Abstract
Purpose of Review
Subcortical structures have long been thought to play a role in language processing. Increasingly spirited debates on language studies, arising from as early as the nineteenth century, grew remarkably sophisticated as the years pass. In the context of non-thalamic aphasia, a few theoretical frameworks have been laid out. The disconnection hypothesis postulates that basal ganglia insults result in aphasia due to a rupture of connectivity between Broca and Wernicke’s areas. A second viewpoint conjectures that the basal ganglia would more directly partake in language processing, and a third stream proclaims that aphasia would stem from cortical deafferentation. On the other hand, thalamic aphasia is more predominantly deemed as a resultant of diaschisis. This article reviews the above topics with recent findings on deep brain stimulation, neurophysiology, and aphasiology.
Recent Findings
The more recent approach conceptualizes non-thalamic aphasias as the offspring of unpredictable cortical hypoperfusion. Regarding the thalamus, there is mounting evidence now pointing to leading contributions of the pulvinar/lateral posterior nucleus and the anterior/ventral anterior thalamus to language disturbances. While the former appears to relate to lexical-semantic indiscrimination, the latter seems to bring about a severe breakdown in word selection and/or spontaneous top-down lexical-semantic operations.
Summary
The characterization of subcortical aphasias and the role of the basal ganglia and thalamus in language processing continues to pose a challenge. Neuroimaging studies have pointed a path forward, and we believe that more recent methods such as tractography and connectivity studies will significantly expand our knowledge in this particular area of aphasiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The basal ganglia are composed of five principal deep brain structures: the caudate nucleus and putamen (which comprise the striatum), globus pallidus, subthalamic nucleus, and substantia nigra (the latter located in the midbrain). This set of nuclei is intertwined in a broader basal ganglia-thalamocortical network that takes part in motor, cognitive, and limbic functions. The striatum is the principal input structure of the basal ganglia and receives afferents from the cerebral cortex, thalamus, and brain stem. After a series of internally reciprocal projections, the basal ganglia transmit their output to the thalamic nuclei that, in turn, project this output back to the same areas of the frontal cortex from which the input originated, thus closing a fronto-basal ganglia-thalamic-frontal loop [1].
The debate on the role of subcortical structures in language processing has emerged in the second half of the nineteenth century, but it is yet far from a definitive closure. Some scholars [2] claim that subcortical structures play no specific role in language processing except for the thalamus. Other authors [3, 4] defend that “subcortical aphasia” exists as a unique clinical entity distinguishable from the classical cortical aphasias, although most researchers agree that its pathophysiology and neuropsychology are not well understood. Moreover, the intrinsic complexity of subcortical circuits has led to a dichotomization of subcortical aphasias as “thalamic” and “non-thalamic” (the latter referring to aphasias caused by lesions in the basal ganglia and subcortical white matter pathways).
As early as 1872, Broadbent [5] proposed that the basal ganglia “generated” words in the same way that it did with motor acts, but scholars did not fully embrace this idea. Kussmaul in 1877 [6] attributed a purely motor role to the basal ganglia while Carl Wernicke, in 1874 [7] and Lichtheim, in 1885 [8], defended the notion that subcortical lesions led to language impairment only by disruption of the connecting pathways among the cortical language areas, thus excluding any direct involvement of the basal ganglia and thalamus in higher mental functions.
One of the earliest descriptions of language alterations caused by subcortical lesions was made by Pierre Marie in 1906 [9], who labeled as “anarthria” the speech impairment caused by lesions in the caudate nucleus, putamen, internal capsule, and thalamus. Later in the twentieth century, studies conducted in patients with Parkinson’s disease submitted to stereotactic surgery led to the observation that either the lesion or stimulation of the thalamus and globus pallidus provoked language alterations during and after surgery. Thus, in 1959, Penfield and Roberts [10] suggested that the thalamus played an integrative role in language. A few years later, Schuell et al. [11] stated that the thalamus was involved in the preverbal feedback concerning the adequacy of formulated responses.
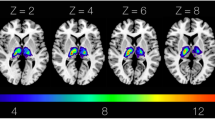
However, significant advances in the study of subcortical lesions followed the advent of neuroimaging techniques, which allowed the precise location of subcortical lesions in larger cohorts of subjects with aphasia. Computerized tomography (CT) and magnetic resonance imaging (MRI) have shed light on the relationship between deep cerebral lesions and aphasic symptoms. Functional neuroimaging studies, such as single-photon emission computerized tomography (SPECT), positron emission tomography (PET), and functional MRI (fMRI), and electrophysiology-based methods (cortical evoked potential), further expanded our knowledge about the role of subcortical structures in language processing. In this paper, we review the main anatomo-clinical aspects regarding subcortical aphasias following stroke.
Non-thalamic Aphasias
Non-thalamic aphasia is by far the most controversial subtype of subcortical aphasia. There are several complications when it comes to studying anatomo-clinical correlations involving an ensemble of structures that are so tightly and reciprocally connected. For this reason, there is little consensus regarding the clinical findings and pathophysiologic mechanisms proposed to explain the role of non-thalamic subcortical structures in aphasias. We begin by describing the heterogeneous clinical findings following basal ganglia lesions reported in the literature. Subsequently, the four main theoretical frameworks that attempt to address all clinical and neuroimaging findings in language disturbances following basal ganglia lesions are discussed.
Clinical Findings in Non-thalamic Aphasias
In a recent comprehensive review [12], we tried to track as precisely as possible the correlation between the site of lesion and clinical findings in cases of pure basal ganglia lesions published in a range of 50 years (1966–2016). Our review encompassed 303 patients and disclosed two main problems in establishing anatomo-clinical correlations regarding vascular non-thalamic aphasias: (a) rarely one can find isolated lesions impinging over a single structure due to intrinsic characteristic of basal ganglia vascularization; (b) basal ganglia structures are highly interconnected in a network involving reciprocal inhibition and stimulation; thus the effects of a given lesion in one structure may lead to multiple (and sometimes opposite) effects in neighboring connected structures. Therefore, finding specific clinical patterns in basal ganglia lesions is a challenging task. However, there are some consistencies as displayed in Table 1. In about one-third of patients, no language alteration was found regardless of lesion site, especially in isolated lesions of the caudate nucleus (56.2%). Naming deficits occurred in almost half of the patients and were particularly prominent in lesions of the putamen (60.4%) and lentiform nucleus (59.3%). Comprehension and repetition deficits also appeared in nearly one-third of patients, particularly in lenticular and striatocapsular lesions. The highest incidence of language disturbances was found in striatopallidal lesions (75%), but the total sample is too small (4 patients) to draw inferences about this particular damage locus. For a more comprehensive description of the lesion-aphasia correlation profile, please refer to Table 3 in the Appendix.
Theoretical Frameworks in Non-thalamic Aphasias
-
1)
Disconnection syndrome: according to this proposal, basal ganglia lesions would disrupt language processing by producing a disconnection between Broca’s and Wernicke’s areas. However, this approach implies a role of periventricular white matter (PVWM) rather than the basal ganglia per se in aphasic symptoms. Thus, damage in pathways connecting the medial geniculate body, temporal lobe (in the temporal isthmus), and the callosal auditory association pathways in the posterior PVWM might account for comprehension deficits. Damage to the external capsule, extreme capsule, and arcuate fasciculus would be critical in repetition disturbances and phonemic paraphasias. Lesions in the anterosuperior PVWM would lead to transcortical motor aphasia (TCMA) by disrupting pathways linking Broca’s area to the supplementary motor cortex. Speech disorders can be found in lesions of the superior PVWM and genu of the internal capsule, where descendent corticobulbar fibers run [25]. Naeser et al. [65, 66] also emphasized the role of the PVWM as a major factor leading to language alterations by describing lesions in the putamen and internal capsule that impaired articulation and naming (in anterosuperior PVWM lesions), comprehension deficits and paraphasias (in posterior PVWM lesions), and global aphasia (associated with more extensive anterior, posterior, and superior PVWM lesions).
