Abstract
Purpose of Review
Attention-deficit/hyperactivity disorder (ADHD) is a heterogeneous and complex neurodevelopmental disorder related to disruptions in various neuronal structures and pathways, dopamine (DA) transporter, and receptor genes, resulting in cognitive and regulation deficits. This article reviews recent research on the biological mechanisms and markers, clinical manifestations, treatments, and outcomes of adult ADHD as well as current controversies within the field.
Recent Findings
New research identifies white matter disruptions in multiple cortical pathways in adults with ADHD. New treatments for ADHD in adults such as viloxazine ER have shown preliminary effectiveness in addition to research showing transcranial direct current stimulation can be an effective treatment for adults with ADHD.
Summary
Although questions exist about the effectiveness of current assessments of and treatments for adult ADHD, recent findings represent a step towards improving the quality of life and outcomes for individuals experiencing this life-long, chronic health condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a heterogeneous and complex neurodevelopmental disorder that represents the extreme end of a bell curve on several traits (i.e., distractibility, sustained attention, inhibition, and self-regulation). The diagnosis of ADHD depends heavily on reports of symptoms from self, parents, significant others/friends, or teachers. There currently do not exist laboratory tests that can reliably predict ADHD. Clinical manifestations of ADHD in adulthood are heterogeneous and disrupt social, occupational, and educational functioning [1]. While prevalence rates of ADHD are sensitive to source and how information is collected, the disorder affects 366.33 million adults globally and 19.86 million individuals (5.2% of the adult population) in the USA [2•, 3]. ADHD appears highly heritable with estimates ranging up to 74% attributed to genetic causes with the effects of each individual gene being relatively small [4, 5]. ADHD is associated with an average 11.1-year reduction in life expectancy and impairment in several other domains (e.g., employment, see Table 1) [6••, 7]. ADHD symptoms appear related to disruptions to the dopamine (DA) transporter and receptor genes [8]. Polymorphisms within the DRD5, DRD2, and DRD4 transporter genes are associated with ADHD. Disruptions in these transporters relate to motivational changes [8, 9]. Norepinephrine and structural changes to the prefrontal cortex, corpus striatum, cerebellum, and various white matter pathways have also been implicated in the pathophysiology of ADHD [10].
Clinical Manifestations and Outcomes
ADHD symptoms had been traditionally child-focused but more attention was brought to the manifestation of adult ADHD starting in the DSM-5. Characteristic clinical symptoms of ADHD are inattention, hyperactivity, and/or impulsivity [1]. The median age of onset (i.e., first diagnosis) of ADHD is six years old [11]. Various studies have found that about half of children with ADHD continue to meet criteria into adulthood, including 366.33 million adults globally and 19.86 (5.2%) million adults in the USA [2•, 3]. Research indicates that four main factors are associated with the persistence of ADHD from childhood to adulthood: severity of childhood ADHD (OR 2.33, 95% CI = 1.6–3.39), treatment for ADHD in childhood (OR 2.09, 95% CI = 1.04–4.18), comorbid conduct disorder in childhood (OR 1.85, 95% CI = 1.06–3.24), and comorbid major depressive disorder in childhood (OR 1.8, 95% CI = 1.1–2.95) [12]. Adults with ADHD are more likely than children with the condition to experience sleep problems [13]. Similar to childhood ADHD, adults with ADHD experience frequent comorbid mental health conditions and impairments in various domains of life (i.e., social, occupational, and educational), and demonstrate an increased risk for suicidal ideation and self-harm especially at high levels of impulsivity [6••, 14]. Adults with ADHD have significantly higher odds of dying from suicide or accidents than those without ADHD (adjusted odds ratio = 1.78, 95% confidence interval = 1.01, 3.12); experience higher rates of being fired from employment (55% compared to 23%); have fewer close friends (4 compared to 5); enroll in college at lower rates (21% compared to 78%); lower marital satisfaction; and more economic and housing instability [6••, 15, 16]. Specifically, research shows ADHD is associated with high divorce rates, lower intimacy and marital satisfaction, and poorer relationship skills [17]. Research suggests ADHD has a correlation with poor school performance including lower test scores and grade point averages—thereby potentially leading to lower employability [18]. Finally, individuals with ADHD experience high rates of justice system involvement, traumatic brain injuries, and accelerated rates of brain ageing [19,20,21]. Taken together, ADHD, especially if untreated, represents significant economic, personal, and social risks to individuals and downstream costs to society.
Diagnosis of ADHD in Adulthood
ADHD in adults may manifest differently than in children/adolescents. For example, while children with ADHD may run and climb at inappropriate times, adults with ADHD may experience general internal restlessness. Furthermore, while children with ADHD may experience consequences in school for not following rules due to their inattention, adults with ADHD and subsequent inattention result in greater consequences (e.g., job loss). As a realization that ADHD symptoms may start later and may persist into adulthood, the DSM-5 and 5-TR criteria for ADHD have been modified. For example, Criterion B (age of onset) was change from 7 to 12 years old, examples of how symptoms may manifest in adulthood were provided (e.g., difficulty with duties in the workplace, easily distracted by unrelated thoughts, forgetful in paying bills, take over what others are doing), and a reduction from 6 to 5 symptoms required in order to meet criteria for ADHD [1]. The assessment of ADHD in adults typically involves a combination of clinical interviews and self-report rating scales, which partially rely on unreliable sources of information (e.g., retrospective recall of childhood symptoms) [22]. However, rating scales often fail to provide substantial information about the diagnosis being assessed, such as onset, duration of symptoms, temporal relationships, contextual factors, or differential diagnoses and are prone to response biases [23]. Objective, performance-based measures (e.g., continuous performance tests) promised an additional ability to detect ADHD symptoms (i.e., attention, hyperactivity/impulsivity) without the drawbacks of retrospective recall, but lack strong discriminant and ecological validity, especially in cases of comorbid presentations of ADHD in adulthood [2425•]. Long-range temporal correlations in various EEG frequency bands have not been able to discriminate ADHD from comorbid disorders [26]. Testing batteries that assess neurocognitive functioning (e.g., working memory, sustained attention, response speed, and variability) are best able to discriminate ADHD from non-ADHD adults [27]. However, similar to continuous performance testing, neurocognitive measures of ADHD in adults lack specificity and cannot reliably discriminate ADHD from other disorders (e.g., anxiety) [28].
