Abstract
While there is an ongoing debate regarding the timing of the maximal surgical effort in epithelial ovarian cancer, it is well established that patients with suboptimal tumor debulking derive no benefit from the surgical procedure. The amount of residual disease after cytoreductive surgery has been repeatedly identified as a strong predictor of survival, and accordingly, the surgical effort to achieve the goal of complete gross tumor resection has been constantly evolving. Centers that have adopted the concept of radical surgery in patients with advanced ovarian cancer have reported improvements in their patients’ survival. In addition to the expected improvements in the pharmacologic treatment of this disease, some of the next challenges in the surgical management of ovarian cancer include the preoperative prediction of suboptimal debulking, improving the drug delivery to the tumor, and increasing access to centers of excellence in ovarian cancer regardless of geographical, financial, or other social barriers. This review will discuss an update on the role of surgery in the treatment of primary epithelial ovarian cancer as it has evolved since the emergence of the concept of surgical cytoreduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the second most common gynecological malignancy in the USA and the most deadly with an estimated 21,980 new cases and 14,270 deaths in 2014 [1]. The current standard of care for advanced ovarian cancer is a combination of cytoreductive surgery and platinum-based chemotherapy [2]. The amount of residual disease after cytoreductive surgery has been repeatedly identified as a strong predictor of survival, and accordingly, the surgical effort to achieve the goal of complete gross tumor resection has been constantly evolving [3]. Notwithstanding the ongoing debate regarding the timing of the maximal surgical effort (primary vs following neoadjuvant chemotherapy), the goal of cytoreductive surgery remains the same [4]. This review will discuss the role of surgery in the treatment of primary epithelial ovarian cancer as it has evolved since the emergence of the concept of surgical cytoreduction [5].
Concept and Evidence
The theoretical benefits of debulking surgery include removal of poorly vascularized tumor where chemotherapeutic agents have poor access as well as the removal of chemoresistant clones leaving behind smaller residual implants with a higher growth fraction which are more susceptible to chemotherapy [6].
Following the seminal report by Griffiths in 1975 [5], overwhelming evidence from multiple institutional retrospective series and pooled data from prospective randomized chemotherapy trials have confirmed the role of cytoreductive surgery in prolonging survival, and the goal of surgery has evolved from optimal tumor residual of <2 cm to a goal of no gross residual disease [7–17]. In the EORTC randomized controlled trial comparing neoadjuvant chemotherapy vs primary surgery, complete gross resection of all macroscopic disease was the strongest independent variable in predicting overall survival, whether the surgery was performed primarily or following neoadjuvant chemotherapy [4].
As the concept of cytoreduction became widely accepted, the extent of surgery required to achieve the desired goal increased accordingly. A legitimate question addressed whether the morbidity and to a lesser degree the mortality associated with major debulking procedures in patients with extensive intra-abdominal disease, negated the benefit hoped for with surgical cytoreduction. Commonly advanced arguments in that regard question whether the potentially debilitated state of some of those patients will lead to a delay in receiving adjuvant chemotherapy and consequently lead to a worse outcome that could be attributed to the detrimental effect of surgery [18, 19]. However, in the reported institutional series, the morbidity associated with major debulking procedures was not associated with a decrease in survival, and it has been a constant finding that institutions that adopted a paradigm shift in their surgical philosophy have observed an improvement in the survival of their patients [10, 16, 20].
Radical Surgery
The extent of surgery performed at the time of primary cytoreductive surgery depends on the location and extent of disease, surgeon and medical center expertise, and the patient’s general condition and comorbidities. The rate of optimal cytoreduction in different national and international centers ranges from less than 25 % to more than 75 % [7]. Historically, disease in the upper abdomen (the diaphragm, liver, and porta hepatis, spleen), rectosigmoid, and extra-abdominal disease were regarded as unresectable disease. However, current surgical practice has demonstrated that, in appropriately selected patients [21], most of these disease locations are amenable to cytoreduction with an associated improvement in patient outcomes, and with manageable patient morbidity [21, 22].
