Abstract
Purpose of Review
Acute internal carotid artery occlusion (ICAO) is associated with high rates of morbidity and mortality, whereas chronic ICAO can present insidiously with recurrent strokes. In this review, we discuss the medical and surgical management approaches among patients with acute, subacute, and chronic ICAO.
Recent Findings
We reviewed the recent literature regarding clinical presentation of acute and chronic cases of ICAO, and discuss the current data, accepted guidelines, and prospects.
Summary
Surgical, endovascular, or a combination (hybrid) revascularization has been shown to be effective in recanalization with improved functional outcomes in patients with ICAO in comparison to systemic thrombolysis or medical therapy alone. Future prospective or randomized clinical trials are warranted to elucidate the procedural superiority for revascularization of patients with ICAO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute ischemic strokes (AIS) due to large vessel occlusions (LVO) contribute disproportionately to morbidity and mortality [1]. Patients with internal carotid artery occlusion (ICAO) manifest varied clinical presentations ranging from being asymptomatic to transient ischemic attacks (TIA) or moderate to severe ischemic strokes [2]. Among symptomatic acute ICAO patients, prevalence of atherothrombosis as an etiology ranges from 51 to 55%, whereas cardioembolic and ICA dissection contribute to 14–19% and 10–13% respectively. Acute strokes occur at a rate of 40–69% in patients with acute ICAO with high mortality (16–55%) among these patients [3]. The symptomology, risk of recurrent strokes, and prognosis are dependent on vascular factors such as chronicity of occlusion, collateral reserve, and cerebral hemodynamics [4].
The management of acute ICAO includes systemic thrombolysis and possibly urgent surgical or endovascular intervention, whereas the management of chronic ICAO involves medical optimization and elective surgical revascularization. Prior literature and clinical practice have demonstrated a lower recanalization rate (~ 23%) among AIS patients with ICAO who have undergone systemic thrombolysis resulting in poor clinical outcomes [5]. However, recent advances in diagnostic imaging, surgical, and endovascular therapy have proven efficacious for recanalization rates and functional outcomes. In this review, we discuss the clinical manifestations and management of patients with ICAO.
Clinical Presentations
Acute Internal Carotid Artery Occlusion
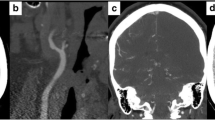
Acute ICAO manifest with ischemic syndromes involving either anterior cerebral artery (ACA) or middle cerebral artery (MCA) territories or involve arterial border zone locations (Fig. 1). Clinical manifestations due to involvement of ipsilateral ACA territory include abulia, akinetic mutism, behavioral changes, contralateral lower extremity weakness, and/or sensory disturbances. Involvement of MCA territory likely results in ipsilateral gaze preference or deviation, homonymous hemianopia, contralateral hemiparesis, hemianesthesia, and aphasia. Other stroke syndromes or stroke symptomology may also present depending on the territories affected.
71-year-old patient presented acutely with left MCA syndrome. A CT head non-contrast shows subtle left MCA territory hypodensity. B CT angiogram demonstrates left cervical ICA occlusion. C Digital subtraction angiogram shows high-grade flow-limiting stenosis of left proximal ICA with marked irregular atherosclerotic plaque. D CT perfusion shows large ischemic penumbra in left MCA territory
The pattern of occlusion plays a significant role in determining the functional outcomes. Not surprisingly, patients with a tandem occlusion in distal branches were observed to have worse functional outcomes at 3 months regardless of treatment in comparison to patients with isolated extracranial ICAO [6, 7].
The extent of cerebral injury and corresponding presentations are contingent upon multiple vascular risk factors. Clinical manifestations among patients with acute ICAO are secondary to failure of ipsilateral collateral reserve that further results in extensive cerebral injury. In acute ICAO, pre-existing collateral reserve and its availability, hemodynamics, and clot burden are critical in determining the extent of injury, clinical course, and management [3, 4, 8].