Adult ADHD Comorbidity and Differential Diagnoses
ADHD in adulthood often co-occurs with other mental health conditions, including major depressive disorder, anxiety disorders, and personality disorders [6••]. However, it is important to differentiate ADHD symptoms from other psychopathologies in cases where the behavioral manifestations may overlap. For example, major depressive disorder (MDD) and borderline personality disorder (BPD) have some features which may present similar behaviors to ADHD. Adults who are experiencing MDD may experience inattentive symptoms similar to those in ADHD; however, they will also experience a loss of interest or pleasure in most activities, fatigue, and anergia [1]. MDD can also result in psychomotor agitation which could look like restlessness. Some researchers have found that symptoms of ADHD and depression/anxiety cannot be adequately assessed via measures of malingering [29]. Adults with symptoms of BPD display similar impulsivity as adults with ADHD; however, they also experience affective instability, intense relationships, suicidal preoccupation, and angry outbursts that are longer and more goal directed [30]. Although the typical feature of inattention in adult ADHD can co-occur in anxiety disorders, anxiety is accompanied by fear, worry, and persistent rumination [1]. In contrast, ADHD inattention is driven by “preferential engagement with novel and stimulating activities or preoccupation with enjoyable activities” (p. 74) [1]. Finally, patterns have been found whereby certain comorbid conditions are associated with certain subtypes of ADHD (e.g., inattentive subtype and dysthymia and anxiety disorders) [31]. Given these overlapping symptom presentations, the lack of reliable, valid performance-based measures, and the high degree of comorbidity, clinicians’ best options for successful diagnosis is a careful clinical interview combined with questionnaire-based behavioral assessments [32]. When possible, both interviews and behavioral assessments should include information from collateral informants such as parents, partners, siblings, and co-workers/friends (when appropriate).
Neurobiology and Neuropathology of ADHD
Several neurobiological theories of ADHD exist and suggest that late maturing brain areas, executive dysfunction, and/or metabolic disturbances may underlie some of the neurocognitive deficits observed within ADHD such as attention and impulse control [33,34,35,36,37,38,39]. The behavioral neuroenergetics theory postulates that inadequate production of lactate by astrocytes causes neuronal energy insufficiency in cognitive resources associated with ADHD symptoms [36, 38]. The state/vigilance regulation theory suggests that ADHD is caused by impaired regulation of the arousal state such that individuals with ADHD manifest deficits in situations that are particularly uninteresting to them [40]. Executive dysfunction theories state that deficits in multiple domains associated with ADHD are caused by “higher-order” central executive (top-down) cognitive dysregulation impairment [35, 39]. For example, the default mode network (DMN)—which activates when the individual is not focused on the external environment—has been theorized to be associated with ADHD [36, 41]. Another theory implicates bottom-up regulation of processing of rewards, in that adults with ADHD experience dysfunction in processing sensory input and identifying which input merits attentional fixation [33]. Other theories hypothesize that deficits in multiple areas (e.g., inhibiting responses, delay of gratification, and attentional control) underlie the behavioral manifestations and neurocognitive deficits observed in ADHD [38]. One of the leading theories on the neurobiology of ADHD holds there is a “maturational delay” of key neuronal structures and pathways that control attentional and executive processes.
Recent research demonstrates functional and structural dysfunction of neural networks involved in processes of executive function, reward anticipation, and attention within adults diagnosed with ADHD. A meta-analysis across studies of structural, whole-brain voxel-based morphometry (VBM) analysis showed that the largest gray matter differences were in several frontal-parietal brain regions, the limbic system, and the corpus callosum [42••]. Other VBM analyses find that participants with ADHD have significantly smaller gray matter volume in the precentral gyrus, medial and orbitofrontal cortex, and (para)cingulate cortices [43]. Conversely, adults with ADHD do not differ on cortical thickness, gyrification index, sulcal depth, or fractal dimension compared to control adults [44]. However, adults with the combined subtype of ADHD show signs of significant thinning of the left anterior insular cortex and adults with the hyperactive subtype demonstrate thinner left pars opercularis cortical thickness [44]. Interestingly, these regions partly, but not completely, overlap with structural differences observed within individuals diagnosed with borderline personality disorder (BPD) and major depressive disorder (MDD), two common comorbid and differential diagnoses for adult ADHD [45].
Regarding white matter disruptions within adult ADHD, research using diffusion tensor imaging (DTI) indicates reduced fractional anisotropy (FA) in white matter regions of the primary motor cortex and regions subserving frontostriatal-thalamic and frontoparietal (i.e., superior longitudinal fasciculus) circuitry in young adults with ADHD [46•]. In contrast, a recent longitudinal diffusion imaging study following individuals from childhood to adulthood found evidence for more rapid development in white matter microstructures, including changes in development of generalized fractional anisotropy in the arcuate fasciculus, superior longitudinal fasciculus, frontal aslant tract, cingulum, inferior fronto-occipital fasciculus (IFOF), frontostriatal tract connecting the prefrontal cortex (FS-PFC), thalamic radiation, corticospinal tract, and corpus callosum [47•]. Finally, research indicates that medication-naive adults with ADHD show increased local connectivity in the dorsal anterior cingulate cortex (dACC) and the superior frontal gyrus (SFG) and decreased local connectivity in the posterior cingulate cortex (PCC) [48]. Thus, in summary, anatomic and functional correlates have been found in studies on adult ADHD in the primary motor cortex, frontal lobe, corpus collosum, in addition to gray matter differences, white matter microstructures, and cortical thinning.
In addition to network and structural differences, the dopaminergic (DA) system plays a critical role in the maintenance of factors associated with ADHD, including attention and motor control, cognitive abilities, and emotion regulation [8]. Deficiencies in DAT reduce the potency of the dopaminergic response leading to deficits in regulating attention [49]. Changes in the DA receptor response are theorized to significantly contribute to the delayed brain development and maturation of individuals with ADHD [8].