-
2)
Direct role of basal ganglia in language processing: after the description of nine patients exhibiting non-fluent aphasia with dysarthria and dysprosodia following isolated striatocapsular infarcts, Damasio et al. [3] postulated that aphasia symptoms might result from deficits in movement programming and perception organization performed by the striatum; nevertheless, the authors also recognized that the interruption of white matter pathways connecting the basal ganglia to prefrontal, frontal, and temporal cortices due to internal capsule damage would play a pivotal role in the language disturbances. Later, Cappa et al. [4] and Mega and Alexander [41] proposed that compromised frontostriatal systems would underlie aphasia symptoms such as non-fluency and anomia by disrupting lexical selection mechanisms. Finally, according to Crosson [67, 68], the role of the basal ganglia in semantically induced lexical selection would be that of engaging or disengaging thalamic modulation over the language cortex through caudate-pallidal-thalamic interactions, which might over-inhibit (caudate nucleus lesions) or disinhibit (globus pallidus lesions) the thalamus. Wallesch and Papagno [69] also postulated a monitoring role of the basal ganglia in lexical selection. Activation of the striatum and thalamus (along with parietal and frontal areas) was documented by fMRI in an ambiguity-resolution task, thus reinforcing the hypothesis that the basal ganglia participate in semantic verification and motor programming preselected language segments [70]. A series of studies by Copland et al. [71,72,73] have demonstrated the role of the basal ganglia in the resolution of lexical ambiguities through selective attentional engagement subserved by fronto-subcortical systems.
-
3)
Dysfunction of remote areas by subcortical deafferentation (diaschisis): the well-known existence of functional impairment in intact regions of the brain that connect to a primary lesion site, or diaschisis, led to the notion that cortical lesions are still ultimately responsible for language impairment, even when the primary lesion is circumscribed to subcortical structures. Studies using SPECT have demonstrated that the long-term persistence of neuropsychological impairment (such as neglect and aphasia) is consistently related to the degree of cortical hypoperfusion associated with subcortical lesions, even in the absence of identifiable structural lesions in the cortex [27, 29].
-
4)
Cortical hypoperfusion: a new perspective to explain subcortical aphasia secondary to basal ganglia and PVWM damage emerged from studies investigating cerebrovascular disease and cognitive impairment. Usually, ischemic striatocapsular lesions are caused by occlusion in the proximal segment of the middle cerebral artery (MCA), or less frequently, occlusion of the internal carotid artery (ICA). Therefore, the amount of cortical neuronal loss consequent to the occurrence of an infarct in these territories is determined by the promptness of flow restoration to the affected area, either by MCA recanalization or an efficient anastomotic circulation. Thus, circulatory dynamics plays a crucial role in the development and recovery from aphasia following basal ganglia injury [74]. Nadeau and Crosson [2] have further developed this theory by considering that (a) the MCA is responsible for the irrigation of the perisylvian cortex; (b) the basal ganglia receive blood supply from lenticulostriate branches, which are terminal branches. It follows that MCA or ICA obstruction is prone to cause greater ischemic damage in lenticulostriate territories while cortical areas may be spared due to an adequate anastomotic circulation, which prevents the occurrence of massive cortical infarction. However, a transient neuronal dysfunction may occur, inducing aphasic symptoms, albeit without evidence of cortical structural alterations. As for cases involving the posterior limb of the internal capsule (supplied by the anterior choroidal artery), aphasic symptoms resemble those of a “thalamic aphasia” due to a thalamic-temporal disconnection. Hemorrhagic strokes, in turn, might cause transient neuronal dysfunction (with consequent language impairment) through the pressure exerted by the clot in the adjacent cortex.
Degenerative diseases such as Parkinson’s and Huntington’s disease, which affect the nigrostriatal system and caudate nucleus, respectively, are alternate models for the role of basal ganglia in language processing. Indeed, impairment in verbal fluency, naming, and syntactic processing were described in both conditions [75, 76]. However, it should be pointed that the degenerative process is not restricted to the basal ganglia but also spreads to the cerebral cortex, especially the frontal lobes [77, 78]
The basal ganglia belong to a network involved in executive functions and acquisition of behaviors both in motor and high-order functions, including cognitive processes and empathic and socially appropriate behaviors [1]. Therefore, it is not surprising that speech planning [79] and prosodic processing [80] may be affected by disorders in the basal ganglia. Moreover, recent theories implicate the striatum in sequential and computational aspects of language processing, combinatorial rule application, and procedural learning, like those associated with morphology and syntax [81,82,83]
Considering the complexity of the subcortical circuitry, we believe that a new promising approach to the problem of subcortical aphasia may rely on connectivity studies. Xu et al. [84•], targeting Broca’s and Wernicke’s areas as regions of interest, described that increase in intrahemispheric and decrease in interhemispheric functional connectivity were associated with better recovery from basal ganglia aphasia. They speculate that this finding may be related to a possible role of cortico-subcortical circuits in favoring intrahemispheric (compensatory) mechanisms that contribute to language recovery.
Thalamic Aphasia
The thalamus is so central to language that many authors stand by the idea that it is the only subcortical center for linguistic processing [67]. Notwithstanding, this structure is subdivided into several different nuclei, and not all of them are thought to provoke aphasia. Primarily, focal lesions that consistently engender language symptoms appear to be located to the pulvinar/lateral posterior thalamus, the anterior thalamic nuclei (ATN), and the ventral anterior nucleus (VA) [85,86,87] (Table 2).
In order to cover each of these nuclei, we introduce the overall semiological fingerprint of thalamic aphasia: De Witte et al. [94] reviewed a sample of 465 thalamic infarction patients and described their foremost traits: out of “1) fluent output, 2) normal or mildly impaired comprehension skills, 3) normal or mildly impaired repetition, 4) moderate to severe anomia characterized by semantic paraphasias, neologisms, and perseverations, 5) hypophonia and/or mild articulation deficits and 6) reduction of spontaneous speech or verbal aspontaneity”, 63.6% of left infarction cases conformed to at least four of these criteria. In full accordance, aphasia resulting from thalamic insult is best recognized for its fluent, paraphasic production, which may degenerate into jargon, with perseverations and preserved repetition skills [56, 67, 85, 107]. Although the non-fluent language is not as prevalent, it is important to note that word-finding is harshly affected, and spontaneous speech often plummets [56, 85, 94].
Furthermore, one must also point out that these deficits are mostly lexical-semantic in nature. Nevertheless, each nucleus portrays a slightly different profile in regard to these symptoms.
The Pulvinar
The pulvinar’s partaking in language is conspicuous and most unsurprising, seeing that it projects eminently to temporoparietal cortices as well as Broca’s area [109]. For instance, a recent study reported that resting-state functional connectivity between the left pulvinar, left middle temporal gyrus, and left inferior parietal lobule was significantly correlated with picture naming often brought down a few notches by thalamic infarction [110]. Indeed, some theoretical models on language and thalamic aphasia place great importance on the pulvinar. Hart et al. [111] ascribed to it a leading role in lexical-semantic retrieval, and Nadeau and Crosson [2] did so to thalamic aphasia. Accordingly, lesions to the pulvinar/LP are prone to cause semantic paraphasias and fluent aphasia, as well as naming deficits [56, 92, 93, 104, 112, 113], albeit other aphasic symptoms are also common. However, we should consider that this nucleus’s input supply can also be cut short by compromises to other structures. Thus, through the pulvinar alone, various focal lesions hold the potential to impinge detrimentally on language cortices, thalamic, or otherwise. For example, Nadeau and Crosson [2] also proposed that basal ganglia and/or nucleus reticularis damage should cause subcortical aphasia mainly through the pulvinar, which would gate inputs in turn to the language cortices.
The pulvinar may support fine semantic discrimination similar to that already described in sensory processes: pulvinar damage and deactivations consistently undermine visual discrimination tasks [114]. This structure contributes to eliciting the mismatch negativity for tone discrimination in vivo [115], thus helping to resolve competition between representations. We should then consider that the pulvinar may play a role in paraphasia, neologisms, and jargon through similar disorganization of fine semantic discrimination in the language cortices.
