Abstract
Purpose of Review
Hypertension and antihypertensive drug utilization are remarkably prevalent in ESRD patients. Management of blood pressure elevation in this population is complicated by many factors, including a multidimensional etiology, challenges in obtaining accurate and appropriately timed blood pressure measurements, highly specific drug dosing requirements, and a paucity of outcomes-based evidence to guide management decisions. The purpose of this review is to summarize and apply knowledge from existing clinical trials to enhance safe and effective use of antihypertensive agents in dialysis patients.
Recent Findings
Two meta-analyses have established the benefit of antihypertensive therapy in ESRD. Data supporting the use of one antihypertensive class over another is less robust; however, beta-blockers have more clearly demonstrated improved cardiovascular outcomes in prospective randomized trials. Interdialytic home blood pressure monitoring has been demonstrated to be better associated with cardiovascular outcomes than clinic pre- or post-dialysis readings and should ideally be considered as a routine part of blood pressure management in this population.
Summary
As data from small trials provides limited guidance for the management of hypertension in ESRD, more research is needed to guide medication selection and utilization. Specifically, large prospective randomized trails comparing cardiovascular outcomes of various medication classes and differing blood pressure targets are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is highly prevalent in the dialysis population, affecting more than 80% of end-stage renal disease (ESRD) patients [1,2,3]. Utilization of antihypertensive agents for treatment of elevated blood pressure is equally common, with estimates of 70–90% of patients receiving antihypertensive treatment [1, 3]. Despite the fact that almost all dialysis patients suffer from hypertension, evidence from robust clinical trials designed to examine the risk and benefit of various management strategies is lacking.
Hypertension in the Dialysis Patient
Etiology of Hypertension and Importance of Dry Weight in the Dialysis Patient
Hypertension is one of the most common causes of chronic kidney disease, accounting for 30% of all cases [4]. Once ESRD develops, the dysfunction of the kidney contributes to further blood pressure dysregulation; therefore, hypertension serves as both a progression factor for kidney disease and a complication of the disease process. Traditional risk factors for hypertension are present in many dialysis patients who have had long-standing hypertension, including smoking, obesity, inactivity, dietary indiscretion, genetics, and others. In addition, renal-specific contributors to hypertension in ESRD are numerous and require special attention, as a successful approach to management of blood pressure elevation must take into account the underlying etiologies (see Fig. 1).
Specific pathophysiological explanations for hypertension in ESRD include increased activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS) [5,6,7]. Interestingly, the origin of sympathetic activation seems to be directly related to diseased kidneys, as bilateral nephrectomy and renal denervation have both demonstrated improved effects on blood pressure control in dialysis patients [8,9,10,11]. With regard to RAAS activation, it is well established that this system is a primary target in pre-dialysis CKD patients; however, it is important to acknowledge that activation of this system persists in ESRD and should continue to be considered as a target for intervention.
Outside of renal-specific etiologies, established secondary causes must be considered in ESRD patients with resistant hypertension. These include hyperaldosteronism, pheochromocytoma, thyroid diseases, sleep apnea, drug-induced hypertension, and others. With regard to drug-induced causes, although all medications known to increase blood pressure should be routinely considered (i.e., NSAIDs, SNRIs, stimulants, estrogens), erythropoiesis stimulating agents (ESAs) deserve extra attention given common use among dialysis patients. Various mechanisms have been proposed to explain the blood pressure elevating effects of ESAs including increased blood viscosity and heightened vasoconstriction [12•]. The effect is a dose-related property and also correlates with achievement of higher hemoglobin targets with use of ESAs [13, 14]. Finally, medication non-adherence is a significant consideration and a likely contributor to uncontrolled hypertension in ESRD patients. It is estimated that dialysis patients take, on average, 19 pills per day with non-adherence rates projected to be greater than 60% [15, 16].
Fluid and sodium balance is the cornerstone of blood pressure management in ESRD [12•, 17•]. With a decline in renal clearance, the ability to excrete fluid and sodium diminishes, leading to volume overload and resulting blood pressure elevation. A plan primarily targeting the achievement of optimal volume status is the first step in addressing hypertension in ESRD, as efficacy of alternative approaches is mitigated by the presence of volume overload and its insurmountable impact on blood pressure. The general approach to attain optimal fluid balance is sodium restriction paired with achievement of a patient’s optimal dry weight.
