a two- to threefold increase in the risk of development or progression of CHD [40]. However, measurements of urinary 5-HIAA are limited by patient inconvenience and incorrect sampling, as well as food and drug intake [8••].
Natriuretic Peptides
NT-proBNP is a useful biomarker for screening patients with carcinoid syndrome. Bhattacharyya et al. showed that at a cut-off level of 260 pg/ml (31pmol/l) NT-proBNP has a sensitivity of 92% and specificity of 91% for the detection of CHD [41]. Using this approach, the number of patients screened to diagnose 1 case of CHD decreased from 5.1 to 1.4 [41]. Moreover, NT-proBNP levels correlate with disease progression and survival [42]. Atrial natriuretic peptide (ANP) plasma levels are also higher in patients with CHD than without [39] and are a reflection of cardiac dysfunction and heart failure, but this biomarker is not used in clinical practice.
Chromogranin A (CgA)
CgA is a glycoprotein secreted by NENs and a monoanalyte biomarker that is generally used to monitor disease status and recurrence, although it has several limitations [43]. It has been shown to be associated with CHD but is not suitable for screening purposes [44].
Activin A
Activin A is a member of the TGF family, which has been shown to be an independent predictor of CHD, although there was no significant difference in activin A levels noted between patients with early versus advanced disease. Activin A levels ≥0.34 ng/mL were found to have 87% sensitivity and 57% specificity for detecting CHD [45].
Imaging
Chest x-ray
Chest radiography is unhelpful in the majority of patients with CHD, as it is normal in about 50% of cases, and changes are often non-specific [5].
Echocardiography
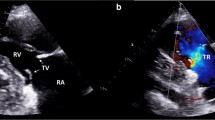
Two-dimensional transthoracic echocardiography (TTE) remains the key investigation for the diagnosis and follow-up of CHD. A wide spectrum of echocardiographic findings of CHD has been described [8••] and often 2D TTE reveals thickening of the tricuspid and pulmonary valve leaflets caused by fibrosis. This is associated with reduced excursion of the valves which are often seen to move in a ‘board-like’ pattern. The reduced mobility of the valves commonly leads to mixed pathology with regurgitation and stenosis [46]. The tricuspid valve is most commonly affected in CHD, and the presence of tricuspid regurgitation is typically associated with a characteristic ‘dagger-shaped’ spectrum on Doppler profile (early peak pressure rise with a subsequent rapid decline) [46]. The fibrous deposition in CHD can also affect the chordae and papillae, which can further impact on the functionality of the heart valves [46]. Although right-sided heart valves are most commonly affected in CHD, the left-sided heart valves can also be involved in up to 10% of cases [5]. Left-sided involvement is usually observed in 3 scenarios: in the presence of a PFO, high disease burden with production of large amounts of vasoactive substances and in primary lung NENs where hormonal substances are able to bypass lung metabolism and enter the left-sided heart chambers [46]. In addition to the detection of valvular abnormalities, 2D TTE may be useful for the assessment of alterations in ventricular strain and myocardial metastases, although masses smaller than 1 cm might be difficult to detect [46]. Agitated saline TTE is also used to detect PFO with early passage of contrast from the right side to the left [32•].
Advanced techniques in echocardiography, such as three-dimensional transthoracic echocardiography (3D TTE) and transoesophageal echocardiography (TOE), can be useful adjuncts in the assessment of CHD [46]. 3D TTE is helpful for the assessment of the tricuspid and pulmonary valves and offers the advantage of visualization of all valve leaflets at the same time, which may be important in cases where a single leaflet is involved [46]. It also allows for a detailed assessment of the subvalvular structures, such as the cordae and papillary muscles, as well as the identification of myocardial metastases with a more accurate estimation of the dimensions and mass effects compared with 2D TTE [46]. TOE may also be helpful in the assessment of the pulmonary valve and may elucidate subtle abnormalities of the tricuspid valve when TTE is equivocal. 3D TOE may sometimes be useful in the preoperative planning of patients that require valve replacement [46].
Cardiac Magnetic Resonance (CMR) and Cardiac CT Scanning
CMR may be useful in cases where TTE fails to provide adequate views of the pulmonary valve and can also provide a more accurate assessment of chamber sizes and function (such as evaluation of abnormal RV size and function in case of tricuspid regurgitation) [46]. It can also allow for identification of myocardial metastases, as well as metastatic spread to surrounding extracardiac structures [46].