Anterior Nuclei
It grows increasingly evident that damage to the anterior thalamic nuclei (ATN) and/or ventral anterior thalamus (VA) robustly results in a sharp plunge in linguistic output (and perseverations): the lack of spontaneous speech and verbal fluency, anomia, as well as the occasional non-fluent aphasia, are most notably observed in anterior thalamic lesions [85, 87, 88, 96, 98, 100, 102, 103, 105, 116, 117]. Likewise, this seems to match an idea proposed by Cox and Heilman [118] about their thalamic aphasia case study, namely, the patient’s lexical-semantic representations seemed intact, but his ability to spontaneously access them was hampered. Such a concept could be intrinsically linked to what may be referred to as a robust disruption of self-initiated generation of language in anterior thalamic aphasia. Furthermore, this may also manifest in perseverations [100] coupled to word-finding difficulties and hypophonia. The study by Fritsch et al. [87] claimed that “(1) aphasic symptoms after an isolated lesion to the thalamus (ITL) are rare (6/52 patients) and that (2) aphasic symptoms after ILT are strongly associated with isolated left anterior thalamic lesion location”. Hence, not only do ATN lesions impinge on generation in language processes, but they are also some of the most common.
Notably, the ATN are thought to propagate theta activity and mediate information transfer between the frontal and (predominantly medial) temporal lobes [119]. In turn, in controlled processing paradigms, the theta range is tightly associated with semantic distance [120, 121] and lexical-semantic retrieval [122]. Frontal and temporal theta activity was linked to word-finding during fluency in a recent study [123]. Leszczyńsk and Staudigl [124] further speculated that the ATN might prop up memory-guided attention. Such data seem to endorse that ATN insults would cut short the spontaneous initiation of more volitional top-down predictions/verbal search, likely through frontotemporal theta synchronizations.
The Motor Thalamus
The VA is pronouncedly connected with Broca’s area and the pre-supplementary motor area (pre-SMA) [125]. Mounting evidence points to the primary effect of VA lesions being a reduction in speech output and fluency, and the incidence of perseverations. Analogically, perseverations of incorrect words in language tasks could be induced by stimulation of more anterior portions of the VL [67, 126,127,128]. Paraphasia is another very robust feature [86, 87, 129], and hypophonia is a fairly common outcome (which is reminiscent of parkinsonian patients, where VA function is altered) [100, 130].
The idea that word selection and retrieval undergo VA and/or pre-SMA processing is not novel [68, 101, 111, 120]. As stated earlier when we referred to the direct role of basal ganglia in language processing, Crosson et al. [68] described a loop consisting of left pre-SMA-dorsal caudate-VA (the GPi theoretically being suppressed by the striatum) that was ignited during word generation, further conjecturing that this circuit would be responsible for selection processes. A role in selection is also concordant with the VA’s intimate connections with the IFG and pre-SMA, which are thought to perform these functions [109]. Since the frontal aslant tract also bridges both, this may implicate the triad in a circuit for word selection; indeed, recent evidence indicates that word-finding difficulties and language in thalamic stroke were strongly correlated with pre-SMA and IFG abnormalities in SPECT recordings [131]. Furthermore, VA lesions might oppose the initiation and/or suppression of speech/selection [132] through a premotor cortex-thalamic network. This idea seems pertinent given that ATN/VA aphasia is fluent despite the reduction in spontaneous speech and the increase in perseverations [100, 104, 108, 119]. Conversely, an MRI study by Nishio et al. [133] claimed that several structures in the rostral vicinity of the ventral intermediate nucleus (VIM) are important for word processing. Tractography analyses in patients with anterior thalamic infarcts have shown that lexical-semantic deficits were related to the disconnection of language-relevant frontal and temporal cortical areas (the middle frontal gyrus) from ventral anterior and ventral lateral thalamic regions.
In that vein, an interesting finding is that parkinsonian patients take a longer time to disambiguate words, lengthening priming of contextually incongruent meanings behaviourally, and electrophysiologically word selection is delayed [134, 135]. When a representation is ambiguous, one of the meanings is favored by contextual variables and word frequency; the VA-VL may respond accordingly with linear tonic transmissions, biasing word selection in the pre-SMA and IFG [136]. Conversely, when the VA is constantly suppressed in Parkinson’s disease, both weak and stronger meanings drive all-or-none bursting amplified by the VA-VL to outlast their due timing, causing erasure of salience [137] and making selection unviable. It would be interesting to explore whether a similar suppression (“disfacilitation” or hyperpolarization) arising from thalamic insults would hamper word selection in a kindred fashion.
Mediodorsal Nucleus
Finally, the mediodorsal nucleus is not commonly linked to aphasia, but it is noteworthy that damage here handicaps verbal memory and causes some measure of anomia, perseveration, and executive deficits [56, 88, 89, 138].
Deep Brain Stimulation Studies
Deep brain stimulation (DBS), a treatment currently used in many neurological and psychiatric disorders, has opened a window of opportunity for observing in vivo human function of subcortical structures in several motor and cognitive domains [139]. The method uses implanted electrodes that deliver current to the brain and also permits electrophysiological recordings of deep brain structures while the individual is awake and capable of performing motor and cognitive tasks. For this reason, DBS procedures performed on patients with motor disturbances have provided an interesting set of data regarding basal ganglia and thalamic participation in language processing.
Basal Ganglia
Nowadays, most DBS procedures on Parkinson’s disease patients target the subthalamic nucleus (STN) and globus pallidus pars interna (GPi) [140]. Post-operative longitudinal language assessment showed that DBS intervention targeting both structures was associated with impairment in phonemic and semantic verbal fluency in several studies [141,142,143]. Moreover, 35–90-Hz stimulation in the STN was correlated with switching (change from one semantic category or letter to another) during VF semantic and phonemic tasks [144]. Wojtecki et al. [145] found increases in 6–12-Hz local field potential (LFP) activity in the STN during a verbal generation task (especially in the ventromedial STN), which was linked to an enhanced coherence between the STN and frontal areas at 6–7 Hz. In the same vein, Hohlefeld et al. [146] described a correlation between lexical accuracy and cortico-subthalamic coherence at the 14–35-Hz range. These data provide evidence for cortex-basal ganglia synchronization in language processing.
Thalamus
Word selection is vulnerable to VA-VL lesions, especially the more anterior portions; a neighboring area, the VIM, is often targeted for DBS treatment of essential tremor, and its stimulation, through current spread, can encroach on the VA-VL complex [147], thereby modulating the latter’s function. This target is convenient for probing a role in language, seeing that VIM infarct per se was shown not to correlate with language symptoms.
A meta-analysis unraveled that both lesions and stimulation thalamic surgery “produce adverse effects on speech. Left-sided and bilateral procedures are approximately 3-fold more likely to cause speech difficulty” [148]. VIM stimulation slowed down verbal fluency, increasing intra-cluster pauses (especially in phonemic fluency) [149]. Intuitively, intra-cluster choices should suffer more significant interference from neighboring nodes, therefore leaving room only for the most salient alternatives to outstand for selection. Consonantly, recent findings documented that VIM stimulation increases the frequency of lexical items in spontaneous speech [150], suggestive of unavailability of weaker tokens, which also applies to thalamic aphasia [101]. Tiedt et al. [145] attributed their findings to a perturbation of thalamic interareal binding [151], “resulting in a lower network connectivity state, reduced lexical activation spread and, finally, slower word production”. Indeed, a recent study documented that acute ischemic thalamic stroke was linked to cortical dysconnectivity [152].