Beyond structural and neurotransmitter alterations, research finds disruptions in important functional processes in adults with ADHD as evidenced by both hypo- and hyperactivation across several cortical and subcortical networks. Functional magnetic resonance imaging (fMRI) analysis indicates significant hypoactivation in several frontal-temporal brain regions including the right postcentral gyrus, the left insula, and the corpus callosum [42••]. Some researchers speculate that underactivation of these brain regions may be related to poor impulse and inhibitory behaviors seen in adult ADHD symptomology. Conversely, hyperactivation has been shown in other brain regions, including the middle occipital gyrus, the right insula, the right precuneus cortex, right caudate nucleus, right central operculum, and structures within the auditory/sensorimotor network [5042••S, ]. Researchers postulated overactivation in these brain regions leads to dysfunctional neuromodulation of circuits affecting executive functioning and attentional control networks [51]. Consistent with this, adults with ADHD engage more strongly the dorsal anterior cingulate cortex, middle temporal gyrus, precuneus, lingual gyrus, precentral gyrus, and insula when compared to healthy controls during task switching paradigms [52]. Despite the substantial progress in uncovering the neurobiological pathways and structures disrupted within adult ADHD, we continue to lack a comprehensive, integrated understanding of the neurobiological substrates of this disorder (e.g., structural, functional, and physiological); this gap hampers our ability to pursue and test novel treatment approaches for ADHD in children and adults.
Biomarkers
Researchers have found evidence for unique biological processes of adults with ADHD that may act as biomarkers. Identifying these biomarkers can be invaluable in both the diagnosis and treatment of adult ADHD. For example, electroencephalogram (EEG) findings suggest differences in brain electrical activity within ADHD adults during executive function and divided/sustained attention tasks [53]. Moreover, adults with ADHD show a selective impairment on P3 event–related potential (ERP) amplitude on EEG measurement [53]. Alpha activity from EEG data is able to typically differentiate between control and ADHD adults but has some inconsistencies [54]. Other EEG studies find different temporal dynamics and longer mean durations of a frontocentral topography for patients with ADHD compared to control patients [55]. A recent systematic review of 21 studies found patterns of people with adult ADHD demonstrate elevated levels of both absolute and relative theta power and alpha activity when compared to a normative population [54]. Additionally, adults with ADHD were found to have an overall decrease in neural activity when engaged with attention demanding tasks [54].
Blood-based biomarkers of adult ADHD have been recently identified, including neuroinflammatory agents. For example, studies have found both positive and negative associations between inflammatory markers and adult ADHD, including increased interleukin-6 and C-reactive protein and decreased levels of tumor necrosis factor-α [56, 57]. It has been suggested that alterations in peripheral inflammations may lead to neurofunctional disruptions that result in ADHD symptomology via reduced dopamine levels and dysregulation of noradrenergic neurotransmission [58]. Pupil diameter is a recently identified candidate physiological biomarker of adult ADHD. Researchers found adult ADHD to be associated with larger pupil diameter and less complexity and symmetricity of dynamic pupil diameter behaviors [59••]. Researchers of this study suggest the larger pupilary diameter is a result of a hyperactive locus coeruleus (LC), a phenomenon already associated with ADHD. Pupilary diameter measurement could prove to be a relatively cheap and convenient diagnostic measurement when assessing for ADHD. Unfortunately, as with other psychiatric disorders, progress towards reliable, clinically useful biomarkers that could aid in the identification and treatment of ADHD continues to lag behind other branches of medicine.
Treatment of Adult ADHD
The guidelines for the treatment of adult ADHD by the National Institute for Health and Care Excellence (NICE) recommend initially using “environment modifications” followed by medications with consistent follow-up [60]. Pharmacotherapies tested in randomized controlled trials in adults include methylphenidate, atomoxetine, dexamfetamine, lisdexamfetamine, guanfacine, bupropion, mixed-amphetamine salts, and modafinil [61]. These medications target several neurochemical pathways, including dopamine and norepinephrine transporters [62]. Few differences have been observed between these medications; however, atomoxetine is associated with improved clinical response and quality of life compared to placebo [61]. For adults with ADHD, stimulant medications continue to be the first-line medication option for adults with ADHD [63]. Recently, however, viloxazine ER (Qelbree), which is a norepinephrine reuptake inhibitor and acts on serotonergic signaling in the brain, has shown some effectiveness in the treatment of ADHD in adults [42••, 6564•, ]. However, medications that increase both dopaminergic and noradrenergic transmission have not been tested in long-term clinical trials [49].
Another important factor is the long-term effects of psychotropic use. Cross-sectional reviews have found that stimulant medications for ADHD across the lifespan are associated with 9–58% reductions in injuries, motor vehicle accidents, and substance use disorder [66, 67]. Furthermore, at least one systematic review provides evidence that medication treatment for ADHD is associated with decreased rates of mood disorders, substance use disorders, suicidality, justice-involvement, motor vehicle crashes, physical injuries including head injuries, and improved academic outcomes [67]. Methylphenidate treatment is significantly associated with cognitive benefits on response inhibition (g [Hedges’ g] = 0.40), working memory (g = 0.24), and sustained attention (g = 0.42) [68]. The clinical benefits of long-term stimulant use remain unclear [69]. Students with ADHD may be depending on stimulant medications to help with cramming whereas students without diagnosable ADHD may attempt to improve their performance by taking non-prescribed stimulant medication [70].
Neuroimaging provides some evidence of the efficacy of medication for treating adult ADHD. Using fMRI, a meta-analysis of ADHD medications on the brains of youth with ADHD found that the ventrolateral prefrontal cortex (area associated with cognitive control) function similarly to those without ADHD [71]. One longitudinal study found that stimulants were associated with the slowing of cortical thinning (0.03 mm/year) over a 4-year period compared to participants not taking stimulants (0.16 mm/year). This finding was later supported by meta-analytic reviews suggesting stimulants may have a “neuro-protective” effect [72,73,74]. In contrast, other studies have found no changes in brain structures of youth and adults with ADHD taking medications [75, 76]. Importantly, chronic exposure to stimulants does not seem to influence total brain volume [77]. The above studies are notwithstanding the adverse events that lead 40% of adults to discontinue stimulant medication use [78]. Importantly, ADHD medications are not associated with an increased rate of substance abuse [79]. Interestingly, a newer treatment, transcranial direct current stimulation (tDCS), in adults with ADHD shows some promise and is associated with greater cortical thickness in the left inferior frontal cortex and stronger decreases in scores on measures of attention when compared to control participants [80••]. Furthermore, higher right subgenual area of the anterior cingulate cortex volumes were associated with significantly higher decrease in inattentive scores in the tDCS group [80••]. Thus, the treatment of adult ADHD with psychotropic medications appears generally beneficial although the impact on some domains (e.g., academics) remains uncertain. Emerging treatments such as TDCS need more rigorous, longitudinal studies to prove their effectiveness and clinical utility. Finally, the relative paucity of longitudinal studies examining potential negative side effects of long-term stimulant use also remains a concern. However, there is some evidence that medication-naive adults with ADHD show increased local connectivity in the dorsal anterior cingulate cortex (dACC) and the superior frontal gyrus (SFG)[69] and decreased local connectivity in the posterior cingulate cortex (PCC) [48, 69].