Colon and Small Intestine
Tumor implants involving the intestinal serosa superficially or the small intestine mesentery focally can be readily excised or ablated. However, when the tumor penetrates deeper in the intestinal wall, or in cases of diffuse infiltration of the mesentery, intestinal resection becomes necessary. Intestinal resection is one of the most common procedures required to remove bulky disease in advanced ovarian cancer and is performed in up to 50 % of optimal cytoreductive operations [23].
The rectosigmoid colon is the intestinal segment most frequently resected during cytoreductive surgery as it is commonly involved in advanced ovarian cancer. Bulky disease involving the cul-de-sac and/or rectosigmoid commonly requires modified posterior pelvic exenteration or an en-bloc resection of the uterus, adnexa, pelvic peritoneum, and rectosigmoid.
The distal ileum and cecum are another part of the intestines that are commonly affected, given their proximity to the right ovary. When involved, these can be resected en-bloc with the pelvic tumor or separately as deemed appropriate. The extent of resection of the ascending colon will depend on the location of disease and will range from a limited ilio-cecectomy to an extended right hemicolectomy.
Involvement of the transverse colon is typically due to bulky omental metastasis extending into the transverse colon itself and/or its mesentery. In the majority of cases of omental caking, a plane can be identified between the transverse colon and the omentum, avoiding the need for a transverse colon resection. However, at times, resection of the omentum en bloc with the transverse colon is necessary. Occasionally, extensive disease may involve the splenic hilum and tail of pancreas which necessitates an associated splenectomy and distal pancreatectomy. In case of extensive involvement of the entire colon, extended left colectomies and subtotal and total colectomies have also been described with acceptable results [24, 25].
When the small intestine is involved, segmental resections can be performed with low associated morbidity. Occasionally, extensive involvement of the mesentery of the small intestine may lead to aborting the cytoreductive procedure if the segment of small intestine to be resected will be large enough to lead to a short bowel syndrome.
Several reports have shown that intestinal resection at the time of cytoreductive surgery for advanced ovarian cancer facilitates optimal cytoreduction and improves survival with an acceptable complication rate [26–31]. The need to perform more than one intestinal resection to achieve optimal cytoreduction does not adversely affect patients’ survival and should not be viewed as an indication to abort the cytoreductive effort [32]. The reported rate of anastomotic leak associated with rectosigmoid resection ranged between 0.8 and 6.8 % in different series. Recent data from the Mayo clinic indicate an increased risk of anastomotic leak associated with the performance of multiple large bowel resections [33]. This complication may lead to a delay in the start of chemotherapy and may be associated with decreased survival [33]. Placement of a routine protective ostomy is not recommended routinely, however may be considered in circumstances known to be associated with a higher rate of anastomotic complications (multiple large bowel resections, previous radiation, very low anastomosis) [33].
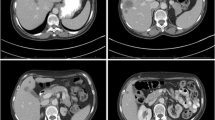
Upper Abdomen
In advanced ovarian cancer, tumor spread to the upper abdomen may involve, in different combinations for a given patient, the diaphragm (uni or bilaterally, superficially or involving the full thickness), the spleen and distal pancreas, the lesser sac, the liver (capsule or parenchyma), the gallbladder, the porta hepatis, the stomach, and the peritoneal surfaces surrounding all these areas. Upper abdominal disease is associated with a worse prognosis when compared to patients with disease limited to the pelvis [34].