Cardiac CT is also useful for the assessment of the degree of valvular damage, especially in cases of heavy calcification, as well as measurement of RV dimensions and evaluation of coronary arteries. It may have greater utility in preoperative planning. In addition, it can detect myocardial metastases [46]. A recent study from the Royal Free Hospital demonstrated the utility of cardiac CT in the evaluation of valvular abnormalities, myocardial metastases and assessment of coronary arteries in a cohort of 32 patients with CHD and concluded that this is a useful tool which should be part of the multimodal assessment of CHD especially in cases where surgical intervention is considered [47•]. Cardiac CT is also preferable to 3D TOE for the assessment of the pulmonary valve especially pre-operatively.
Positron Emission Tomography (PET)
Functional imaging with radiolabeled somatostatin analogues (typically Gallium-68-DOTATOC/DOTATATE PET/CT) utilises the ability of many NETs to overexpress somatostatin receptors. Therefore, these neoplasms and their metastases are often easily identifiable on PET scans. Carcinoid cardiac metastases (myocardiac and/or pericardial) may be detected by functional imaging studies, and this may be helpful in the evaluation of patients with CHD [47•].
Management
General Principles
A multidisciplinary approach is recommended for the management of patients with CHD [48]. The team should consist of cardiologists, oncologists, cardiovascular surgeons, radiologists, gastroenterologists, anaesthesiologists, GI and hepatobiliary surgeons, endocrinologists, nutritionists and clinical nurse specialists (Fig. 2). Management of these patients in an experienced, tertiary centre is necessary [48, 49]. A holistic approach is also important focusing on assessment of the nutritional needs and overall performance status, NET disease status, major organ function and the effects of CHD on the management of the underlying NET [8••]. The management of CHD in NET patients with carcinoid syndrome has been associated with a substantial economic burden [50].
Pharmacotherapy for Heart Failure
Loop or thiazide diuretics and aldosterone antagonists can be used for the symptomatic management of right heart failure associated with CHD [8••]. There is no evidence for use of other standard therapies for heart failure, such as angiotensin-converting enzyme inhibitors, angiotensin-receptor antagonists or beta-blockers [32•]. Improvement in symptoms of heart failure with pharmacotherapy should not be considered as reassurance that management is effective and sufficient but rather should be used as a window to optimise and assess the patient for consideration of valve surgery, if appropriate [32•].
Management of Carcinoid Syndrome
The use of somatostatin analogues (SSA) is the mainstay therapy for the management of carcinoid syndrome. The long-acting SSAs octreotide LAR and lanreotide autogel are commonly used and have proven efficacy as antiproliferative therapies for NETs [51, 52]. Refractory symptoms can be managed with above-label doses of SSA, and short-acting octreotide subcutaneous injections can provide additional relief [32•]. If these measures are not sufficient, other options may include:
-
1.
Alfa-interferons, which may be effective in the control of carcinoid syndrome, but their use is limited by their side effect profile [32•]
-
2.
Telotristat ethyl, which is an inhibitor of tryptophan hydroxylase and thus reduces serotonin secretion. It has known efficacy in the reduction of diarrhoea associated with carcinoid syndrome and urinary 5-HIAA levels [53], but there is no evidence that it can cause regression or prevent progression of CHD
-
3.
Peptide receptor radionuclide therapy (PRRT) is mainly used as an effective therapy for growth control in progressive NETs with high somatostatin receptor expression [54] but has also been shown to improve quality of life and diarrhoea in patients with midgut NETs [55]. Caution is needed in patients with CHD and heart failure due to the need for concomitant amino acid and fluid infusions [8••], although a recent study from Kings College Hospital suggested that PRRT can be safely given before or after valve surgery in patients with CHD [56]
-
4.
Trans-arterial embolisation (TAE) can be used with caution in patients with CHD and often may be performed in stages with anaesthetic cover and recovery in HDU/ITU [32•]
-
5.
