Abstract
An adequate control of blood pressure is essential to reduce the risk of target organ damages and cardiovascular events in patients with hypertension. Yet, it is well recognized that a substantial proportion of treated patients remain hypertensive despite treatment. Several reasons have been evoked to explain why so many patients are not adequately controlled. Among them, medical inertia, a poor long-term adherence, and the need to prescribe several antihypertensive drugs to reach the target blood pressure have been identified as major limitations to the success of antihypertensive therapy. In this context, the use of single-pill combinations (SPC) containing two or three drugs in one pill has an important role in reducing the impact of some of these issues. Indeed, the use of SPC enables to reduce the pill burden and to improve the treatment efficacy without increasing the incidence of side effects. However, besides their major advantages, SPC have also some limitations such as a possible lack of flexibility or a higher cost. The purpose of this review is to discuss the place of SPC in the actual management of hypertension. The active development of new single-pill combinations in last years can be considered as a significant improvement in the physicians’ capacity to treat hypertension effectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of two pharmacological agents in a single pill has been available for the treatment of hypertension since the mid-1960s. Today, numerous single-pill combinations (SPC) exist and are used not only to treat hypertension [1, 2] but also to manage several other chronic diseases characterized by a high morbidity and mortality risk and an elevated pill burden such as, for example, type 2 diabetes [3], chronic obstructive lung disease [4], or HIV [5].
In the management of hypertension, it took some time until the use of single-pill combinations got really accepted but today, theses combinations are frequently prescribed and the authorities of many countries have agreed to take in charge their reimbursement. Most national and international guidelines recommend the prescription of SPC as one of the main step in the therapeutic approach of elevated arterial blood pressure (BP) [6]. For example, in the 2013 publication of the joint European Society of Hypertension (ESH)/European Society of Cardiology (ESC) guidelines for the management of arterial hypertension, SPC can be used as first as well as second-line therapies to achieve the recommended target BP of <140/90 mmHg [6]. In recent years, fixed-dose combinations have gained a major role in hypertension with the recognition that most patients need more than two antihypertensive agents to have their BP under control in clinical trials as well as in clinical practice [7–10]. Moreover, as multiple therapies have been associated with a rather low long-term persistence, particularly in the primary and secondary prevention of cardiovascular diseases [11••], an increased use of SPC has been identified as one efficient means of reducing the overall pill burden which in turn should improve the long-term BP control and reduce the incidence of cardiovascular complications in treated hypertensive patients. This latter point is particularly important as it is obvious that despite all efforts, the percentage of patients treated for hypertension who have their BP on target remains low, generally below 50 %. Consequently, the cardiovascular risk of these patients is persistently high despite therapy [12–14].
The purpose of the present article is to review the reasons which have lead to the development of SPC, to discuss the various SPC available on the market today and to evaluate the advantages and limitations of SPCs as well as their impact in the actual management of hypertension.
Reasons for Developing Single-Pill Combinations in Hypertension
Although a reserpine-based combination was available in 1966 already, the true development of single-pill combinations (SPC) started in the early 1990s as a consequence of several clinical and pharmacological observations [7]. In these years, the therapeutic strategy proposed to treat hypertensive patients was based essentially on the so-called stepped care therapy. According to this strategy, the treatment was started with a first drug and after reaching the maximal dose of this drug, a second antihypertensive agent was added, followed by a third or a fourth one if necessary until a satisfactory BP control was obtained. It became, however, rapidly evident that although a single drug would have been the preferred option to treat hypertensive patients, a monotherapy was at best effective in correcting BP in a limited percentage of patients (between 40 and 50 %) with stage I or II hypertension and most patient ended up taking 2 to 4 drugs per day. The limited ability of monotherapies to control BP was elegantly demonstrated by the study of Materson et al. who assessed how frequently various drugs given in monotherapy were controlling BP [15]. Recent surveys conducted in a large set of patients followed in clinical practice actually confirmed the results of the initial observation [16•, 17, 18]. In addition, it has been well recognized that the pharmacology of all antihypertensive drugs, except loop diuretics, is characterized by a relatively flat dose–response curve. Hence, there is little if any additional antihypertensive benefit of increasing the dose of these drugs above the maximal recommended doses [19]. Indeed, in a large meta-analysis, Wald et al. have shown that combining antihypertensive drugs provides a 5-fold greater additional decrease in BP than doubling the dose of any of the antihypertensive monotherapies [19]. In addition, whereas increasing the drug dose had little impact on the antihypertensive efficacy, it had a significant influence on the occurrence of side effects which increased dose-dependently with most drug classes except blockers of the renin-angiotensin system which have dose-independent side effects. These observations resulted in the conclusion that, when BP is insufficiently controlled with a monotherapy, it is preferable and more effective to use a combination of drugs than to pursue with a higher dose of the same drug. This resulted in a major change in management paradigm favoring an earlier use of drug combinations and, in particular, SPC at low dose rather than free-drug combinations. One alternative to maintain as many patients as possible on a single antihypertensive agent would have been to apply sequential monotherapy, a therapeutic strategy implying to test several monotherapies in the same patient in order to find the drug that provides the best control of BP and the opportunity to stay on a monotherapy [7]. However, this approach did not generate a big enthusiasm, as it was time-consuming, probably less effective than starting with a fixed low-dose combination [17] and in any case limited to patients with mild hypertension and a low cardiovascular risk.
