Abstract
Purpose of Review
To elucidate the hemodynamic, autonomic, vascular, hormonal, and local mechanisms involved in the blood pressure (BP)–lowering effect of dynamic resistance training (DRT) in prehypertensive and hypertensive populations.
Recent Findings
The systematic search identified 16 studies involving 17 experimental groups that assessed the DRT effects on BP mechanisms in prehypertensive and/or hypertensive populations. These studies mainly enrolled women and middle-aged/older individuals. Vascular effects of DRT were consistently reported, with vascular conductance, flow-mediated dilation, and vasodilatory capacity increases found in all studies. On the other hand, evidence regarding the effects of DRT on systemic hemodynamics, autonomic regulation, hormones, and vasoactive substances are still scarce and controversial, not allowing for any conclusion.
Summary
The current literature synthesis shows that DRT may promote vascular adaptations, improving vascular conductance and endothelial function, which may have a role in the BP-lowering effect of this type of training in prehypertensive and hypertensive individuals. More studies are needed to explore the role of other mechanisms in the BP-lowering effect of DRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is estimated to affect 1 billion individuals worldwide. It is considered a major cardiovascular risk factor, causing 8 million deaths per year with most of them because of stroke, myocardial infarct, or sudden death [1]. Regarding its pathophysiological mechanisms, hypertension is determined by high cardiac output (CO) in few specific cases (e.g., early disease stage), but its most common hemodynamic determinant is the increase in systemic vascular resistance (SVR) caused by mechanisms such as elevated sympathetic vasomotor tone, hyperactivity of the renin-angiotensin-aldosterone system (RAAS), and vascular dysfunction and remodeling [2].
Despite the expressive progress on the efficacy of pharmacological antihypertensive treatment, the rates of blood pressure (BP) control among the hypertensive individuals remain low (i.e., 43.5%) [3••], highlighting the importance of non-pharmacological approaches. Additionally, these approaches also prevent hypertension development, which is relevant since the absolute hypertension burden has increased in the last decades [4]. Therefore, as part of the non-pharmacological approach, exercise training is recommended as a first-line therapy for individuals with prehypertension and stage 1 hypertension and is indicated as a complementary intervention to pharmacological treatment for hypertensive individuals at the other stages [5, 6].
Classically, guidelines recommend aerobic training in hypertension because of the high level of evidence regarding its BP-lowering effect [3••, 5, 6]. However, more recently, dynamic resistance training (DRT) was also included as a non-pharmacological intervention for hypertension prevention and treatment, as highlighted in the American College of Cardiology and American Heart Association Guideline for High Blood Pressure Management [3••]. DRT, also called strength training, is composed of exercises in which force is exerted against a resistance with alternated phases of muscle shortening and lengthening [7]. A meta-analysis [8••] including 64 controlled trials (n=2344 participants) reported significant reductions of systolic (SBP) and diastolic (DBP) BPs after DRT, with greater reduction associated with higher baseline BP [i.e., hypertensive individuals, −5.7 (IC: −9.0, −2.7) / −5.2 (−8.4, −1.9); prehypertensive individuals, −3.0 (−5.1, −1.0) / −3.3 (−5.3, −1.4); normotensive individuals, 0.0 (−2.5, 2.5) / −0.9 (−2.1, 2.2) mmHg for ∆SBP/∆DBP].
Despite the recommendation of DRT for hypertension prevention and treatment, little is known regarding the mechanisms responsible for the BP-lowering effect of this type of training as most of the studies did not include any mechanistic measure [9]. However, some investigations have studied the effects of DRT on isolated mechanisms related to BP control, assessing markers of autonomic modulation, vascular function, hormonal regulation, or others. Therefore, it is interesting to join this information within a comprehensive literature synthesis about the possible mechanisms behind the BP-lowering effect of DRT, exposing the strength and weakness of the current scientific evidence. This synthesis can drive future experimental and clinical trials on this subject, leading to a more precise development of the knowledge in this area of investigation.
Thus, this study reviewed the current literature about the effects of DRT on BP hemodynamic, autonomic, hormonal, and vascular mechanisms, aiming to synthesize them in a possible model for the BP-lowering effect of DRT.