Surgical cytoreduction can be used for the management of carcinoid syndrome. However, the risk of morbidity and mortality in patients with CHD may preclude this treatment, since high right heart pressures may increase the risk of intra-operative bleeding in liver surgery [32•]
Surgery for CHD
The main indications for surgical intervention in CHD include severe symptomatic valve regurgitation/stenosis (fatigue, symptoms of right heart failure) or progressive asymptomatic right ventricular enlargement or dysfunction [8••]. Fewer patients undergo surgery prior to planned hepatic surgery as a curative resection or palliative intervention [8••]. Generally, only patients with a life expectancy of over 12 months are considered for surgery [32•]. A recent retrospective study from the Erasmus MC revealed that tricuspid valve replacement for CHD has evolved into the most frequent indication for tricuspid valve surgery in the last two decades [57].
Clinical Outcomes
Earlier studies reported a significant perioperative mortality which was usually over 10% [32•], but more recently, the 30-day mortality for surgical intervention has been estimated at about 5% in expert centres [58]. This improvement is probably multifactorial and may be a reflection of careful patient selection with a focus on early intervention, improved overall surgical management, centralised care and increased surgical experience in expert centres with a high volume of cases [58]. Late survival however appears to be limited by NET disease progression, and a recent retrospective analysis from the Mayo clinic reported overall survival estimates at 1, 3 and 5 years of 69%, 48% and 34%, respectively [32, 58].
Valve Surgery
Surgery consists of replacement of any valve with severe regurgitation or stenosis together with closure of PFO, if present. Sometimes, moderately affected valves may also be replaced at the same time given the unpredictable course of CHD and risk of progression of fibrotic changes in moderately diseased valves if they are left in situ [32•]. Bioprosthetic valves are usually the preferred option, as patients can avoid long-term anticoagulation and are at lower risk of thrombosis [32•]. In addition, a significant proportion of patients with operated carcinoid heart disease will require additional non-cardiac interventions which could be complicated by perioperative management of mechanical valve prostheses. The durability of bioprosthetic valves is usually longer than the expected survival of these patients, and therefore, this is not generally an issue [32•]. Mechanical valves may be preferred in selected cases, such as in patients who need anticoagulation with warfarin for other reasons or patients with ovarian carcinoids who have a favourable prognosis after valve surgery and oophorectomy [58]. The number of valves replaced has not been found to be a risk factor for mortality [58], and in a small proportion of cases, all heart valves may need to be replaced [32•]. Coronary artery bypass grafting is also performed in a minority of cases with ischaemic heart disease, and removal of myocardial metastases may be required in selected cases [32•].
Peri-operative Management and Follow-up
The peri-operative management should be coordinated by an experienced multidisciplinary team [8••]. Patient admission is required for commencement of an octreotide infusion at a dosage of 50 μg/h administered 12 h before the procedure and continued throughout the operation and until the patient is haemodynamically stable and off inotropes [8••]. This is initiated to reduce the risk of carcinoid crisis, and the rate can be increased to 100–200 μg/h, if necessary [8••]. Following surgery, patients should be admitted to an intensive care unit and extubated as soon as clinically appropriate [32•]. Subsequently, they can be transferred to a cardiothoracic surgical ward, where they can receive physiotherapy and NET team assessment [32•].
In patients with bioprosthetic valves in sinus rhythm, anticoagulation with warfarin should be initiated and continued for 6 months, while patients with metallic heart valves or patients with bioprosthetic valves in atrial fibrillation should remain on anticoagulation indefinitely [32•]. A formal baseline echocardiogram is essential following surgery and should be performed within 6–8 weeks [32•]. Thereafter, clinical assessment and echocardiographic surveillance should be performed every 3–12 months depending on comorbidities [8••]. This surveillance strategy will assess for the risk of recurrent disease in the prosthetic valve, which is a rare occurrence, and the remaining native valves and also exclude the risk of valve thrombosis [32•]. An important consideration to reduce the risk of carcinoid recurrence in the prosthetic valve is the optimal control of carcinoid syndrome ensuring that urinary 5-HIAA levels remain lower than 300 μmol/l [8••].
Non-surgical Interventions
Percutaneous catheter-based interventions may be considered in high-risk patients with CHD who are not fit for surgery and have been successfully performed in selected cases [8••]. This minimally invasive option can also be used for closure of PFO [8••].
Conclusions
The presence of CHD is a poor prognostic factor in NET patients. Clinical presentation is often late and control of symptoms with careful fluid management and diuretics is necessary, but eventually, valve replacement is the only treatment that can improve outcome in patients with advanced CHD. Management of NET-CHD patients by an experienced multidisciplinary team within a centre of expertise is essential.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–42.
