Abstract
Imported cutaneous leishmaniasis (CL) is a growing problem with increasing global travel to endemic areas. Returned travellers seeking care encounter significant barriers to treatment, including diagnostic delays and difficult access to anti-leishmanial drugs. Treatment recommendations in non-endemic settings are a moving target, reflecting recent developments in Leishmania diagnostics and therapeutics. Accumulating experience with molecular-based species identification has enabled species-directed therapy. Clinicians are reevaluating more toxic traditional regimens in light of newly approved therapeutic agents and emerging data on local cutaneous treatments. Referral centers are implementing treatment decision algorithms designed to maximize efficacy while minimizing adverse events. Although management strategies continue to evolve, treatment of CL in non-endemic settings remains controversial. Persistent reliance on expert opinion reflects lack of research focused on travellers and limited randomized controlled trial evidence. We herein review the current epidemiology of cutaneous leishmaniasis in travellers and species-specific evidence for available therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leishmaniasis is a protozoan parasitic infection endemic in 98 countries, with over 350 million people at risk globally and 0.7–1.3 million new cases per year [1]. Sandflies transmit the infection to humans by inoculating Leishmania promastigotes into exposed skin, resulting in cutaneous, mucocutaneous, or visceral disease syndromes. Clinical manifestations depend on causative Leishmania species and underlying host immunity. Although formerly limited to rural tropical and subtropical populations, cutaneous leishmaniasis is an increasing problem in travellers with the rise in adventure travel and ecotourism in the past decade [2••].
Guidelines for treatment of cutaneous leishmaniasis (CL) in returned travellers are evolving [3••, 4••]. Increasing availability of molecular diagnostics, including PCR-based assays, has enabled a shift towards species-directed treatment. Recent FDA approval of anti-leishmanial drugs such as miltefosine has expanded the range of therapeutic options [5]. With new data supporting local cutaneous treatments, clinicians are reevaluating the risks and benefits of systemic therapy. Referral centers are exploring novel algorithmic approaches to maximize cure rates while minimizing medication-related adverse events [6••].
Despite recent advances, optimal treatment of CL in travellers remains controversial. Clinicians lack evidence to inform decision-making, relying on small studies, personal experience, and expert opinion. Few studies focus on travellers. Extrapolation of data derived from Leishmania-endemic settings may inadequately reflect the natural history or treatment response in travellers, an immunologically naïve population with very different exposure rates and genetics. We herein review the epidemiology of CL in travellers and discuss major treatment options, integrating a species-specific approach.
Vector/Pathogen
Leishmania spp. are a diverse group of intracellular trypanosomid protozoans, with over 20 species causing human infection [7]. Although individual species have unique transmission patterns, local reservoirs, and predominant clinical features, Leishmania are broadly subdivided into Old World and New World species. Old World cutaneous leishmaniasis (OWCL) acquired in Africa, Asia, the Middle East, and Mediterranean/southern Europe is transmitted by sandflies of the genus Phlebotomus. Major causative species include Leishmania major, Leishmania tropica, Leishmania infantum, Leishmania donovani, and Leishmania aethiopica. In general, Old World species cause more indolent cutaneous disease without spread to mucosal sites. L. infantum and L. donovani also cause visceral leishmaniasis, but rarely concurrent with cutaneous disease.
New World cutaneous leishmaniasis (NWCL) is endemic throughout Latin America, ranging from Mexico to Argentina. Transmitted by sandflies of the Lutzomyia genus, two distinct New World subgenera have differing propensities towards complicated disease. Members of the Viannia subgenus including Leishmania Viannia braziliensis, L. (V.) guyanensis, L. (V.) panamensis, and L. (V.) peruviana may be locally aggressive and can progress to destructive mucocutaneous infection (mucocutaneous leishmaniasis (MCL)). The Leishmania subgenus includes Leishmania (Leishmania mexicana, L. (L.) amazonensis, and L. (L.) venezuelensis, and almost never involves the naso- or oropharyngeal mucosa.
Epidemiology in Travellers
Imported CL is a growing problem due to increasing global tourism, adventure travel to remote destinations, and expanding military operations in endemic countries [8, 9•]. CL was the third most common dermatologic diagnosis and the most frequent cause of cutaneous ulcer in a large series of patients presenting to GeoSentinel surveillance network clinics worldwide [2••]. The majority of returned travellers with CL were young and male and acquired infection in Costa Rica, Bolivia, and Afghanistan [2••]. Most North American civilian travellers acquire CL in Latin America, whereas Old World species predominate in European centers [2••, 6••, 8]. Infections occur in both short- and long-term travellers [10].
Exotic travel is not a prerequisite for infection, as travellers can acquire CL in common southern European tourist destinations. Most infections in a series of European travellers occurred during 1–3-week summer vacations in Spain, Italy, Malta, and Greece [10]. Destinations included the Balearic Islands, Sicily, and the Peloponnese, and L. donovani was the predominate species. Military activity in Iraq and Afghanistan has also led to an explosion of OWCL in coalition forces deployed to these areas. More than 1300 US army personnel in Iraq have acquired L. major infection since 2003, with additional cases of L. tropica from Afghanistan [11, 12].
Clinical Manifestations
CL in travellers classically presents as a painless cutaneous ulcer with a granulomatous base and raised violaceous borders, occurring at the sandfly bite site. Lesions typically begin as a small macule that evolves into an inflammatory papule, followed by a nodule that ulcerates over weeks to months [13]. Lesions may be single or multiple, and lymphocutaneous spread frequently occurs in travellers with L. (V.) braziliensis infection [7, 11, 14]. Depending on causative species and host immunity, CL can take on many different appearances including nodular, verrucous, psoriaform, zosteriform, and chancre-like lesions. Ulcers become painful with secondary bacterial or fungal infection.
The incubation period for cutaneous leishmaniasis is species and host dependent. US military personnel with CL due to L. major presented an average of 9 s± 5 weeks after initial infection, although this represents an almost exclusively young, healthy, male population [15]. Time to presentation in other studies varied from week to months and rarely years, such that clinicians and patients may not associate the lesion with travel [13, 16•].
Risk of Mucocutaneous Leishmaniasis
Progression to mucocutaneous disease is the major feared complication of New World L. Vianna complex infections. Dissemination to nasal, oral, and hypopharyngeal mucosa manifests as destructive ulcerative or granulomatous lesions. Untreated MCL leads to serious sequelae including nasal septum and alae perforation and destruction, disfigurement, and rarely death related to airway compromise [13] MCL is rarely concurrent with the initial cutaneous infection, usually presenting 1–5 years after resolution, and occasionally as long as 35–50 years later [7, 17••, 18]. Intercurrent cutaneous and mucosal involvement may be more likely in travellers compared to MCL occurring in endemic populations. Early symptoms include nasal stuffiness and mild bleeding, with associated mucosal erythema and edema progressing to ulceration. Hoarseness or dysphonia signal laryngeal involvement.