Methods
Literature Search
A systematic literature review was conducted in the US National Library of Medicine and National Institutes of Health (i.e., PubMed) database. Multiple advanced searches were performed including key terms related to the population (“hypertension” OR “hypertensive” OR ‘hypertensives” OR “prehypertension” OR “prehypertensive” OR “prehypertensives” OR “pre-hypertension” OR “pre-hypertensive” OR “pre-hypertensives”), the intervention (“resistance exercise” OR “strength exercise” OR “resistance training” OR “strength training”), and the outcome (“hemodynamic” OR “cardiac output” OR “stroke volume” OR “heart rate” OR “autonomic” OR “sympathetic” OR “parasympathetic” OR “vagal” OR “sympathovagal” OR “vasomotor” OR “baroreflex” OR “vascular” OR “endothelial” OR “arterial diameter” OR “nitric oxide” OR “flow-mediated dilation” OR “blood flow” OR “vasoactive” OR “vasodilation” OR vasodilatory capacity” OR “angiotensin” OR “renin-angiotensin” OR “endothelin” OR “catecholamines” OR “epinephrine” OR “adrenaline” OR “norepinephrine” OR noradrenaline). The search included all sources up to October 9, 2020. Manual searches upon the reference lists of the identified articles were also performed to complement the database search.
Selection Criteria
Records identified by database and manual search were initially analyzed based on their title and abstract review and excluded if they did not attend the following criteria: (1) to be a clinical trial; (2) to be conducted with humans; (3) to have investigated prehypertensive and/or hypertensive individuals; (4) to have assessed the chronic effects of DRT; and (5) to have included at least one group that had performed only DRT (i.e., not in combination with aerobic training). The full texts of the remaining studies were assessed for eligibility and excluded due to the following criteria: (1) any exclusion criterion of the screening phase was identified; (2) have not assessed a BP control mechanism; and (3) have performed sub-analyses or presented the same data of another included study.
Data were extracted by one author (RYF) and checked by another (LCB), and discrepancies were resolved by critical discussion. Descriptive data regarding the characteristics of the sample (gender, age, clinical status, and antihypertensive use), the DRT protocol (volume, intensity, frequency, and intervention length), and the experimental design (study arms and sample size) were extracted from each included study. Afterwards, the effects of DRT on BP mechanisms reported by each paper were analyzed.
Results
A flow diagram describing the search and screening process is shown in Fig. 1. The initial database search identified 316 records, and 2 other records were identified by a manual search, totalizing 318 records. By titles and abstracts review, 290 studies were identified for not fulfilling this review criteria, and by full paper reading, another 12 papers were excluded. Thus, 16 studies were included and analyzed [10,11,12,13,14, 15•, 16,17,18, 19•, 20,21,22,23,24,25]. As one of them [22] compared two different protocols of DRT (i.e., non-periodized vs. periodized), this review included the effects of DRT in 17 different experimental groups.
Study Characteristics
Study characteristics are shown in Table 1. Half of the studies (n=8) involved samples composed of both men and women, while 6 (37.5%) studies included only women and two studies (12.5%) involved only men. The great majority (87.5%) of the studies involved middle-aged or older individuals, and all (except for one) that studied only women involved only older women. Prehypertensive individuals were included in 7 studies (43.8%), while hypertensive individuals (81.3%) were investigated in 13 studies. In five studies, prehypertension was defined based on the 7th Joint National Committee’s cutoff point (i.e., SBP/DBP between 120/80 and 139/89) [26], while in two studies, elevated BP was based on the criteria of the 6th Brazilian Guideline of Arterial Hypertension [27] or the consensus statement of the International Diabetes Federation [28] (i.e., SBP/DBP between 130/85 and 139/89). Considering the studies with hypertensive individuals, six studies defined hypertension by previous diagnosis or use of antihypertensive therapy, while other six considered hypertension as BP levels higher than 140/90 mmHg [26, 27], and one used both criteria (i.e., antihypertensive drug use or BP > 140/90 mmHg). Antihypertensive medication use was cited in 11 (68.8%) studies.