Modlin IM, Kidd M, Latich I, et al. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128(6):1717–51.
• Laskaratos FM, Rombouts K, Caplin M, et al. Neuroendocrine tumors and fibrosis: an unsolved mystery? Cancer. 2017;123(24):4770–90. https://doi.org/10.1002/cncr.31079This review article provides a comprehensive overview of the pathophysiology of fibrosis in neuroendocrine neoplasms.
Modlin IM, Shapiro MD, Kidd M. Carcinoid tumors and fibrosis: an association with no explanation. Am J Gastroenterol. 2004;99(12):2466–78. https://doi.org/10.1111/j.1572-0241.2004.40507.x.
Gustafsson BI, Hauso O, Drozdov I, et al. Carcinoid heart disease. Int J Cardiol. 2008;129(3):318–24. https://doi.org/10.1016/j.ijcard.2008.02.019.
Fox DJ, Khattar RS. Carcinoid heart disease: presentation, diagnosis, and management. Heart. 2004;90(10):1224–8. https://doi.org/10.1136/hrt.2004.040329.
Grozinsky-Glasberg S, Grossman AB, Gross DJ. Carcinoid Heart Disease: from pathophysiology to treatment--'something in the way it moves'. Neuroendocrinology. 2015;101(4):263–73. https://doi.org/10.1159/000381930.
•• Davar J, Connolly HM, Caplin ME, et al. Diagnosing and managing carcinoid heart disease in patients with neuroendocrine tumors: an expert statement. J Am Coll Cardiol. 2017;69:1288–304 This review is an expert statement that provides a comprehensive overview of the management of carcinoid heart disease.
Møller JE, Pellikka PA, Bernheim AM, et al. Prognosis of carcinoid heart disease: analysis of 200 cases over two decades. Circulation. 2005;112:3320–7.
Antonini A, Poewe W. Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson’s disease. Lancet Neurol. 2007;6(9):826–9. https://doi.org/10.1016/S1474-4422(07)70218-1.
Connolly HM, Crary JL, McGoon MD, et al. Valvular heart disease associated with fenfluramine-phentermine. N Engl J Med. 1997;337(9):581–8. https://doi.org/10.1056/NEJM199708283370901.
Horvath J, Fross RD, Kleiner-Fisman G, et al. Severe multivalvular heart disease: a new complication of the ergot derivative dopamine agonists. Mov Disord. 2004;19(6):656–62. https://doi.org/10.1002/mds.20201.
Mason JW, Billingham ME, Friedman JP. Methysergide-induced heart disease: a case of multivalvular and myocardial fibrosis. Circulation. 1977;56(5):889–90.
Roth BL. Drugs and valvular heart disease. N Engl J Med. 2007;356(1):6–9. https://doi.org/10.1056/NEJMp068265.
Rothman RB, Baumann MH, Savage JE, et al. Evidence for possible involvement of 5-HT(2B) receptors in the cardiac valvulopathy associated with fenfluramine and other serotonergic medications. Circulation. 2000;102(23):2836–41.
Zanettini R, Antonini A, Gatto G, et al. Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med. 2007;356(1):39–46. https://doi.org/10.1056/NEJMoa054830.
Fitzgerald LW, Burn TC, Brown BS, et al. Possible role of valvular serotonin 5-HT(2B) receptors in the cardiopathy associated with fenfluramine. Mol Pharmacol. 2000;57(1):75–81.
Setola V, Hufeisen SJ, Grande-Allen KJ, et al. 3,4-methylenedioxymethamphetamine (MDMA, “Ecstasy”) induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro. Mol Pharmacol. 2003;63(6):1223–9. https://doi.org/10.1124/mol.63.6.1223.
Nebigil CG, Hickel P, Messaddeq N, et al. Ablation of serotonin 5-HT(2B) receptors in mice leads to abnormal cardiac structure and function. Circulation. 2001;103(24):2973–9.
Nebigil CG, Jaffre F, Messaddeq N, et al. Overexpression of the serotonin 5-HT2B receptor in heart leads to abnormal mitochondrial function and cardiac hypertrophy. Circulation. 2003;107(25):3223–9. https://doi.org/10.1161/01.CIR.0000074224.57016.01.