Dry weight is a term used to describe a patient’s post-dialysis weight, once maximal fluid has been removed by dialysis. Maximizing volume removal, thus lowering a patient’s dry weight, has been demonstrated to result in improved blood pressure control in clinical trials [18, 19]. There are many different approaches to attainment of dry weight including ultrafiltration, extended dialysis duration, and increased dialysis frequency. Isolated ultrafiltration offers the advantage of minimizing patient time and financial resources given that additional dialysis time is not required; however, more aggressive removal of fluid is associated with unpleasant side effects during dialysis, including hypotension, cramps, nausea, and vomiting, making the strategy less desirable and potentially intolerable for patients. Another key challenge in dry weight management is determination of an optimal weight goal. There are currently no standardized measures to accurately identify an appropriate target weight for a patient, and active research in the utilization of ultrasound and bio-impedance for this purpose is underway [20]. Until these, more innovative measures are validated, a trial-and-error approach of “probing” the weight (i.e., gradually pushing the dry weight lower with subsequent dialysis sessions) to the lowest tolerated weight is the most common approach in practice [21].
Sodium restriction is paramount in minimizing intradialytic weight gain which, in return, allows for better tolerance in achievement of optimal dry weight [22]. A sodium restriction of 1.5 g of sodium per day is recommended, [12•] a task that can be highly challenging for patients given the prevalence of high-sodium foods in the US diet. Patient education and continued monitoring of dietary adherence is critical to ensure optimization of these efforts. In addition to dietary restriction, sodium concentration of dialysate can also be modified. Dialysate solutions with high-sodium concentration may result in fewer side effects during dialysis treatment (e.g., hypotension, muscle cramps, nausea/vomiting); however, clinical trials have demonstrated increased interdialytic weight gain with high-sodium concentration solutions and have suggested benefit with minimizing sodium concentration based on individual patients’ pre-dialysis sodium levels [23, 24].
Measurement of Blood Pressure in the Dialysis Patient
In addition to the complex and multifaceted etiology of hypertension in patients with ESRD, accurate measurement of blood pressure in this population proves to be perhaps an even greater challenge. The routine shifts in volume status contribute to significant fluctuations in blood pressure, making it difficult to determine which blood pressure readings should be used to determine the patient’s true blood pressure and their level of control. Substantial fluid gain between dialysis sessions can lead to acutely elevated pre-dialysis blood pressure readings while rapid fluid loss throughout a dialysis session can lead to intradialytic and post-dialysis hypotension. Although frequent blood pressure measurement is necessary during dialysis for management of acute issues linked to volume homeostasis, evidence supports that home blood pressure measurement and ambulatory blood pressure monitoring provide a more accurate estimate of blood pressure which is more reliably correlated to cardiovascular outcomes compared to pre- or post-dialysis readings [25••, 26, 27].
Given the cost, patient discomfort, and overall burden associated with ambulatory blood pressure monitoring, a practical alternative in routine practice may be to request that a patient monitor blood pressure at home at specific intervals. For example, monitor twice-daily readings on non-dialysis days for 1 week every month. This allows for treatment decisions to be based on average blood pressure readings which include a large range of blood pressure data points. Home blood pressure monitoring frequency can be tailored to individual patients, with more frequent monitoring necessary in those apparently lacking optimal blood pressure controls.
Blood Pressure Targets in the Dialysis Patient
While blood pressure targets continue to be debated in the general public, even less conclusive evidence exists to guide blood pressure targets for patients with ESRD. Conflicting results are seen when pre- and post-dialysis blood pressure levels are correlated with cardiovascular outcomes. For example, a U-shaped curve has been demonstrated in clinical trials, showing worse outcomes in individuals with lowest and highest pre- or post-dialysis blood pressures [28]. In contrast, lower interdialytic blood pressures levels, measured by home or ambulatory blood pressure monitoring, have been consistently associated with improved cardiovascular endpoints [26, 27].
Although ACC/AHA, JNC 8, and KDIGO hypertension guidelines exclude ESRD patients in their recommendations and no current guidelines address management of hypertension in ESRD, a 2016 European consensus statement on the management of hypertension in ESRD suggests that an average BP > 135/85 mmHg, using measurements collected in the morning and in the evening over 6 non-dialysis days, can be used as a threshold to define hypertension in ESRD [12•].
Outcomes Supporting Use of Antihypertensive Agents in Dialysis Patients
Two meta-analyses have been performed examining the cardiovascular benefits of antihypertensive therapy in dialysis patients. The first included eight trials containing 1679 patients in total. Active treatment with blood pressure lowering medications was associated with reduced mean blood pressure (4.5 mmHg systolic and 2.3 mmHg diastolic decline) and a reduced risk of cardiovascular events (RR 0.7, 95% CI 0.55–0.92), all-cause mortality (RR 0.8, 95% CI 0.66–0.96), and cardiovascular mortality (RR 0.71, 95% CI 0.5–0.99) [29••]. A second meta-analysis, including 5 of the 8 studies in the aforementioned analysis, evaluated data for 1202 patients. Similar results were found, including an improved hazard ratio for cardiovascular events (HR 0.69, 95% CI 0.56–0.84) [30••]. Notably, when patients receiving antihypertensive therapy were evaluated according to hypertensive status, hypertensive vs. normotensive, the cardiovascular benefit was retained in the hypertensive group but diminished in the normotensive group (HR 0.49, 95% CI 0.35–0.67 and 0.86, 95% CI 0.67–1.12 respectively) [30••].