Chronic Internal Carotid Artery Occlusion
Chronic ICAO is usually found incidentally on routine neuroimaging. However, patients may present with ipsilateral ischemic events likely due to hypoperfusion or stump embolism to the distal vascular territory [3]. Patients may present with premonitory transient symptoms involving monocular vision loss, headache, transient paresthesia, or aphasia. Additionally, diagnostic imaging often demonstrates covert ipsilateral cortical or border zone infarcts.
Management
Treatment of Acute Internal Carotid Artery Occlusion
The diagnosis of AIS in the setting of ICAO typically portends a poor prognosis and hemodynamic profile remains critical among these patients. Restoration of intracranial vasculature, evaluation of collateral reserve, and maximizing cerebral perfusion via permissive hypertension are of utmost importance to prevent extension of penumbral tissue and restrict infarct burden. In acute setting, patients are allowed permissive hypertension up to recommended blood pressure (BP) of 220/120 mmHg. Patients with ICAO who are treated with IV thrombolysis (IVT) warrant strict BP monitoring parameters, i.e., < 180/105 mmHg [9].
The current standard of care among AIS patients secondary to symptomatic ICAO is centered on early reperfusion to restrict infarct growth. Although IVT is associated with lower rates of recanalization in patients with AIS due to proximal large vessel occlusion especially ICAO, use of IVT prior to endovascular therapy (EVT) is associated with increased rates of successful reperfusion, reduced total number of device passes, reduced duration of the procedure, and improved modified Rankin scale scores at 3 months [10••, 11].
EVT has evolved and become a standard of care among patients with proximal LVO, especially in patients with ICAO [12, 13]. A multicenter, retrospective study, ICARO-3, compared the post-treatment functional outcomes at 3 months among AIS patients with cervical ICAO who were treated with systemic thrombolysis and/or EVT [14]. The authors observed a significant reduction in mortality among patients treated with EVT, whereas the functional outcome at 3 months were similar in the treatment groups. Similarly, a smaller cohort Brazilian study was conducted that involved patients with symptomatic isolated cervical ICAO undergoing EVT [15]. The authors reported good neurological outcome post-EVT at 3 months without symptomatic ICH. Patients who were not amenable to carotid recanalization underwent carotid artery stenting (CAS). Endovascular recanalization with CAS of acute or subacute ICAO has a high revascularization rate and noted to be safe in selected AIS patients. Additionally, CAS in cases without tandem occlusions were observed to have a rapid neurological improvement within 24 h after CAS [16].
Treatment of Subacute and Chronic Internal Carotid Artery Occlusion
Subacute to chronic ICAO is usually incidentally diagnosed on neuroimaging, and either remain asymptomatic or could manifest as transient cerebral ischemic events. In patients with a known chronic ICAO, it is important to medically optimize stroke risk factors such as hypertension, diabetes mellitus, and hyperlipidemia. Counseling for tobacco cessation, healthy lifestyle modifications, and medication compliance remains critical along with medical management. Antithrombotic therapy remains the crux for secondary stroke prevention in patients with ICAO. Currently, the most used antithrombotic therapy is aspirin as there is limited evidence to support dual anti-platelet therapy administration for patients with subacute or chronic ICAO [17].
Interestingly, multiple randomized control trials (RCTs) including EC/IC Bypass, Japanese EC-IC Bypass Trial, JET, and COSS trials have evaluated the efficacy of surgical revascularization versus medical conservative treatment [18,19,20,21]. Although the JET trial did show a reduction in major stroke or death at 2 years in the surgical group when compared to the medical therapy group, majority of RCTs failed to establish superiority of surgical approach over medical therapy in patients with chronic ICAO [19, 22, 23]. These results were further corroborated in a Cochrane systematic review and meta-analysis which included 21 trials involving 2591 patients with symptomatic ICAO. The authors concluded that EC-IC bypass surgery in these patients was neither superior nor inferior to medical treatment alone [24].