Pena-Silva RA, Miller JD, Chu Y, Heistad DD. Serotonin produces monoamine oxidase-dependent oxidative stress in human heart valves. Am J Physiol Heart Circ Physiol. 2009;297(4):H1354–60. https://doi.org/10.1152/ajpheart.00570.2009.
Miller JD, Chu Y, Brooks RM, et al. Dysregulation of antioxidant mechanisms contributes to increased oxidative stress in calcific aortic valvular stenosis in humans. J Am Coll Cardiol. 2008;52(10):843–50. https://doi.org/10.1016/j.jacc.2008.05.043.
Meng XM, Nikolic-Paterson DJ, Lan HY. TGF-beta: the master regulator of fibrosis. Nat Rev Nephrol. 2016;12(6):325–38. https://doi.org/10.1038/nrneph.2016.48.
Jian B, Xu J, Connolly J, et al. Serotonin mechanisms in heart valve disease I: serotonin-induced up-regulation of transforming growth factor-beta1 via G-protein signal transduction in aortic valve interstitial cells. Am J Pathol. 2002;161(6):2111–21.
Bhattacharyya S, Toumpanakis C, Caplin ME, Davar J. Analysis of 150 patients with carcinoid syndrome seen in a single year at one institution in the first decade of the twenty-first century. Am J Cardiol. 2008;101:378–81.
Buchanan-Hughes A, Pashley A, Feuilly M, et al. Carcinoid heart disease: prognostic value of 5- hydroxyindoleacetic acid levels and impact on survival - a systematic literature review. Neuroendocrinology. 2020.
Pellikka PA, Tajik AJ, Khandheria BK, et al. Carcinoid heart disease. Clinical and echocardiographic spectrum in 74 patients. Circulation. 1993;87(4):1188–96.
De Jesus T, Luis SA, Ryu JH, et al. Carcinoid heart disease in patients with bronchopulmonary carcinoid. J Thorac Oncol. 2018;13:1602–5.
Westberg G, Wangberg B, Ahlman H, et al. Prediction of prognosis by echocardiography in patients with midgut carcinoid syndrome. Br J Surg. 2001;88(6):865–72. https://doi.org/10.1046/j.0007-1323.2001.01798.x.
Denney WD, Kemp WE Jr, Anthony LB, et al. Echocardiographic and biochemical evaluation of the development and progression of carcinoid heart disease. J Am Coll Cardiol. 1998;32(4):1017–22.
Moller JE, Connolly HM, Rubin J, et al. Factors associated with progression of carcinoid heart disease. N Engl J Med. 2003;348(11):1005–15. https://doi.org/10.1056/NEJMoa021451.
• Steeds RP, Sagar V, Shetty S, et al. Multidisciplinary team management of carcinoid heart disease. Endocr Connect. 2019;8:R184–r199 An interesting review article on the multidisciplinary management of carcinoid heart disease.
• Spada F, Laskaratos F, Crona J, Oleinikov K, Zandee W, Lamarca A, Alonso Gordoa T, Frassoni S, Munir A, Liu M, Panero A, Öberg K. A retrospective multicentre evaluation of the outcomes and management of carcinoid heart disease in patients with advanced midgut NETs: a NET-CONNECT Descriptive Study. Neuroendocrinology 2020; 110. A multicentre study on clinical outcomes of patients with carcinoid heart disease over the last decade.
Bhattacharyya S, Davar J, Dreyfus G, Caplin ME. Carcinoid heart disease. Circulation. 2007;116:2860–5.
Hart EA, Meijs TA, Meijer RCA, et al. Carcinoid heart disease: a guide for screening and timing of surgical intervention. Neth Hear J. 2017;25:471–8.
Ross EM, Roberts WC. The carcinoid syndrome: comparison of 21 necropsy subjects with carcinoid heart disease to 15 necropsy subjects without carcinoid heart disease. Am J Med. 1985;79(3):339–54.
Himelman RB, Schiller NB. Clinical and echocardiographic comparison of patients with the carcinoid syndrome with and without carcinoid heart disease. Am J Cardiol. 1989;63(5):347–52.
Robiolio PA, Rigolin VH, Wilson JS, et al. Carcinoid heart disease. Correlation of high serotonin levels with valvular abnormalities detected by cardiac catheterization and echocardiography. Circulation. 1995;92(4):790–5.