Risk of mucosal dissemination varies significantly with species and region of acquisition. Ninety percent of mucosal disease occurs in Bolivia, Peru, and Brazil, in particular with L. (V.) braziliensis and L. (V.) peruviana infection in high Andean regions [1, 17••]. Between 2 and 10 % of L. (V.) braziliensis infections in Brazil progressed to MCL, while rates approached 13 % in Peru, 12–14.5 % in Bolivia, and 6.9–7.7 % in Ecuador [16•, 17••, 69, 70]. By contrast, in Central America, mucosal involvement occurs in less than 1 % of L. (V.) braziliensis infections [14, 17••]. Risk factors for MCL identified in a major systematic review include multiple lesions, ulcer size >4 cm2, head and neck localization, incomplete treatment course, and acquisition in high Andean countries, in particular Bolivia [17••].
MCL is rare in travellers and has not been systematically evaluated. In a pooled analysis of specialized travel clinics, 3 % (range 0–25 %) of patients had mucocutaneous involvement. However, selection bias strongly influenced these estimates, and data included immigrants as well as travellers [17••]. In the absence of high-risk factors (Table 2), immunocompetent travellers are thought unlikely to develop MCL [3••].
Diagnosis
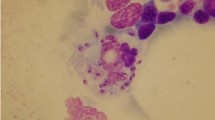
A confirmed parasitologic diagnosis is essential in travellers. Parasite DNA amplification using PCR is now the preferred diagnostic approach, as PCR is highly sensitive and can provide species-level identification, particularly if paired with restriction fragment length polymorphism (RFLP) analysis or gene sequencing. PCR availability remains limited to major reference centers for tropical diseases [73–76]. Leishmania amastigotes may be identified on direct microscopy of thin smears or on histopathology of skin biopsies, though sensitivity of direct examination is limited. Amastigotes are best visualized under oil immersion using H&E or Giemsa staining, with tissue sections cut at 3–4 μm [11]. Leishmania spp. can also be cultured on specialized media such as Nicolle-McNeal-Novy (NNN) or Tobie’s medium, but this process is slow, laborious, and technically challenging. Sensitivity of non-PCR-based techniques varies with lesion morphology and specimen quality and paradoxically decreases with longer duration of infection.
Traditional techniques for tissue specimen collection include lesion scraping, fine-needle aspiration, and biopsy. Punch-biopsies are most useful for non-ulcerative CL and when alternative diagnoses are likely. Recent advances in specimen collection include filter-paper-based techniques and cytology-brush scrapings [77, 78]. Both are painless, can be obtained in the setting of bacterial or fungal secondary infection, and are particularly helpful in children.
Treatment
Recommended first-line and alternative treatments in expert guidelines differ, reflecting experience at individual centers and limited data in travellers [3••, 4••, 6••, 13]. Even in endemic populations, there are comparatively few well-designed, adequately powered randomized controlled trials for CL. Treatment guidelines have shifted towards a species-based approach, made possible by molecular diagnostics [4••]. Although species-directed therapy can inform decision-making, treatment depends on multiple factors including risk of mucocutaneous spread, extent and location of lesions, host immune status, treatment toxicity, patient preference, and reliability of follow-up. Patients responding to treatment show clinical improvement within 4–6 weeks, achieve complete re-epithelialization of the ulcer base within 3 to 6 months, and ultimately develop an atrophic scar [9•]. A single treatment course is not always curative, particularly with extensive cutaneous involvement and immunocompromise [6••, 79]. Follow-up should continue for at least 1 year after treatment completion to monitor for relapse [3••]. In patients for whom causative species is known to be L. (V.) braziliensis or in patients who acquired their CL in high Andean regions, follow-up with annual rhinoscopic examination should continue for a decade after treatment (Table 1).
Local Cutaneous Treatments
Local therapies have significant advantages in returned travellers: they are convenient, inexpensive, and avoid systemic treatment toxicity. Potential options include wound care alone, intralesional antimonials (ILSb), cryotherapy, paromomycin creams, and thermotherapy. Local treatments are typically reserved for mild disease in immunocompetent patients. Most studies exclude patients with lesions >3–4 cm in diameter, more than three to five lesions, associated lymphadenopathy, and immunocompromise. Topical therapies are well established for OWCL and NWCL due to L. mexicana and may also be considered for L. Viannia species when risk of MCL is low (Table 2). Local therapy is unsuitable for sensitive areas including the genitalia, eye lids, and lips and is also discouraged for facial lesions.
-
1.
Wound care, watchful waiting
The natural history for most CL is spontaneous resolution. Local wound care to promote healing and prevent secondary bacterial infection is effective for species that re-epithelialize over weeks to months. Single-lesion L. major resolved by 45 days in 20–45 % of patients, with 40–90 % cure by 3 months, and close to 100 % by 1 year [80, 81]. L. tropica is often more persistent, with 1 to 10 % resolving within 3 months, two thirds being cured by 1 year, and the remainder healing over 1 to 3 years [80, 82]. Among New World species, L. mexicana has high rates of spontaneous cure approaching 88 % at 3 months, but only 68 % at 6 months due to relapse [83]. Other NWCL species have more prolonged time to resolution. Six-month cure rates in endemic populations with L. (V.) braziliensis were only 2–17 % [24•, 83].
Observation and wound care is effective in pre-selected travellers. Cleaning and wound dressing resulted in complete lesion re-epithelialization at 42–60 days in 92 % (n = 23/25) of French returned travellers with low-risk limited disease, defined by the following criteria: four or fewer lesions; lesion size <4 cm; non-sensitive location; infection caused by L. major, L. mexicana, or other species showing signs of self-cure; and immunocompetent, non-diabetic host [6••]. Although this strategy avoids toxicity, watchful waiting is not universally acceptable to travellers, who often request active treatment [9•].
-
2.
Intralesional antimonials plus cryotherapy
Combined intralesional antimonials (ILSb) and cryotherapy is the preferred first-line treatment option for OWCL in several European guidelines and can be considered in mild NWCL at low risk for mucosal involvement [3••, 4••]. Both treatments are individually effective for OWCL compared with placebo, but combination therapy resulted in significantly higher cure rates (89–91 %) compared with either cryotherapy (57–68 %) or intralesional antimony (56–75 %) monotherapy [19–21]. Major randomized controlled trials took place in L. tropica- and L. major-endemic areas, with minimal published efficacy data for other Old World species.
Clinicians in Latin America are increasingly using intralesional antimony for NWCL, although long-term risk of subsequent mucosal disease is not yet established. Intralesional antimony was effective for L. (V.) braziliensis in two small studies. In an RCT including 80 Bolivian patients with small single-lesion CL, ILSb cured 70 % of patients at 6 months, compared with 20 % receiving cryotherapy, and 17 % in the placebo group [24•]. An older observational study of 74 Brazilian patients treated with ILSb revealed 6-month complete re-epithelialization in 80 % of patients. Three quarters were followed for at least 5 years, with no evidence of relapse or mucosal involvement [25]. Although there are no species-specific data evaluating intralesional antimony plus cryotherapy for other New World species, many experts consider this an option [4••].
Cryotherapy is readily accessible in dermatology clinics, but drug availability and lack of technical expertise in administration are major barriers to intralesional antimony treatment in North America [9•]. Cryotherapy and ILSb injections caused transient pain, as well as local erythema, edema, and vesicles [24•].