Another good reason to use combinations was the fact that hypertension has a multifactorial pathophysiology. Therefore, a therapy acting on several different mechanisms should have a greater efficacy in controlling BP than any monotherapy focusing on a single BP control pathway. With the use of combination of drugs, a greater percentage of patients could be brought to target more quickly. This hypothesis has now been demonstrated very clearly in surveys or meta-analyses [16•, 17, 19].
At last, combining therapeutic strategies might offer some advantages on the development of side effects. This was actually the principle of the initial concept of fixed low-dose combinations according to which combining a low dose of two therapeutic agents has a greater antihypertensive efficacy but induces fewer side effects than a high-dose monotherapy. With the greatly improved tolerability profile of newer antihypertensive drugs such as angiotensin receptor blockers (ARB), the concept of low-dose combinations was progressively abandoned in favor of high-dose SPCs. In this respect, when combining therapeutic strategies, each component has the potential of neutralizing counter-regulatory mechanisms and thereby of reducing the development of potential side effects while the blood pressure-lowering effect of each component of the combination is enhanced. One good example of such a synergism is the association of a blocker of the renin-angiotensin system (RAS) and a thiazide diuretic. The thiazide-induced natriuresis potentiates the antihypertensive efficacy of the RAS blocker by stimulating renin, whereas the RAS blocker limits the kaliuresis induced by the thiazide diuretic and therefore limits the incidence of hypokalemia [20]. Another example is the reduction of the incidence of peripheral edema with calcium channel blockers when these are associated with a RAS blocker [21].
Single-Pill Combinations in Hypertension: a Large Choice
In todays guidelines, the pharmacological treatment of hypertension is based essentially on three drug classes that can be prescribed as first-line therapy, i.e., diuretics, blockers of the RAS (angiotensin converting enzyme (ACE) inhibitors and ARBs) and calcium channel blockers (CCB) [6, 22, 23]. Other classes, such as beta-blockers, alpha-blockers, aldosterone antagonists, and vasodilators, are recommended only in certain specific clinical conditions or as backup lines of treatment. As shown in Table 1, a large number of various SPCs are available today. Indeed, SPCs include combinations of diuretics, associations of RAS blockers and diuretics, RAS blockers and CCB, RAS blockers and beta-blockers, beta-blockers and CCB, and beta-blockers and diuretics. Moreover, several SPCs containing a triple combination of a diuretic, a CCB and a blocker of the renin-angiotensin system have been launched for patients insufficiently controlled with a dual therapy. As discussed earlier, many of these SPCs containing two antihypertensive agents can be prescribed as first-line therapy when the cardiovascular risk is high and the likelihood to normalize BP with a single drug therapy is low [6].
Each of these SPCs has a good rationale to justify its development and use in clinical practice. Thus, the combination of a potassium-sparing diuretic (spironolactone, amiloride, or triamterene) with a thiazide diuretic enables to limit the potassium losses and the thiazide-induced hypokalemia. The correction of hypokalemia may reduce the risk of cardiac arrhythmias, glucose intolerance, and sexual impotence which seems to be mediated by the thiazide-induced hypokalemia [24]. In the Systolic Hypertension in the Elderly Program (SHEP), participants who had hypokalemia after 1 year of treatment with a low-dose diuretic did not experience the reduction in cardiovascular events achieved among those who did not have hypokalemia suggesting that hypokalemia may limit the protective effects of lowering BP [25]. Clinically, diuretics have been found to be equally effective in reducing cardiovascular events as a CCB-based therapy (nifedipine GITS) [26]. A recent study in patients with resistant hypertension has suggested that combining diuretics is also a useful approach to improve BP control by reducing the compensatory sodium reabsorption in the distal segments of the nephron [27]. Yet, combinations of diuretics containing a potassium-sparing agent must be used cautiously in patients with reduced renal function and should not be prescribed to patients with severe renal insufficiency or pre-existing hyperkalemia.