DRT frequency varied from 2 to 3 sessions per week. Training period varied from 1 to 6 months with most of the studies presenting training periods between 8 and 12 weeks (n=10, 62.5%). Training protocol varied considerably among the studies. The number of exercises varied from 3 to 11, the number of sets from 1 to 4, and the number of repetitions from 8–10 to 15–20. Exercise intensity was established as 50 to 80% of 1RM in 5 studies, was based on 10–15 RM in 3 studies, was defined based on subjective effort in 3 studies, used other methods (number of repetitions or percentage of 10RM) in 4 studies, and was not reported in 1 study.
DRT Effects
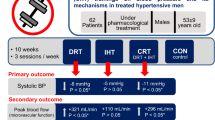
Results from each study and a summary of results for each variable are presented, respectively, in Table 2 and Fig. 2.
Absolute number of experimental conditions from the reviewed studies with prehypertensive and/or hypertensive individuals that found changes that favor and do not favor a blood pressure lowering effect of dynamic resistance training. Variables analysed were systolic blood pressure (SBP); diastolic blood pressure (DBP); mean blood pressure (MBP); cardiac output (CO); stroke volume (SV); heart rate (HR); systemic vascular resistance (SVR); vascular conductance; vasodilatory capacity; flow mediated dilation (FMD); nitric oxide (NO); arterial diameter; sympathetic vasomotor modulation (LF_SBP); and pressor hormones. Results favoring blood pressure lowering were defined by a significant decrease for CO, SVR, SV, HR, sympathovagal balance, LF_SBP, and pressor hormones and by a significant increase for vascular conductance, vasodilatory capacity, FMD, and arterial diameter
SBP and DBP responses to DRT evaluated in 16 experimental groups showed a decrease in SBP in 11 groups (68.8%) and a decrease in DBP in 9 groups (56.3%). Six of 8 (75.0%) experimental groups that assessed MBP showed a reduction after DRT. In only 4 experimental groups, DRT did not promote any BP-lowering effect on SBP, DBP, or MBP.
Systemic hemodynamic determinants of BP were only assessed in one experimental group in which DRT did not change CO, SVR, nor BP. Additionally, HR was assessed in 8 experimental groups and decreased after DRT in 4 (50.0%), did not change in 3 (37.5%), and increased in 1 of them (12.5%). Stroke volume (SV) was decreased in the only study that measured it.
Cardiac autonomic regulation was assessed in 3 experimental groups by means of HR variability. Almost all indexes assessed in these experimental groups did not change with DRT, except for the 0V% index that increased after DRT (33.3%). Vasomotor sympathetic modulation was assessed in only 1 experimental group through the low-frequency component of SBP variability, and it decreased after DRT.
Pressor hormones (i.e., catecholamines, markers of the renin-angiotensin-aldosterone system, vasopressin, and kinins) were measured in 3 experimental groups, but they did not change in any of them.
Local hemodynamics were evaluated in 4 experimental groups. All of them assessed the upper limb (arm or forearm), and one experimental group had lower limb (calf) hemodynamics assessed. Upper limb vascular conductance increased in all experimental groups (3 studies), and blood flow increased in 2 of 3 groups (66.6%). Calf vascular conductance and blood flow increased after DRT in the only experimental group that had this variable assessed.
Regarding vascular function, vasodilatory capacity was assessed by plethysmography in 2 experimental groups and by flow-mediated dilation using ultrasonography in another 4. These parameters increased in all the experimental groups. The brachial diameter was measured in 3 experimental groups and did not change in any of them after TRD.
Different vasoactive substances were measured in 7 experimental groups. Markers of nitric oxide (NO) were measured in all of them and did not change in 4 (57.1%), increased in 2 (28.6%), and decreased in one (14.3%). Endothelin and prostacyclin markers were assessed in two experimental groups, being unchanged in one (50.0%), whereas the other presented a decrease in endothelin 1 and an increase on prostacyclin (50.0%).
Discussion
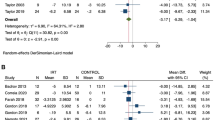
The current systematic review showed that mechanisms responsible for the BP-lowering effect of DRT in prehypertensive and hypertensive individuals have been poorly investigated in literature, with results mainly sustained by studies with middle-aged or older women. The most robust available evidence regarding these mechanisms is limited to local hemodynamics, suggesting that the BP-lowering effect of DRT is accompanied by increased vascular conductance and vasodilatory responses, while there is poor or no evidence that DRT affects systemic hemodynamics, cardiovascular autonomic regulation, RAAS components, or vasoactive substances (Fig. 3).