Limitations of both meta-analyses include the small number and size of included trials. Another important consideration is the significant variation in design of each trial. Some trials were designed to evaluate effectiveness of blood pressure lowering with specific drug therapy; whereas, other trials were designed to examine cardiovascular effects of specific antihypertensive classes in patients at high CV risk, with or without hypertension. Furthermore, a variety of different medications were utilized in the individual trials. For these reasons, it is not possible to draw conclusions about preferred classes of antihypertensive agents in ESRD patients from this data.
Medication classes with well-established evidence of benefit in the general population do not always produce benefit in an ESRD population. A prime example of this is statin therapy, which has not been demonstrated to provide cardiovascular benefit in an ESRD population [31,32,33]. For this reason, extrapolating information from trials performed in the general population to an ESRD population must be done with caution. From this standpoint, the information generated form these meta-analysis supporting a basic role of antihypertensive therapy is the ESRD population is pivotal in guiding pharmacotherapy management for this population.
Use of Antihypertensive Agents in the Dialysis Patient
Compared with the general population and the non-dialysis CKD population, determining an optimal antihypertensive medication regimen for a patient on dialysis requires an entirely new approach for medication class selection, individual agent choice, drug dosing, and timing of drug administration. As noted previously, classes of antihypertensive medications with well-established benefits demonstrated in clinical trials in the general population might not confer the same benefits in the ESRD population. Furthermore, renal clearance and dialyzability of individual medications must be carefully considered when selecting a specific drug regimen.
Selection of antihypertensive therapy in the general population is based on cardiovascular benefit of individual classes, as demonstrated in large-scale clinical trials. In the ESRD population, this data does not exist; therefore, treatment decisions are less clear. A recent survey among 160 practicing US nephrologists designed to examine prescribing patterns revealed that the largest percentage of respondents (68%) ranked calcium channel blockers (specifically nifedipine and amlodipine) as most effective in the treatment of hypertension in dialysis patients, followed by beta-blockers (35%), ACEIs (32%), ARBs (29%), and diuretics (25%) [34]. The diversity of practice preference highlighted by the survey responses stems from the lack of evidence-based guidance that exists for pharmacologic management of this condition. Furthermore, it must be noted that, given the numerous challenges associated with maintaining adequate blood pressure, many patients require treatment with multiple antihypertensive agents.
A report from a KDIGO clinical controversy conference, concludes that current evidence is not available to support use of one class of antihypertensive agents over another in ESRD [17•]. In contrast, within the 2016 European consensus document, it is specifically recommended that beta-blockers should be considered as first-line therapy, followed by dihydropyridine calcium channel blockers as second-line agents [12•]. Both organizations highlight the need for clinical trials examining efficacy of antihypertensive therapy in reducing cardiovascular disease outcomes in the dialysis population.
With regard to drug dosing in dialysis, two primary factors must be considered: the extent to which the drug is renally eliminated and the significance of the removal of the drug via dialysis. If a medication is not eliminated by the kidneys (e.g., primarily undergoes hepatic metabolism) and is not removed via dialysis, no drug-dosing modifications need to be considered. In contrast, if a drug is removed by the kidney, dialysis, or both, dosing adjustments will likely be necessary. For example, if a drug is almost entirely renally eliminated and does undergo appreciable dialysis removal, consideration may be given to non-traditional dosing strategies, such as thrice weekly observed post-dialysis dosing. This innovative dosing strategy is based on the idea that a renally eliminated drug will maintain activity throughout the entire interdialytic time period and can then be cleared during the dialysis session and re-dosed for the next interim period. Table 1 summarizes guidance in applying these general properties to specific antihypertensive agents.
Although many guidance documents related to drug dosing in dialysis exist to aid in proper dosing, it is critical to have a basic understanding of drug removal processes to fully appreciate the variability with which a medication may be removed via dialysis, even at the same dose in the same patient. Dialyzability of a medication is indirectly related to the medication’s volume of distribution, protein binding, and molecular weight, meaning that as these drug characteristics increase, the dialyzability of the medication decreases and vice versa. Table 2 provides an overview of these drug-specific pharmacokinetic medication properties for commonly used antihypertensive agents that may be encountered in the dialysis patient.