Single-pill combinations containing a blocker of the renin-angiotensin system (ACE inhibitor, ARB, or renin inhibitor) and a diuretic (thiazide, chlorthalidone, indapamide) belong today to the most frequently used combinations in the management of hypertension. There is strong physiological rationale for this association. Indeed, the negative sodium balance induced by the diuretic triggers the release of renin and the production of angiotensin II. Hence, the maintenance of BP becomes angiotensin II-dependent. In this context, blockade of the reactive activation of the RAS enhances the BP lowering effect of diuretics. Conversely, the diuretic-induced stimulation of aldosterone leading to hypokalemia is blunted with the administration of the RAS blocker therefore preserving an intact potassium balance [20, 28]. This SPC is generally very well tolerated, and several studies have demonstrated that the association of a RAS blocker and a diuretic is superior in terms of BP control to a high dose of the RAS blocker alone. Recently, the issue of which is the best diuretic has been the topic of some discussions. Indeed, there is more clinical evidence that chlorthalidone reduces cardiovascular events in hypertension than hydrochlorothiazide (HCTZ) [29], and differences in potency between HCTZ and chlorthalidone in favor of the latter have been clearly demonstrated [30]. Yet, almost all RAS blockers are currently combined with low doses of HCTZ. SPCs with low doses of indapamide and perindopril [31, 32] and, more recently, of the ARB azilsartan medoxomil and chlorthalidone are available. These combinations have been shown to be effective in lowering BP [33] and/or preventing cardiovascular events [31]. For example, recent comparative studies have suggested that the SPC of azilsartan medoxomil and chlorthalidone induces a greater fall in 24-h ambulatory BP than azilsartan/HCTZ [34] or olmesartan/HCTZ [35].
Today, the SPC of a RAS blocker and a CCB has gained a great popularity. The two classes of drugs can be prescribed as first-line therapy in hypertension and have been shown to prevent the development of cardiovascular events. One advantage of the combination is that the incidence of peripheral edema induced by the CCB is significantly blunted although not entirely abolished by the RAS blocker [36, 37] The sudden enthusiasm for this combination of drugs is to be attributed to the very interesting findings of the ACCOMPLISH trial (Avoiding Cardiovascular Events in Combination Therapy in Patients Living with Systolic Hypertension) which compared two fixed-dose combinations in patients with a high cardiovascular risk. The results of this trial have demonstrated that the fixed-dose combination of benazepril/amlodipine is superior to the benazepril/HCTZ combination in reducing cardiovascular as well as renal events in high cardiovascular risk patients [10, 38]. In this trial, the benazepril/amlodipine SPC reduced the relative risk of cardiovascular events by 20 % and the relative risk of progression of chronic kidney disease by 48 % despite a similar overall BP control in the two groups. The clinical benefits of combining a RAS blocker and a CCB were also supported by the results of the INVEST [INternational VErapamil SR-Trandolapril] and ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) trials [39, 40]. These two trials did not use fixed-dose combinations but investigated the efficacy and clinical benefits of a therapeutic strategy based on a CCB as first-line therapy and a RAS blocker as second line of treatment in comparison to a beta-blocker-based strategy in which a diuretic could be added in second line. The INVEST trial assessed the clinical benefits of the Verapamil SR +/− trandolapril on cardiovascular events in patients with coronary heart disease, and the control group received atenolol +/− HCTZ. Both strategies were equally effective in terms of prevention of cardiovascular events. In the ASCOT trial, an amlodipine-based therapy was compared to an atenolol-based therapy with the possibility to add perindopril to amlodipine and HCTZ to atenolol. In this trial, the CCB-RAS blocker association was found to be superior to the beta-blocker-diuretic to prevent cardiovascular events and reduce cardiovascular mortality. Since then, several other SPCs combining an ACE inhibitor or an ARB or a renin inhibitor with amlodipine or another CCB such as lercanidipine have been launched for the treatment of hypertension [21].