A small literature examines the role of behavioral-based treatments either alone or in combination with medication. When comparing pharmacotherapy alone to pharmacotherapy plus psychotherapy for adults with ADHD, one study found no difference in outcomes between the groups [81]. Nonetheless, some adults with ADHD experience side effects from medication or experience persistent difficulties suggesting that behavioral approaches (with or without medication) may be viable options to augment or replace traditional psychotropic treatment for some individuals [82]. Research suggests that non-pharmacological treatments such as cognitive behavioral and mindfulness-based therapies may be appropriate components for comprehensive treatment of adult ADHD [83]. For example, mindfulness-based treatments have been shown through neuroimaging to minimize distractibility in ADHD participants through enhancement of the default mode network (DMN) and can also assist with difficulties caused by emotional dysregulation [84]. Additionally, cognitive behavioral therapies focus on providing skills for managing inattention, impulsivity, and hyperactivity symptoms while cognitively restructuring certain unhelpful thinking patterns [83]. Emerging research suggests that diet via its impact on the gut microbiome may be an important avenue for treatment of adults and children with ADHD [85, 86].
Current controversies
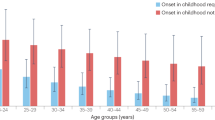
Several major controversies continue to roil the field of adult ADHD research. Multiple longitudinal studies released in the last 7 years found some adults with ADHD symptoms did not have childhood symptoms [87, 88]. However, researchers argue that these studies showing symptoms of ADHD appearing in adulthood could be associated with shifts from “subthreshold ADHD” in childhood to full symptoms in adulthood, or the low reliability of retrospective recall used by studies in adulthood [87, 88]. Regardless of phenotypic presentation or childhood onset, providers are recommended to still treat symptoms of adult ADHD due to the impairment and high comorbidity associated with ADHD [31]. Specifically, 50 percent of adult patients with ADHD have at least one comorbid psychiatric condition [31].
Adults with ADHD also display differential patterns of symptoms compared to children. For example, a dimension called Sluggish Cognitive Tempo (SCT; “forgetfulness, day-dreaminess,” and “sluggishness/drowsiness”) accounted for the majority of the variance (44.5–65.9%) in executive functioning deficits compared to the hyperactivity (8.5%) dimension in adults with ADHD [89]. SCT may serve as an important dimension because it is significantly associated with fewer years of education, less income, and academic problems above inattention and hyperactivity/impulsivity symptoms [89, 90]. Researchers suggest that different attentional networks may be implicated in SCT versus ADHD [91]. Placebo-controlled trials of lisdexamfetamine have shown large treatment effects for adults with ADHD and comorbid SCT symptoms [92]. The DSM-5-TR defines hyperactivity symptoms in a way that may not accurately capture the experiences of adults (e.g., “fidgets…leaves seat”) [1].
Concerns regarding medication abuse have led to a degree of hesitancy in treating ADHD on the part of clinicians and medical providers, particularly in the case of co-occurring substance abuse. No clear guidelines exist for the treatment of this comorbidity, with some stating that exposure to stimulants could sensitize the brain to the rewarding effects of drugs, increasing the risk for substance abuse [12, 93,94,95]; however, longitudinal studies do not necessarily support this assertion [79]. Additionally, the ethics of withholding ADHD treatment from individuals with current or past substance use disorders remains contested [94], although a period of sobriety prior to beginning treatment with stimulant medication is usually considered best practice. ADHD medication abuse has been noted in various populations outside of individuals diagnosed with substance use disorders. For example, college students have turned to prescription stimulants both to enhance academic performance and recreationally, with some estimates noting that the lifetime and past-year prevalence rates 8.3% and 5.9% use these substances without a diagnosis [96, 97]. Additionally, there is evidence that some college students with ADHD sell this medication to others. Among students with ADHD and prescriptions, 29% had sold their ADHD medications in their lifetime [98]. Concerns also exist about harmful drug interactions. In particular, cytochrome P450 (CYP) 2D6 inhibitors (which include many types of antidepressants, such as bupropion, fluoxetine, and duloxetine) increase amphetamine levels, which has the same effect as a higher dosage, although evidence suggests that it is possible to mitigate potential effects [16, 99]. Sex differences in neuropsychological functioning of ADHD in adults is another area of emerging interest [100••, 101]. For example, some studies have found dynamic functional network connectivity differences in females compared to males [102]. This is an important finding as measures and treatments are often developed in mostly male samples. Finally, the difficulties associated with performance-based tasks to assess ADHD symptoms, the reliance on questionnaire- and interview-based measures for diagnoses, and the lack of a reliable, consistent neurocognitive phenotype represent significant questions within the ADHD field [25
Conclusions
ADHD in adults is now recognized as a real diagnostic entity and research illustrates it is associated with significant behavioral and psychosocial dysfunction. Although gains have been made in describing and diagnosing ADHD in adults, the field continues to rely substantially on interview- and questionnaire-based assessment methods. While many of the biological, psychosocial, and developmental substrates of adult ADHD have been elucidated, we lack a coherent, integrated theory explaining how these deficits interact. Moreover, the lack of large-scale, longitudinal investigations examining ADHD across development and within the context of psychiatric comorbidity is also a problem. Stimulant medications have been shown to be effective in the management of ADHD symptoms within adults although long-term findings are less consistent. Moreover, newer treatment approaches such as TDCS and combination medication and behavioral therapy approaches, while promising, remain in need of well-controlled, randomized clinical trials to prove their effectiveness. Questions remain regarding the safety and effectiveness of ADHD medication in the context of substance use disorders and with respect to adult-onset ADHD (e.g., does this group represent a distinct subset of ADHD cases or rather merely ADHD that went undetected during childhood). Finally, studies have begun to examine sex differences in the course, treatment, and prognosis of adult ADHD although this literature remains under-developed. Similarly, the field is in need of a better understanding of how ADHD functions and treatment effectiveness within diverse groups.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders [Internet]. In: DSM-5-TR. American Psychiatric Association Publishing; 2022. Available from: https://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425787.
Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: a global systematic review and meta-analysis. J Glob Health. 2021;11:04009. This study represents a significant step forward in understanding the global prevalence rate in ADHD. Persistent ADHD across the globe was 2.58%.
Fayyad J, Sampson NA, Hwang I, Adamowski T, Aguilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV adult ADHD in the World Health Organization World Mental Health Surveys. ADHD Atten Def Hyp Disord. 2017;9:47–65.
Faraone SV, Larsson H. Genetics of attention deficit hyperactivity disorder. Mol Psychiatry. 2019;24:562–75.
Makris N, Biederman J, Monuteaux MC, Seidman LJ. Towards conceptualizing a neural systems-based anatomy of attention-deficit/hyperactivity disorder. Dev Neurosci. 2009;31:36–49.
Barkley RA. ADHD adversely impacts health, mortality risk, and estimated life expectancy by adulthood. ADHD Rep. 2020;28(1-4):14. The author conducted a cumulative risk assessment based on data from 14 variables related to ADHD, including health and lifestyle patterns. The findings were that accidental injury and death by suicide were significant factors, leading to an 11.1-year reduction in life expectancy for individuals with ADHD into adulthood.
Barkley RA, editor. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. Fourth edition. Paperback ed. New York, NY: The Guilford Press; 2018.
Wu J, Xiao H, Sun H, Zou L, Zhu L-Q. Role of dopamine receptors in ADHD: a systematic meta-analysis. Mol Neurobiol. 2012;45:605–20.
Volkow ND, Wang G-J, Newcorn JH, Kollins SH, Wigal TL, Telang F, et al. Motivation deficit in ADHD is associated with dysfunction of the dopamine reward pathway. Mol Psychiatry. 2011;16:1147–54.
Mehta TR, Monegro A, Nene Y, Fayyaz M, Bollu PC. Neurobiology of ADHD: a review. Curr Dev Disord Rep. 2019;6:235–40.
Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53:34–46.e2.
Caye A, Spadini AV, Karam RG, Grevet EH, Rovaris DL, Bau CHD, et al. Predictors of persistence of ADHD into adulthood: a systematic review of the literature and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25:1151–9.
Gregory AM, Agnew-Blais JC, Matthews T, Moffitt TE, Arseneault L. ADHD and sleep quality: longitudinal analyses from childhood to early adulthood in a twin cohort. J Clin Child Adolesc Psychol. 2017;46:284–94.
Beach VL, Gissandaner TD, Schmidt AT. The UPPS model of impulsivity and suicide: a systematic literature review. Arch Suicide Res. 2022;26:985–1006.
London AS, Landes SD. Attention deficit hyperactivity disorder and adult mortality. Prev Med. 2016;90:8–10.
Schjøtt J, Heitmann K, Bakkebø T, Jahnsen JA. Review of questions concerning clinical drug interactions in ADHD treatment from physicians in Norway. Front Pharmacol. 2020;11:607915.
Wozniak J. Attention-deficit/hyperactivity disorder and problematic romantic relationships in adulthood: a review of the literature. Spectrum [Internet]. 2022; Available from: https://spectrumjournal.ca/index.php/spectrum/article/view/158
Varrasi S, Boccaccio FM, Guerrera CS, Platania GA, Pirrone C, Castellano S. Schooling and occupational outcomes in adults with ADHD: predictors of success and support strategies for effective learning. Educ Sci. 2022;13:37.
Richmond-Rakerd LS, Caspi A, Ambler A, d’Arbeloff T, De Bruine M, Elliott M, et al. Childhood self-control forecasts the pace of midlife aging and preparedness for old age. Proc Natl Acad Sci USA. 2021;118:e2010211118.
Maloney KA, Schmidt AT. Juvenile delinquency and antisocial behavior: a brief overview of theories, definitions, and statistics. The SAGE encyclopedia of criminal psychology: SAGE Publications; 2019.
Schmidt AT, Beers SR, Levin HS. Rehabilitation and outcome of head injuries. Principles and practice of pediatric neurosurgery. Thieme Medical Publishers; 2014. p. 737–49.
Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur psychiatr. 2019;56:14–34.
Aita SL, Sofko CA, Hill BD, Musso MW, Boettcher AC. Utility of the Personality Assessment Inventory in detecting feigned attention-deficit/hyperactivity disorder (ADHD): the Feigned Adult ADHD Index. Arch Clin Neuropsychol. 2018;33:832–44.
Barkley RA. Neuropsychological testing is not useful in the diagnosis of ADHD: stop it (or prove it)! ADHD Rep. 2019;27:1–8.
Pagán AF, Huizar YP, Schmidt AT. Conner’s continuous performance test and adult ADHD: a systematic literature review. J Atten Disord. 2023;27:231–49. The authors reviewed 35 articles which utilized the Conner’s continuous performance test for adults with ADHD. Findings indicated that reliability and discriminant and ecological validity were moderate with mixed sensitivity and specificity
Huang J, Ahlers E, Bogatsch H, Böhme P, Ethofer T, Fallgatter AJ, et al. The role of comorbid depressive symptoms on long-range temporal correlations in resting EEG in adults with ADHD. Eur Arch Psychiatry Clin Neurosci. 2022;272:1421–35.
Nikolas MA, Marshall P, Hoelzle JB. The role of neurocognitive tests in the assessment of adult attention-deficit/hyperactivity disorder. Psychol Assess. 2019;31:685–98.