Beta-Blockers
Although not recognized as first-line therapy for management of hypertension in the general population, beta-blockers are commonly used in the management of hypertension in ESRD [17•]. Mechanistically, this class is beneficial in mitigating the increased sympathetic activity seen in ESRD. Furthermore, the established benefits of beta-blockers in the general population with established cardiovascular disease is a major consideration for patients with ESRD given substantially higher rates of cardiovascular disease and cardiovascular-related death in this population. For these reasons, clinical trials have been conducted to evaluate the effectiveness of beta-blockers in dialysis populations to a greater extent than other antihypertensive classes. In one trial of 114 dialysis patients with cardiomyopathy, patients were randomized to receive carvedilol or placebo. After 2 years, 51.7% in the carvedilol group died compared to 73.2% in the placebo group (p < 0.1) [39••]. In a second trial, the HAPDL trial, atenolol was compared to lisinopril in 200 patients with hypertension [40]. Although the primary outcome of LV mass index improved the same extent in both groups, the trial was terminated early due to the beneficial effects seen with atenolol with regard to prevention of serious cardiovascular events, including MI, stroke, heart failure hospitalizations, and cardiovascular death. Notably, there was no significant difference in blood pressure control between the two agents; however, atenolol was associated with numerically lower blood pressure levels as well. Although small, these trials suggest benefit with use of beta-blockers in patients with ESRD making this class a primary consideration for first-line therapy.
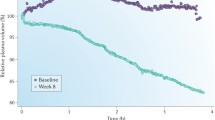
In terms of usability, beta-blockers vary widely with regard to their renal elimination and dialyzability. Atenolol, for example, is highly renally eliminated and highly dialyzable. These properties have been exploited in non-traditional dosing approaches involving supervised administration thrice weekly, post-dialysis. In a small trial examining 3 weeks of this atenolol dosing strategy among 8 dialysis patients, mean 44-h ambulatory systolic blood pressure levels fell from 144 to 127 mmHg [41]. Of note, the previously mentioned HAPDL trial comparing lisinopril to atenolol used this dosing strategy for both agents [40]. The advantage of in-clinic dosing offered by this approach cannot be overstated given the high pill burden and complex drug regimens that are common among ESRD patients. On the other hand, small trials have supported the use of non-dialyzable beta-blockers, citing the benefit conferred from maintenance of intradialysis beta-blocker effects [42]. Decisions regarding selection of a specific beta-blocker should be individualized, with thrice weekly dosing preferred for patients challenged by medication adherence. Table 2 includes specific pharmacokinetic information for each beta-blocker, which should be considered for selection and dosing of each agent.
Calcium Channel Blockers
In the general population, calcium channel blockers are effective agents commonly utilized in the treatment of hypertension, angina, and supraventricular tachycardia. These agents are divided into two subclasses based on primary site of action, with dihydropyridines showing higher selectivity for vascular smooth muscle and non-dihydropyridines acting primarily in the myocardium. Although both subclasses demonstrate similar efficacy in blood pressure lowering, the dihydropyridines are typically preferred over non-dihydropyridines in the dialysis population and are overall considered second-line agents for the treatment of hypertension. The preference for dihydropyridines is based on a larger body of data assessing the effectiveness in patients on dialysis in comparison to the non-dihydropyridines [17•]. In one trial of 251 patients on hemodialysis, amlodipine dosed at 10 mg/day was associated with a non-significant improvement in survival and a 47% reduction in the composite secondary endpoint of all-cause mortality or cardiovascular event when compared with placebo [43••].
Calcium channel blockers have favorable pharmacokinetic properties for use in the dialysis population. Most of these agents primarily undergo hepatic elimination and none of them are dialyzable. Patients receiving dihydropyridine calcium channel blockers should be closely monitored as fluid retention and edema are common adverse effects associated with these medications. Most of these agents only require once-daily administration and have broad dosing ranges. Concomitant administration of non-dihydropyridine calcium channel blockers and beta-blockers should be avoided due to increased risk of bradycardia and electrical conduction defects.
Renin Angiotensin Aldosterone System Antagonists
RAAS inhibition with use of angiotensin II converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) is inarguably first-line therapy in patients with hypertension and CKD not receiving dialysis. Furthermore, these agents are recognized as first-line therapy for the general population with hypertension, coronary artery disease, or heart failure. As increased RAAS activity is a documented contributor to hypertension in ESRD, it is logical to also employ these medications in dialysis patients with blood pressure elevation. While small trials have documented improved cardiovascular outcomes with use of ACEI/ARB therapy compared to placebo [44,45,46,47], there is currently no evidence to support an advantage in clinical outcomes with this class of antihypertensive agents compared to other classes when used in an ESRD population [40].