Whether one SPC is superior to the other in preventing hypertension-induced target organ damages and cardiovascular complications and whether some groups of patients have greater benefits from some combinations than others are frequent questions asked by physicians in charge of hypertensive patients. Regarding the first question, the results of the ACCOMPLISH and ASCOT trials suggest that some combinations of drugs are indeed superior to some others. However, it is always important to consider the characteristics of patients enrolled in these studies before extrapolating the results to the entire hypertensive population, For instance, although both studies were conducted in patients at high cardiovascular risk, the ACCOMPLISH trial included more patients of African origin. Thus, the results of ACCOMPLISH may not be applicable to all populations around the world. Moreover the findings of one trial may contradict those of other studies leaving physicians with a great difficulty to conclude for their patients. For example, it is generally thought that obese patients should probably not receive a diuretic, unless absolutely necessary, because of the high risk of inducing a glucose intolerance and increasing the incidence of type 2 diabetes [41]. Yet, in a post hoc analysis of the ACCOMPLISH trial, the thiazide-based treatment was found to give less cardiovascular protection in patients with a normal weight than in obese patients whereas amlodipine was equally effective whatever the body weight [42]. According to the latter observation, diuretics should be recommended in obese patients. This example illustrates the difficulty to define which category of hypertensive patients will benefit the most from the various combination therapies available in clinical practice. Specifically designed studies should be conducted to answer these questions. While waiting for the results of such studies, the critical issue remains to control BP with the most effective combination. In this respect, Stergiou et al. examined the additional BP lowering effect of adding a diuretic, a CCB, or an ACE inhibitor on top of an ARB in patients uncontrolled with the maximal dose of ARB alone [43]. Although all three drugs added to the ARB lowered BP, only the addition of the CCB or a diuretic induced a significant decrease in BP enabling to increase the percentage of patients under control. This observation further confirms our initial hypothesis that combining drugs with different modes of action is preferable to an increase in dose of drugs or combining drugs acting on the same mechanism of BP control. In this respect, one has to mention that combining an ACE inhibitor and an ARB or a renin inhibitor is no longer recommended by guidelines because of the increased risk of acute renal failure and hyperkalemia as observed in the ONTARGET trial [6, 44].
Taken together, the data available in the literature on the use of SPC in hypertension suggest that two SPCs containing two antihypertensive agents tend to prevail in the management of hypertensive patients, i.e., the combination of a RAS blocker and a diuretic and the association of a RAS blocker and a dihydropyridine CCB.
From Dual to Triple Single-Pill Combination
When evaluating the data of the large clinical trials in hypertension, it is evident that most patients with a high cardiovascular risk but also those with mild to moderate hypertension and a lower risk need more than 2 drugs to normalize their BP [6]. There are also disturbing results around the world showing that because of medical inertia, many patients with uncontrolled BP are maintained on a two-drug combination therapy when they should probably receive an additional drug to obtain an adequate control of their BP [18, 45]. Thus, debating on which is the best SPC of two drugs may be of limited interest when a substantial percentage of patients (between 30 and 70 % depending on the studied populations and severity of hypertension) will need three drugs or more and the main issue is to convince physicians to prescribe them [46]. In difficult-to-treat patients or pseudo-resistant patients, the prescription of a SPC containing three drug classes recommended as first-line therapies may be very helpful to fight against clinical inertia and improve BP control [6, 46]. A new strategy has therefore emerged with the rapid development of various SPC containing a RAS blocker (ACE inhibitor, ARB, or aliskiren), a CCB (generally amlodipine), and a diuretic (HCTZ or indapamide) [47] [48–50]. Clinical studies have now been published demonstrating that these triple combinations in a single pill effectively reduce BP in patients uncontrolled on a dual therapy either as fixed or as free combinations [51]. The prescription of single-pill triple combinations should therefore be encouraged in patients with uncontrolled BP on a well-dosed dual therapy and in difficult-to-treat patients. They can also be used to replace a triple free-drug combination in order to simplify the therapeutic regimen. One advantage of these SPC is the ability to increase progressively the treatment intensity while staying on the same initial drugs, an approach which tends to reassure patients.