Summary model showing the actual evidence regarding the possible mechanisms involved in the blood pressure lowering effect of dynamic resistance training (DRT) in pre-hypertensive and/or hypertensive individuals. NO, nitric oxide; RAAS, renin-angiotensin-aldosterone system. ?, available literature presents scare results (i.e., just one study was performed); →, available literature indicates that DRT does not change this outcome; ↑, available literature indicates that DRT increases this outcome; ↓, available literature indicates that DRT decreases this outcome
The current review found scarce data regarding the hemodynamic determinant of the BP-lowering effect of DRT. As BP is determined by the product between CO and SVR and hypertension is caused by pathologic elevations in one or both of these factors [2], the effect of DRT lowering BP must involve a decrease of CO (central adaptation) and/or SVR (peripheral adaptation). Nevertheless, in line with previous reports in normotensives [29, 30], the only study [12] that assessed these outcomes in hypertensive individuals did not observe any effect of DRT on BP, CO, or SVR. Thus, more studies are required to reveal the systemic hemodynamic determinant of the BP-lowering effect of DRT. However, based on the evidence revealed by this review regarding local hemodynamics and vascular function, an effect on peripheral mechanisms seems more probable.
Central Adaptations
CO is determined by the product between SV or HR [31]. Studies with middle-aged and older normotensive individuals have consistently shown no change in SV after DRT [29, 30]. On the other hand, in the current review, the only study that assessed SV in hypertensive individuals [12] observed a significant decrease after 6 months of DRT. Nevertheless, despite this reduction, CO did not change because HR increased after DRT, suggesting that changes in SV may be compensated by HR changes. Additionally, in this specific study, BP did not decrease after training. Thus, an SV reduction may be obtained with DRT, but more studies are needed to verify this effect, and they may also consider the HR responses. Moreover, it is important to keep in mind that hypertension is not usually associated with an increase in SV [2], suggesting that a decrease in this parameter may not compensate for the disease pathophysiological mechanisms.
Many studies have evaluated HR responses to DRT, but their results are controversial. A HR-lowering effect was found in four experimental groups, with DRT decreasing HR in two of them [23, 25] and preventing the increase in HR observed in the control group in the other two [22]. However, the other half of the studies did not observe any HR decrease after DRT [12, 13, 17, 18]. Considering HR autonomic regulation, three studies evaluated HR variability [11, 13, 25], and in two of them [11, 13], HR variability parameters did not change with DRT, suggesting no effect on central autonomic regulation. On the other hand, the third study [25] reported a reduction of HR (Cohen’s d = 1.20; large effect) accompanied by a decrease in 0V% (Cohen’s d = 0.88; moderate effect) that is a marker of cardiac sympathetic modulation. However, in this study, other indices related to cardiac sympathetic modulation (i.e., LFR-R and LF/HF) were not changed by DRT. Thus, the effects of DRT on HR and its autonomic regulation remain unclear and need future elucidation.
Therefore, together, the current evidence does not support a decrease in CO as the main hemodynamic systemic mechanism responsible for the BP-lowering effect of DRT because DRT seems not to promote resting bradycardia as a hallmark response, and even when DRT decreases SV, a compensatory increase in HR may happen. Nevertheless, it is possible that DRT decreases CO in those hypertensive individuals with elevated CO as the main hypertensive mechanism, which should be assessed by future research.
Peripheric Adaptations to DRT
SVR is determined by many mechanisms, such as local hemodynamics, vascular function, vasomotor autonomic regulation, hormonal influences, and vasoactive substances.
The current review revealed a consistent effect of DRT on local hemodynamics and vascular function. Along this line, baseline blood flow and vascular conductance increased after DRT in almost all studies that assessed these variables. Additionally, in one study [17], these variables were assessed in different vascular beds (forearm and calf), and the increase was observed in both sites, which may reflect the whole-body DRT protocol employed in the study.
The current review also indicates an DRT effect improving the vascular function of the resistance vessels. This effect was observed in two studies that reported an increased vasodilatory response to reactive hyperemia when assessed by plethysmography [14, 17]. In one of these studies [17], the improvement occurred on both arm and calf, showing a whole-body effect. Additionally, in prehypertensive individuals, the improvement obtained with DRT resulted in a vasodilatory capacity greater than observed in normotensive individuals. Finally, in prehypertensive and hypertensive individuals, the improvement has been shown to be greater than observed with aerobic training [14].
