Abstract
Prognosis for patients with glioblastoma continues to be limited, despite an aggressive, multimodal treatment including alkylating chemotherapy. Temozolomide, the most widely used alkylating agent in glioblastoma, is cytotoxic to cells by inducing DNA damage but can be rapidly repaired by the protein O 6-methylguanine DNA methyltransferase (MGMT). In a subset of glioblastomas, the MGMT promoter is methylated, impairing the repair mechanism and conferring chemosensitivity. However, MGMT is overexpressed in 60 % of glioblastomas providing an inherent resistance to alkylating agents and challenging the role of temozolomide in this population. This article reviews the data establishing MGMT promoter methylation as a prognostic factor in glioblastoma and its potential role as a predictor of temozolomide response. It focuses on results from recent studies in newly diagnosed glioblastoma, and the role of temozolomide in MGMT-unmethylated patients. We then turn the discussion to alternatives to temozolomide for newly diagnosed patients as well as therapeutic options at the time of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
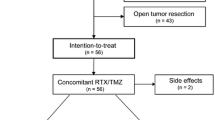
Glioblastoma (GBM) is the most common primary malignant brain tumor in adults with approximately 10,000 cases diagnosed annually in the USA [1] and a generally dismal prognosis despite an aggressive, multimodal treatment. In 2005, Stupp et al. [2] published a landmark study demonstrating a 2.5-month overall survival benefit with the addition of the alkylating agent temozolomide to surgery and radiation [2]. The results of this large trial established the role of temozolomide, along with maximal safe resection and radiation, for the treatment of newly diagnosed GBM patients <65 years old [2]. Preliminary evidence that inactivation of the protein O 6-methylguanine DNA methyltransferase (MGMT) conferred sensitivity to temozolomide [3, 4] and temozolomide’s efficacy in recurrent glioma [5–7] served as supporting data for this large, randomized, phase 3 trial. Subset analyses confirmed improved survival and sensitivity to temozolomide for tumors deficient in MGMT (defined by MGMT promoter methylation) compared to those with adequate MGMT expression (defined by an unmethylation promoter) [2, 8]. However, significant debate remains with respect to whether incorporation of temozolomide should be based upon MGMT methylation status. In this review, we will focus on MGMT promoter-unmethylated GBM patients who have a worse prognosis and a presumed inherent resistance to temozolomide. We will discuss the current understanding of the importance of MGMT methylation, the results of several trials examining the optimal treatments for unmethylated patients, as well as novel therapies that are under investigation.
MGMT Methylation
Temozolomide and other alkylating agents, including the nitrosoureas carmustine and lomustine, are commonly used cytotoxic chemotherapies for newly diagnosed and recurrent GBM as well as lower-grade gliomas. They induce apoptosis and cell death by methylating guanine at the O 6 position, initiating a double-strand break in the DNA, and cell cycle arrest [9, 10]. The MGMT protein removes the damaging alkyl groups from the O 6 position of guanine and repairs the DNA. The alkylated protein is then degraded, requiring constant replenishment for DNA repair to be effective [10]. High expression of MGMT in cancer cells, including glioma cells, account for the predominant mechanism of resistance to alkylating agents [11–13]. Mutations in genes in the mismatch repair family, including mutL homolog 1 (MLH1) and mutS homolog (MSH) family (MSH2, MSH3, and MSH6) and promoter methylation of MLH, also lead to resistance by impairing the cell’s ability to correct DNA damage [14, 15].
Though early studies measuring MGMT expression by immunohistochemistry (IHC) appeared to predict response to alkylating agents, there were substantial interobserver variability and inconsistent correlations with clinical outcome [16]. There was also an unclear relationship between MGMT expression by IHC and its functional inactivation by promoter methylation [16]. CpG island hypermethylation results from epigenetic changes frequently seen in malignant cells. Methylation of the MGMT promoter blocks protein transcription, impairing the cell’s DNA repair function and making the malignant cells more susceptible to the cytotoxic effects of alkylating agents [17].