Pros and Cons of Single-Pill Combinations
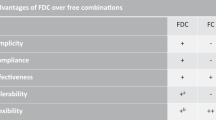
Like all novelties in a therapeutic area, the development of single-pill combinations has pros and cons as discussed recently [52•, 53•] (Table 2). First, it is interesting to note that a survey performed in different European countries has suggested that physicians prefer the term “single-pill combination” to “fixed-dose combination” because the latter gives an impression of limitation due to the fixed characteristic of the description [54].
Regarding the advantages of SPCs, the main argument in favor is the ability to simplify the treatment and to reduce the pill burden, two factors which have been reported as extremely important to support the persistence of therapy in chronic diseases such as hypertension [55•]. Indeed, the lack of persistence has been well described in hypertension with close to 50 % of newly treated patients having interrupted their treatment after 1 year [56]. Several meta-analyses have shown that the use of SPC can lead to a better BP control in hypertension and to a reduced risk of poor adherence [57–59]. However, one has to emphasize that these meta-analyses were conducted on a rather small number of clinical studies and were based on methods of assessing drug adherence which were not always the most adequate ones [60]. Interestingly, the use of SPC is not associated with an increased incidence of side effects because of the positive drug interactions discussed previously in this review. Thus, the prescription of SPC results in a better long-term adherence, a greater decrease in BP, an increased percentage of patients under control, and a reduction in side effects. One important aspect of SPC is the duration of action of the various components included in the combination. Indeed, in order to further improve drug adherence and to increase the therapeutic coverage when patients forget one or more drug doses, it is important that the SPC contains two or three long-acting components in order to maintain BP control even in the context of missed doses [61]. Another advantage is the possibility to use SPCs based on the same initial drug which provides the ability to increase the intensity of the treatment progressively based on drugs that are known and tolerated by the patient thus enabling a kind of continuity of care.
Whether the use of SPC and the associated increase in treatment persistence are associated with a reduction in cardiovascular events and an improved protection has not been firmly demonstrated prospectively but there are some retrospective evidence suggesting that it is indeed the case [62]. For example, in the analysis of a cohort of 242,594 patients with hypertension followed between 2000–2001 and 2007 in Italy, Corrao et al. found that a high adherence to treatment is associated with a 37 % lower risk of cardiovascular outcomes [63].
Several arguments are often opposed to the use of SPC [53•]. As discussed above, the duration of action of individual components may not be equivalent, and this may not justify a single daily dosing of the combination. The use of fixed-dose combinations may result in less flexibility in modifying the doses of individual components and the exposure of patients to unnecessary therapy. Yet, one has to emphasize that many SPCs are provided with several dosages of each component resulting in a high flexibility. Physicians may be confronted with the difficulty to identify the cause of an expected side effect occurring after the prescription of a SPC. In that case, the entire combination should be withdrawn and replaced by free drugs. New galenic forms of the SPC might overcome some of these limitations by separating the different components within a tablet, but this type of SPC is not yet available. It is worth emphasizing that in some cases, physicians do not really know the exact content of single-pill combinations, an observation that may explain some redundant drug prescriptions. As poor adherence is not completely abolished in patients receiving a SPC containing two or three drugs, a physician may be worried by a sudden interruption of treatment which may cause a rebound hypertension and potentially severe complications in particular when the patient was taking a triple combination. There may also be a risk of severe hypotension and malaise in patients uncontrolled on a dual therapy because of non-adherence who are starting on a new single-pill triple therapy. At last, economic arguments may limit the prescription of SPCs because they are in general more expensive than equivalent free combinations now that most antihypertensive drugs are generic.
Conclusions
In the absence of new drugs reaching the market for the treatment of hypertension, the development of single-pill combinations containing two or three antihypertensive agents can be considered as the one of the major contributions to the improvement of hypertension management in the population. With time, SPCs have gained full recognition for their efficacy and usefulness. Today, SPCs tend to replace monotherapies in a very large proportion of clinical situations. Patients with stage 1 hypertension and a low cardiovascular risk and a high probability to have their BP normalized with a single antihypertensive drug should remain on a monotherapy. All other hypertensive patients are good candidates to receive a SPC containing either two or three components. In many countries, SPC are well accepted by physicians and health authorities who have understood the benefits and convenience that SPC provide to patients. In some other countries, the economic concerns will perhaps be overcome with the availability of generic or low-cost SPCs and the demonstration of long-term savings due to a better BP control and the reduction of invalidating cardiovascular events such as stroke, congestive heart failure, and chronic kidney insufficiency.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Waeber B, Brunner HR. Combination antihypertensive therapy: does it have a role in rational therapy? Am J Hypertens. 1997;10(7 Pt 2):131S–7.