The present findings also suggest an effect of DRT on conduit vessels, improving endothelial function measured by FMD. Concerning these effects, a previous meta-analysis [32] involving 396 subjects with different clinical characteristics (e.g., congestive heart failure, coronary artery disease and peripheral artery disease, type 2 diabetes, and healthy individuals) has already reported an overall effect of DRT improving FMD. Thus, the current review confirmed this effect in individuals with high BP since all four studies [15•, 16, 19•, 20] that have assessed FMD reported an increase after DRT. Interestingly, these studies involved different samples including young prehypertensive individuals [16], medicated hypertensive individuals [15•], a mix of prehypertensive and medicated hypertensive individuals [19•], and individuals with metabolic syndrome and elevated BP [20]. Among these studies, Beck et al. [16] reported that DRT was able to revert the endothelial dysfunction present in prehypertension. Additionally, these studies reported that DRT effects on FMD were similar to those reported for moderate continuous aerobic training [16, 19•], high-intensity interval training [20], and combined training [19•, 20].
The mechanisms explaining vascular function improvement induced by DRT are out of the scope of this review. However, it is possible to speculate that shear stress increase produced during exercise may be involved. Skeletal muscle contractions increase the production of vasodilatory factors (e.g., CO2, adenosine, lactate/H+, and K+) [33]. However, during dynamic resistance exercise, the contracted muscle mass around the blood vessels imposes a mechanic restriction to blood flow increase [34]. Nevertheless, after each repetition and set, the cessation of contraction allows for the increase in blood flow, reflecting an ischemia/reperfusion condition that may acutely increase shear stress and chronically improve vascular function [31, 35]. Future studies, however, should confirm the role of shear stress on this improvement.
The vascular function improvements reported on both conduit and resistance vessels after DRT might reflect a more favorable vasoactive balance [31]. Along this line, Beck et al. [16] reported a favorable vasoactive balance after DRT characterized by a concomitant increase on humoral markers of NO and prostacyclin with a decrease of endothelin 1. Additionally, another study [10] found NO increase after DRT to be inversely correlated with SBP decrease (r=-0.63; p<0.05). The increase of NO bioavailability with DRT could be a consequence of enhanced oxidant/antioxidant balance [24] after DRT. However, it is important to mention that the other 5 studies that measured NO markers and the other study that assessed prostaglandin and endothelin found different results. Thus, future studies should confirm the favorable effect of DRT over vasoactive balance. The dissociation concerning the controversial effect of DRT on NO and the well-shown increase of endothelial function produced by this training might be explained by the fact that endothelial function was measured after a stimulus while NO markers were assessed in baseline conditions. Future studies should consider this aspect.
Despite the consistent effect on vascular function, the current literature review did not show any DRT effect on vascular structure as none of the studies reported brachial arterial diameter changes after training. This absence of effect might reflect the short length of the interventions (i.e., 8 to 12 weeks) given that structural adaptations might require longer periods to occur than functional adaptations [36]. Actually, a study with young healthy men [37] reported an increase in brachial arterial diameter and a decrease in wall-to-lumen ratio after 6 months of DRT. Future studies with longer periods of training should be designed to verify whether DRT can affect the hypertension-induced vessel remodeling.
Vascular function and structure are affected by neural and hormonal mechanisms. In the current review, the only study that evaluated the effects of DRT on vascular autonomic regulation reported a decrease in BP variability (low-frequency band in spectral analyses) similar to the reduction observed in a parallel group that performed aerobic training [13]. As BP variability is a marker of vasomotor sympathetic modulation, this result suggests that DRT may decrease muscle sympathetic nerve activity (MSNA) in individuals with high BP. However, no study has directly assessed MSNA in individuals with elevated BP, and a study with normotensives reported no change [38]. Nevertheless, high BP levels are associated with altered MSNA, which may potentiate an effect of DRT decreasing this activity in individuals with elevated BP, which still need to be investigated.