Despite the apparent advantages of MGMT promoter methylation status over IHC, defining methylation status has its own challenges. Numerous methylation-specific PCR assays are referenced in the literature. They vary in their ability to quantitate methylation status and cover different CpG island sites [3, 18]. The extent of CpG island methylation needed for transcriptional silencing and precise correlation of individual sites with outcomes are poorly defined [16, 19, 20]. MGMT protein expression can also be affected by methylation of the body of the gene, independent of the promoter [20, 21]. The cutoff between MGMT methylation and unmethylation, as defined by methylation-specific PCR, is complicated by methylation pattern, heterogeneity, and tissue contamination with non-neoplastic-methylated cells [22••]. This makes the classifying partially or borderline-methylated results difficult, with wide variability among laboratories. This lack of standardization complicates the interpretation of the literature on the prognostic and predictive impact of MGMT methylation status.
Unmethylated MGMT and Temozolomide in Newly Diagnosed GBM
Because MGMT methylation status has historically rarely been an entry, or stratification, criterion in newly diagnosed or recurrent glioma trials, the results are susceptible to the biases inherent to interpreting secondary endpoints with incomplete and underpowered data [23]. However, the consistency of results demonstrating improved outcomes for methylated patients, regardless of treatment, and an added benefit with temozolomide, suggest that MGMT methylation is both prognostic and predictive (Table 1).
Several phase 2 studies in newly diagnosed elderly patients suggested improved prognoses in methylated patients, regardless of treatment. ANOCEF was a single arm, phase 2 study looking at temozolomide monotherapy in newly diagnosed elderly patients >70 years of age demonstrating significantly longer progression-free survival (PFS) and overall survival (OS) for methylated patients [24]. A phase 2 study investigating the combination therapy with temozolomide and radiation in elderly patients demonstrated significantly longer median PFS (mPFS) and median OS (mOS) for methylated versus unmethylated patients [25]. The German Glioma Network, a prospective observational study of 233 elderly GBM patients >70 years of age, suggested MGMT as a predictive marker for chemotherapeutic response. The mPFS for methylated and unmethylated patients was longest in those treated with chemoradiation at ∼7 months. While the mOS significantly improved by 5.3 months by adding chemotherapy to radiation in methylated patients, the improvement of 1.6 months in the unmethylated patients was not significant [26•]. These findings suggest, at least in the elderly population, that adding chemotherapy to radiation is not beneficial for unmethylated patients.
The NOA-08 trial was a large, phase 3 study designed to test temozolomide monotherapy as a non-inferior treatment to standard radiation (60 Gy) in patients with newly diagnosed high-grade gliomas >65 years of age. MGMT promoter methylation was tested in 51 % of samples using two distinct methylation-specific PCRs, and 35 % were methylated. The authors reported that MGMT promoter methylation status was a predictive marker of response to temozolomide in the elderly and proposed temozolomide monotherapy in elderly patients who are MGMT methylation versus radiation therapy alone in those unmethylated [27•]. The Nordic trial sought to further test the temozolomide’s efficacy as a monotherapy to standard radiation (60 Gy) and hypofractionated radiation (34 Gy in 3–4 Gy over 2 weeks) in newly diagnosed GBM patients >60 years of age. MGMT methylation status was assessed in 59 % of patients, and 45 % of tumors were methylated [28•]. Results supported prior evidence demonstrating efficacy of hypofractionated radiation (40 Gy) in elderly patients [29]. Conclusions were similar to those from the NOA-08 study, with inferior mOS in MGMT-unmethylated patients, regardless of treatment, and no added survival benefit with chemotherapy [28•].
Findings from these studies have led many European neuro-oncologists to routinely test MGMT methylation in all newly diagnosed patients >65 years of age. Patients not felt to be candidates for standard treatment chemoradiation (based primarily on performance status) are treated with radiation or temozolomide monotherapy, depending on their MGMT methylation status [30••]. An ongoing NCIC-led phase 3 study (NCT00482677) will address whether adding temozolomide to hypofractionated radiation in newly diagnosed elderly GBM is beneficial. Patients are stratified by MGMT promoter methylation, age, and extent of resection. Several quality-of-life assessments will also be reported (clinicaltrials.gov). For patients <65 years of age, there is insufficient evidence for withholding temozolomide in unmethylated patients. In the USA, there is generally more reluctance to omit temozolomide for treatment of newly diagnosed unmethylated patients, likely related to the challenges surrounding MGMT promoter methylation testing and the hesitancy to withhold any treatment in a disease with such limited options.