Tumor spread to the upper abdomen was considered for a significant period of time as nonresectable disease and an indication for neoadjuvant chemotherapy. It is still a primary reason for suboptimal debulking in many contemporary centers. One reasonable explanation for this is that resection of disease in the upper abdomen requires surgical skills that are not part of the standard gynecologic oncology procedures, and multidisciplinary teams with special interest and expertise in oncologic surgery are essential. What may appear as overwhelming disease to the surgeon (regardless of specialty) with little exposure to ovarian cancer surgery (or other peritoneal surface malignancy surgery) may actually constitute a relatively common primary debulking case for the experienced team. Another commonly advanced argument for avoiding the resection of disease in the upper abdomen is that the morbidity associated with upper abdominal procedures as part of a cytoreduction surgery is likely to outweigh the benefits of an optimal or complete tumor resection. However, centers with interest and expertise in the surgical treatment of advanced ovarian cancer have expanded the frontier of primary debulking to the upper abdomen and provided evidence over the last decade from their single institutional experiences about the feasibility, the morbidity, and survival advantage associated with tumor debulking in the upper abdomen.
Common upper abdominal procedures performed for surgical cytoreduction include diaphragm peritonectomy or full-thickness resection, splenectomy with or without distal pancreatectomy, cholecystectomy, and resection of parenchymal liver disease and porta hepatis disease [35–39]. Once it was shown that resection of disease in these areas was surgically feasible, ensuing data demonstrated that although the morbidity associated with these procedures was significant (up to 22 %), a survival advantage was observed when compared to patients with suboptimal debulking. In the Memorial Sloan-Kettering series, patients with bulky upper abdominal disease who underwent optimal cytoreduction had a 28 % decreased risk of relapse and a 33 % decreased risk of death compared to patients who underwent suboptimal cytoreduction [22, 40, 41].
Chest
When advanced ovarian cancer spreads to the chest, it is most commonly identified on preoperative imaging as either enlarged mediastinal nodes or as pleural effusions with or without associated pleural tumor implants. Video-assisted thoracic surgery (VATS) performs better than CT for evaluating pleural tumor implants. Macroscopic pleural disease was identified by VATS in 50–69 % of patients with a moderate to large pleural effusion of which 33–73 % had lesions >1 cm. Even among patients with cytology negative pleural effusion, 36 % were found to have macroscopic disease [42–46]. Presence of moderate to large pleural effusion on imaging is independently associated with poorer overall survival in advanced ovarian cancer. Even for optimally cytoreduced patients, the median survival was lower for patients with stage IV cytology proven malignant pleural effusion as compared to stage III [47, 48]. In addition to its diagnostic role, VATS can be used to resect pleural and mediastinal disease. Another surgical approach involves transdiaphragmatic resection of pleural and mediastinal disease during an abdominal debulking procedure.
The effect of intrathoracic debulking on patient survival is unknown at this time [44]. The feasibility of intrathoracic debulking is counterbalanced by the argument that ovarian cancer recurrences in the chest uncommonly occur in isolation and are rarely a cause of patients’ death [49, 50]. At this time, and until additional data is available, an acceptable approach involves performing a VATS on all patients with moderate to large pleural effusions. In case unresectable gross disease is identified in the chest, the patient is referred for neoadjuvant chemotherapy. In the presence of disease amenable to surgical resection, intrathoracic debulking is done, followed by intra-abdominal debulking either during the same surgery or at a different time, depending on the amount of disease in the chest and in the abdomen and the overall condition of the patient [44].
Moving Forward
In the last decade, the experience of many centers has been published demonstrating that surgical removal of all gross disease is feasible in the majority of cases, regardless of the initial tumor burden.
It is hoped that the identification of new pharmacologic agents will be able at some point to eradicate more permanently residual microscopic disease and provide prolonged survivals and ultimately cure from this disease. Concurrently, additional advances in the surgical management of ovarian cancer are hoped to contribute to an improvement in outcomes of patients with advanced disease.