Regarding vasoactive hormones, all the studies in the current review that focused on RAAS components found no significant effect. Moraes et al. [21] investigated hypertensive individuals employing a comprehensive evaluation including humoral concentrations of angiotensin I, angiotensin II, angiotensin 1–7, and ACE activity. Cononie et al. [12] evaluated angiotensin I and angiotensin II in pooled and separated analyses of normotensive and hypertensive individuals. Beck et al. [16] studied young prehypertensive individuals and measured angiotensin II plasma concentration. Therefore, there is no evidence of a DRT effect on RAAS. However, humoral concentrations of RAAS markers do not necessarily reflect tissue (local) RAAS activity, and future studies should evaluate the effects of DRT on local angiotensin II.
Additional Considerations
The present results add new information about the role of DRE in hypertension prevention and treatment. Despite the BP-lowering effect of this type of training that supports its recommendation in prehypertension [39] and hypertension [8••], the present review found vascular function improvement as the main mechanism for this effect. As vascular dysfunction is associated with increased risk for hypertension development (with a reduction of 0.62% in FMD associated with an increase of 20 mmHg in SBP) [40] and cardiovascular events in patients with cardiovascular diseases (with a reduction of 1 standard deviation in FMD doubling the risk of cardiovascular events) [41], the effect of DRT improving vascular function strengthens its recommendation for hypertension prevention and treatment.
It is important to mention some limitations of this review. The literature search was performed only in PubMed, and more data may be found in other databases. However, the execution of additional manual searches based on studies’ references list might have attenuated this potential bias. Although only studies with prehypertensive and hypertensive individuals were included, there was a high heterogeneity among the samples regarding BP levels (prehypertensive or controlled hypertensive or uncontrolled hypertensive individuals), BP status definition (based on different cutoff values or pre-participation diagnosis or antihypertensive use), and antihypertensive treatment (untreated or treated with different medication classes). Although this heterogeneity is common in literature, the mechanisms behind the BP-lowering effect of DRT might differ among the specific groups, which need more data and standardized population definition to be investigated. Additionally, although age and sex are known to influence BP level [42] and its mechanisms, such as vascular function [43], very few data in the present review derived from studies with young adults or only with men. Despite these data pointed out for vascular benefits of DRT in young individuals [16, 17] and in men [14, 16, 17], more studies are needed especially because an improvement in these populations might have an important impact on hypertension prevention. As many studies’ main outcome was the effect of DRT on BP, it is also possible that some of them were adequately powered to detect BP changes, but not BP mechanism alterations. Therefore, it would be important to conduct future studies establishing BP mechanisms as the main outcomes.
Conclusion
Based on the findings and discussion of this review, the need for more investigations regarding the mechanisms behind the BP-lowering effect of DRT is clear. Nevertheless, the current literature synthesis indicates that DRT may promote vascular adaptations, improving vascular conductance and endothelial function, which may have a role in the BP-lowering effect of this type of training. On the other hand, there is no robust evidence to support that DRT decreases sympathetic activity nor RAAS activity, while its effects on vasoactive substances are controversial.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lawes CM, Hoorn S, Vander RA. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Beevers G, Lip GY, O’Brien E. The pathophysiology of hypertension. BMJ. 2001;322:912–6.
•• Whelton PK, Carey RM, Aronow WS, Ovbiagele B, Casey DE, Smith SC, et al. 2017 ACC / AHA / AAPA / ABC / ACPM / AGS / APhA / ASH / ASPC / NMA / PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association T. Hypertension. 2018;71:1269–324. This important guideline for hypertension management was the first to establish dynamic resistance training as one of the best proven nonpharmacological interventions.
Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline. J Am Heart Assoc. 2018;7:e008888.
Williams B, Mancia G, Spiering W, Rosei E, Azizi M, Burnier M. 2018 ESC/ESH Guidelines for the management of arterial hypertension. J Hypertens. 2018;36:1953–2041.
Malachias M, Souza W, Plavnik F, Rodrigues C, Sociedade Brasileira de Cardiologia. 7a Diretriz Brasileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107:1–83 Available from: www.arquivosonline.com.br.
Kraemer WJ, Ratamess NA, Flanagan SD, Shurley JP, Todd JS, Todd TC. Understanding the science of resistance training: an evolutionary perspective. Sport Med Springer International Publishing. 2017;47:2415–35.