Beyond Temozolomide in Unmethylated MGMT Newly Diagnosed GBM
Given the especially poor prognosis of unmethylated patients, several trials have looked at novel targets as alternatives or additions to temozolomide in this population. The CENTRIC and CORE trials are the largest studies to date to stratify by MGMT methylation status in newly diagnosed GBM [31, 32]. Cilengitide is an αvβ3/5 integrin inhibitor. Phase 1/2a results in newly diagnosed noted improved PFS of 13.4 in methylated versus 3.4 months in unmethylated patients and improved mOS of 23.2 months in methylated compared to 13.1 months in unmethylated [33]. CENTRIC was the randomized phase 3 study of cilengitide with standard chemoradiation versus standard treatment alone in newly diagnosed MGMT-methylated patients. The mOS in both arms was 26.3 months, and mPFS was not significantly different between the treatment and control, again confirming the MGMT methylation’s prognostic effect [32]. The comparative trial for MGMT-unmethylated patients was the CORE study, a randomized, phase 2, open-labeled study with two doses of cilengitide on 1:1:1 randomization with the hypothesis that intensifying cilengitide may be more efficacious in patients with a worse prognosis. Patients were randomized to standard cilengitide or dose-intensified cilengitide to standard chemoradiation, versus standard chemoradiation. Preliminary results demonstrated that, though mPFS was not significantly different between the groups, there was a significantly longer mOS in the standard dose of cilengitide at 16.3 months as compared to 13.4 months in the control arm and 14.5 months in the dose-intensified arm [31]. These findings are encouraging, and we are awaiting the results of the final analysis.
Multiple European-led trials [34–36] have used radiation alone, over chemoradiation, as the comparative arm in trials of novel targets to replace temozolomide. The GLARIUS trial, a randomized phase 2 study of irinotecan/bevacizumab/radiation versus chemoradiation with temozolomide in newly diagnosed unmethylated GBM, found a significantly prolonged mPFS of 9.7 months in the experimental arm versus 5.9 months in the standard arm [34]. The mOS of 16.6 months in the experimental arm suggests that it is reasonable to omit temozolomide in newly diagnosed unmethylated patients and encourages further investigation with this combination [22••, 34]. The S039 trial tested enzastaurin, an inhibitor of phosphoinositide-3 kinase/Akt and protein kinase C, in a single arm phase 2 trial in newly diagnosed, unmethylated GBM. The mPFS was 6.6 months and mOS 15 months. However, the study failed to reach its primary endpoint of PFS at 6 months of 55 % [36]. EORTC 2608 was a randomized, controlled, phase 2 study of temsirolimus, a mTOR inhibitor, in a newly diagnosed unmethylated GBM failed to find a difference in OS >12 months between the experimental arm and standard of care [35].
MGMT in Recurrent GBM
In the recurrent setting, MGMT methylation status has yet to guide treatment. Preliminary data suggested that prolonged exposure to temozolomide may suppress MGMT activity, therefore making the cells more susceptible [37•]. This hypothesis led to a series of studies of dose-dense schedules to prevent repletion of MGMT and improve sensitivity to temozolomide and shift the outcome of unmethylated patients toward those who are methylated. The RESCUE study was a phase 2 trial investigating metronomic temozolomide at the first progression after standard chemoradiation. Though mOS was significantly shorter in unmethylated patients, mPFS from initiation of metronomic temozolomide was similar despite methylation status [38]. Several phase 2 studies of dose-intensified temozolomide at recurrence—one on alternating weeks [39] and another on a 21 days on and 7 days off schedule [40]—failed to demonstrate a difference in PFS between methylated and unmethylated patients [39, 40]. Preliminary results of the phase 2 DIRECTOR trial of alternative temozolomide dosing, which closed prematurely from withdraw of support, demonstrated that MGMT promoter-unmethylated patients failed to benefit from temozolomide rechallenge [41]. A large, randomized trial of dose-dense temozolomide (21 days on and 7 days off of 100 mg/m2) in the adjuvant setting (RTOG 0525) in newly diagnosed GBM patients resolved the conflicting data on timing of standard temozolomide and efficacy of alternative dosing. No improvement was seen in PFS or OS with dose-dense temozolomide, regardless of MGMT promoter methylation status [37•]. These findings, in addition to results from dose-dense temozolomide at recurrence, suggest that unmethylated tumors cannot be “sensitized” to temozolomide by intensifying the dose.