-
3.
Paromomycin-containing ointments
Paromomycin is an aminoglycoside antibiotic active against Leishmania that can be locally applied to cutaneous ulcers. Less than 10 % of topical paromomycin is systemically absorbed, avoiding aminoglycoside-associated vestibular and renal toxicity [26••]. Mild to moderate skin irritation is common. More significant local inflammatory reactions occur when administered in methylbenzethonium chloride (MBCL) vehicle, occasionally requiring treatment interruption.
Topical 15 % paromomycin-12 % MBCL is a recommended first-line treatment for L. major in several guidelines [3••], but is not superior to placebo when delivered in alternate vehicles such as urea [22, 84]. Proposed hypotheses for differing vehicle-related efficacy are synergistic anti-leishmanial activity with MBCL, and improved skin penetration resulting from a heightened inflammatory reaction [84]. In meta-analysis, curative efficacy of topical paromomycin-MBCL for L. major was comparable to intralesional antimonials [84]. Paromomycin was also effective for L. major when co-formulated with 0.5 % gentamicin as the compound WR 279,396 [26••]. Both 15 % paromomycin-0.5 % gentamicin and paromomycin ointment cured 80–94 % of ulcerative L. major in Tunisia, compared with 58–71 % in the placebo group [26••, 27]. Although not systematically evaluated, topical paromomycin may be less effective for nodular lesions typical of L. donovani and L. aethiopica or hyperkeratotic forms of L. tropica [84].
Meta-analysis of small randomized controlled trials for NWCL suggests that topical paromomycin is superior to lacebo, equivalent to intralesional meglumine antimoniate, and inferior to systemic antimonials [84]. Topical 15 % paromomycin-12 % MBCL and 15 % paromomycin-0.5 % gentamicin were both superior to placebo in several small studies of L. (V.) panamensis, L. (V.) braziliensis, and L. mexicana. In L. (V.) panamensis infection, paromomycin combined with either 12 % MBCL or 0.5 % gentamicin achieved 79 to 90 % cure rates [30, 31]. In areas of Guatemala endemic for L. (V.) braziliensis (75 %) and L. mexicana (25 %), 15 % paromomycin-12 % MBCL cured 91.4 % of patients at 13 weeks compared with a 39.4 % in the placebo group [32]. Follow-up duration was insufficient to evaluate progression to MCL, and most studies took place in comparatively low risk areas of Central America [17••, 31].
Topical 15 % paromomycin-12 % MBCL is available in Israel under the trade name “Leshcutan,” but is not FDA-approved and difficult to obtain except through compounding pharmacies. The Walter-Reed formulation (WR 279,396) 15 % paromomycin-5 % gentamicin is not yet commercially available.
-
4.
Thermotherapy
Leishmania amastigotes are temperature sensitive and can be targeted with localized heat generated by high-energy radiofrequency waves [22]. Radiofrequency heat therapy (RFHT) is an easily administered, single-visit treatment with minimal side effects [34]. ThermoMed Model 1.8 (Thermosurgery Technologies, Inc., Phoenix, AZ) is the only FDA-cleared current field radiofrequency generator and is not widely available [11, 12].
RFHT is effective for OWCL lesions less than 3–5 cm, with cure rates similar to both intralesional and systemic antimonials [3••, 12, 22, 34, 35, 85]. Pooled efficacy for L. major based on 1 RCT and 2 observational studies was 82 % (95 % CI 73–89 %) [4••]. In patients with L. tropica, single RFHT treatment cured 94 % at 12 weeks and 98 % at 6 months, with no relapses observed up to 1 year [34]. There was no significant difference compared with patients receiving intralesional antimony [34]. Two randomized studies of L. tropica in Afghanistan also found cure rates similar to intralesional antimony, with 54 % complete re-epithelialization at 100 days [35] and 83 % at 6 months [36] A few studies noted shorter time-to-cure and superior cosmetic result using thermotherapy, but these results have not been consistently reproduced [34, 35, 39].
Thermotherapy is a possible first-line option for L. mexicana, with 90–95 % cure at 8–20 weeks in a prospective observational study of 201 patients [38]. Interestingly, all 23 patients with cartilage involvement of the ear (Chiclero’s ulcer) experienced complete resolution, though this area is normally difficult to treat [38, 86]. For L. Viannia spp. infections, thermotherapy is superior to placebo, but inferior to intralesional and systemic antimonials [16•, 39]. In two related Colombian RCTs, 6-month curative efficacy for L. (V.) panamensis and L. (V.) braziliensis in thermotherapy-treated patients was inferior to IM meglumine antimoniate (58 vs. 72 %) [87], but similar to miltefosine (58 vs. 59 %) [37•]. Thermotherapy performed poorly in Guatemalan patients with confirmed L. (V.) braziliensis, curing only 9 of 14 (64 %) patients compared with 11 of 14 (79 %) treated with meglumine antimoniate and 0 of 11 in the placebo group [39].
-
5.
Adjunctive therapies
Imiquimod is an immunomodulator involved in the TH1 immune response, acting as an agonist for toll-like receptor 7 on macrophages and dendritic cells [88]. Some experts use topical imiquimod as adjunctive treatment for CL to both accelerate healing and reduce residual scarring, particularly in children and with facial lesions. Two small RCTs in L. (V.) braziliensis and L. (V.) peruviana-endemic areas revealed faster time-to-healing and improved cosmetic result using topical imiquimod in combination with systemic pentavalent antimony, compared with antimony monotherapy [88, 89]. More patients receiving imiquimod experienced local erythema, but no other major side effects occurred [88]. In meta-analysis, adjunctive topical imiquimod resulted in improved 3-month cure rates, but did not affect long-term cure at 6 and 12 months (134 participants; ITT; RR: 1.45; 95 % CI: 1.12–1.88; I2 0 %) [16•, 90].
Systemic Therapy
Systemic treatment is indicated for immunosuppressed patients, extensive or large numbers of lesions, mucosal involvement, local treatment failure, and lesions in sensitive locations. Older literature recommends systemic therapy for all L. Viannia complex NWCL, particularly L. (V.) braziliensis. This is no longer an absolute rule. Systemic treatments have significant associated toxicities, pose a risk to patients with co-morbid illness, and are complex to administer, with intensive monitoring requirements. In choosing therapy, clinicians must weigh risk of future MCL, for which actual evidence of risk mitigation by systemic treatment does not exist, against the potential for treatment-related adverse events. Table 2 describes current indications for parenteral treatment based on expert opinion. Although systemic therapy may decrease risk of future complications, MCL can still occur despite full courses of parenteral therapy [17••, 91].
-
1.