•• MacDonald HV, Johnson BT, Huedo-Medina TB, Livingston J, Forsyth KC, Kraemer WJ, et al. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: a meta-analysis. J Am Heart Assoc. 2016;5:e003231 This is a comprehensive meta-analysis attending high-quality standards that proposed dynamic resistance training as a viable stand-alone therapeutic exercise option.
Fagard RH, Cornelissen VA. Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil. 2007;14:12–7.
Tomeleri CM, Marcori AJ, Ribeiro AS, Gerage AM, Padilha CDS, Schiavoni D, et al. Chronic blood pressure reductions and increments in plasma nitric oxide bioavailability. Int J Sports Med. 2017;38:290–9.
Trevizani GA, Seixas MB, Benchimol-Barbosa PR, Vianna JM, Pinto da Silva L, Nadal J. Effect of resistance training on blood pressure and autonomic responses in treated hypertensives. J Strength Cond Res. 2018;32:1462–70.
Cononie C, Graves J, Pollock M, Phillips I, Sumners C, Hagberg J. Effect of exercise training on blood pressure in 70- to 79-yr-old men and women. Med Sci Sports Exerc. 1991;23:505–11.
Collier SR, Kanaley JA, Carhart R, Frechette V, Tobin MM, Bennett N, et al. Cardiac autonomic function and baroreflex changes following 4 weeks of resistance versus aerobic training in individuals with pre-hypertension. Acta Physiol. 2009;195:339–48.
Collier SR, Kanaley JA, Carhart R, Frechette V, Tobin MM, Hall AK, et al. Effect of 4 weeks of aerobic or resistance exercise training on arterial stiffness, blood flow and blood pressure in pre- and stage-1 hypertensives. J Hum Hypertens. 2008;22:678–86.
• Boeno FP, Ramis TR, Munhoz SV, Farinha JB, CEJ M, Leal-Menezes R, et al. Effect of aerobic and resistance exercise training on inflammation, endothelial function and ambulatory blood pressure in middle-aged hypertensive patients. J Hypertens. 2020;38:2501–9 This contemporary randomized controlled trial with hypertensive patients supported dynamic resistance training as a valuable non-pharmacological treatment for these patients by showing that its effects reducing ambulatory blood pressure and improving vascular function are similar to those observed with aerobic training in a head-to-head comparison.
Beck DT, Casey DP, Martin JS, Emerson BD, Braith R. Exercise training improves endothelial function in young prehypertensives. Exp Biol Med. 2013;238:433–41.
Beck DT, Martin JS, Casey DP, Braith RW. Exercise training improves endothelial function in resistance arteries of young prehypertensives. J Hum Hypertens. 2014;28:303–9.
Terra DF, Mota Rabelo M, Thomaz RH, Bezerra LMA, Lima RM, Ribeiro AG, et al. Redução da Pressão Arterial e do Duplo Produto de Repouso após Treinamento Resistido em Idosas Hipertensas. Arq Bras Cardiol. 2008;91:299–305.
• Pedralli M, Marschner R, Kollet D, Neto S, Eibel B, Tanaka H, et al. Different exercise training modalities produce similar endothelial function improvements in individuals with prehypertension or hypertension: a randomized clinical trial exercise, endothelium and blood pressure. Sci Rep. 2020;10:7628 This randomized clinical trial showed that dynamic resistance training promoted reductions on ambulatory systolic blood pressure (24-h period) and increases on flow-mediated dilation of similar magnitudes when compared with aerobic training. Besides that, an intervention that combined aerobic and dynamic resistance training did not show superior effects when compared with both exercise modes performed alone. Thus, its results reinforced the clinical value of dynamic resistance training in the management of pre-hypertension and hypertension.
Stensvold D, Tjønna A, Skaug E. Strength training versus aerobic interval training to modify risk factors of metabolic syndrome. J Appl Physiol. 2010;108:804–10.
Moraes M, Bacurau R. Chronic conventional resistance exercise reduces blood pressure in stage 1 hypertensive men. J Strength Cond Res 2012;0:1–8.
Coelho-Júnior HJ, Gonçalves I d O, NOS C, Cenedeze MA, Bacurau RF, Asano RY, et al. Non-periodized and daily undulating periodized resistance training on blood pressure of older women. Front Physiol. 2018;9:1–13.