Our Experience
According to American Heart Association/American Stroke Association guidelines, AIS patients with proximal LVO on vessel imaging are treated with IVT followed by endovascular therapy. Based on the recent AHA/ASA guidelines, we have modified our institutional IV thrombolysis protocol to incorporate use of IV Tenecteplase (TNK) as an alternative to alteplase among AIS patients with LVO undergoing endovascular thrombectomy [25]. In our limited experience, 39 AIS patients were treated with IV TNK, and of those 7 were diagnosed with ICAO on vessel imaging. We have observed ease of IV TNK administration with a single bolus dose, improved drip-ship transfer process from spoke hospitals, improved rates of recanalization, and reduced bleeding complication rates with IV TNK [26].
In acute cases of symptomatic ICAO, we use CT perfusion to assess the volume of infarct core and salvageable penumbra [27]. The cases of ICAO secondary to atherothrombosis with heavy plaque burden usually require balloon angioplasty occasionally followed by stent placement as a revascularization procedure. Patients with tandem occlusion additionally require endovascular thrombectomy and the decision is usually based on stroke severity, presence of ipsilateral collaterals, and at discretion of treating neurointerventionalist. As the risk of in situ thrombosis or stent thrombosis is high, we prefer to use Eptifibatide after balloon angioplasty and/or stent placement due to its short half-life (~ 2.5 h) in the initial 12 to 24 h, followed by dual antiplatelet therapy.
The current standard of care regarding symptomatic subacute ICAO is usually contingent upon symptom onset and stability of atherosclerotic plaque. Patients with chronic ICAO are managed conservatively with antithrombotic therapy and lifestyle modifications in outpatient stroke clinic follow-up. Conservative treatment involves treatment with antithrombotic agents, BP and cholesterol lowering medications, and counseling for lifestyle management including weight loss. However, in patients with chronic ICAO presenting with recurrent ischemic events secondary to impaired cerebrovascular reserve and insufficient collateral supply, extracranial-intracranial (EC-IC) bypass surgery is often considered. The cerebrovascular reserve capacity is studied using radioisotope single-photon emission CT and acetazolamide challenge. Select patients who have failed maximum medical therapy with significant impairment of cerebrovascular reserve are selected to undergo EC-IC bypass.
Future of Internal Carotid Artery Occlusion Management
A multicenter, prospective study in China is currently enrolling patients with symptomatic subacute or chronic ICAO to assess the technical feasibility and safety of EVT in this cohort [28•]. The primary goal is to evaluate ipsilateral TIA or stroke risk over a 2-year period among the patients who received EVT and standard medical therapy. Recently, there has been use of hybrid surgery, a combination of CEA and endovascular treatment for ICAO that has been noted to be efficacious. In this hybrid surgery, initially CEA is performed on the carotid lesion to remove hard plaques followed by endovascular treatment for the more distal carotid lesions allowing ease of traversing the true lumen and reducing device-related complications such as dissections and perforations [29•]. A small sized study reported that the recanalization of non-tapered or non-stump ICAO with hybrid surgery was more successful than EVT alone. The authors reported the recanalization rate in hybrid surgery was 88.2% as compared to EVT alone (53.3%), along with fewer perioperative complications in hybrid group [29•]. Interestingly, a systematic review objectively classified types of ICAO and statistically evaluated amenability to hybrid surgery in 389 patients with ICAO. The study identified type A (tapered) and type B (stump) ICAO with superior benefit from EVT as it showed a high rate of recanalization (95.4%) and low complication rates (13.7%). Type C (complete) ICAO from its bifurcation with supraclinoid reconstitution may benefit best from hybrid surgery as it had lower recanalization (45.7%) and higher complications (46%) in comparison to EVT alone. Type D (complete) ICAO from its bifurcation without supraclinoid reconstitution should be considered for CEA as it had much lower recanalization rate (29.8%) and higher complication rate (29.8) with hybrid surgery [30]. Additionally, there is a protocol for a systematic review in the works to examine the efficacy of surgical revascularization by EC-IC bypass for ICAO with primary endpoints of subsequent stroke and death in the perioperative and 2-year post-operative period [31].