Pentavalent antimony (SbV)
Pentavalent antimonials are no longer drugs of choice for NWCL in North American travellers due to toxicity, complexity of administration, and availability of other effective treatments [92, 93]. Sodium stibogluconate is administered at a dose of 20 mg/kg IV daily for 20 days and can only be obtained in North America through a CDC Investigational New Drug application. Due to lack of FDA approval, US health insurance plans may not reimburse costs associated with intravenous treatment, and home antibiotic infusion programs are ill-equipped to handle administration and required monitoring [9•]. Mild to moderate adverse effects occur in most patients, including fatigue, arthralgia, gastrointestinal complaints, transaminitis, elevated lipase with symptoms of pancreatitis, mild thrombocytopenia, and ECG abnormalities [11, 94, 95]. Up to 25–65 % of patients require treatment interruptions [11, 95]. Although most patients resume therapy within days, severe adverse events including more severe cytopenias, symptomatic arrhythmias, major cardiac repolarization abnormalities, acute tubular necrosis, and fulminant hepatitis can occur, primarily in patients over age 55 or with underlying co-morbidities [46]. SbV is contraindicated with any major cardiac, renal, or hepatic disease and should be used with extreme caution in older patients.
Pentavalent antimonials typically cure 70–96 % of NWCL depending on geographic location, strain, and severity [22, 39, 40, 54]. For L. (V.) braziliensis and L. (V.) peruviana, antimonials are highly effective, although foci of possible antimonial resistance are emerging in South America [16•, 96, 97]. Pentavalent antimony is not recommended for CL due to L. (V.) guyanensis due to low cure rates [96]. Although effective for L. (V.) panamensis and L. mexicana, other less toxic treatments have equal or better efficacy [3••, 43, 67].
Parenteral antimonials are not first-line drugs for OWCL, given poorly documented efficacy and other better tolerated treatments [22]. In published RCTs, parenteral antimonials were equivalent or inferior to those administered intralesionally [22]. One small study suggests improved efficacy with adjunctive pentoxifylline (81.3 % n = 26/32 vs. 50 % n = 16/32) [49]. Despite poor evidence, experts endorse systemic antimonials in some national guidelines and continue to use them for complex, treatment refractory OWCL [47, 98].
-
2.
Miltefosine
Miltefosine is an oral alkylphosphocholine analog emerging as an effective alternative to parenteral antimony. In March 2014, miltefosine became the first FDA-approved drug for treatment of cutaneous and mucocutaneous leishmaniasis [5]. The recommended treatment course is 2.5 mg/kg/day for 28 days (maximum dose 150 mg/day). Current approval is limited to L. (V.) braziliensis, L. (V.) panamensis, and L. (V.) guyanensis infection in patients over age 12, and mucocutaneous leishmaniasis due to L. (V.) braziliensis [5].
Pooled results of 4 RCTs demonstrated similar efficacy of miltefosine and systemic antimonials for NWCL, with no significant difference in cure at 6 months (584 participants; RR 1.12; 95 % CI 0.85 to 1.47) [16•, 40, 44, 45, 51••] Species-specific efficacy varies. Cure rates for L. (V.) panamensis range from 60 to 94 % in Colombia [37•, 40, 51••, 52, 53]. In children with L. (V.) panamensis, miltefosine treatment failure rates were only 8.3 %, compared with 36 % in the group receiving meglumine antimoniate [51••]. For L. (V.) guyanensis in Brazil, miltefosine was superior to antimonials, with 6-month cure rates of 71.4 % (n = 40/56) compared with 53.6 % (n = 15/28) (p < 0.05) [44]. For L. (V.) braziliensis, meta-analysis revealed an overall trend towards superiority of miltefosine compared with pentavalent antimony (ITT; RR 1.41; 95 % CI 0.98 to 2.03) [16•]. However, cure rates among RCTs were heterogeneous. Miltefosine cured 88 % of L. (V.) braziliensis in Bolivia [54], 73 % in Brazil [45], 49 % in Colombia [40], and only 33 % in Guatemala [52]. L. mexicana responds poorly to miltefosine in vitro, with only 60 % efficacy in one human trial [52, 99].
Miltefosine is a successful salvage therapy for patients with refractory OWCL, but randomized controlled trial data is lacking. Miltefosine cured 88 % (n = 30/34) of Dutch soldiers with aggressive L. major infection acquired in Afghanistan that did not respond to intralesional antimony [55]. In a small open-label Iranian RCT, miltefosine cured 26 of 32 patients (81.3 %) at 3 months, compared with 25 of 31 (80.6 %) of those treated with IM meglumine antimoniate [48].
Mild adverse effects are common and usually do not require treatment interruption. Gastrointestinal complaints including vomiting (40 %) and diarrhea (20 %) occur mainly in the first week [56]. Teratogenicity is a major consideration for reproductive-aged women. Contraception should be used during therapy and for 4–5 months after treatment completion due to miltefosine’s long half-life [5, 100].
Liposomal amphotericin B (L-AMB)
Expert guidelines rank liposomal amphotericin B as a first-line option based on high cure rates in observational studies and successful treatment of severe refractory disease, including in immuncompromised patients [3••, 6••, 57•]. L-AMB is FDA-approved only for visceral leishmaniasis, but is used off label for cutaneous disease in US and Canadian centers. The most common regimen is a short intravenous course of 3–5 mg/kg daily administered on days 1–5, with a sixth dose on day 10. Transient infusion reactions requiring premedication occur in up to 25 %, and reversible grade 2 nephrotoxicity affects 5–6 % of patients [57•]. Risk of nephrotoxicity is reduced by intravenous pre-hydration.
Published data on L-AMB in travellers is sparse, but observational studies document high cure rates of 80–90 %. In 19 US soldiers infected with multiple New and Old World species, including 2 with mucosal involvement and 3 failing systemic antimonials, L-AMB cured 84 % after initial treatment and all after a second course [58]. L-AMB cured 85 % (n = 30/34) of Israeli travellers with L. (V.) braziliensis, which was similar to a parenteral antimony comparison group (70 %, n = 24/34, p > 0.05) [57•]. Single-course L-AMB cured 11 of 13 (85 %) German travellers with L. (V.) braziliensis [56]. L. tropica fully responded to L-AMB in 84 % of Israeli patients, most with prior topical treatment failure [59]. L-AMB has not been evaluated extensively in endemic settings.
-
3.
Oral azoles (fluconazole, ketoconazole)
Fluconazole is a potential outpatient systemic treatment option, with apparent dose-dependent efficacy. Randomized controlled trial data exists only for L. major. Fluconazole cured 81 % of Iranian patients treated with 400 mg daily for 6 weeks, compared with 48 % in those receiving 200 mg daily [60]. Low-dose 200 mg fluconazole is not consistently effective. One Saudi Arabian RCT noted 3-month cure rates of 79 % compared with 34 % in the placebo group [61]. However, 6 weeks of fluconazole cured only 44 % of French travellers infected with L. major, which is similar to placebo rates in other studies [62].
One prospective observational study evaluated cure rates for cutaneous L. (V.) braziliensis with escalating doses of fluconazole, administered for 4–12 weeks [63]. Fluconazole cured all patients (n = 8) treated with 8 mg/kg/day, compared with 93 % (n = 14) dosed at 6.5 mg/kg/day and 75 % (n = 8) at 5 mg/kg/day [63]. Ketoconazole was ineffective in Guatemalan L. (V.) braziliensis, but cured 89 % of patients with L. mexicana and was superior to both placebo and pentavalent antimony in this subgroup [101]. Some centers have entirely eliminated fluconazole from treatment recommendations due to therapeutic failures [6••].