However, there may be more encouraging results for response of unmethylated tumors to other alkylating agents. BELOB, a large, randomized, three-arm phase 2 study of lomustine versus bevacizumab (10 mg/kg) versus combination (with reduced lomustine to 90 mg/m2) in the first recurrence of GBM, demonstrated a PFS at 9 months of 63 % for the combination group versus 43 % for lomustine alone and 38 % for bevacizumab alone [42•]. Though mPFS and mOS were significantly longer, regardless of treatment, the encouraging results prompted an ongoing randomized, phase 3 study of lomustine versus lomustine plus bevacizumab (EORTC 26101; NCT01290939) to further clarify the benefit of adding bevacizumab to lomustine (clinicaltrials.org). Though it is difficult to draw conclusions about the different treatments specifically on unmethylated subgroup, there appears to be a cytotoxic effect of alkylating nitrosourea chemotherapies on unmethylated tumors [42•].
Conclusion
In conclusion, inactivation of the MGMT promoter through methylation increases the sensitivity of malignant cells to the DNA-damaging effects of alkylating agents. However, the MGMT promoter is methylated in ∼40 % of GBM, leaving 60 % with a presumed inherent resistance to temozolomide and other alkylating agents. The data complied from numerous subset analyses clearly demonstrates MGMT promoter methylation to be a prognostic factor in GBM. The data also appear to consistently identify MGMT promoter methylation as a predictive biomarker of response to temozolomide. Applying these results clinically is challenging. While unmethylated patients appear to have less of a response to temozolomide, it is difficult to withhold an approved chemotherapy from those with the poorest prognosis. However, based on the data presented above and the recently released European guidelines, it is reasonable to omit temozolomide in elderly patients who are unmethylated or younger patients with a poor functional status. Though the data are unclear regarding the optimal dose of radiation, it is also reasonable to treat elderly patients with hypofractionated (34–40 Gy) versus standard (60 Gy) therapy. At recurrence, there is no evidence for treating unmethylated patients with temozolomide at any dose or schedule. However, other alkylating agents, such as lomustine, particularly in combination with bevacizumab, are reasonable considerations in the appropriate clinical setting and within discussions of quality of life.
References
Papers of particular interest, published recently, have been highlights as: • Of importance •• Of major importance
CBTRUS. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2004–2008. http://www.cbtrusorg. 2012 [updated 2012; cited 14 Aug 2014].
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96.
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, et al. Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med. 2000;343(19):1350–4.
Hegi ME, Diserens AC, Godard S, Dietrich PY, Regli L, Ostermann S, et al. Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res. 2004;10(6):1871–4.
Newlands ES, Stevens MF, Wedge SR, Wheelhouse RT, Brock C. Temozolomide: a review of its discovery, chemical properties, pre-clinical development and clinical trials. Cancer Treat Rev. 1997;23(1):35–61.
Stupp R, Gander M, Leyvraz S, Newlands E. Current and future developments in the use of temozolomide for the treatment of brain tumours. Lancet Oncol. 2001;2(9):552–60.
Yung WK, Albright RE, Olson J, Fredericks R, Fink K, Prados MD, et al. A phase II study of temozolomide vs. procarbazine in patients with glioblastoma multiforme at first relapse. Br J Cancer. 2000;83(5):588–93.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003.
Liu L, Markowitz S, Gerson SL. Mismatch repair mutations override alkyltransferase in conferring resistance to temozolomide but not to 1,3-bis(2-chloroethyl)nitrosourea. Cancer Res. 1996;56(23):5375–9.
Pegg AE. Repair of O(6)-alkylguanine by alkyltransferases. Mutat Res. 2000;462(2–3):83–100.
Hotta T, Saito Y, Fujita H, Mikami T, Kurisu K, Kiya K, et al. O6-Alkylguanine-DNA alkyltransferase activity of human malignant glioma and its clinical implications. J Neurooncol. 1994;21(2):135–40.
Belanich M, Pastor M, Randall T, Guerra D, Kibitel J, Alas L, et al. Retrospective study of the correlation between the DNA repair protein alkyltransferase and survival of brain tumor patients treated with carmustine. Cancer Res. 1996;56(4):783–8.