Predicting Suboptimal Debulking
Patients with suboptimal tumor debulking derive no benefit from the surgical procedure and are only exposed to its complications. Predicting which patients are likely to have an unresectable tumor will allow the timely referral of these patients to neoadjuvant chemotherapy and will avoid the potential complications of an unnecessary surgery. Preoperative imaging, tumor markers, and laparoscopic scores have been used in different combinations in the past [51•]. No reproducible and reliable model has been uniformly validated and adopted. A recently published prospective multicenter trial evaluating the combination of preoperative CT and serum CA-125 has identified three clinical and six radiologic predictive variables which were used to create a mathematical model that can predict the probability of suboptimal debulking [51•]. Despite the potential utility of this model, no universal threshold can be recommended at this time for which to mandate direct referral to neoadjuvant chemotherapy, as this will depend on the individual surgeon and the context in which he practices.
Improving Drug Delivery to the Tumor: Hyperthermic Intraperitoneal Chemotherapry (HIPEC)
Intraperitoneal chemotherapy has been part of the standard recommended adjuvant chemotherapy regimen in patients with optimal or complete cytoreduction of advanced ovarian cancer, since the publication of the results of GOG 172 in 2006 [2]. Preclinical models have also demonstrated that hyperthermia is tumoricidal and can increase the cytotoxic effect of many chemotherapy agents [52–54]. The rationale for HIPEC is therefore to combine the local delivery of the drug with hyperthermia in order to improve outcomes. HIPEC is administered in the operating room at the end of the cytoreductive procedure. The intraoperative administration allows to overcome the technical difficulties encountered in the outpatient setting related to port malfunction or secondary to the formation of abdominal adhesions preventing the uniform distribution of the drug. Although multiple mostly single institution experiences have been published [55], it is important to evaluate this modality through prospective rigorous clinical trials [56•]. At this time, there is no prospective data demonstrating and quantifying the clinical benefit of this treatment modality, or the optimal agents and doses to use, whether in the primary or the recurrent setting [54]. The results of several ongoing trials are awaited to answer these questions.
Access to Care
As discussed above, the cornerstone of management of ovarian cancer involves the combination of a maximal surgical effort and combination chemotherapy that includes an intraperitoneal component when appropriate. Both components require a high level of expertise and can only be provided in centers with the appropriate surgical, medical, and nursing resources. At the same time that new drugs and drug delivery options continue to be developed, it is important to ensure that all patients with ovarian cancer can overcome geographical, social, and economical barriers to have access to the current standard treatment modalities that have been shown to provide improved outcomes [57••]. As proposed by Bristow et al., in the USA, transplant surgery offers a template on how regionalization of care can create a model where care is only provided by approved centers. The adoption of a similar centralized system for ovarian cancer will likely be associated with a more efficient delivery of the appropriate care, a more efficient process to enroll patients in clinical trials, and ultimately, this would translate into improved outcomes.
Conclusion
Primary debulking surgery followed by adjuvant chemotherapy is the cornerstone for the management of advanced ovarian cancer. Once the decision has been made to perform cytoreductive surgery, the goal of cytoreductive surgery should be to achieve maximal cytoreduction, as each incremental decrease in residual disease below 1 cm is associated with an incremental improvement in overall survival. However, an aggressive surgical approach may result in increased morbidity, which may have a negative impact on the oncologic outcome. Patients with poor performance status and unresectable disease are candidates for neoadjuvant chemotherapy. Currently, there are no uniformly validated and accepted preoperative selection criteria for immediate referral to neoadjuvant chemotherapy as compared to surgical exploration. Current practices vary depending on the individual surgeon and the context in which he practices. A promising new strategy is the combination of maximal cytoreductive effort and HIPEC. Access to care in centers of excellence in ovarian cancer for all patients with ovarian cancer should be a priority for national organizations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29.
Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354(1):34–43.
Chang SJ, Bristow RE. Evolution of surgical treatment paradigms for advanced-stage ovarian cancer: redefining ‘optimal’ residual disease. Gynecol Oncol. 2012;125(2):483–92.
Vergote I, Tropé CG, Amant F, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363(10):943–53.
Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr. 1975;42:101–4.
Covens AL. A critique of surgical cytoreduction in advanced ovarian cancer. Gynecol Oncol. 2000;78(3 Pt 1):269–74.