Grogan K, Gormley CI, Rooney B, Whelan R, Kiiski H, Naughton M, et al. Differential diagnosis and comorbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99–115.
Grant AF, Lace JW, Teague CL, Lowell KT, Ruppert PD, Garner AA, et al. Detecting feigned symptoms of depression, anxiety, and ADHD, in college students with the structured inventory of malingered symptomatology. Appl Neuropsychol Adult. 2022;29:443–51.
Asherson P, Young AH, Eich-Höchli D, Moran P, Porsdal V, Deberdt W. Differential diagnosis, comorbidity, and treatment of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657–72.
Ohnishi T, Kobayashi H, Yajima T, Koyama T, Noguchi K. Psychiatric comorbidities in adult attention-deficit/hyperactivity disorder: prevalence and patterns in the routine clinical setting. Innov Clin Neurosci. 2019;16:11–6.
Maloney KA, Schmidt AT. Psychological assessment in medical settings: overview and practice implications. In: The Wiley encyclopedia of health psychology, volume III: Clinical health psychology & behavioral medicine. John Wiley & Sons; 2021. p. 235–44.
Alexander L, Farrelly N. Attending to adult ADHD: a review of the neurobiology behind adult ADHD. Ir J Psychol Med. 2018;35:237–44.
Hegerl U, Hensch T. The vigilance regulation model of affective disorders and ADHD. Neurosci Biobehav Rev. 2014;44:45–57.
Baroni A, Castellanos FX. Neuroanatomic and cognitive abnormalities in attention-deficit/hyperactivity disorder in the era of ‘high definition’ neuroimaging. Curr Opin Neurobiol. 2015;30:1–8.
Kofler MJ, Alderson RM, Raiker JS, Bolden J, Sarver DE, Rapport MD. Working memory and intraindividual variability as neurocognitive indicators in ADHD: examining competing model predictions. Neuropsychol. 2014;28:459–71.
Gawrilow C, Kuhnhausen J, Schmid J, Stadler G. Hyperactivity and motoric activity in ADHD: characterization, assessment, and intervention. Front Psychiatry [Internet]. 2014;5 Available from: http://journal.frontiersin.org/article/10.3389/fpsyt.2014.00171/abstract
Killeen PR. Models of attention-deficit hyperactivity disorder. Behav Process. 2019;162:205–14.
Matthews M, Nigg JT, Fair DA. Attention deficit hyperactivity disorder. In: Andersen SL, Pine DS, editors. The neurobiology of childhood [Internet]. Berlin, Heidelberg: Springer Berlin Heidelberg; 2013. p. 235–66. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/978-3-662-45758-0_249.
Jadidian A, Hurley RA, Taber KH. Neurobiology of adult ADHD: emerging evidence for network dysfunctions. JNP. 2015;27:173–8.
Janssen TWP, Hillebrand A, Gouw A, Geladé K, Van Mourik R, Maras A, et al. Neural network topology in ADHD; evidence for maturational delay and default-mode network alterations. Clin Neurophysiol. 2017;128:2258–67.
. Yu M, Gao X, Niu X, Zhang M, Yang Z, Han S, et al. Meta-analysis of structural and functional alterations of brain in patients with attention-deficit/hyperactivity disorder. Front Psychiatry. 2023;13:1070142. The authors reviewed 29 VBM studies and 36 fMRI studies which found key structural and functional alterations in the left superior frontal gyrus and the corpus callosum
Bralten J, Greven CU, Franke B, Mennes M, Zwiers MP, Rommelse NNJ, et al. Voxel-based morphometry analysis reveals frontal brain differences in participants with ADHD and their unaffected siblings. Jpn. 2016;41:272–9.
Maier S, Philipsen A, Perlov E, Runge K, Matthies S, Ebert D, et al. Left insular cortical thinning differentiates the inattentive and combined subtype of adult attention-deficit/hyperactivity disorder. J Psychiatry Res. 2023;159:196–204.
Cao Y, Xie H, Sun H, Xiao H, Long X, Qiu C, et al. Common and distinct patterns of gray matter alterations in young adults with borderline personality disorder and major depressive disorder. Eur Arch Psychiatry Clin Neurosci. 2022;272:1569–82.
. Jones SA, Tipsord J, Nagel BJ, Nigg JT. A preliminary study of white matter correlates of a laboratory measure of attention and motor stability in attention-deficit/hyperactivity disorder. J Psychiatric Res. 2023;160:110–6. In a new measure of ADHD attention and motor behavior (the QbTest), associations were found between motor activity and inattention and MRI findings, including differences in primary motor cortex white matter
Chiang H-L, Tseng W-YI, Tseng W-L, Tung Y-H, Hsu Y-C, Chen C-L, et al. Atypical development in white matter microstructures in ADHD: a longitudinal diffusion imaging study. Asian J Psychiatr. 2023;79:103358. The ADHD groups showed abnormalities in white matter microstructures, supporting the delayed brain maturation hypothesis
Marcos-Vidal L, Martínez-García M, Martín de Blas D, Navas-Sánchez FJ, Pretus C, Ramos-Quiroga JA, et al. Local functional connectivity as a parsimonious explanation of the main frameworks for ADHD in medication-naïve adults. J Atten Disord. 2022;26:1788–801.
Perugi G, De Rosa U, Barbuti M. What value do norepinephrine/dopamine dual reuptake inhibitors have to the current treatment of adult attention deficit hyperactivity disorder (ADHD) treatment armamentarium? Expert Opin Pharmacother. 2022;23:1975–8.
Sörös P, Hoxhaj E, Borel P, Sadohara C, Feige B, Matthies S, et al. Hyperactivity/restlessness is associated with increased functional connectivity in adults with ADHD: a dimensional analysis of resting state fMRI. BMC Psychiatry. 2019;19:43.
Cao H. Prefrontal-cerebellar dynamics during post-success and post-error cognitive controls in major psychiatric disorders. Psychol Med. 2022:1–8.
Dibbets P, Evers EAT, Hurks PPM, Bakker K, Jolles J. Differential brain activation patterns in adult attention-deficit hyperactivity disorder (ADHD) associated with task switching. Neuropsychol. 2010;24:413–23.