Another recent study assessing left VA-VL (particularly the VA and VLa) stimulation showed that it suppressed verbal abstraction [152]; the same was not true of the VIM. The authors underscored that the VA-VLa receives its principal inputs from the GP and SNr while projecting extensively to the IFG (which supports verbal abstraction), consequently leading to repercussions for verbal abstraction ability. Similarly, perseveration of incorrect words was also induced by stimulation of the VLa in a few studies [67, 127, 128]. Conversely, the VLp is intertwined with cerebellar circuitry and communicates with the non-cognitive motor cortex. In line with that are classic studies by Ojemann [126, 153]: 60-Hz stimulation of the VL prolonged the duration of oral reading responses with slurring and motor distortions (and some other motor-related findings came out concerning VIM stimulation) [154]. Another example of language increments is found in Pedrosa et al. [155]: 10-Hz stimulation of the VL enhanced phonemic and semantic fluency, whereas 120–150-Hz stimulation impaired them, suggesting short-term synaptic depression with high-frequency stimulation [156]. Paradoxically, anomia ensues from 60-Hz VL stimulation most reliably when electrodes are placed near the intralaminar groups [126, 153]. However, there are findings that 50-Hz stimulation of the centromedian nucleus actually enhances motor speech and semantic retrieval [157, 158].
Conclusions
As a conclusion of this review, we believe that some issues are worth mentioning: firstly, we focused our review on left hemispheric lesions; however, it does not imply that language alterations do not occur in subcortical right hemisphere lesions, in both left and right-handed individuals. On the contrary, there are several reports of language impairment following right basal ganglia and thalamic lesions. The findings are heterogeneous regarding right basal lesions, and aphasia occurred mainly in left-handed patients [12]. In right thalamic lesions, lexico-semantic impairment, as revealed by anomia and paraphasias, can be more consistently found, although in most cases there are no reports of patients’ handedness [94, 95]. Secondly, we must take into account that the classification non-thalamic × thalamic aphasias only makes sense (if any) from the structural/vascular perspective, given that language is organized on a multisynaptic network that involves the neocortex, basal ganglia, thalamus, and also the cerebellum forming a closed-loop circuit [159•]. Consequently, an isolated structural lesion may impact the whole functional system, although with different intensity and patterns, irrespectively of its location. Therefore, it is our opinion that in the future, subcortical aphasia studies will benefit primarily from tractography and cortical connectivity studies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wichmann T, DeLong MR. The basal ganglia. In: Kandel ER, Schwartz JH, Jessell TM, Siegelbaum SA, Hudspeth AJ, editors. Principles of Neural Science. 5th ed. New York: McGraw-Hill; 2013. p. 982–98.
Nadeau SE, Crosson B. Subcortical aphasia. Brain Lang. 2000. https://doi.org/10.1006/brln.1997.1707.
Damasio AR, Damasio H, Rizzo M, Varney N, Gersh F. Aphasia with nonhemorrhagic lesions in the basal ganglia and internal capsule. Arch Neurol. 1982. https://doi.org/10.1001/archneur.1982.00510130017003.
Cappa SF, Cavallotti G, Guidotti M, Papagno C, Vignolo LA. Subcortical aphasia: two clinical-CT correlation studies. Cortex. 1983. https://doi.org/10.1016/s0010-9452(83)80016-1.
Broadbent G. On the cerebral mechanisms of speech and thought. Med Chir Trans. 1872. https://doi.org/10.1177/095952877205500108.
Kussmaul A. Disturbances of speech. Cyclopedie Pract Med. 1877;14:581.
Wernicke C. Der aphasische Symptomencomplex. Breslau: Cohn & Weigert; 1874.
Lichtheim L. On aphasia. Brain. 1885;7:433–84.
Marie P. The third left frontal convolution plays no special role in the function of language. Semaine Médicale. 1906;26:241–7.
Penfield W, Roberts L. Speech and brain mechanisms. Princeton: Princeton University Press; 1959.
Schuell H, Jenkins JJ, Jimenez-Pabon E. Aphasia in adults. New York: Harper & Row; 1965.
Radanovic M, Mansur LL. Aphasia in vascular lesions of the basal ganglia: a comprehensive review. Brain Lang. 2017. https://doi.org/10.1016/j.bandl.2017.05.003.
Cambier J, Elghozi D, Strube E. Hémorragie de la tête du noyau caudé gauche. Désorganisation du discours et de l’expression graphique, perturbations des séries gestuelles [Hemorrhage of the head of the left caudate nucleus: disorganization of speech and graphic expression, and disturbances in gestures (author's transl)]. Rev Neurol (Paris). 1979;135:763–74.
Alexander MP, LoVerme SR Jr. Aphasia after left hemispheric intracerebral hemorrhage. Neurology. 1980. https://doi.org/10.1212/wnl.30.11.1193.
Metter EJ, Riege WH, Hanson WR, Kuhl DE, Phelps ME, Squire LR, et al. Comparison of metabolic rates, language, and memory in subcortical aphasias. Brain Lang. 1983. https://doi.org/10.1016/0093-934x(83)90054-8.
Wallesch CW, Kornhuber HH, Brunner RJ, Kunz T, Hollerbach B, Suger G. Lesions of the basal ganglia, thalamus, and deep white matter: differential effects on language functions. Brain Lang. 1983. https://doi.org/10.1016/0093-934x(83)90046-9.
Puel M, Demonet JF, Cardebat D, Bonafé A, Gazounaud Y, Guiraud-Chaumeil B, Rascol A. Aphasies sous-corticales. Etude neurolinguistique avec scanner X de 25 cas [Subcortical aphasia. Neurolinguistic and x-ray computed tomography studies of 25 cases]. Rev Neurol (Paris). 1984;140:695–710.
Stein RW, Kase CS, Hier DB, Caplan LR, Mohr JP, Hemmati M, Henderson K. Caudate hemorrhage. Neurology. 1984. https://doi.org/10.1212/wnl.34.12.1549.
Vergara F, Verdugo R, Guzmán N. Subcortical aphasia in striatal vascular lesion. Rev Chil Neuro-Psiquiat. 1984;22:215–20.
Fromm D, Holland AL, Swindell CS, Reinmuth OM. Various consequences of subcortical stroke. Prospective study of 16 consecutive cases. Arch Neurol. 1985. https://doi.org/10.1001/archneur.1985.04060090025009.
Tanridag O, Kirshner HS. Aphasia and agraphia in lesions of the posterior internal capsule and putamen. Neurology. 1985. https://doi.org/10.1212/wnl.35.12.1797.
Wallesch CW. Two syndromes of aphasia occurring with ischemic lesions involving the left basal ganglia. Brain Lang. 1985. https://doi.org/10.1016/0093-934x(85)90090-2.
Lieberman RR, Ellenberg M, Restum WH. Aphasia associated with verified subcortical lesions: three case reports. Arch Phys Med Rehabil. 1986;67:410–4.
Olsen TS, Bruhn P, Oberg RG. Cortical hypoperfusion as a possible cause of 'subcortical aphasia'. Brain. 1986. https://doi.org/10.1093/brain/109.3.393.
Alexander MP, Naeser MA, Palumbo CL. Correlations of subcortical CT lesion and aphasia profiles. Brain. 1987. https://doi.org/10.1093/brain/110.4.961.
Mehler MF. A novel disorder of linguistic expression following left caudate nucleus infarction. PP-153. Neurology. 1987;37:167.
Perani D, Vallar G, Cappa S, Messa C, Fazio F. Aphasia and neglect after subcortical stroke. Brain. 1987. https://doi.org/10.1093/brain/110.5.1211.
Viader F, Lechevalier B, Eustache F, Rollet I, Bouvard G, Petit MC. Un cas d’aphasie avec troubles du discours par infarctus des noyaux caudé et lenticulaire gauches. [A case of aphasia with speech disorders by infarction of the left caudate nucleus and putamen]. Rev Neurol (Paris). 1987;143:814–22.
Vallar G, Perani D, Cappa SF, Messa C, Lenzi GL, Fazio F. Recovery from aphasia and neglect after subcortical stroke: neuropsychological and cerebral perfusion study. J Neurol Neurosurg Psychiatry. 1988. https://doi.org/10.1136/jnnp.51.10.1269.