When using ACEIs or ARBs in dialysis patients, it is important to note the significant variability in renal clearance and dialyzability of each individual agent. ARBs, in general, are metabolized by the liver and do not undergo appreciable dialysis removal. In contrast, certain ACEIs, lisinopril for example, are predominantly eliminated by the kidneys and do undergo substantial dialysis removal making dosing more complex. As mentioned previously, supervised thrice weekly dosing of lisinopril has been evaluated in clinical trials and has been shown to result in significant blood pressure reduction [40]. Refer to Table 2 for additional detail regarding specific drug properties of each individual agent.
While ACEIs and ARBs are overall well tolerated, hyperkalemia is an important consideration. Despite potassium removal with dialysis, hyperkalemia is a chronic issue for some patients and may limit utilization of this medication class. It should be noted that patiromer, a potassium binder studied for daily use in non-dialysis CKD patients with hyperkalemia taking RAAS antagonists, has also been studied in a small number of dialysis patients and has demonstrated safe and effective potassium and phosphorus lowering [48]. Addition of daily patiromer therapy may be considered in ESRD patients with hyperkalemia due to ACEI/ARB therapy who may otherwise benefit; however, widespread use of patiromer is limited by high cost and the requirement to separate administration from other medications by 4 h to avoid medication binding and consequent diminished effects.
Aldosterone Antagonists
Aldosterone antagonists, spironolactone and eplerenone, have established efficacy in the management of heart failure in the general population and are widely accepted as add-on agents to ACEI/ARB therapy in the treatment of proteinuria in CKD. In ESRD, the activation of the RAAS system can be addressed with use of ACEI/ARB therapy; however, it has been demonstrated that increased levels of aldosterone persist in a phenomenon referred to as “aldosterone breakthrough” [49]. Furthermore, the increased prevalence of left ventricular hypertrophy and overall of burden of cardiovascular disease among the ESRD population make the aldosterone antagonist class attractive given the known morbidity and mortality benefits conferred with use of these medications in patients with heart failure. Small trials examining the efficacy and safety of aldosterone antagonists have been performed in ESRD patients and have shown benefit in surrogate cardiovascular outcomes, including ejection fraction improvements and decrease in LVH prevalence [50,51,52]. Hyperkalemia is the primary safety concern. Although more prevalent in these small trials, the extent of hyperkalemia was determined to be manageable and did not require drug discontinuation.
It should be noted that both spironolactone and eplerenone undergo significant renal elimination and are not removed by dialysis. For this reason, drug accumulation and resulting hyperkalemia is a significant concern for patients with impaired renal clearance and has led to the recommendation against use of these agents in patients with CKD and ESRD. Despite this concern, use of these agents has been explored in ESRD populations, as described previously, given the potential gains that may exist which could outweigh these potential risks. Although at highest risk of drug accumulation among CKD patients, ESRD patients are more closely monitored than non-dialysis CKD patients, with thrice-weekly dialysis clinic visit. This allows for routine monitoring of potassium, making risks associated with hyperkalemia potentially less concerning for dialysis patients compared to the non-dialysis CKD population.
A notably large prospective trial, ALCHEMIST, is underway and projected to be complete in 2024 [53]. This trial will evaluate the effectiveness of spironolactone compared to placebo in over 800 ESRD patients. The primary outcome is time to first incident of non-fatal MI, acute coronary syndrome, hospitalization for heart failure or non-fatal stroke, or cardiovascular (CV) death after approximately 2 years of treatment. The level of evidence in establishing safety/efficacy of antihypertensive therapy in ESRD patients that will be produced from this trial is highly anticipated and is a good step in meeting the evidence needs that have been highlighted by several organizations [12•, 17•].
Diuretics
It is commonly thought that diuretic therapy is ineffective in ESRD due to lack of urine production as a result of renal function decline. In ESRD patients with residual renal function, making at least 100 ml of urine per day, loop diuretics may be efficacious in improving blood pressure and overall health outcomes for dialysis patients [54]. It is suggested that diuretic therapy may assist in decreasing fluid accumulation over the interdialytic period which allows for less aggressive fluid removal during dialysis, fewer intradialytic hypotensive episodes, and more success at achieving optimal dry weight [12•, 55]. Although maximizing doses can lead to maximized efficacy, serious side effects, namely ototoxicity, are also dose related. For this reason, dosing should not exceed usual limits.