Conclusion
The management of ICAO has long remained controversial regarding medical and surgical treatment. In patients presenting with acute ICAO with or without tandem occlusion, permissive hypertension, IV thrombolysis, and revascularization with endovascular therapy remain the gold standard for improved clinical outcomes, whereas patients with subacute to chronic ICAO, medical management involving optimizing the risk factors (i.e., hypertension, diabetes mellitus, hyperlipidemia, smoking cessation) and encouraging healthy lifestyle modifications remain critical. Medical management with antithrombotic regimens and lifestyle modification remains crucial to prevent recurrent strokes. Larger randomized clinical trials are warranted to further assess hybrid surgical options for optimal intervention.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Malhotra K, Gornbein J, Saver JL. Ischemic strokes due to large-vessel occlusions contribute disproportionately to stroke-related dependence and death: a review. Front Neurol. 2017. https://doi.org/10.3389/fneur.2017.00651.
Clagett GP, Faught WE, van Bemmelen PS, Mattos MA, Hodgson KJ, Barkmeier LD, Ramsey DE. Presentation and natural history of internal carotid artery occlusion. J Vasc Surg. 1993;18:512–24.
Malhotra K, Goyal N, Tsivgoulis G. Internal carotid artery occlusion: pathophysiology, diagnosis, and management. Curr Atheroscler Rep. 2017. https://doi.org/10.1007/s11883-017-0677-7.
Malhotra, Liebeskind. Collaterals in ischemic stroke. In: Malhotra, Konark; Liebeskind, David S. | download. https://ur.booksc.eu/book/80863057/ddc2de. Accessed 23 Sep 2021.
Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, José A-S, Molina CA. Tandem internal carotid artery/middle cerebral artery occlusion. Stroke. 2006;37:2301–5.
Kim DJ, Kim DI, Byun JS, Jung JY, Suh SH, Kim EY, Heo JH. Intra-arterial thrombolytic therapy for hyperacute ischemic stroke caused by tandem occlusion. Cerebrovasc Dis. 2008;26:184–9.
Ozdemir O, Bussière M, Leung A, Gulka I, Lee D, Chan R, Spence JD, Pelz D. Intra-arterial thrombolysis of occluded middle cerebral artery by use of collateral pathways in patients with tandem cervical carotid artery/middle cerebral artery occlusion. Am J Neuroradiol. 2008;29:1596–600.
Persoon S, Luitse MJA, de Borst GJ, et al. Symptomatic internal carotid artery occlusion: a long-term follow-up study. J Neurol Neurosurg Psychiatry. 2011;82:521–6.
Kim SM, Woo HG, Kim YJ, Kim BJ. Blood pressure management in stroke patients. J Neurocrit Care. 2020;13:69–79.
•• Goyal N, Tsivgoulis G, Pandhi A, et al. Impact of pretreatment with intravenous thrombolysis on reperfusion status in acute strokes treated with mechanical thrombectomy. J NeuroIntervent Surg. 2019;11:1073–1079. IVT is associated with lower rates of recanalization in patients with AIS due to proximal large vessel occlusion; however, use of IVT prior to EVT is associated with increased rates of successful reperfusion, reduced total number of device passes, reduced duration of the procedure, and improved mRS scores.
Katsanos AH, Malhotra K, Goyal N, et al. Intravenous thrombolysis prior to mechanical thrombectomy in large vessel occlusions. Ann Neurol. 2019;86:395–406.
Lin MP, Tsivgoulis G, Alexandrov AV, Chang JJ. Factors affecting clinical outcome in large-vessel occlusive ischemic strokes. Int J Stroke. 2014;10:479–84.
Mokin M, Kass-Hout T, Kass-Hout O, Dumont TM, Kan P, Snyder KV, Hopkins LN, Siddiqui AH, Levy EI. Intravenous thrombolysis and endovascular therapy for acute ischemic stroke with internal carotid artery occlusion. Stroke. 2012;43:2362–8.
Paciaroni M, Inzitari D, Agnelli G, et al. Intravenous thrombolysis or endovascular therapy for acute ischemic stroke associated with cervical internal carotid artery occlusion: the ICARO-3 study. J Neurol. 2014;262:459–68.