Guarnaschelli C, Pistarini C, Fugazza G, Baldi M. Lesioni cerebrali profonde: aspetti neuroriabilitativi [Deep cerebral lesions: neuro-rehabilitative aspects]. Riv Neurol. 1989;59:15–8.
Saggese JA, Toboada EO, Duhart JE, Adaro FV. Afasias de localización profunda [Aphasia of deep localization]. Neurologia. 1989;4:233–7.
Caplan LR, Schmahmann JD, Kase CS, Feldmann E, Baquis G, Greenberg JP, et al. Caudate infarcts. Arch Neurol. 1990. https://doi.org/10.1001/archneur.1990.00530020029011.
Robin DA, Schienberg S. Subcortical lesions and aphasia. J Speech Hear Disord. 1990. https://doi.org/10.1044/jshd.5501.90.
Weiller C, Ringelstein EB, Reiche W, Thron A, Buell U. The large striatocapsular infarct. A clinical and pathophysiological entity. Arch Neurol. 1990. https://doi.org/10.1001/archneur.1990.00530100051013.
De Renzi E, Colombo A, Scarpa M. The aphasic isolate. A clinical-CT scan study of a particularly severe subgroup of global aphasics. Brain. 1991. https://doi.org/10.1093/brain/114.4.1719.
Pedraza L, Donoso FA, Poblete BAM, González VR. Subcortical aphasias. Rev Neurol Arg. 1991;16:107–12.
Sonobe N, Yashima Y, Takahashi Y, Katayose K, Kumashiro H. Three cases of anomic aphasia after lesions in and/or around the basal ganglia. Fukushima J Med Sci. 1991;37:29–40.
Démonet JF, Celsis P, Puel M, Cardebat D, Marc-Vergnes JP, Rascol A. Thlamic and non-thalamic subcortical aphasia: a neurolinguistic and SPECT approach. In: Vallar G, Cappa SP, Wallesch CW, editors. Neuropsychological disorders associated with subcortical lesions. New York: Oxford University Press; 1992. p. 397–411.
Kennedy M, Murdoch BE. Chronic aphasia subsequent to striato-capsular and thalamic lesions in the left hemisphere. Brain Lang. 1993. https://doi.org/10.1006/brln.1993.1019.
Willmes K, Poeck K. To what extent can aphasic syndromes be localized? Brain. 1993. https://doi.org/10.1093/brain/116.6.1527.
Mega MS, Alexander MP. Subcortical aphasia: the core profile of capsulostriatal infarction. Neurology. 1994. https://doi.org/10.1212/wnl.44.10.1824.
Milhaud D, Magnié MN, Roger PM, Bedoucha P. Infarctus du noyau caudé ou infarctus striato-capsulaires antérieurs? [Infarction of the caudate nucleus or anterior striato-capsular infarction?]. Rev Neurol (Paris). 1994;150:286–91.
Pullicino P, Lichter D, Benedict R. Micrographia with cognitive dysfunction: “minimal” sequelae of a putaminal infarct. Mov Disord. 1994. https://doi.org/10.1002/mds.870090323.
Fuh JL, Wang SJ. Caudate hemorrhage: clinical features, neuropsychological assessments and radiological findings. Clin Neurol Neurosurg. 1995. https://doi.org/10.1016/0303-8467(95)00059-s.
Fabbro F, Clarici A, Bava A. Effects of left basal ganglia lesions on language production. Percept Mot Skills. 1996. https://doi.org/10.2466/pms.1996.82.3c.1291.
Giroud M, Lemesle M, Madinier G, Billiar T, Dumas R. Unilateral lenticular infarcts: radiological and clinical syndromes, aetiology, and prognosis. J Neurol Neurosurg Psychiatry. 1997. https://doi.org/10.1136/jnnp.63.5.611.
Halkar RK, Sisterhen C, Ammons J, Galt JR, Alazraki NP. Tc-99m ECD SPECT imaging in aphasia caused by subcortical infarct. Clin Nucl Med. 1997. https://doi.org/10.1097/00003072-199712000-00010.
Takahashi W, Ohnuki Y, Ohta T, Hamano H, Yamamoto M, Shinohara Y. Mechanism of reduction of cortical blood flow in striatocapsular infarction: studies using [123I]iomazenil SPECT. Neuroimage. 1997. https://doi.org/10.1006/nimg.1997.0284.
Friederici AD, von Cramon DY, Kotz SA. Language related brain potentials in patients with cortical and subcortical left hemisphere lesions. Brain. 1999. https://doi.org/10.1093/brain/122.6.1033.
Kumral E, Evyapan D, Balkir K. Acute caudate vascular lesions. Stroke. 1999. https://doi.org/10.1161/01.str.30.1.100.
Warren JD, Smith HB, Denson LA, Waddy HM. Expressive language disorder after infarction of left lentiform nucleus. J Clin Neurosci. 2000. https://doi.org/10.1054/jocn.1999.0238.
Hua MS, Chen ST, Chu YC. Chinese writing function in patients with left versus right putaminal hemorrhage. J Clin Exp Neuropsychol. 2001. https://doi.org/10.1076/jcen.23.3.372.1182.
Riecker A, Wildgruber D, Grodd W, Ackermann H. Reorganization of speech production at the motor cortex and cerebellum following capsular infarction: a follow-up functional magnetic resonance imaging study. Neurocase. 2002. https://doi.org/10.1076/neur.8.5.417.16181.
Kotz SA, Frisch S, von Cramon DY, Friederici AD. Syntactic language processing: ERP lesion data on the role of the basal ganglia. J Int Neuropsychol Soc. 2003. https://doi.org/10.1017/S1355617703970093.
Kuljic-Obradovic DC. Subcortical aphasia: three different language disorder syndromes? Eur J Neurol. 2003. https://doi.org/10.1046/j.1468-1331.2003.00604.x.
Radanovic M, Azambuja M, Mansur LL, Porto CS, Scaff M. Thalamus and language: interface with attention, memory and executive functions. Arq Neuropsiquiatr. 2003. https://doi.org/10.1590/s0004-282x2003000100006.
Russmann H, Vingerhoets F, Ghika J, Maeder P, Bogousslavsky J. Acute infarction limited to the lenticular nucleus: clinical, etiologic, and topographic features. Arch Neurol. 2003. https://doi.org/10.1001/archneur.60.3.351.
Charron M, Pluchon C, Besson MN, Gil R. Troubles de la communication après régression d'une aphasie sous-corticale: disconnexion fronto-sous-corticale? [Communication disorders after decline in sub-cortical aphasia: the role of fronto-sub-cortical disconnection?]. Rev Neurol (Paris). 2004. https://doi.org/10.1016/s0035-3787(04)71016-4.
Radanovic M, Mansur LL, Azambuja MJ, Porto CS, Scaff M. Contribution to the evaluation of language disturbances in subcortical lesions: a pilot study. Arq Neuropsiquiatr. 2004. https://doi.org/10.1590/s0004-282x2004000100009.
Troyer AK, Black SE, Armilio ML, Moscovitch M. Cognitive and motor functioning in a patient with selective infarction of the left basal ganglia: evidence for decreased non-routine response selection and performance. Neuropsychologia. 2004. https://doi.org/10.1016/j.neuropsychologia.2003.12.003.
de Boissezon X, Démonet JF, Puel M, Marie N, Raboyeau G, Albucher JF, Chollet F, Cardebat D. Subcortical aphasia: a longitudinal PET study. Stroke. 2005. https://doi.org/10.1161/01.STR.0000169947.08972.4f.
Krishnan G, Tiwari S, Pai AR, Rao SN. Variability in aphasia following subcortical hemorrhagic lesion. Ann Neurosci. 2012. https://doi.org/10.5214/ans.0972.7531.190404.
Peñaloza C, Rodríguez-Fornells A, Rubio F, De Miquel MA, Juncadella M. Language recovery and evidence of residual deficits after nonthalamic subcortical stroke: a 1 year follow-up study. J Neurolinguistics. 2014. https://doi.org/10.1016/j.jneuroling.2014.08.001.