Other Antihypertensive Agents
Other classes of antihypertensive agents include alpha-blockers, alpha agonists, and vasodilators. Alpha-blockers may be especially useful in patients with residual renal function and comorbid benign prostate hypertrophy given known benefits in enhancement of urinary flow. Clonidine offers the advantage of weekly transdermal patch administration, a particularly attractive option for certain ESRD patients with very high pill burden. Given its centrally acting alpha agonist activity, however, sedation and dry mouth limit widespread use due to intolerance, even when administered transdermally. Finally, vasodilators are useful adjuncts for blood pressure lowering due optimal tolerability. Potential drawbacks include multiple daily dosing and peripheral edema.
Conclusion
In the absence of consensus guidelines, practitioners involved in optimizing the use of antihypertensive agents in ESRD patients are required to combine knowledge generated from small trials with fundamental knowledge of hypertension etiology in ESRD and basic concepts associated with drug dosing in dialysis. Involvement of the entire multi-disciplinary dialysis team and engagement of the patient in decision-making are critical components for successful management of blood pressure. The need for future research in this area is a great, given the substantial cardiovascular-related morbidity and mortality in this high-risk population.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Agarwal R. Epidemiology of interdialytic ambulatory hypertension and the role of volume excess. Am J Nephrol. 2011;34:381–90.
Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003;115:291–7.
Sarafidis PA, Mallamaci F, Loutradis C, Ekart R, Torino C, Karpetas A, et al. Prevalence and control of hypertension by 48-h ambulatory blood pressure monitoring in haemodialysis patients: a study by the European Cardiovascular and Renal Medicine (EURECA-m) working group of the ERA-EDTA. Nephrol Dial Transplant. 2018. https://doi.org/10.1093/ndt/gfy147.
Centers for Disease Control and Prevention. National Chronic Kidney Disease Fact Sheet, 2017. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2017.
Nishimura M, Tokoro T, Nishida M, Hashimoto T, Kobayashi H, Yamazaki S, et al. Sympathetic overactivity and sudden cardiac death among hemodialysis patients with left ventricular hypertrophy. Int J Cardiol. 2010;142:80–6.
Tong YQ, Hou HM. Alteration of heart rate variability parameters in nondiabetic hemodialysis patients. Am J Nephrol. 2007;27:63–9.
Kornerup HJ, Schmitz O, Danielsen H, Pedersen EB, Giese J. Significance of the renin-angiotensin system for blood pressure regulation in end-stage renal disease. Contrib Nephrol. 1984;41:123–7.
Converse RL Jr, Jacobsen TN, Toto RD, Jost CM, Cosentino F, Fouad- Tarazi F, et al. Sympathetic overactivity in patients with chronic renal failure. N Engl J Med. 1992;327:1912–8.
Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters K, et al. Sympathetic nerve activity in end-stage renal disease. Circulation. 2002;106:1974–9.
Ott C, Schmid A, Ditting T, Sobotka PA, Veelken R, Uder M, et al. Renal denervation in a hypertensive patient with end-stage renal disease and small arteries: a direction for future research. J Clin Hypertens (Greenwich). 2012;14:799–801.
Papademetriou V, Doumas M, Anyfanti P, Faselis C, Kokkinos P, Tsioufis C. Renal nerve ablation for hypertensive patients with chronic kidney disease. Curr Vasc Pharmacol. 2014;12:47–54.
• Sarafidis P, Persub A, Agarwal R, Burnierf M, de Leeuwg P, Ferroi C, et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association ^ European Dialysis and Transplant Association (ERA-EDTA) and the hypertension and the kidney working group of the European Society of Hypertension (ESH). J Hypertens. 2017;35:657–76 This position paper is a comprehensive review of management of hypertension in dialysis, including etiology, blood pressure measurement, suggested blood pressure targets, utilization of antihypertensive agents, recommended first and second-line therapies, and opportunities for future research.
Eggena P, Willsey P, Jamgotchian N, Truckenbrod L, Hu MS, Barrett JD, et al. Influence of recombinant human erythropoietin on blood pressure and tissue renin-angiotensin systems. Am J Phys. 1991;261:E642–6.
Koulouridis I, Alfayez M, Trikalinos TA, Balk EM, Jaber BL. Dose of erythropoiesis-stimulating agents and adverse outcomes in CKD: a metaregression analysis. Am J Kidney Dis. 2013;61:44–56.
Schmid H, Hartmann B, Schiffl H. Adherence to prescribed oral medication in adult patients undergoing chronic hemodialysis: a critical review of the literature. Eur J Med Res. 2009;14:185–90.
Chiu Y, Teitelbaum I, Misra M, de Leon E, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol. 2009;4:1089–96.