-
4.
Pentamidine
Rarely used in travellers, pentamidine is a first-line option for L. (V.) panamensis and L. (V.) guyanensis in areas of South America. Cure rates for L. (V.) panamensis are consistently greater than 90 % in older observational studies in endemic populations [41•, 64]. Treatment response for L. (V.) guyanensis appears similar to L. (V.) panamensis and comparable to antimonials [16•, 64, 65]. Emerging drug resistance is a concern, with lower cure rates approaching 60 % observed in more recent studies [43, 66]. Efficacy in L. (V.) braziliensis is poor and inferior to systemic antimony [16•, 67]. Pentamidine cured only 35 % of patients with L. (V.) braziliensis in Peru, compared with 78 % of those treated with parenteral sodium stibogluconate (p < 0.001) [67].
Conclusion
Returned travellers with cutaneous leishmaniasis encounter significant barriers to treatment. First-line anti-leishmanial drugs are difficult to access in non-endemic settings, such that availability often determines treatment selection. Clinicians are faced with limited data to direct management. The existing literature is plagued by heterogeneous methodology with non-uniform clinical endpoints, inconsistent treatment regimens, small sample sizes, high loss to follow-up, and often absence of a control group [3••, 16•, 22]. High-quality randomized controlled trials are urgently needed in both endemic populations and travellers, as fundamental questions remain unanswered. Does species-oriented treatment improve outcome? What is the true risk of mucocutaneous leishmaniasis in travellers, and are risk factors similar to endemic populations? How do local treatments compare with systemic therapy in patients with New World CL? How should we treat high-risk groups including children, immunocompromised hosts, and patients with co-morbid illness? Facilitating rapid access to Leishmania molecular diagnostics and anti-leishmanial drugs, expanding treatment options, including investment in ethnopharmaceutical and novel therapeutic approaches, and rigorously evaluating existing therapies are priorities in the next decade, and will require ongoing international collaboration.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
WHO | Leishmaniasis [Internet]. [cited 2014 Dec 3]. Available from: http://www.who.int/mediacentre/factsheets/fs375/en/
Leder K, Torresi J, Libman M. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158:456–68. Describes most common diagnoses in ill returned travellers presenting to Geosentinel clinics worldwide according to travel destination and syndromic presentation.
Blum J, Buffet P, Visser L, Harms G, Bailey MS, Caumes E, et al. LeishMan recommendations for treatment of cutaneous and mucosal leishmaniasis in travelers, 2014: LeishMan recommendations. J Travel Med. 2014;21:116–29. Species-specific treatment recommendations for CL in travellers based on a systematic literature review by a European expert panel. This review uses the Oxford evidence grading system and incorporates expert opinion.
Hodiamont CJ, Kager PA, Bart A, de Vries HJC, van Thiel PPAM, Leenstra T, et al. Species-directed therapy for leishmaniasis in returning travellers: a comprehensive guide. PLoS Negl Trop Dis. 2014;8:e2832. Species-directed treatment guidelines based on pooled efficacy estimates for available therapies. Final treatment ranking was performed by an expert panel.
Miltefosine (Impavido) for leishmaniasis. Med Lett Drugs Ther. 2014;56:89–90.
Morizot G, Kendjo E, Mouri O, Thellier M, Perignon A, Foulet F, et al. Travelers with cutaneous leishmaniasis cured without systemic therapy. Clin Infect Dis. 2013;57:370–80. Prospective study examining the impact of a standardized treatment algorithm for management of CL in returned French travellers. Demonstrates high cure rates using local therapies in travellers with limited cutaneous disease.
Mansueto P, Seidita A, Vitale G, Cascio A. Leishmaniasis in travelers: a literature review. Travel Med Infect Dis. 2014;12:563–81.
Pavli A, Maltezou HC. Leishmaniasis, an emerging infection in travelers. Int J Infect Dis. 2010;14:e1032–9.
Murray HW. Leishmaniasis in the United States: treatment in 2012. Am J Trop Med Hyg. 2012;86:434–40. Describes increasing use of miltefosine and liposomal amphotericin B for treatment of imported CL in North America. Addresses practical considerations of accessing and administering anti-leishmanial drugs in the United States.
Ehehalt U, Schunk M, Jensenius M, van Genderen PJJ, Gkrania-Klotsas E, Chappuis F, et al. Leishmaniasis acquired by travellers to endemic regions in Europe: a EuroTravNet multi-centre study. Travel Med Infect Dis. 2014;12:167–72.
Magill AJ. Cutaneous leishmaniasis in the returning traveler. Infect Dis Clin North Am. 2005;19:241–66. x–xi.
Aronson NE, Wortmann GW, Byrne WR, Howard RS, Bernstein WB, Marovich MA, et al. A randomized controlled trial of local heat therapy versus intravenous sodium stibogluconate for the treatment of cutaneous Leishmania major infection. PLoS Negl Trop Dis. 2010;4, e628.
WHO. Control of the leishmaniases. Report of a the WHO Expert Committee on the Control of Leishmaniases; 2010 p. 1–186. Report No. 949.
Bailey MS. Cutaneous leishmaniasis in British troops following jungle training in Belize. Travel Med Infect Dis. 2011;9:253–4.
Weina PJ, Neafie RC, Wortmann G, Polhemus M, Aronson NE. Old world leishmaniasis: an emerging infection among deployed US military and civilian workers. Clin Infect Dis. 2004;39:1674–80.
Reveiz L, Maia-Elkhoury ANS, Nicholls RS, Sierra Romero GA, Yadon ZE. Interventions for American cutaneous and mucocutaneous leishmaniasis: a systematic review update. Schallig HDFH, editor. PLoS ONE. 2013;8:e61843. Systematic review of the evidence for treatment of New World CL, including systemic, topical and physical therapies.
Blum J, Lockwood DNJ, Visser L, Harms G, Bailey MS, Caumes E, et al. Local or systemic treatment for New World cutaneous leishmaniasis? Re-evaluating the evidence for the risk of mucosal leishmaniasis. Int Health. 2012;4:153–63. Discusses the use of local and systemic therapy for NWCL in travellers, focusing on risk factors for mucocutaneous leishmanaisis.
Schleucher RD, Zanger P, Gaessler M, Knobloch J. Successful diagnosis and treatment 50 years after exposure: is mucocutaneous leishmaniasis still a neglected differential diagnosis? J Travel Med. 2008;15:466–7.
Asilian A, Sadeghinia A, Faghihi G, Momeni A. Comparative study of the efficacy of combined cryotherapy and intralesional meglumine antimoniate (Glucantime) vs. cryotherapy and intralesional meglumine antimoniate (Glucantime) alone for the treatment of cutaneous leishmaniasis. Int J Dermatol. 2004;43:281–3.
Salmanpour R, Razmavar MR, Abtahi N. Comparison of intralesional meglumine antimoniate, cryotherapy and their combination in the treatment of cutaneous leishmaniasis. Int J Dermatol. 2006;45:1115–6.
El Darouti MA, Al Rubaie SM. Cutaneous leishmaniasis. Treatment with combined cryotherapy and intralesional stibogluconate injection. Int J Dermatol. 1990;29:56–9.