Jaeckle KA, Eyre HJ, Townsend JJ, Schulman S, Knudson HM, Belanich M, et al. Correlation of tumor O6 methylguanine-DNA methyltransferase levels with survival of malignant astrocytoma patients treated with bis-chloroethylnitrosourea: a Southwest Oncology Group study. J Clin Oncol. 1998;16(10):3310–5.
Fink D, Aebi S, Howell SB. The role of DNA mismatch repair in drug resistance. Clin Cancer Res. 1998;4(1):1–6.
Esteller M. CpG island hypermethylation and tumor suppressor genes: a booming present, a brighter future. Oncogene. 2002;21(35):5427–40.
Weller M, Stupp R, Reifenberger G, Brandes AA, van den Bent MJ, Wick W, et al. MGMT promoter methylation in malignant gliomas: ready for personalized medicine? Nat Rev Neurol. 2010;6(1):39–51.
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG. Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res. 1999;59(4):793–7.
Vlassenbroeck I, Califice S, Diserens AC, Migliavacca E, Straub J, Di Stefano I, et al. Validation of real-time methylation-specific PCR to determine O6-methylguanine-DNA methyltransferase gene promoter methylation in glioma. J Mol Diagn. 2008;10(4):332–7.
Everhard S, Tost J, El Abdalaoui H, Criniere E, Busato F, Marie Y, et al. Identification of regions correlating MGMT promoter methylation and gene expression in glioblastomas. Neuro Oncol. 2009;11(4):348–56.
Sciuscio D, Diserens AC, van Dommelen K, Martinet D, Jones G, Janzer RC, et al. Extent and patterns of MGMT promoter methylation in glioblastoma- and respective glioblastoma-derived spheres. Clin Cancer Res. 2011;17(2):255–66.
Moen EL, Stark AL, Zhang W, Dolan ME, Godley LA. The role of gene body cytosine modifications in MGMT expression and sensitivity to temozolomide. Mol Cancer Ther. 2014;13(5):1334–44.
Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, et al. MGMT testing-the challenges for biomarker-based glioma treatment. Nat Rev Neurol. 2014;10(7):372–85. Wick et al. thoroughly review recent data on the relationship of MGMT methylation status as a biomarker.
Hart MG, Garside R, Rogers G, Stein K, Grant R. Temozolomide for high grade glioma. Cochrane Database Syst Rev. 2013;4, CD007415.
Gallego Perez-Larraya J, Ducray F, Chinot O, Catry-Thomas I, Taillandier L, Guillamo JS, et al. Temozolomide in elderly patients with newly diagnosed glioblastoma and poor performance status: an ANOCEF phase II trial. J Clin Oncol. 2011;29(22):3050–5.
Brandes AA, Franceschi E, Tosoni A, Benevento F, Scopece L, Mazzocchi V, et al. Temozolomide concomitant and adjuvant to radiotherapy in elderly patients with glioblastoma: correlation with MGMT promoter methylation status. Cancer. 2009;115(15):3512–8.
Reifenberger G, Hentschel B, Felsberg J, Schackert G, Simon M, Schnell O, et al. Predictive impact of MGMT promoter methylation in glioblastoma of the elderly. Int J Cancer. 2012;131(6):1342–50. Reifenberger et al. report on a large, prospective, observational trial of elderly GBM patients and demonstrate no added benefit of adding temozolomide to patients with unmethylated MGMT promoter.
Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012;13(7):707–15. Wick et al. conducted a large study of elderly patients with high-grade glioma and found temozolomide monotherapy to be non-inferior to radiation in MGMT-methylated patients.
Malmstrom A, Gronberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012;13(9):916–26. Malmostrom et al. conducted a large, randomized trial of elderly patients with GBM and found no benefit of adding temozolomide to MGMT-unmethylated patients.
Roa W, Brasher PM, Bauman G, Anthes M, Bruera E, Chan A, et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004;22(9):1583–8.
Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, et al. EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol. 2014;15(9):e395–403. Weller et al. outline European guidelines for the treatment of high-grade gliomas, including MGMT-unmethylated GBM.