• Levin NW, Kotanko P, Eckardt K, Kasiske BL, Chazot C, Cheung A, et al. Blood pressure in chronic kidney disease stage 5D – report from a kidney disease: improving global outcomes controversies conference. Kidney Int. 2010;77(4):273–84. https://doi.org/10.1038/ki.2009.469 This position paper is a comprehensive review of management of hypertension in dialysis, including etiology, blood pressure measurement, utilization of antihypertensive agents, and opportunities for future research.
Agarwal R, Alborzi P, Satyan S, Light RP. Dry-weight reduction in hypertensive hemodialysis patients (DRIP): a randomized, controlled trial. Hypertension. 2009;53:500–7.
Ozkahya M, Toz H, Qzerkan F, Duman S, Ok E, Basci A, et al. Impact of volume control on left ventricular hypertrophy in dialysis patients. J Nephrol. 2002;15:655–60.
Torino C, Gargani L, Sicari R, Letachowicz K, Ekart R, Fliser D, et al. The agreement between auscultation and lung ultrasound in hemodialysis patients: the LUST study. Clin J Am Soc Nephrol. 2016;11:2005–11.
Agarwal R, Bouldin JM, Light RP, Garg A. Probing dry-weight improves left ventricular mass index. Am J Nephrol. 2011;33:373–80.
Kayikcioglu M, Tumuklu M, Ozkahya M, Ozdogan O, Asci G, Duman S, et al. The benefit of salt restriction in the treatment of end-stage renal disease by haemodialysis. Nephrol Dial Transplant. 2009;24:956–62.
de Paula FM, Peixoto AJ, Pinto LV, Dorigo D, Patricio PJ, Santos SF. Clinical consequences of an individualized dialysate sodium prescrip- tion in hemodialysis patients. Kidney Int. 2004;66:1232–8.
Munoz MJ, Bayes LY, Sun S, Doss S, Schiller B. Effect of lowering dialysate sodium concentration on interdialytic weight gain and blood pressure in patients undergoing thrice-weekly in-center nocturnal hemodialysis: a quality improvement study. Am J Kidney Dis. 2011;58:956–63.
•• Alborzi P, Patel N, Agarwal R. Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol. 2007;2:1228–34 This prospective trial helped to establish the utility of home blood pressure measurement as an accurate means for monitoring blood pressure in ESRD based on correlation with cardiovascular outcomes.
Zoccali C, Mallamaci F, Tripepi G, Benedetto FA, Cottini E, Giacone G, et al. Prediction of left ventricular geometry by clinic, pre-dialysis and 24-h ambulatory BP monitoring in hemodialysis patients: CREED investigators. J Hypertens. 1999;17:1751–8.
Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and postdialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol. 2006;1:389–98.
Zager PG, Nikolic J, Brown RH, Campbell MA, Hunt WC, Peterson D, et al. ‘U’ curve association of blood pressure and mortality in hemodialysis patients. Medical Directors of Dialysis Clinic, Inc. Kidney Int. 1998;54:561–9.
•• Heerspink HJ, Ninomiya T, Zoungas S, de Zeeuw D, Grobbee DE, Jardine MJ, et al. Effect of lowering blood pressure on cardiovascular events and mortality in patients on dialysis: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2009;373:1009–15 This meta-analysis, including nine clinical trials, was the first of its kind published to establish the cardiovascular benefit of antihypertensive agents in ESRD patients.
•• Agarwal R, Sinha AD. Cardiovascular protection with antihypertensive drugs in dialysis patients: systematic review and meta-analysis. Hypertension. 2009;53:860–6 This meta-analysis, including five clinical trials, helped to confirm the cardiovascular benefit of antihypertensive agents in ESRD patients and highlighted potentially greater benefit in dialysis patients with hypertension specifically.
Wanner C, Krane V, Marz W. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;53:238–48.
Fellstrom BC, Jardine AG, Schmieder RE. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360:1395–407.
Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377:2181–92.
Mallappallil M, Fishbane S, Wanchoo R, Lerma E, Roche-Recinos A, Salifu M. Practice patterns in transitioning patients from chronic kidney disease to dialysis: a survey of United States nephrologists. BMC Nephrol 2018:19. https://doi.org/10.1186/s12882-018-0943-0.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71(6):1269–324. https://doi.org/10.1161/hyp.0000000000000066.
Aronoff GR. Drug prescribing in renal failure: dosing guidelines for adults and children. 5th ed. Philadelphia: American College of Physicians; 2009.
Mallamaci F, Zoccali C. Hypertension. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2015.
Agarwal R, Georgianos PI. Pharmacotherapy of hypertension in chronic dialysis patients. Clin J Am Soc Nephrol. 2016;11:2062–75. https://doi.org/10.2215/CJN.00870116.