González U, Pinart M, Reveiz L, Alvar J. Interventions for Old World cutaneous leishmaniasis. Cochrane Database Syst Rev. 2008;CD005067.
Ranawaka RR, Weerakoon HS. Randomized, double-blind, comparative clinical trial on the efficacy and safety of intralesional sodium stibogluconate and intralesional 7% hypertonic sodium chloride against cutaneous leishmaniasis caused by L. donovani. J Dermatol Treat. 2010;21:286–93.
Soto J, Rojas E, Guzman M, Verduguez A, Nena W, Maldonado M, et al. Intralesional antimony for single lesions of bolivian cutaneous leishmaniasis. Clin Infect Dis. 2013;56:1255–60. RCT demonstrating superiority of intralesional antimony compared with cryotherapy and placebo for treatment of single lesion CL in Bolivia due to L. braziliensis.
Oliveira-Neto MP, Schubach A, Mattos M, da Costa SC, Pirmez C. Intralesional therapy of American cutaneous leishmaniasis with pentavalent antimony in Rio de Janeiro, Brazil—an area of Leishmania (V.) braziliensis transmission. Int J Dermatol. 1997;36:463–8.
Ben Salah A, Ben Messaoud N, Guedri E, Zaatour A, Ben Alaya N, Bettaieb J, et al. Topical paromomycin with or without gentamicin for cutaneous leishmaniasis. N Engl J Med. 2013;368:524–32. RCT evaluating the efficacy of topical paromomycin and topical paromomycin-gentamicin compared with placebo for cutaneous L. major.
Ben Salah A, Buffet PA, Morizot G, Ben Massoud N, Zâatour A, Ben Alaya N, et al. WR279,396, a third generation aminoglycoside ointment for the treatment of Leishmania major cutaneous leishmaniasis: a phase 2, randomized, double blind, placebo controlled study. PLoS Negl Trop Dis. 2009;3, e432.
el-On J, Halevy S, Grunwald MH, Weinrauch L. Topical treatment of Old World cutaneous leishmaniasis caused by Leishmania major: a double-blind control study. J Am Acad Dermatol. 1992;27:227–31.
Asilian A, Davami M. Comparison between the efficacy of photodynamic therapy and topical paromomycin in the treatment of Old World cutaneous leishmaniasis: a placebo-controlled, randomized clinical trial. Clin Exp Dermatol. 2006;31:634–7.
Krause G, Kroeger A. Topical treatment of American cutaneous leishmaniasis with paramomycin and methylbenzethonium chloride: a clinical study under field conditions in Ecuador. Trans R Soc Trop Med Hyg. 1994;88:92–4.
Sosa N, Capitan Z, Nieto J, Nieto M, Calzada J, Paz H, et al. Randomized, double-blinded, phase 2 trial of WR 279,396 (Paromomycin and Gentamicin) for Cutaneous Leishmaniasis in Panama. Am J Trop Med Hygiene [Internet]. 2013 [cited 2013 Sep 29]; Available from: http://www.ajtmh.org/cgi/doi/10.4269/ajtmh.12-0736
Arana BA, Mendoza CE, Rizzo NR, Kroeger A. Randomized, controlled, double-blind trial of topical treatment of cutaneous leishmaniasis with paromomycin plus methylbenzethonium chloride ointment in Guatemala. Am J Trop Med Hyg. 2001;65:466–70.
Armijos RX, Weigel MM, Calvopiña M, Mancheno M, Rodriguez R. Comparison of the effectiveness of two topical paromomycin treatments versus meglumine antimoniate for New World cutaneous leishmaniasis. Acta Trop. 2004;91:153–60.
Bumb RA, Prasad N, Khandelwal K, Aara N, Mehta RD, Ghiya BC, et al. Long-term efficacy of single-dose radiofrequency-induced heat therapy vs. intralesional antimonials for cutaneous leishmaniasis in India. Br J Dermatol. 2013;168:1114–9.
Reithinger R, Mohsen M, Wahid M, Bismullah M, Quinnell RJ, Davies CR, et al. Efficacy of thermotherapy to treat cutaneous leishmaniasis caused by Leishmania tropica in Kabul, Afghanistan: a randomized, controlled trial. Clin Infect Dis. 2005;40:1148–55.
Safi N, Davis GD, Nadir M, Hamid H, Robert LL, Case AJ. Evaluation of thermotherapy for the treatment of cutaneous leishmaniasis in Kabul, Afghanistan: a randomized controlled trial. Mil Med. 2012;177:345–51.
López L, Cruz C, Godoy G, Robledo SM, Vélez ID. Thermotherapy effective and safer than miltefosine in the treatment of cutaneous leishmaniasis in Colombia. Rev Inst Med Trop Sao Paulo. 2013;55. RCT comparing thermotherapy and miltefosine for CL due to L. panamensis and L. braziliensis in Colombian military personnel.
Velasco-Castrejon O, Walton BC, Rivas-Sanchez B, Garcia MF, Lazaro GJ, Hobart O, et al. Treatment of cutaneous leishmaniasis with localized current field (radio frequency) in Tabasco. Mexico Am J Trop Med Hyg. 1997;57:309–12.
Navin TR, Arana BA, Arana FE, de Mérida AM, Castillo AL, Pozuelos JL. Placebo-controlled clinical trial of meglumine antimonate (glucantime) vs. localized controlled heat in the treatment of cutaneous leishmaniasis in Guatemala. Am J Trop Med Hyg. 1990;42:43–50.
Velez I, Lopez L, Sanchez X, Mestra L, Rojas C, Rodriguez E. Efficacy of miltefosine for the treatment of American cutaneous leishmaniasis. Am J Trop Med Hyg. 2010;83:351–6.
Monge-Maillo B, López-Vélez R. Therapeutic options for old world cutaneous leishmaniasis and new world cutaneous and mucocutaneous leishmaniasis. Drugs. 2013;73:1889–920. Comprehensive evidence-based review of available treatments for Old World and New World CL.
González U, Pinart M, Rengifo-Pardo M, Macaya A, Alvar J, Tweed JA, et al. Interventions for American cutaneous and mucocutaneous leishmaniasis. Cochrane Database Syst Rev. 2009;CD004834.
Neves LO, Talhari AC, Gadelha EPN, Silva Júnior RM da, Guerra JA de O, Ferreira LC de L, et al. A randomized clinical trial comparing meglumine antimoniate, pentamidine and amphotericin B for the treatment of cutaneous leishmaniasis by Leishmania guyanensis. An Bras Dermatol. 2011;86:1092–101.
Chrusciak-Talhari A, Dietze R, Chrusciak Talhari C, da Silva RM, Gadelha Yamashita EP, de Oliveira PG, et al. Randomized controlled clinical trial to access efficacy and safety of miltefosine in the treatment of cutaneous leishmaniasis caused by Leishmania (Viannia) guyanensis in Manaus. Brazil Am J Trop Med Hyg. 2011;84:255–60.