Nabors L, Fink K, Mikkelsen T, Grujicic D, Tarnawski R, Nam D, et al. A randomized phase II study investigating cilengitide added to standard chemoradiotherapy in patients with newly diagnosed glioblastoma with unmethylated O6-methylguanine-DNA methyltransferase (MGMT) gene promoter: initial report of the CORE study. Eur J Cancer. 2013;49 Suppl 3:S17–8.
Stupp R, Hegi ME, Gorlia T, Erridge S, Grujicic D, Steinbach JP, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma and methylated O6-methylguanine-DNA methyltransferase (MGMT) gene promoter: key results of the multicenter, randomized, open-label, controlled, phase III CENTRIC study. J Clin Oncol. 2013;31 Suppl 3:2009.
Stupp R, Hegi ME, Neyns B, Goldbrunner R, Schlegel U, Clement PM, et al. Phase I/IIa study of cilengitide and temozolomide with concomitant radiotherapy followed by cilengitide and temozolomide maintenance therapy in patients with newly diagnosed glioblastoma. J Clin Oncol. 2010;28(16):2712–8.
Herrlinger U, Schaefer N, Steinbach JP, Weyerbrock A, Hau P, Goldbrunner R, et al. Survival and quality of life in the randomized, multicenter GLARIUS trial investigating bevacizumab/irinotecan versus standard temozolomide in newly diagnosed, MGMT-non-methylated glioblastoma patients. J Clin Oncol. 2014;32 Suppl 5:2042.
Wick W, Gorlia T, van den Bent MJ, Vecht CJ, Steuve J, Brandes AA, et al. Radiation therapy and concurrent plus adjuvant temsirolimus (CCI-779) versus chemo-irradiation with temozolomide in newly diagnosed glioblastoma without methylation of the MGMT gene promoter. J Clin Oncol. 2014;32 Suppl 5:2003.
Wick W, Steinbach JP, Platten M, Hartmann C, Wenz F, von Deimling A, et al. Enzastaurin before and concomitant with radiation therapy, followed by enzastaurin maintenance therapy, in patients with newly diagnosed glioblastoma without MGMT promoter hypermethylation. Neuro Oncol. 2013;15(10):1405–12.
Gilbert MR, Wang M, Aldape KD, Stupp R, Hegi ME, Jaeckle KA, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol. 2013;31(32):4085–91. Gilbert et al. found no benefit to treatment with dose-dense temozolomide compared to conventional dosing for newly diagnosed GBM, regardless of MGMT promoter methylation status.
Perry JR, Belanger K, Mason WP, Fulton D, Kavan P, Easaw J, et al. Phase II trial of continuous dose-intense temozolomide in recurrent malignant glioma: RESCUE study. J Clin Oncol. 2010;28(12):2051–7.
Wick A, Felsberg J, Steinbach JP, Herrlinger U, Platten M, Blaschke B, et al. Efficacy and tolerability of temozolomide in an alternating weekly regimen in patients with recurrent glioma. J Clin Oncol. 2007;25(22):3357–61.
Norden AD, Lesser GJ, Drappatz J, Ligon KL, Hammond SN, Lee EQ, et al. Phase 2 study of dose-intense temozolomide in recurrent glioblastoma. Neuro Oncol. 2013;15(7):930–5.
Tabatabai G, Wick W, Steinbach JP, Wick A, Schnell O, Hau P et al. MGMT promoter methylation as a prognostic biomarker for benefit from dose-intensified temozolomide rechallenge in progressive glioblastoma: first results from the randomized phase II DIRECTOR trial. J Clin Oncol. 2014;32(5s):(supple; abstr 2015).
Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, et al. Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol. 2014;15(9):943–53. Taal et al. reported an improved PFS9 in recurrent GBM treated with lomustine/bevacizumab compared to bevacizumab alone, regarding of MGMT promoter methylation status.
Compliance with Ethics Guidelines
Conflict of Interest
Jennie W. Taylor declare no conflict of interest.
David Schiff has received paid travel and accommodations from Merck to speak in a symposium about glioma.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuro-Oncology
Rights and permissions
About this article
Cite this article
Taylor, J.W., Schiff, D. Treatment Considerations for MGMT-Unmethylated Glioblastoma. Curr Neurol Neurosci Rep 15, 507 (2015). https://doi.org/10.1007/s11910-014-0507-z
Published:
DOI: https://doi.org/10.1007/s11910-014-0507-z