•• Cice G, Ferrara L, D’Andrea A, D’Isa S, Di Benedetto A, Cittadini A, et al. Carvedilol increases two-year survival in dialysis patients with dilated cardiomyopathy: a prospective, placebo controlled trial. J Am Coll Cardiol. 2003;41:1438–44 This is one of very few prospective, randomized controlled, double blind studies examining antihypertensive agents in ESRD to find clinically and statistically significant benefit with treatment.
Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transplant. 2014;29:672–81.
Agarwal R. Supervised atenolol therapy in the management of hemodialysis hypertension. Kidney Int. 1999;55:1528–35.
Weir MA, Dixon SN, Fleet JL, Roberts MA, Hackam DG, Oliver MJ, et al. Beta-blocker dialyzability and mortality in older patients receiving hemodialysis. J Am Soc Nephrol. 2015;26:987–96.
•• Tepel M, Hopfenmueller W, Scholze A, Maier A, Zidek W. Effect of amlodipine on cardiovascular events in hypertensive haemodialysis patients. Nephrol Dial Transplant. 2008;23:3605–12 This is one of very few prospective, randomized controlled, double blind studies examining antihypertensive agents in ESRD; clinically and statistically significant benefit with treatment was found.
Takahashi A, Takase H, Toriyama T, Sugiura T, Kurita Y, Ueda R, et al. Candesartan, an angiotensin II type-1 receptor blocker, reduces cardiovascular events in patients on chronic haemodialysis – a randomized study. Nephrol Dial Transplant. 2006;21:2507–12.
Leidig M, Bambauer R, Kirchertz EJ, Szabã T, Handrock R, Leinung D, et al. Efficacy, safety and tolerability of valsartan 80 mg compared to irbesartan 150 mg in hypertensive patients on long-term hemodialysis (VALID study). Clin Nephrol. 2008;69:425–32.
Suzuki H, Kanno Y, Sugahara S, Ikeda N, Shoda J, Takenaka T, et al. Effect of angiotensin receptor blockers on cardiovascular events in patients undergoing hemodialysis: an open-label randomized controlled trial. Am J Kidney Dis. 2008;52:501–6.
Agarwal R, Lewis R, Davis JL, Becker B. Lisinopril therapy for hemodialysis hypertension: hemodynamic and endocrine responses. Am J Kidney Dis. 2001;38:1245–50.
Bushinsky DA, Rossignol P, Spiegel DM, Benton WW, Yuan J, Block GA, et al. Patiromer decreases serum potassium and phosphate levels in patients on hemodialysis. Am J Nephrol. 2016;44:404–10.
Bomback AS. Mineralocorticoid receptor antagonists in end-stage renal disease: efficacy and safety. Blood Purif. 2016;41:166–70.
Matsumoto Y, Mori Y, Kageyama S, Arihara K, Sugiyama T, Ohmura H, et al. Spironolactone reduces cardiovascular and cerebrovascular morbidity and mortality in hemodialysis patients. J Am Coll Cardiol. 2014;63:528–36.
Lin C, Zhang Q, Zhang H, Lin A. Long-term effects of low-dose spironolactone on chronic dialysis patients: a randomized placebo- controlled study. J Clin Hypertens (Greenwich). 2016;18:121–8.
Walsh M, Manns B, Garg AX, Bueti J, Rabbat C, Smyth A, et al. The safety of eplerenone in hemodialysis patients: a noninferiority randomized controlled trial. Clin J Am Soc Nephrol. 2015;10:1602–8.
Brest UH. ALdosterone Antagonist Chronic HEModialysis Interventional Survival Trial (ALCHEMIST). ClinicalTrials.gov: Bethesda (MD): National Library of Medicine (US). 2018. https://clinicaltrials.gov/ct2/show/NCT01848639. Accessed 7 Nov 2018.
Medcalf JF, Harris K, Walls J. Role of diuretics in the preservation of residual renal function in patients on continuous ambulatory peritoneal dialysis. Kidney Int. 2001;59:1128–33.
Ahmed S, Guffey D, Minard C, Workeneh B. Efficacy of loop diuretics in the management of undocumented patients with end-stage renal disease. Am J Emerg Med. 2016;34:1552–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Antihypertensive Agents: Mechanisms of Drug Action
Rights and permissions
About this article
Cite this article
Fravel, M.A., Bald, E. & Fraer, M. Antihypertensive Agents in the Dialysis Patient. Curr Hypertens Rep 21, 5 (2019). https://doi.org/10.1007/s11906-019-0909-z
Published:
DOI: https://doi.org/10.1007/s11906-019-0909-z