Machado PR, Ampuero J, Guimarães LH, Villasboas L, Rocha AT, Schriefer A, et al. Miltefosine in the treatment of cutaneous leishmaniasis caused by Leishmania braziliensis in Brazil: a randomized and controlled trial. PLoS Negl Trop Dis. 2010;4, e912.
Oliveira LF, Schubach AO, Martins MM, Passos SL, Oliveira RV, Marzochi MC, et al. Systematic review of the adverse effects of cutaneous leishmaniasis treatment in the New World. Acta Trop. 2011;118:87–96.
Firdous R, Yasinzai M, Ranja K. Efficacy of glucantime in the treatment of Old World cutaneous leishmaniasis. Int J Dermatol. 2009;48:758–62.
Mohebali M, Fotouhi A, Hooshmand B, Zarei Z, Akhoundi B, Rahnema A, et al. Comparison of miltefosine and meglumine antimoniate for the treatment of zoonotic cutaneous leishmaniasis (ZCL) by a randomized clinical trial in Iran. Acta Trop. 2007;103:33–40.
Sadeghian G, Nilforoushzadeh MA. Effect of combination therapy with systemic glucantime and pentoxifylline in the treatment of cutaneous leishmaniasis. Int J Dermatol. 2006;45:819–21.
Negera E, Gadisa E, Hussein J, Engers H, Kuru T, Gedamu L, et al. Treatment response of cutaneous leishmaniasis due to Leishmania aethiopica to cryotherapy and generic sodium stibogluconate from patients in Silti, Ethiopia. Trans R Soc Trop Med Hyg. 2012;106:496–503.
Rubiano LC, Miranda MC, Muvdi Arenas S, Montero LM, Rodríguez-Barraquer I, Garcerant D, et al. Noninferiority of miltefosine versus meglumine antimoniate for cutaneous leishmaniasis in children. J Infect Dis. 2012;205:684–92. RCT of miltefosine versus systemic antimonials for CL due to L. panamensis and L. guyanensis in Colombia. One of the few RCTs focusing on outcomes in children.
Soto J, Arana BA, Toledo J, Rizzo N, Vega JC, Diaz A, et al. Miltefosine for new world cutaneous leishmaniasis. Clin Infect Dis. 2004;38:1266–72.
Soto J, Toledo J, Gutierrez P, Nicholls RS, Padilla J, Engel J, et al. Treatment of American cutaneous leishmaniasis with miltefosine, an oral agent. Clin Infect Dis. 2001;33:E57–61.
Soto J, Rea J, Balderrama M, Toledo J, Soto P, Valda L, et al. Efficacy of miltefosine for Bolivian cutaneous leishmaniasis. Am J Trop Med Hyg. 2008;78:210–1.
Van Thiel PPAM, Leenstra T, Kager PA, de Vries HJ, van Vugt M, van der Meide WF, et al. Miltefosine treatment of Leishmania major infection: an observational study involving Dutch Military Personnel Returning from Northern Afghanistan. Clin Infect Dis. 2010;50:80–3.
Harms G, Scherbaum H, Reiter-Owona I, Stich A, Richter J. Treatment of imported New World cutaneous leishmaniasis in Germany. Int J Dermatol. 2011;50:1336–42.
Solomon M, Pavlotzky F, Barzilai A, Schwartz E. Liposomal amphotericin B in comparison to sodium stibogluconate for Leishmania braziliensis cutaneous leishmaniasis in travelers. J Am Acad Dermatol. 2013;68:284–9. Prospective observational study demonstrating high cure rates of liposomal amphotericin B for cutaneous L. braziliensis in a small cohort of Israeli travellers.
Wortmann G, Zapor M, Ressner R, Fraser S, Hartzell J, Pierson J, et al. Lipsosomal Amphotericin B for treatment of cutaneous leishmaniasis. Am J Trop Med Hyg. 2010;83:1028–33.
Solomon M, Pavlotsky F, Leshem E, Ephros M, Trau H, Schwartz E. Liposomal amphotericin B treatment of cutaneous leishmaniasis due to Leishmania tropica. J Eur Acad Dermatol Venereol. 2011;25:973–7.
Emad M, Hayati F, Fallahzadeh MK, Namazi MR. Superior efficacy of oral fluconazole 400 mg daily versus oral fluconazole 200 mg daily in the treatment of cutaneous leishmania major infection: a randomized clinical trial. J Am Acad Dermatol. 2011;64:606–8.
Alrajhi AA, Ibrahim EA, De Vol EB, Khairat M, Faris RM, Maguire JH. Fluconazole for the treatment of cutaneous leishmaniasis caused by Leishmania major. N Engl J Med. 2002;346:891–5.
Morizot G, Delgiudice P, Caumes E, Laffitte E, Marty P, Dupuy A, et al. Healing of Old World cutaneous leishmaniasis in travelers treated with fluconazole: drug effect or spontaneous evolution? Am J Trop Med Hyg. 2007;76:48–52.
Sousa AQ, Frutuoso MS, Moraes EA, Pearson RD, Pompeu MML. High-dose oral fluconazole therapy effective for cutaneous leishmaniasis due to Leishmania (Vianna) braziliensis. Clin Infect Dis. 2011;53:693–5.
Soto-Mancipe J, Grogl M, Berman JD. Evaluation of pentamidine for the treatment of cutaneous leishmaniasis in Colombia. Clin Infect Dis. 1993;16:417–25.
Lai A, Fat EJSK, Vrede MA, Soetosenojo RM, Lai A, Fat RFM. Pentamidine, the drug of choice for the treatment of cutaneous leishmaniasis in Surinam. Int J Dermatol. 2002;41:796–800.
Van der Meide WF, Sabajo LOA, Jensema AJ, Peekel I, Faber WR, Schallig HDFH, et al. Evaluation of treatment with pentamidine for cutaneous leishmaniasis in Suriname. Int J Dermatol. 2009;48:52–8.
Andersen EM, Cruz-Saldarriaga M, Llanos-Cuentas A, Luz-Cjuno M, Echevarria J, Miranda-Verastegui C, et al. Comparison of meglumine antimoniate and pentamidine for peruvian cutaneous leishmaniasis. Am J Trop Med Hyg. 2005;72:133–7.
The Medical Letter. Drugs for parasitic infections. 3rd ed. New York: The Medical Letter, Inc; 2013.
Jones TC, Johnson WD, Barretto AC, Lago E, Badaro R, Cerf B, et al. Epidemiology of American cutaneous leishmaniasis due to Leishmania braziliensis braziliensis. J Infect Dis. 1987;156:73–83.
Davies CR, Reithinger R, Campbell-Lendrum D, Feliciangeli D, Borges R, Rodriguez N. The epidemiology and control of leishmaniasis in Andean countries. Cad Saude Publica. 2000;16:925–50.
Machado-Coelho GLL, Caiaffa WT, Genaro O, Magalhães PA, Mayrink W. Risk factors for mucosal manifestation of American cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 2005;99:55–61.
Muñoz G, Davies CR. Leishmania panamensis transmission in the domestic environment: the results of a prospective epidemiological survey in Santander, Colombia. Biomedica. 2006;26 Suppl 1:131–44.