Tocci G, Ferrucci A, Guida P, Avogaro A, Comaschi M, Corsini A, et al. An analysis of the management of cardiovascular risk factors in routine clinical practice in Italy: an overview of the main findings of the EFFECTUS study. High Blood Press Cardiovasc Prev Off J Ital Soc Hypertens. 2011;18(1):19–30.
Blonde L, San Juan ZT, Bolton P. Fixed-dose combination therapy in type 2 diabetes mellitus. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2014;20(12):1322–32.
Malerba M, Morjaria JB, Radaeli A. Differential pharmacology and clinical utility of emerging combination treatments in the management of copd—role of umeclidinium/vilanterol. Int J Chron Obstruct Pulmon Dis. 2014;9:687–95.
Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an international association of physicians in aids care panel. Ann Intern Med. 2012;156(11):817–33. W-284, W-285, W-286, W-287, W-288, W-289, W-290, W-291, W-292, W-293, W-294.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 esh/esc guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the european society of hypertension (esh) and of the european society of cardiology (esc). J Hypertens. 2013;31(7):1281–357.
Brunner HR, Menard J, Waeber B, Burnier M, Biollaz J, Nussberger J, et al. Treating the individual hypertensive patient: considerations on dose, sequential monotherapy and drug combinations. J Hypertens. 1990;8(1):3–11. discussion 13–19.
Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens. 2002;4(6):393–404.
Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (hot) randomised trial. Hot study group. Lancet. 1998;351(9118):1755–62.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417–28.
Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(9):882–887 e881. Very interesting paper on the issue of drug adherence in primary and secondary prevention demonstrating the true problems in real life.
Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167(2):141–7.
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–7.
Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–11. J Hum Hypertens. 2015;29(4):247–53.
Materson BJ, Reda DJ, Cushman WC, Massie BM, Freis ED, Kochar MS, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The department of veterans affairs cooperative study group on antihypertensive agents. N Engl J Med. 1993;328(13):914–21.
Bronsert MR, Henderson WG, Valuck R, Hosokawa P, Hammermeister K. Comparative effectiveness of antihypertensive therapeutic classes and treatment strategies in the initiation of therapy in primary care patients: a distributed ambulatory research in therapeutics network (DARTNet) study. J Am Board Fam Med JABFM. 2013;26(5):529–38. An interesting survey on the efficacy of various therpauetic strategies of hypertension in promary care settings.
Mourad JJ, Waeber B, Zannad F, Laville M, Duru G, Andrejak M, et al. Comparison of different therapeutic strategies in hypertension: a low-dose combination of perindopril/indapamide versus a sequential monotherapy or a stepped-care approach. J Hypertens. 2004;22(12):2379–86.
Schafer HH, Sudano I, Theus GR, Noll G, Burnier M. Target blood pressure attainment with antihypertensive therapy in swiss primary care. Blood Press. 2012;21(4):211–9.
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.
Kochar M, Guthrie R, Triscari J, Kassler-Taub K, Reeves RA. Matrix study of irbesartan with hydrochlorothiazide in mild-to-moderate hypertension. Am J Hypertens. 1999;12(8 Pt 1):797–805.
Burnier M, Vuignier Y, Wuerzner G. State-of-the-art treatment of hypertension: established and new drugs. Eur Heart J. 2014;35(9):557–62.
Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development G. Management of hypertension: summary of nice guidance. BMJ. 2011;343:d4891.
Armstrong C. JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90(7):503–4.
Alderman MH, Piller LB, Ford CE, Probstfield JL, Oparil S, Cushman WC, et al. Clinical significance of incident hypokalemia and hyperkalemia in treated hypertensive patients in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension. 2012;59(5):926–33.
Franse LV, Pahor M, Di Bari M, Somes GW, Cushman WC, Applegate WB. Hypokalemia associated with diuretic use and cardiovascular events in the systolic hypertension in the elderly program. Hypertension. 2000;35(5):1025–30.
Brown MJ, Palmer CR, Castaigne A, de Leeuw PW, Mancia G, Rosenthal T, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS Study: intervention as a goal in hypertension treatment (insight). Lancet. 2000;356(9227):366–72.