Hoskins WJ, McGuire WP, Brady MF, et al. The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol. 1994;170:974–9.
Eisenkop SM, Spirtos NM. What are the current surgical objectives, strategies, and technical capabilities of gynecologic oncologists treating advanced epithelial ovarian cancer? Gynecol Oncol. 2001;82(3):489–97.
Chi DS, Eisenhauer EL, Lang J, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol. 2006;103(2):559–64.
Aletti GD, Dowdy SC, Gostout BS, et al. Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol. 2006;107(1):77–85.
Winter 3rd WE, Maxwell GL, Tian C, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25(24):3621–7.
Du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115(6):1234–44.
Peiretti M, Zanagnolo V, Aletti GD, et al. Role of maximal primary cytoreductive surgery in patients with advanced epithelial ovarian and tubal cancer: Surgical and oncological outcomes. Single institution experience. Gynecol Oncol. 2010;119(2):259–64.
Kommoss S, Rochon J, Harter P, et al. Prognostic impact of additional extended surgical procedures in advanced-stage primary ovarian cancer. Ann Surg Oncol. 2010;17(1):279–86.
Wimberger P, Wehling M, Lehmann N, et al. Influence of residual tumor on outcome in ovarian cancer patients with FIGO stage IV disease: an exploratory analysis of the AGO-OVAR (Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group). Ann Surg Oncol. 2010;17(6):1642–8.
Harter P, Muallem ZM, Buhrmann C, et al. Impact of a structured quality management program on surgical outcome in primary advanced ovarian cancer. Gynecol Oncol. 2011;121(3):615–9.
Chang SJ, Bristow RE, Ryu HS. Impact of complete cytoreduction leaving no gross residual disease associated with radical cytoreductive surgical procedures on survival in advanced ovarian cancer. Ann Surg Oncol. 2012;19(13):4059–67.
Wright JD, Lewin SN, Deutsch I, et al. Defining the limits of radical cytoreductive surgery for ovarian cancer. Gynecol Oncol. 2011;123(3):467–73.
Wright JD, Herzog TJ, Neugut AI, et al. Effect of radical cytoreductive surgery on omission and delay of chemotherapy for advanced-stage ovarian cancer. Obstet Gynecol. 2012;120(4):871–81.
Chi DS, Eisenhauer EL, Zivanovic O, et al. Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol. 2009;114(1):26–31.
Aletti GD, Eisenhauer EL, Santillan A, et al. Identification of patient groups at highest risk from traditional approach to ovarian cancer treatment. Gynecol Oncol. 2011;120(1):23–8.
Chi DS, Zivanovic O, Levinson KL, et al. The incidence of major complications after the performance of extensive upper abdominal surgical procedures during primary cytoreduction of advanced ovarian, tubal, and peritoneal carcinomas. Gynecol Oncol. 2010;119(1):38–42.
Hoffman MS, Zervose E. Colon resection for ovarian cancer: intraoperative decisions. Gynecol Oncol. 2008;111(2 Suppl):S56–65.
Silver DF, Bou ZN. Extended left colon resections as part of complete cytoreduction for ovarian cancer: tips and considerations. Gynecol Oncol. 2009;114(3):427–30.
Song YJ, Lim MC, Kang S, et al. Total colectomy as part of primary cytoreductive surgery in advanced Müllerian cancer. Gynecol Oncol. 2009;114(2):183–7.
Shimada M, Kigawa J, Minagawa Y, Irie T, et al. Significance of cytoreductive surgery including bowel resection for patients with advanced ovarian cancer. Am J Clin Oncol. 1999;22(5):481–4.
Mourton SM, Temple LK, Abu-Rustum NR, et al. Morbidity of rectosigmoid resection and primary anastomosis in patients undergoing primary cytoreductive surgery for advanced epithelial ovarian cancer. Gynecol Oncol. 2005;99(3):608–14.