Tavares CAP, Fernandes AP, Melo MN. Molecular diagnosis of leishmaniasis. Expert Rev Mol Diagn. 2003;3:657–67.
Murray HW, Berman JD, Davies CR, Saravia NG. Advances in leishmaniasis. Lancet. 2005;366:1561–77.
Singh S. New developments in diagnosis of leishmaniasis. Indian J Med Res. 2006;123:311–30.
Bensoussan E, Nasereddin A, Jonas F, Schnur LF, Jaffe CL. Comparison of PCR assays for diagnosis of cutaneous leishmaniasis. J Clin Microbiol. 2006;44:1435–9.
Boggild AK, Valencia BM, Veland N, Pilar Ramos A, Calderon F, Arevalo J, et al. Non-invasive cytology brush PCR diagnostic testing in mucosal leishmaniasis: superior performance to conventional biopsy with histopathology. El-Sayed NM, editor. PLoS ONE. 2011;6:e26395.
Boggild AK, Valencia BM, Espinosa D, Veland N, Ramos AP, Arevalo J, et al. Detection and species identification of Leishmania DNA from filter paper lesion impressions for patients with American cutaneous leishmaniasis. Clin Infect Dis. 2010;50:e1–6.
Mosimann V, Neumayr A, Hatz C, Blum JA. Cutaneous leishmaniasis in Switzerland: first experience with species-specific treatment. Infection. 2013;41:1177–82.
Bailey MS, Lockwood DNJ. Cutaneous leishmaniasis. Clin Dermatol. 2007;25:203–11.
Ben Salah A, Zakraoui H, Zaatour A, Ftaiti A, Zaafouri B, Garraoui A, et al. A randomized, placebo-controlled trial in Tunisia treating cutaneous leishmaniasis with paromomycin ointment. Am J Trop Med Hyg. 1995;53:162–6.
Dowlati Y. Cutaneous leishmaniasis: clinical aspect. Clin Dermatol. 1996;14:425–31.
Herwaldt BL, Arana BA, Navin TR. The natural history of cutaneous leishmaniasis in Guatemala. J Infect Dis. 1992;165:518–27.
Kim DH, Chung HJ, Bleys J, Ghohestani RF. Is paromomycin an effective and safe treatment against cutaneous leishmaniasis? A meta-analysis of 14 randomized controlled trials. PLoS Negl Trop Dis. 2009;3, e381.
Sadeghian G, Nilfroushzadeh MA, Iraji F. Efficacy of local heat therapy by radiofrequency in the treatment of cutaneous leishmaniasis, compared with intralesional injection of meglumine antimoniate. Clin Exp Dermatol. 2007;32:371–4.
Valencia BM, Miller D, Witzig RS, Boggild AK, Llanos-Cuentas A. Novel low-cost thermotherapy for cutaneous leishmaniasis in Peru. PLoS Negl Trop Dis. 2013;7, e2196.
López L, Robayo M, Vargas M, Vélez ID. Thermotherapy. An alternative for the treatment of American cutaneous leishmaniasis. Trials. 2012;13:58.
Miranda-Verástegui C, Llanos-Cuentas A, Arévalo I, Ward BJ, Matlashewski G. Randomized, double-blind clinical trial of topical imiquimod 5% with parenteral meglumine antimoniate in the treatment of cutaneous leishmaniasis in Peru. Clin Infect Dis. 2005;40:1395–403.
Arevalo I, Tulliano G, Quispe A, Spaeth G, Matlashewski G, Llanos-Cuentas A, et al. Role of imiquimod and parenteral meglumine antimoniate in the initial treatment of cutaneous leishmaniasis. Clin Infect Dis. 2007;44:1549–54.
Miranda-Verastegui C, Tulliano G, Gyorkos TW, Calderon W, Rahme E, Ward B, et al. First-line therapy for human cutaneous leishmaniasis in Peru using the TLR7 agonist imiquimod in combination with pentavalent antimony. PLoS Negl Trop Dis. 2009;3, e491.
Netto EM, Marsden PD, Llanos-Cuentas EA, Costa JM, Cuba CC, Barreto AC, et al. Long-term follow-up of patients with Leishmania (Viannia) braziliensis infection and treated with Glucantime. Trans R Soc Trop Med Hyg. 1990;84:367–70.
Croft SL, Sundar S, Fairlamb AH. Drug resistance in leishmaniasis. Clin Microbiol Rev. 2006;19:111–26.
Reithinger R, Dujardin J-C, Louzir H, Pirmez C, Alexander B, Brooker S. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581–96.
Wise ES, Armstrong MS, Watson J, Lockwood DN. Monitoring toxicity associated with parenteral sodium stibogluconate in the day-case management of returned travellers with New World cutaneous leishmaniasis [corrected]. PLoS Negl Trop Dis. 2012;6, e1688.
Mlika RB, Hamida MB, Hammami H, Jannet SB, Badri T, Fenniche S, et al. Should we continue to indicate meglumine antimoniate as first-line treatment for cutaneous leishmaniasis in Tunisia. Dermatol Ther. 2012;25:615–8.
Romero GA, Guerra MV, Paes MG, Macêdo VO. Comparison of cutaneous leishmaniasis due to Leishmania (Viannia) braziliensis and L. (V.) guyanensis in Brazil: therapeutic response to meglumine antimoniate. Am J Trop Med Hyg. 2001;65:456–65.
Rojas R, Valderrama L, Valderrama M, Varona MX, Ouellette M, Saravia NG. Resistance to antimony and treatment failure in human Leishmania (Viannia) infection. J Infect Dis. 2006;193:1375–83.
Bailey MS, Green AD, Ellis CJ, O’Dempsey TJ, Beeching NJ, Lockwood DN, et al. Clinical guidelines for the management of cutaneous leishmaniasis in British military personnel. J R Army Med Corps. 2005;151:73–80.
Escobar P, Matu S, Marques C, Croft SL. Sensitivities of Leishmania species to hexadecylphosphocholine (miltefosine), ET-18-OCH(3) (edelfosine) and amphotericin B. Acta Trop. 2002;81:151–7.
Dorlo TPC, van Thiel PPAM, Huitema ADR, Keizer RJ, de Vries HJC, Beijnen JH, et al. Pharmacokinetics of miltefosine in Old World cutaneous leishmaniasis patients. Antimicrob Agents Chemother. 2008;52:2855–60.
Navin TR, Arana BA, Arana FE, Berman JD, Chajón JF. Placebo-controlled clinical trial of sodium stibogluconate (Pentostam) versus ketoconazole for treating cutaneous leishmaniasis in Guatemala. J Infect Dis. 1992;165:528–34.
Compliance with Ethics Guidelines
Conflict of Interest
Andrea Boggild and Adrienne Showler have no disclosures relevant to this work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Tropical, Travel and Emerging Infections
Rights and permissions
About this article
Cite this article
Showler, A.J., Boggild, A.K. Cutaneous Leishmaniasis in Travellers: a Focus on Epidemiology and Treatment in 2015. Curr Infect Dis Rep 17, 37 (2015). https://doi.org/10.1007/s11908-015-0489-2
Published:
DOI: https://doi.org/10.1007/s11908-015-0489-2