De Sá CA, Catani D, Cardoso AM, Da Silva Grigoletto ME, Battiston FG, Corralo VS. Resistance training affects the hemodynamic parameters of hypertensive and normotensive women differently, and regardless of performance improvement. J Exerc Sci Fit. 2020;18:122–8.
Dantas FFO, Brasileiro-Santos M d S, RMF B, do Nascimento LS, LRC C, Ritti-Dias RM, et al. Effect of strength training on oxidative stress and the correlation of the same with forearm vasodilatation and blood pressure of hypertensive elderly women: a randomized clinical trial. PLoS One. 2016;11:1–19.
Oliveira-Dantas FF, do Brasileiro-Santos MS, Thomas SG, Silva AS, Silva DC, RAV B, et al. Short-term resistance training improves cardiac autonomic modulation and blood pressure in hypertensive older women. J Strength Cond Res. 2020;34:37–45.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo J Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52.
Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Neufrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95:1–51.
Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome - A new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80.
Anton MM, Cortez-Cooper MY, DeVan AE, Neidre DB, Cook JN, Tanaka H. Resistance training increases basal limb blood flow and vascular conductance in aging humans. J Appl Physiol. 2006;101:1351–5.
Kanegusuku H, Queiroz ACC, Silva VJD, De Mello MT, Ugrinowitsch C, Forjaz CLM. High-intensity progressive resistance training increases strength with no change in cardiovascular function and autonomic neural regulation in older adults. J Aging Phys Act. 2015;23:339–45.
Mohrman DE, Heller LJ. Cardiovascular physiology. 9th ed. Medical M-HE/, editor. 2018.
Ashor AW, Lara J, Siervo M, Celis-Morales C, Oggioni C, Jakovljevic DG, et al. Exercise modalities and endothelial function: a systematic review and dose–response meta-analysis of randomized controlled trials. Sports Med. 2015;45:279–96.
Sarelius I, Pohl U. Control of muscle blood flow during exercise: local factors and integrative mechanisms. Acta Physiol. 2010;199:349–65.
Asmussen E. Similarities and dissimilarities between static and dynamic exercise. Circ Res. 1981;48:I3–10.
Tinken TM, Thijssen DHJ, Hopkins N, Dawson EA, Cable NT, Green DJ. Shear stress mediates endothelial adaptations to exercise training in humans. Hypertension. 2010;55:312–8.
Green DJ, Hopman MTE, Padilla J, Laughlin MH, Thijssen DHJ. Vascular adaptation to exercise in humans: role of hemodynamic stimuli. Physiol Rev. 2017;97:495–528.
Spence AL, Carter HH, Naylor LH, Green DJ. A prospective randomized longitudinal study involving 6 months of endurance or resistance exercise. Conduit artery adaptation in humans. J Physiol. 2013;591:1265–75.
Carter JR, Ray CA, Downs EM, Cooke WH. Strength training reduces arterial blood pressure but not sympathetic neural activity in young normotensive subjects. J Appl Physiol. 2003;94:2212–6.
Hanssen H, Boardman H, Deiseroth A, Moholdt T, Simonenko M, Kränkel N, et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: a consensus document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur J Prev Cardiol. 2021.
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation. 2004;109:613–9.
Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4:e002270.
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. J Am Med Assoc. 2003;290:199–206.
Skaug EA, Aspenes ST, Oldervoll L, Mørkedal B, Vatten L, Wisløff U, et al. Age and gender differences of endothelial function in 4739 healthy adults: the HUNT3 fitness study. Eur J Prev Cardiol. 2013;20:531–40.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Funding
This study was supported by the Brazilian National Council for Scientific and Technological Development (CNPQ, process 304436/2018-6), the São Paulo Research Foundation (FAPESP, process 2018/12390-1) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, process 0001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to Participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mechanisms of Hypertension and Target-Organ Damage
Rights and permissions
About this article
Cite this article
Fecchio, R.Y., Brito, L.C., Peçanha, T. et al. Potential Mechanisms Behind the Blood Pressure–Lowering Effect of Dynamic Resistance Training. Curr Hypertens Rep 23, 35 (2021). https://doi.org/10.1007/s11906-021-01154-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11906-021-01154-5