Estes JM, Leath 3rd CA, Straughn Jr JM, et al. Bowel resection at the time of primary debulking for epithelial ovarian carcinoma: outcomes in patients treated with platinum and taxane-based chemotherapy. J Am Coll Surg. 2006;203(4):527–32.
Aletti GD, Podratz KC, Jones MB, et al. Role of rectosigmoidectomy and stripping of pelvic peritoneum in outcomes of patients with advanced ovarian cancer. J Am Coll Surg. 2006;203(4):521–6.
Tebes SJ, Cardosi R, Hoffman MS. Colorectal resection in patients with ovarian and primary peritoneal carcinoma. Am J Obstet Gynecol. 2006;195(2):585–9.
Park JY, Seo SS, Kang S, et al. The benefits of low anterior en bloc resection as part of cytoreductive surgery for advanced primary and recurrent epithelial ovarian cancer patients outweigh morbidity concerns. Gynecol Oncol. 2006;103(3):977–84.
Salani R, Zahurak ML, Santillan A, et al. Survival impact of multiple bowel resections in patients undergoing primary cytoreductive surgery for advanced ovarian cancer: a case-control study. Gynecol Oncol. 2007;107(3):495–9.
Kalogera E, Dowdy SC, Mariani A, et al. Multiple large bowel resections: potential risk factor for anastomotic leak. Gynecol Oncol. 2013;130(1):213–8.
Hamilton CA, Miller A, Miller C, et al. The impact of disease distribution on survival in patients with stage III epithelial ovarian cancer cytoreduced to microscopic residual: a Gynecologic Oncology Group study. Gynecol Oncol. 2011;122(3):521–6.
Cliby W, Dowdy S, Feitoza SS, et al. Diaphragm resection for ovarian cancer: technique and short-term complications. Gynecol Oncol. 2004;94(3):655–60.
Eisenkop SM, Spirtos NM, Lin WC. Splenectomy in the context of primary cytoreductive operations for advanced epithelial ovarian cancer. Gynecol Oncol. 2006;100(2):344–8.
Magtibay PM, Adams PB, Silverman MB, et al. Splenectomy as part of cytoreductive surgery in ovarian cancer. Gynecol Oncol. 2006;102(2):369–74.
Dowdy SC, Loewen RT, Aletti G, et al. Assessment of outcomes and morbidity following diaphragmatic peritonectomy for women with ovarian carcinoma. Gynecol Oncol. 2008;109(2):303–7.
Martinez A, Pomel C, Mery E, et al. Celiac lymph node resection and porta hepatis disease resection in advanced or recurrent epithelial ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol. 2011;121(2):258–63.
Eisenhauer EL, Abu-Rustum NR, Sonoda Y, et al. The addition of extensive upper abdominal surgery to achieve optimal cytoreduction improves survival in patients with stages IIIC-IV epithelial ovarian cancer. Gynecol Oncol. 2006;103(3):1083–90.
Zivanovic O, Sima CS, Iasonos A, et al. The effect of primary cytoreduction on outcomes of patients with FIGO stage IIIC ovarian cancer stratified by the initial tumor burden in the upper abdomen cephalad to the greater omentum. Gynecol Oncol. 2010;116(3):351–7.
Juretzka MM, Abu-Rustum NR, Sonoda Y, et al. The impact of video-assisted thoracic surgery (VATS) in patients with suspected advanced ovarian malignancies and pleural effusions. Gynecol Oncol. 2007;104(3):670–4.
Cohen-Mouly S, Badia A, Bats AS, et al. Role of video-assisted thoracoscopy in patients with ovarian cancer and pleural effusion. Int J Gynecol Cancer. 2009;19(9):1662–5.
Diaz JP, Abu-Rustum NR, Sonoda Y, et al. Video-assisted thoracic surgery (VATS) evaluation of pleural effusions in patients with newly diagnosed advanced ovarian carcinoma can influence the primary management choice for these patients. Gynecol Oncol. 2010;116(3):483–8.