Castro-Afonso De, Henrique L, et al. Endovascular reperfusion for acute isolated cervical carotid occlusions: the concept of ‘hemodynamic thrombectomy’. Interventional Neurology. 2018;8(1):27–37. https://doi.org/10.1159/000493021.
Jovin Tudor G, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke. 2005;36(11):2426–2430. https://doi.org/10.1161/01.str.0000185924.22918.51.
Paciaroni M, Bogousslavsky J. Antithrombotic therapy in carotid artery stenosis: an update. Eur Neurol. 2014;73:51–6.
EC/IC Bypass Study Group. Failure of extracranial–intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial. N Engl J Med. 1985;313(19):1191–200.
Gertler JP, Cambria RP. The role of external carotid endarterectomy in the treatment of ipsilateral internal carotid occlusion: Collective review. J Vasc Surg. 1987;6:158–67.
A; OKO [JET study (Japanese ec-ic Bypass Trial)]. In: Nihon rinsho. Japanese Journal of clinical medicine. https://pubmed.ncbi.nlm.nih.gov/17461199/. Accessed 23 Sep 2021.
Grubb RL, Powers WJ, Derdeyn CP, Adams HP, Clarke WR. The carotid occlusion surgery study. Neurosurg Focus. 2003;14:1–7.
Group EIBS. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial. N Engl J Med. 1985;313:1191–200.
Powers WJ, Clarke WR, Grubb RL, Videen TO, Adams HP, Derdeyn CP, COSS Investigators for the. Extracranial-Intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia. JAMA. 2011;306:1983.
Fluri F, Engelter S, Lyrer P. Extracranial-intracranial arterial bypass surgery for occlusive carotid artery disease. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.cd005953.pub2.
Powers WJ, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):2019. https://doi.org/10.1161/str.0000000000000211.
Hackett CT, et al. Abstract 25: Tenecteplase is safe and efficacious in telestroke patients with confirmed large vessel occlusions. Stroke. 2022. www.ahajournals.org/doi/10.1161/str.53.suppl_1.25.
Brott TG, et al. “Carotid revascularization for prevention of stroke: carotid endarterectomy and carotid artery stenting. Mayo Clin Proc. 2004;79(9):1197–208. https://doi.org/10.4065/79.9.1197.
• Endovascular recanalization and standard medical management for symptomatic nonacute intracranial artery occlusion trial - full text view. In: Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04864691. Accessed 23 Sep 2021. A multicenter, prospective study in China evaluating symptomatic subacute or chronic ICAO to assess technical feasibility and safety of EVT with primary goal to evaluate ipsilateral composite TIA/stroke risk in patients who received EVT and standard medical therapy (SMT) versus SMT alone.
• Li J, Wang C, Zou S, Liu Y, Qu L. Hybrid surgery for nontaper or nonstump lesions in symptomatic subacute or chronic internal carotid occlusion: a better solution. World Neurosurg. 2019;122: e1416–25. https://doi.org/10.1016/j.wneu.2018.11.075. Recently, hybrid surgery, a combination of CEA and EVT, for ICAO has been noted to be efficacious by allowing ease of traversing the true lumen and reducing device related complications.
Zanaty M, Roa JA, Jabbour PM, Samaniego EA, Hasan DM. Recanalization of the chronically occluded internal carotid artery: review of the literature. World Neurosurg: X, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/31872191/.
Bai X, Feng Y, Yang K, Wang T, Luo J, Wang X, Ling F, Ma Y, Jiao L. Extracranial-intracranial bypass surgery for occlusive atherosclerotic disease of the anterior cerebral circulation: protocol for a systematic review and meta-analysis. Syst Rev. 2020. https://doi.org/10.1186/s13643-020-01325-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors do not have existing conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Stroke.
Rights and permissions
About this article
Cite this article
Saini, H., Cerejo, R., Williamson, R. et al. Internal Carotid Artery Occlusion: Management. Curr Neurol Neurosci Rep 22, 383–388 (2022). https://doi.org/10.1007/s11910-022-01201-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-022-01201-x