Salomone S, Fleming GR, Bramham J, O’Connell RG, Robertson IH. Neuropsychological deficits in adult ADHD: evidence for differential attentional impairments, deficient executive functions, and high self-reported functional impairments. J Atten Disord. 2020;24:1413–24.
Adamou M, Fullen T, Jones SL. EEG for diagnosis of adult ADHD: a systematic review with narrative analysis. Front Psychiatry. 2020;11:871.
Férat V, Arns M, Deiber M-P, Hasler R, Perroud N, Michel CM, et al. Electroencephalographic microstates as novel functional biomarkers for adult attention-deficit/hyperactivity disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2022;7:814–23.
Misiak B, Wójta-Kempa M, Samochowiec J, Schiweck C, Aichholzer M, Reif A, et al. Peripheral blood inflammatory markers in patients with attention deficit/hyperactivity disorder (ADHD): a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2022;118:110581.
Yang LL, Stiernborg M, Skott E, Söderström Å, Giacobini M, Lavebratt C. Proinflammatory mediators and their associations with medication and comorbid traits in children and adults with ADHD. Eur Neuropsychopharmacol. 2020;41:118–31.
Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL. Attention-deficit/hyperactivity disorder and inflammation: what does current knowledge tell us? A systematic review. Front Psychiatry. 2017;8:228.
Nobukawa S, Shirama A, Takahashi T, Takeda T, Ohta H, Kikuchi M, et al. Identification of attention-deficit hyperactivity disorder based on the complexity and symmetricity of pupil diameter. Sci Rep. 2021;11:8439. The authors utilized pupil diameter analyses to assist in the diagnosis of adult ADHD. Low temporal complexity in addition to large diameters of pupils was associated with ADHD in this sample which may provide an addition tool for the diagnosis of adult ADHD
National Guideline Centre. Attention deficit hyperactivity disorder: diagnosis and management [Internet]. London: National Institute for Health and Care Excellence (NICE); 2019. Available from: http://www.ncbi.nlm.nih.gov/books/NBK493361/
Elliott J, Johnston A, Husereau D, Kelly SE, Eagles C, Charach A, et al. Pharmacologic treatment of attention deficit hyperactivity disorder in adults: a systematic review and network meta-analysis. Gluud C, editor. PLoS ONE. 2020; 15: e0240584.
da Silva BS, Grevet EH, Silva LCF, Ramos JKN, Rovaris DL, Bau CHD. An overview on neurobiology and therapeutics of attention-deficit/hyperactivity disorder. Discov Ment Health. 2023;3:2.
Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5:727–38.
Faraone SV, Gomeni R, Hull JT, Chaturvedi SA, Busse GD, Melyan Z, et al. Predicting efficacy of viloxazine extended-release treatment in adults with ADHD using an early change in ADHD symptoms: machine learning post hoc analysis of a phase 3 clinical trial. Psychiatry Res. 2022;318:114922. The authors examined the response of adults to viloxazine ER, a new nonstimulant recently approved for adults
Nasser A, Hull JT, Chaturvedi SA, Liranso T, Odebo O, Kosheleff AR, et al. A phase III, randomized, double-blind, placebo-controlled trial assessing the efficacy and safety of viloxazine extended-release capsules in adults with attention-deficit/hyperactivity disorder. CNS Drugs. 2022;36:897–915.
Chang Z, Ghirardi L, Quinn PD, Asherson P, D’Onofrio BM, Larsson H. Risks and benefits of attention-deficit/hyperactivity disorder medication on behavioral and neuropsychiatric outcomes: a qualitative review of pharmacoepidemiology studies using linked prescription databases. Biol Psychiatry. 2019;86:335–43.
Boland H, DiSalvo M, Fried R, Woodworth KY, Wilens T, Faraone SV, et al. A literature review and meta-analysis on the effects of ADHD medications on functional outcomes. J Psychiatr Res. 2020;123:21–30.
Tamminga HGH, Reneman L, Huizenga HM, Geurts HM. Effects of methylphenidate on executive functioning in attention-deficit/hyperactivity disorder across the lifespan: a meta-regression analysis. Psychol Med. 2016;46:1791–807.
Armstrong-Hoskowitz N, Schmidt AT, Henderson CE, Nelson DV, Allen BJ. A field study of the impact of psychotropic medication on delinquency and juvenile justice system involvement among a high risk sample of children and adolescents. J Offender Rehabil. 2020;59:334–53.
Craig SG, Davies G, Schibuk L, Weiss MD, Hechtman L. Long-term effects of stimulant treatment for ADHD: what can we tell our patients? Curr Dev Disord Rep. 2015;2:1–9.
Rubia K, Alegria A, Brinson H. Imaging the ADHD brain: disorder-specificity, medication effects and clinical translation. Expert Rev Neurother. 2014;14:519–38.
Shaw P, Sharp WS, Morrison M, Eckstrand K, Greenstein DK, Clasen LS, et al. Psychostimulant treatment and the developing cortex in attention deficit hyperactivity disorder. AJP. 2009;166:58–63.
Frodl T, Skokauskas N. Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects: meta-analysis of structural MRI ADHD studies. Acta Psychiatrica Scandinavica. 2012;125:114–26.
Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, et al. Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging–based neuroimaging studies. J Clin Psychiatry. 2013;74:902–17.
Hoogman M, Bralten J, Hibar DP, Mennes M, Zwiers MP, Schweren LSJ, et al. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis. Lancet Psychiatry. 2017;4:310–9.
Hoogman M, Muetzel R, Guimaraes JP, Shumskaya E, Mennes M, Zwiers MP, et al. Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. AJP. 2019;176:531–42.
Castellanos FX. Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA. 2002;288:1740.
Cunill R, Castells X, Tobias A, Capellà D. Atomoxetine for attention deficit hyperactivity disorder in the adulthood: a meta-analysis and meta-regression: atomoxetine discontinuation in adult ADHD. Pharmacoepidemiol Drug Saf. 2013;22:961–9.
Humphreys KL, Eng T, Lee SS. Stimulant medication and substance use outcomes: a meta-analysis. JAMA Psychiatry. 2013;70:740.