Kang EK, Sohn HM, Han MK, Paik NJ. Subcortical aphasia after stroke. Ann Rehabil Med. 2017. https://doi.org/10.5535/arm.2017.41.5.725.
Naeser MA, Alexander MP, Helm-Estabrooks N, Levine HL, Laughlin SA, Geschwind N. Aphasia with predominantly subcortical lesion site. Arch Neurol. 1982. https://doi.org/10.1001/archneur.1982.00510130004002.
Naeser MA, Palumbo CL, Helm-Estabrooks N, Stiassny-Eder D, Albert ML. Severe nonfluency in aphasia. Role of the medial subcallosal fasciculus and other white matter pathways in recovery of spontaneous speech. Brain. 1989. https://doi.org/10.1093/brain/112.1.1.
Crosson B. Subcortical functions in language: a working model. Brain Lang. 1985. https://doi.org/10.1016/0093-934x(85)90085-9.
Crosson B, Benefield H, Sadek J, Moore A, Wierenga C, et al. Left and right basal ganglia and frontal activity during language generation. Contributions to lexical, semantic, and phonological processes. J Int Neuropsychol Soc. 2003. https://doi.org/10.1017/SI35561770397010X.
Wallesch C-W, Papagno C. Subcortical aphasia. In: Rose FC, Whurr R, Wyke MA, editors. Aphasia. London: Whurr Publishers; 1988. p. 256–87.
Ketteler D, Kastrau F, Vohn R, Huber W, et al. Neuroimage. 2008. https://doi.org/10.1016/j.neuroimage.2007.10.023.
Copland DA, Chenery HJ, Murdoch BE. Understanding ambiguous words in biased sentences: evidence of transient contextual effects in individuals with nonthalamic subcortical lesions and Parkinson’s disease. Cortex. 2000. https://doi.org/10.1016/s0010-9452(08)70541-0.
Copland DA, Chenery HJ, Murdoch BE. Discourse priming of homophones in individuals with dominant nonthalamic subcortical lesions, cortical lesions and Parkinson’s disease. J Clin Exp Neuropsychol. 2001. https://doi.org/10.1076/jcen.23.4.538.1233.
Copland D. The basal ganglia and semantic engagement: potential insights from semantic priming in individuals with subcortical vascular lesions, Parkinson’s disease, and cortical lesions. J Int Neuropsychol Soc. 2003. https://doi.org/10.1017/51355617703970081.
Weiller C, Isensee C, Rijntjes M, Huber W, Müller S, Bier D, et al. Recovery from Wernicke’s aphasia: a positron emission tomographic study. Ann Neurol. 1995. https://doi.org/10.1002/ana.410370605.
Cohen H. Language impairment in Parkinson’s Disease. In: Stemmer B, Whitaker HA, editors. Handbook of Neurolinguistics. New York: Academic Press; 1998. p. 475–83.
Skeel RJ, Crosson B, Nadeau SE, Algina J, Bauer RM, Fennell EB. Basal ganglia dysfunction, working memory, and sentence comprehension in patients with Parkinson’s disease. Neuropsychologia. 2001. https://doi.org/10.1016/s0028-3932(01)00026-4.
Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003. https://doi.org/10.1016/s0197-4580(02)00065-9.
Nadeau SE. Subcortical language mechanisms. In: Stemmer B, Whitaker HA, editors. Handbook of the Neuroscience of Language. San Diego: Academic Press; 2008. p. 329–40.
Duffy JR. Motor speech disorders: substrates, differential diagnosis, and management. 2nd ed. St Louis: Mosby; 2005.
Prosody KD. In: Cognitive Neuroscience of Language. New York: Psychology Press; 2015.
Teichmann M, Dupoux E, Cesaro P, Bachoud-Lévi AC. The role of the striatum in sentence processing: evidence from a priming study in early stages of Huntington’s disease. Neuropsychologia. 2008. https://doi.org/10.1016/j.neuropsychologia.2007.07.022.
Teichman M, Rosso C, Martini J-B, Bloch I, Brugières P, Duffau H, et al. A cortical-subcortical syntax pathway linking Broca’s area and the striatum. Hum Brain Mapp. 2015. https://doi.org/10.1002/hbm.22769.
• Shi ER, Zhang Q. A domain-general perspective on the role of the basal ganglia in language and music: benefits of music therapy for the treatment of aphasia. Brain Lang. 2020. https://doi.org/10.1016/j.bandl.2020.104811The authors trace an interesting parallel between the domain-general function of basal ganglia in language and music using rhythm processing as the basis for their discussion.
• Xu L, Huang L, Cui W, Yu Q. Reorganized functional connectivity of language centers as a possible compensatory mechanism for basal ganglia aphasia. Brain Inj. 2020. https://doi.org/10.1080/02699052.2020.1716995This study focus in functional connectivity to support the notion that lesions of cortico-subcortical circuits lead to inter- and intrahemispheric modifications that result in different patterns of language recovery.
Llano DA. The thalamus and language. In: Hickock G, Small SL, editors. Neurobiology of Language. London: Academic Press; 2016. p. 95–114. https://doi.org/10.1016/B978-0-12-407794-2.00009-2.
•• Crosson B. The role of cortico-thalamo-cortical circuits in language: recurrent circuits revisited. Neuropsychol Rev. 2019. https://doi.org/10.1007/s11065-019-09421-8The author further develops his well-known model regarding cortico-thalamic-cortical circuits role in lexical-semantic integration that is critical for efficient word retrieval.
Fritsch M, Krause T, Klostermann F, Villringer K, Ihrke M. Nolte, CH. “Thalamic aphasia” after stroke is associated with left anterior lesion location. J Neurol. 2020. https://doi.org/10.1007/s00415-019-09560-1.
Temel M, Polat BSA, Kayali N, Karadas O. Cognitive profile of patients with thalamic hemorrhage according to lesion localization. Dement Geriatr Cogn Dis Extra. 2021. https://doi.org/10.1159/000516439.
Sandson TA, Daffner KR, Carvalho PA, Mesulam MM. Frontal lobe dysfunction following infarction of the left-sided medial thalamus. Arch Neurol. 1991. https://doi.org/10.1001/archneur.1991.00530240106031.
Bulleid L, Hughes T, Leach P. A case of transient thalamic dysphasia-considering the role of the thalamus in language. Childs Nerv Syst. 2018. https://doi.org/10.1007/s00381-018-3967-7.
Osawa A, Maeshima S. Aphasia and unilateral spatial neglect due to acute thalamic hemorrhage: clinical correlations and outcomes. Neurol Sci. 2016. https://doi.org/10.1007/s10072-016-2476-2.
Bruzzone MJ, Gill R, Ruland S. Teaching NeuroImages: aphasia after infarction of the left pulvinar nucleus. Neurology. 2016. https://doi.org/10.1212/WNL.0000000000003003.
Giraldez MB, Gill R, Ruland S. Aphasia after infarction of the left posterior pulvinar nucleus of the thalamus-case report and literature review. J Neurol Sci. 2015. https://doi.org/10.1016/j.jns.2015.08.1316.
De Witte L, Brouns R, Kavadias D, Engelborghs S, De Deyn PP, Mariën P. Cognitive, affective and behavioural disturbances following vascular thalamic lesions: a review. Cortex. 2011. https://doi.org/10.1016/j.cortex.2010.09.002.
•• Rangus I, Fritsch M, Endres M, Udke B, Nolte CH. Frequency and phenotype of thalamic aphasia. J Neurol. 2021. https://doi.org/10.1007/s00415-021-10640-4In this paper, the authors examined a cohort of 52 patients with unilateral thalamic lesions using 3-Tesla MRI studies resulting in a highly accurate analysis of the correlation between lesion site and aphasia profile.