Mironov O, Sala E, Mironov S, et al. Thoracic metastasis in advanced ovarian cancer: comparison between computed tomography and video-assisted thoracic surgery. J Gynecol Oncol. 2011;22(4):260–8.
Klar M, Farthmann J, Bossart M, et al. Video-assisted thoracic surgery (VATS) evaluation of intrathoracic disease in patients with FIGO III and IV stage ovarian cancer. Gynecol Oncol. 2012;126(3):397–402.
Eitan R, Levine DA, Abu-Rustum N, et al. The clinical significance of malignant pleural effusions in patients with optimally debulked ovarian carcinoma. Cancer. 2005;103(7):1397–401.
Mironov O, Ishill NM, Mironov S, et al. Pleural effusion detected at CT prior to primary cytoreduction for stage III or IV ovarian carcinoma: effect on survival. Radiology. 2011;258(3):776–84.
Aletti GD, Podratz KC, Cliby WA, et al. Stage IV ovarian cancer: disease site-specific rationale for postoperative treatment. Gynecol Oncol. 2009;112(1):22–7.
Perri T, Ben-Baruch G, Kalfon S, et al. Abdominopelvic cytoreduction rates and recurrence sites in stage IV ovarian cancer: is there a case for thoracic cytoreduction? Gynecol Oncol. 2013;131(1):27–31.
Suidan RS, Ramirez PT, Sarasohn DM, et al. A multicenter prospective trial evaluating the ability of preoperative computed tomography scan and serum CA-125 to predict suboptimal cytoreduction at primary debulking surgery for advanced ovarian, fallopian tube, and peritoneal cancer. Gynecol Oncol. 2014;134(3):455–61. Efforts to try to predict preoperatively surgical outcome may allow avoiding unnecessary surgery in patients with high likelihood of suboptimal debulking.
Giovanella BC, Stehlin Jr JS, Morgan AC. Selective lethal effect of supranormal temperatures on human neoplastic cells. Cancer Res. 1976;36:3944–50.
Engin K. Biological rationale for hyperthermia in cancer treatment (II). Neoplasma. 1994;41(5):277–83.
Pölcher M, Zivanovic O, Chi DS. Cytoreductive surgery for advanced ovarian cancer. Womens Health. 2014;10(2):179–90.
Chua TC, Robertson G, Liauw W, et al. Intraoperative hyperthermic intraperitoneal chemotherapy after cytoreductive surgery in ovarian cancer peritoneal carcinomatosis: systematic review of current results. J Cancer Res Clin Oncol. 2009;135:1637–45.
Zivanovic O, Abramian A, Kullmann M, et al. HIPEC ROC I: a phase i study of cisplatin administered as hyperthermic intraoperative intraperitoneal chemoperfusion followed by postoperative intravenous platinum-based chemotherapy in patients with platinum-sensitive recurrent epithelial ovarian cancer. Int J Cancer. 2015;136(3):699–708. It is important to study HIPEC in the setting of well designed clinical trials and not extrapolate from heterogeneous single institution retrospective series.
Bristow RE, Chang J, Ziogas A, et al. High-volume ovarian cancer care: survival impact and disparities in access for advanced-stage disease. Gynecol Oncol. 2014;132(2):403–10. It is important to study and remove the barriers to access appropriate surgical care for ovarian cancer at the time as we continue to improve that standard.
Compliance with Ethics Guidelines
Conflict of Interest
Deepa Maheswari Narasimhulu, Fady Khoury-Collado, and Dennis S. Chi declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Gynecologic Cancers.
Rights and permissions
About this article
Cite this article
Narasimhulu, D.M., Khoury-Collado, F. & Chi, D.S. Radical Surgery in Ovarian Cancer. Curr Oncol Rep 17, 16 (2015). https://doi.org/10.1007/s11912-015-0439-z
Published:
DOI: https://doi.org/10.1007/s11912-015-0439-z