Rodrigues da Silva PH, Leffa DT, Luethi MS, Rohde LA, Brunoni AR. Associations between brain morphology and transcranial direct current stimulation as treatment of inattention in adults with attention deficit/hyperactivity disorder. Brain Stimul. 2023;16:350. A new treatment called transcranial direct current stimulation (tDCS) was evaluated in terms of changes in brain volume or cortical thickness. Changes were found in the superior frontal cortex and decreases in subjective ADHD inattentive scores were associated with higher cortical thickness
Corbisiero S, Bitto H, Newark P, Abt-Mörstedt B, Elsässer M, Buchli-Kammermann J, et al. A comparison of cognitive-behavioral therapy and pharmacotherapy vs. pharmacotherapy alone in adults with attention-deficit/hyperactivity disorder (ADHD)—a randomized controlled trial. Front. Psychiatry. 2018;9:571.
Krinzinger H, Hall CL, Groom MJ, Ansari MT, Banaschewski T, Buitelaar JK, et al. Neurological and psychiatric adverse effects of long-term methylphenidate treatment in ADHD: a map of the current evidence. Neurosci Biobehav Rev. 2019;107:945–68.
Nimmo-Smith V, Merwood A, Hank D, Brandling J, Greenwood R, Skinner L, et al. Non-pharmacological interventions for adult ADHD: a systematic review. Psychol Med. 2020;50:529–41.
Bachmann K, Lam AP, Philipsen A. Mindfulness-based cognitive therapy and the adult ADHD brain: a neuropsychotherapeutic perspective. Front Psychiatry [Internet]. 2016;7 Available from: http://journal.frontiersin.org/Article/10.3389/fpsyt.2016.00117/abstract
Breda V, Cerqueira RO, Ceolin G, Koning E, Fabe J, McDonald A, et al. Is there a place for dietetic interventions in adult ADHD? Prog Neuropsychopharmacol Biol Psychiatry. 2022;119:110613.
Iliodromiti Z, Triantafyllou A-R, Tsaousi M, Pouliakis A, Petropoulou C, Sokou R, et al. Gut microbiome and neurodevelopmental disorders: a link yet to be disclosed. Microorganisms. 2023;11:487.
Barkley RA. Is there an adult onset type of ADHD? Issues in establishing persistence and remission of ADHD from childhood to adulthood. ADHD Rep. 2016;24(6-7):13–4.
Taylor LE, Kaplan-Kahn EA, Lighthall RA, Antshel KM. Adult-onset ADHD: a critical analysis and alternative explanations. Child Psychiatry Hum Dev. 2022;53:635–53.
Barkley RA. Barkley Adult ADHD Rating Scale-IV (BAARS-IV). New York: Guilford Press; 2011.
Becker SP, Langberg JM, Luebbe AM, Dvorsky MR, Flannery AJ. Sluggish Cognitive Tempo is associated with academic functioning and internalizing symptoms in college students with and without attention-deficit/hyperactivity disorder: SCT in college students. J Clin Psychol. 2014;70:388–403.
Becker S, Barkley RA. Sluggish cognitive tempo. Oxford textbook of attention deficit hyperactivity disorder. Oxford, England: Oxford University Press; 2018. p. 147–53.
Adler LA, Leon TL, Sardoff TM, Krone B, Faraone SV, Silverstein MJ, et al. A placebo-controlled trial of lisdexamfetamine in the treatment of comorbid Sluggish Cognitive Tempo and adult ADHD. J Clin Psychiatry [Internet]. 2021;82 Available from: https://www.psychiatrist.com/jcp/neurodevelopmental/a-placebo-controlled-trial-of-lisdexamfetamine-in-the-treatment-of-comorbid-sluggish-cognitive-tempo-and-adult-adhd/
Asherson P. Drug treatments for ADHD reduce risk of substance use disorders. AJP. 2017;174:827–8.
McGough JJ. Treatment controversies in adult ADHD. AJP. 2016;173:960–6.
Caye A, Rocha TB-M, Anselmi L, Murray J, Menezes AMB, Barros FC, et al. Attention-deficit/hyperactivity disorder trajectories from childhood to young adulthood: evidence from a birth cohort supporting a late-onset syndrome. JAMA. Psychiatry. 2016;73:705.
Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacother. 2006;26:1501–10.
Wilens T, Zulauf C, Martelon M, Morrison NR, Simon A, Carrellas NW, et al. Nonmedical stimulant use in college students: association with attention-deficit/hyperactivity disorder and other disorders. J Clin Psychiatry. 2016;77:940–7.
Upadhyaya HP, Rose K, Wang W, O’Rourke K, Sullivan B, Deas D, et al. Attention-deficit/hyperactivity disorder, medication treatment, and substance use patterns among adolescents and young adults. J Child Adolesc Psychopharmacol. 2005;15:799–809.
Schoretsanitis G, de Leon J, Eap CB, Kane JM, Paulzen M. Clinically significant drug–drug interactions with agents for attention-deficit/hyperactivity disorder. CNS Drugs. 2019;33:1201–22.
Carucci S, Narducci C, Bazzoni M, Balia C, Donno F, Gagliano A, et al. Clinical characteristics, neuroimaging findings, and neuropsychological functioning in attention-deficit hyperactivity disorder: sex differences. J of Neuroscience Res. 2022:25038. The authors of this article examined the neurological structure and functioning of ADHD across sex. Researchers found that studies included male participants at disproportionately higher levels but some differences in memory and visual-spatial deficits were found in females
Mooney MA, Bhatt P, Hermosillo RJM, Ryabinin P, Nikolas M, Faraone SV, et al. Smaller total brain volume but not subcortical structure volume related to common genetic risk for ADHD. Psychol Med. 2021;51:1279–88.
Agoalikum E, Klugah-Brown B, Wu H, Jing J, Biswal BB. Gender differences in dynamic functional network connectivity in pediatric and adult patients with attention-deficit/hyperactivity disorder. Brain Connect. 2023;2022:69.
Acknowledgements
We would like to thank the journal for the opportunity to present this information.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pagán, A.F., Huizar, Y.P., Short, T.R. et al. Adult Attention-Deficit/Hyperactivity Disorder: a Narrative Review of Biological Mechanisms, Treatments, and Outcomes. Curr Neurol Neurosci Rep 23, 451–460 (2023). https://doi.org/10.1007/s11910-023-01280-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01280-4