Nishio Y, Hashimoto M, Ishii K, Mori E. Neuroanatomy of a neurobehavioral disturbance in the left anterior thalamic infarction. J Neurol Neurosurg Psychiatry. 2011. https://doi.org/10.1136/jnnp.2010.236463.
Levin N, Ben-Hur T, Biran I, Wertman E. Category specific dysnomia after thalamic infarction: a case-control study. Neuropsychologia. 2005. https://doi.org/10.1016/j.neuropsychologia.2004.12.001.
Rai M, Okazaki Y, Inoue N, Araki K, Fukunaga R, Sawada T. Object use impairment associated with left anterior thalamic infarction. Eur Neurol. 2004. https://doi.org/10.1159/000082371.
Carrera E, Michel P, Bogousslavsky J. Anteromedian, central, and posterolateral infarcts of the thalamus: three variant types. Stroke. 2004. https://doi.org/10.1161/01.STR.0000147039.49252.2f.
Ghika-Schmid F, Bogousslavsky J. The acute behavioral syndrome of anterior thalamic infarction: a prospective study of 12 cases. Ann Neurol. 2000;48:220–7.
Raymer AM, Moberg P, Crosson B, Nadeau S, Rothi LJ. Lexical-semantic deficits in two patients with dominant thalamic infarction. Neuropsychologia. 1997. https://doi.org/10.1016/s0028-3932(96)00069-3.
Clarke S, Assal G, Bogousslavsky J, Regli F, Townsend DW, Leenders KL, Blecic S. Pure amnesia after unilateral left polar thalamic infarct: topographic and sequential neuropsychological and metabolic (PET) correlations. J Neurol Neurosurg Psychiatry. 1994. https://doi.org/10.1136/jnnp.57.1.27.
Lucchelli F, De Renzi E. Proper name anomia. Cortex. 1992. https://doi.org/10.1016/s0010-9452(13)80050-0.
Bruyn RPM. Thalamic aphasia A conceptual critique J Neurol. 1989. https://doi.org/10.1007/BF00314212.
Mori E, Yamadori A, Mitani Y. Left thalamic infarction and disturbance of verbal memory: a clinicoanatomical study with a new method of computed tomographic stereotaxic lesion localization. Ann Neurol. 1986. https://doi.org/10.1002/ana.410200604.
Graff-Radford NR, Damasio H, Yamada T, Eslinger PJ, Damasio AR. Nonhaemorrhagic thalamic infarction. Clinical, neuropsychological and electrophysiological findings in four anatomical groups defined by computerized tomography. Brain. 1985. https://doi.org/10.1093/brain/108.2.485.
Gorelick PB, Hier DB, Benevento L, Levitt S, Tan W. Aphasia after left thalamic infarction. Arch Neurol. 1984. https://doi.org/10.1001/archneur.1984.04050230082026.
Archer CR, Ilinsky IA, Goldfader PR, Smith KR Jr. Case report. Aphasia in thalamic stroke: CT stereotactic localization. J Comput Assist Tomogr. 1981. https://doi.org/10.1097/00004728-198106000-00024.
Bohsali AA, Triplett W, Sudhyadhom A, Gullett JM, McGregor K, Fitzgerald DB, et al. Broca’s area–thalamic connectivity. Brain Lang. 2015. https://doi.org/10.1016/j.bandl.2014.12.001.
Liu J, Cui Z, Li L. Local and whole-network topologies reveal that pulvinar and semantic hub interactions correlate with picture vocabulary. Neuroreport. 2020. https://doi.org/10.1097/WNR.0000000000001444.
Hart J Jr, Maguire MJ, Motes M, Mudar RA, Chiang HS, Womack KB, Kraut MA. Semantic memory retrieval circuit: role of pre-SMA, caudate, and thalamus. Brain Lang. 2013. https://doi.org/10.1016/j.bandl.2012.08.002.
Crosson B Subcortical functions in language and memory. New York: Guilford; 1992.
Neau JP, Bogousslavsky J. The syndrome of posterior choroidal artery territory infarction. Ann Neurol. 1996. https://doi.org/10.1002/ana.410390614.
Fang Q, Chou XL, Peng B, Zhong W, Zhang LI, Tao HW. A differential circuit via retino-colliculo-pulvinar pathway enhances feature selectivity in visual cortex through surround suppression. Neuron. 2020. https://doi.org/10.1016/j.neuron.2019.10.02.
Lakatos P, O’Connell MN, Barczak A, McGinnis T, Neymotin S, Schroeder CE, et al. The thalamocortical circuit of auditory mismatch negativity. Biol Psychiatry. 2020. https://doi.org/10.1016/j.biopsych.2019.10.029.
Moreaud O, Pellat J, Charnallet A, Carbonnel S, Brennen T. Deficiency in the reproduction and learning proper names after left tubero-thalamic ischemic lesion. Rev Neurol (Paris). 1995;151:93–9.
Szirmai I, Vastagh I, Szombathelyi E, Kamondi A. Strategic infarcts of the thalamus in vascular dementia. J Neurol Sci. 2002. https://doi.org/10.1016/s0022-510x(02)00273-3.
Cox DE, Heilman KM. Dynamic-intentional thalamic aphasia: a failure of lexical-semantic self-activation. Neurocase. 2011. https://doi.org/10.1080/13554794.2010.504731.
Jankowski MM, Ronnqvist KC, Tsanov M, Vann SD, Wright NF, Erichsen JT, et al. The anterior thalamus provides a subcortical circuit supporting memory and spatial navigation. Front Syst Neurosci. 2013. https://doi.org/10.3389/fnsys.2013.00045.
Lam JM, Globas C, Hosp JA, Karnath HO, Wächter T, Luft AR. Impaired implicit learning and feedback processing after stroke. Neuroscience. 2016. https://doi.org/10.1016/j.neuroscience.2015.11.051.
Solomon EA, Lega BC, Sperling MR, Kahana MJ. Hippocampal theta codes for distances in semantic and temporal spaces. Proc Natl Acad Sci U S A. 2019. https://doi.org/10.1073/pnas.1906729116.
Bastiaansen MC, Oostenveld R, Jensen O, Hagoort P. I see what you mean: theta power increases are involved in the retrieval of lexical semantic information. Brain Lang. 2008. https://doi.org/10.1016/j.bandl.2007.10.006.
Mousavi N, Nazari MA, Babapour J, Jahan A. Electroencephalographic characteristics of word finding during phonological and semantic verbal fluency tasks. Neuropsychopharmacol Rep. 2020. https://doi.org/10.1002/npr2.12129.
Leszczyński M, Staudigl T. Memory-guided attention in the anterior thalamus. Neurosci Biobehav Rev. 2016. https://doi.org/10.1016/j.neubiorev.2016.04.015.
Ford AA, Triplett W, Sudhyadhom A, Gullett J, McGregor K, Fitzgerald DB, Mareci T, et al. Broca's area and its striatal and thalamic connections: a diffusion-MRI tractography study. Front Neuroanat. 2013. https://doi.org/10.3389/fnana.2013.00008.
Ojemann GA. Language and the thalamus: object naming and recall during and after thalamic stimulation. Brain Lang. 1975. https://doi.org/10.1016/s0093-934x(75)80057-5.
Ojemann GA. The neurobiology of language and verbal memory: observations from awake neurosurgery. Int J Psychophysiol. 2003. https://doi.org/10.1016/s0167-8760(03)00051-5.
Johnson MD, Ojemann GA. The role of the human thalamus in language and memory: evidence from electrophysiological studies. Brain Cogn. 2000. https://doi.org/10.1006/brcg.1999.1101.
Graff-Radford NR. Syndromes due to acquired thalamic damage. In: Feinberg TE, Farah MJ, editors. Behavioral Neurology and Neuropsychology. New York: McGraw-Hill; 1997. p. 443.
Prabhakar AT, Shaikh AI, Vijayaraghavan A, Rynjah G. Thalamic hypophonia and the neural control of phonation. Neurol India. 2018. https://doi.org/10.4103/0028-3886.246247.