Zuetenhorst JM, Bonfrer JM, Korse CM, et al. Carcinoid heart disease: the role of urinary 5-hydroxyindoleacetic acid excretion and plasma levels of atrial natriuretic peptide, transforming growth factor-beta and fibroblast growth factor. Cancer. 2003;97(7):1609–15. https://doi.org/10.1002/cncr.11226.
Bhattacharyya S, Toumpanakis C, Chilkunda D, et al. Risk factors for the development and progression of carcinoid heart disease. Am J Cardiol. 2011;107:1221–6.
Bhattacharyya S, Toumpanakis C, Caplin ME, Davar J. Usefulness of N-terminal pro-brain natriuretic peptide as a biomarker of the presence of carcinoid heart disease. Am J Cardiol. 2008;102:938–42.
Dobson R, Burgess MI, Valle JW, et al. Serial surveillance of carcinoid heart disease: factors associated with echocardiographic progression and mortality. Br J Cancer. 2014;111:1703–9.
Kidd M, Bodei L, Modlin IM. Chromogranin A: any relevance in neuroendocrine tumors? Curr Opin Endocrinol Diabetes Obes. 2016;23:28–37.
Korse CM, Taal BG, de Groot CA, et al. Chromogranin-A and N-terminal pro-brain natriuretic peptide: an excellent pair of biomarkers for diagnostics in patients with neuroendocrine tumor. J Clin Oncol. 2009;27:4293–9.
Bergestuen DS, Edvardsen T, Aakhus S, et al. Activin A in carcinoid heart disease: a possible role in diagnosis and pathogenesis. Neuroendocrinology. 2010;92(3):168–77. https://doi.org/10.1159/000318014.
Agha AM, Lopez-Mattei J, Donisan T, et al. Multimodality imaging in carcinoid heart disease. Open Heart. 2019;6:e001060.
• Davar J LO, Caplin M, Toumpanakis C. Features of carcinoid heart disease identified by cardiac computed tomography. J Cardiovasc Comp Tomogr 2020; In press. A recent study on the role of cardiac CT as an imaging modality for the diagnosis and management of carcinoid heart disease.
Askew JW, Connolly HM. Carcinoid valve disease. Curr Treat Options Cardiovasc Med. 2013;15:544–55.
Laskaratos FM, Caplin M. Treatment challenges in and outside a network setting: gastrointestinal neuroendocrine tumours. Eur J Surg Oncol. 2019;45(1):52–9. https://doi.org/10.1016/j.ejso.2018.03.012.
Joish VN, Perez-Olle R, Lapuerta P, et al. Burden of carcinoid heart disease in patients with carcinoid syndrome initiating somatostatin analogues. Clin Ther. 2019;41:1716–1723.e1712.
Caplin ME, Pavel M, Ćwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371:224–33.
Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27:4656–63.
Pavel M, Gross DJ, Benavent M, et al. Telotristat ethyl in carcinoid syndrome: safety and efficacy in the TELECAST phase 3 trial. Endocr Relat Cancer. 2018;25:309–22.
Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 Trial of (177)Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Strosberg J, Wolin E, Chasen B, et al. Health-related quality of life in patients with progressive midgut neuroendocrine tumors treated with (177)Lu-dotatate in the phase III NETTER-1 trial. J Clin Oncol. 2018;36:2578–84.
Davis LM, Nicou N, Martin W, et al. Timing of peptide receptor radiotargeted therapy in relation to cardiac valve surgery for carcinoid heart disease in patients with neuroendocrine metastases and cardiac syndrome. A single-centre study from a centre of excellence. Nucl Med Commun. 2020;41:575–81.
Veen KM, Quanjel TJM, Mokhles MM, et al. Tricuspid valve replacement: an appraisal of 45 years of experience. Interact Cardiovasc Thorac Surg. 2020;30:896–903.
Nguyen A, Schaff HV, Abel MD, et al. Improving outcome of valve replacement for carcinoid heart disease. J Thorac Cardiovasc Surg. 2019;158:99–107.e102.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Conflict of Interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuroendocrine Neoplasms
Rights and permissions
About this article
Cite this article
Laskaratos, FM., Davar, J. & Toumpanakis, C. Carcinoid Heart Disease: a Review. Curr Oncol Rep 23, 48 (2021). https://doi.org/10.1007/s11912-021-01031-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01031-z