Obayashi S. The supplementary motor area responsible for word retrieval decline after acute thalamic stroke revealed by coupled SPECT and near-infrared spectroscopy. Brain Sci. 2020. https://doi.org/10.3390/brainsci10040247.
Janssen N, Mendieta CCR. The dynamics of speech motor control revealed with time-resolved fMRI. Cereb Cortex. 2020. https://doi.org/10.1093/cercor/bhz084.
Nishio Y, Hashimoto M, Ishii K, Ito D, Mugikura S, Takahashi S, Mori E. Multiple thalamo-cortical disconnections in anterior thalamic infarction: implications for thalamic mechanisms of memory and language. Neuropsychologia. 2014. https://doi.org/10.1016/j.neuropsychologia.2013.11.025.
Chenery HJ, Angwin AJ, Copland DA. The basal ganglia circuits, dopamine, and ambiguous word processing: a neurobiological account of priming studies in Parkinson's disease. J Int Neuropsychol Soc. 2008. https://doi.org/10.1017/S1355617708080491.
León-Cabrera P, Pagonabarraga J, Morís J, Martínez-Horta S, Marín-Lahoz J, Horta-Barba A, et al. Neural signatures of predictive language processing in Parkinson’s disease with and without mild cognitive impairment. Cortex. 2021. https://doi.org/10.1016/j.cortex.2021.03.032.
Alario FX, Chainay H, Lehericy S, Cohen L. The role of the supplementary motor area (SMA) in word production. Brain Res. 2006. https://doi.org/10.1016/j.brainres.2005.11.104.
Swadlow HA, Gusev AG. The impact of ‘bursting’ thalamic impulses at a neocortical synapse. Nat Neurosci. 2001. https://doi.org/10.1038/86054.
Mesulam M-M. Behavioral neuroanatomy. Large-scale networks, association cortex, frontal syndromes, the limbic system, and hemispheric specializations. In: Mesulam M-M, editor. Principles of Behavioral and Cognitive Neurology. 2nd ed. New York: Oxford University Press; 2000. p. 1–120.
Eisinger RS, Urdaneta ME, Foote KD, Okun MS, Gunduz A. Non-motor characterization of the basal ganglia: evidence from human and non-human primate electrophysiology. Front Neurosci. 2018. https://doi.org/10.3389/fnins.2018.00385.
Williams NR, Okun MS. Deep brain stimulation (DBS) at the interface of neurology and psychiatry. J Clin Invest. 2013. https://doi.org/10.1172/JCI68341.
Parsons TD, Rogers SA, Braaten AJ, Woods SP, Tröster AI. Cognitive sequelae of subthalamic nucleus deep brain stimulation in Parkinson’s disease: a meta-analysis. Lancet Neurol. 2006. https://doi.org/10.1016/S1474-4422(06)70475-6.
Okun MS, Fernandez HH, Wu SS, Kirsch-Darrow L, Bowers D, Bova F, et al. Cognition and mood in Parkinson’s disease in subthalamic nucleus versus globus pallidus interna deep brain stimulation: The COMPARE Trial. Ann Neurol. 2009. https://doi.org/10.1002/ana.21596.
Mikos A, Bowers D, Noecker AM, McIntyre CC, Won M, Chaturvedi A, et al. Patient-specific analysis of the relationship between the volume of tissue activated during DBS and verbal fluency. Neuroimage. 2011. https://doi.org/10.1016/j.neuroimage.2010.03.068.
Anzak A, Gaynor L, Beigi M, Limousin P, Hariz M, Zrinzo L, et al. A gamma band specific role of the subthalamic nucleus in switching during verbal fluency tasks in Parkinson’s disease. Exp Neurol. 2011. https://doi.org/10.1016/j.expneurol.2011.07.010.
Wojtecki L, Elben S, Vesper J, Schnitzler A. The rhythm of the executive gate of speech: subthalamic low-frequency oscillations increase during verbal generation. Eur J Neurosci. 2017. https://doi.org/10.1111/ejn.13429.
Hohlefeld FU, Ewald A, Ehlen F, Tiedt HO, Horn A, Kühn AA, et al. Neural correlates of lexical decisions in Parkinson’s disease revealed with multivariate extraction of cortico-subthalamic interactions. Clin Neurophysiol. 2017. https://doi.org/10.1016/j.clinph.2016.12.026.
Ehlen F, Schoenecker T, Kühn AA, Klostermann F. Differential effects of deep brain stimulation on verbal fluency. Brain Lang. 2014. https://doi.org/10.1016/j.bandl.2014.04.002.
Alomar S, King NK, Tam J, Bari AA, Hamani C, Lozano AM. Speech and language adverse effects after thalamotomy and deep brain stimulation in patients with movement disorders: a meta-analysis. Mov Disord. 2017. https://doi.org/10.1002/mds.26924.
Ehlen F, Vonberg I, Tiedt HO, Horn A, Fromm O, Kühn AA, Klostermann F. Thalamic deep brain stimulation decelerates automatic lexical activation. Brain Cogn. 2017. https://doi.org/10.1016/j.bandc.2016.10.001.
Tiedt HO, Ehlen F, Wyrobnik M, Klostermann F. Thalamic but not subthalamic neuromodulation simplifies word use in spontaneous language. Front Hum Neurosci. 2021. https://doi.org/10.3389/fnhum.2021.656188.
Liu S, Guo J, Meng J, Wang Z, Yao Y, Yang J, et al. Abnormal EEG complexity and functional connectivity of brain in patients with acute thalamic ischemic stroke. Comput Math Methods Med. 2016. https://doi.org/10.1155/2016/2582478.
Wang D, Jorge A, Lipski WJ, Kratter IH, Henry LC, Richardson RM. Lateralized effect of thalamic deep brain stimulation location on verbal abstraction. Mov Disord. 2021. https://doi.org/10.1002/mds.28606.
Ojemann G. Language and verbal memory functions during and after human thalamic stimulation. Neurol Neurocir Psiquiatr. 1977;18:35–45.
Mücke D, Hermes A, Roettger TB, Becker J, Niemann H, Dembek TA, et al. The effects of thalamic deep brain stimulation on speech dynamics in patients with essential tremor: an articulographic study. PLoS One. 2018. https://doi.org/10.1371/journal.pone.0191359.
Pedrosa DJ, Auth M, Pauls KA, Runge M, Maarouf M, Fink GR, Timmermann L. Verbal fluency in essential tremor patients: the effects of deep brain stimulation. Brain Stimul. 2014. https://doi.org/10.1016/j.brs.2014.02.012.
Farokhniaee A, McIntyre CC. Theoretical principles of deep brain stimulation induced synaptic suppression. Brain Stimul. 2019. https://doi.org/10.1016/j.brs.2019.07.005.
Bhatnagar SC, Mandybur GT. Effects of intralaminar thalamic stimulation on language functions. Brain Lang. 2005. https://doi.org/10.1016/j.bandl.2004.05.002.
Hebb AO, Ojemann GA. The thalamus and language revisited. Brain Lang. 2013. https://doi.org/10.1016/j.bandl.2012.06.010.
• Silveri MC. Contribution of the cerebellum and the basal ganglia to language production: speech, word fluency, and sentence construction—evidence from pathology. Cerebellum, 10.1007/s12311-020-01207-6. 2021; An interesting review that integrates the basal ganglia and cerebellar circuits in particular aspects of language production, from motor (speech) to cognitive (sentence construction) abilities.
Petersen SE, Fox PT, Posner MI, Mintun M, Raichle ME. Positron emission tomographic studies of the cortical anatomy of single-word processing. Nature. 1988. https://doi.org/10.1038/331585a0.
Author information
Authors and Affiliations
Contributions
Almeida VN: manuscript preparation and revision; Radanovic M: conceptualization, manuscript preparation, and revision
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Radanovic, M., Almeida, V.N. Subcortical Aphasia. Curr Neurol Neurosci Rep 21, 73 (2021). https://doi.org/10.1007/s11910-021-01156-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-021-01156-5