Bobrie G, Frank M, Azizi M, Peyrard S, Boutouyrie P, Chatellier G, et al. Sequential nephron blockade versus sequential renin-angiotensin system blockade in resistant hypertension: a prospective, randomized, open blinded endpoint study. J Hypertens. 2012;30(8):1656–64.
MacKay JH, Arcuri KE, Goldberg AI, Snapinn SM, Sweet CS. Losartan and low-dose hydrochlorothiazide in patients with essential hypertension. A double-blind, placebo-controlled trial of concomitant administration compared with individual components. Arch Intern Med. 1996;156(3):278–85.
Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension. 2012;59(6):1110–7.
Peterzan MA, Hardy R, Chaturvedi N, Hughes AD. Meta-analysis of dose–response relationships for hydrochlorothiazide, chlorthalidone, and bendroflumethiazide on blood pressure, serum potassium, and urate. Hypertension. 2012;59(6):1104–9.
Patel A, Group AC, MacMahon S, Chalmers J, Neal B, Woodward M, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the advance trial): a randomised controlled trial. Lancet. 2007;370(9590):829–40.
Mogensen CE, Viberti G, Halimi S, Ritz E, Ruilope L, Jermendy G, et al. Effect of low-dose perindopril/indapamide on albuminuria in diabetes: preterax in albuminuria regression: premier. Hypertension. 2003;41(5):1063–71.
Sica D, Bakris GL, White WB, Weber MA, Cushman WC, Huang P, et al. Blood pressure-lowering efficacy of the fixed-dose combination of azilsartan medoxomil and chlorthalidone: a factorial study. J Clin Hypertens. 2012;14(5):284–92.
Bakris GL, Sica D, White WB, Cushman WC, Weber MA, Handley A, et al. Antihypertensive efficacy of hydrochlorothiazide vs chlorthalidone combined with azilsartan medoxomil. Am J Med. 2012;125(12):1229 e1221–10.
Cushman WC, Bakris GL, White WB, Weber MA, Sica D, Roberts A, et al. Azilsartan medoxomil plus chlorthalidone reduces blood pressure more effectively than olmesartan plus hydrochlorothiazide in stage 2 systolic hypertension. Hypertension. 2012;60(2):310–8.
Makani H, Bangalore S, Romero J, Htyte N, Berrios RS, Makwana H, et al. Peripheral edema associated with calcium channel blockers: incidence and withdrawal rate–a meta-analysis of randomized trials. J Hypertens. 2011;29(7):1270–80.
de la Sierra A. Mitigation of calcium channel blocker-related oedema in hypertension by antagonists of the renin-angiotensin system. J Hum Hypertens. 2009;23(8):503–11.
Bakris GL, Sarafidis PA, Weir MR, Dahlof B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (accomplish): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–81.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the anglo-scandinavian cardiac outcomes trial-blood pressure lowering arm (ascot-bpla): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906.
Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, et al. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The international verapamil-trandolapril study (invest): a randomized controlled trial. JAMA. 2003;290(21):2805–16.
Bakris G, Molitch M, Zhou Q, Sarafidis P, Champion A, Bacher P, et al. Reversal of diuretic-associated impaired glucose tolerance and new-onset diabetes: results of the star-let study. J Cardiometab Syndr. 2008;3(1):18–25.
Weber MA, Jamerson K, Bakris GL, Weir MR, Zappe D, Zhang Y, et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the accomplish randomised controlled trial. Lancet. 2013;381(9866):537–45.
Stergiou GS, Makris T, Papavasiliou M, Efstathiou S, Manolis A. Comparison of antihypertensive effects of an angiotensin-converting enzyme inhibitor, a calcium antagonist and a diuretic in patients with hypertension not controlled by angiotensin receptor blocker monotherapy. J Hypertens. 2005;23(4):883–9.
Mann JF, Anderson C, Gao P, Gerstein HC, Boehm M, Ryden L, et al. Dual inhibition of the renin-angiotensin system in high-risk diabetes and risk for stroke and other outcomes: results of the ONTARGET trial. J Hypertens. 2013;31(2):414–21.
Campbell DJ, McGrady M, Prior DL, Coller JM, Boffa U, Shiel L, et al. Most individuals with treated blood pressures above target receive only one or two antihypertensive drug classes. Intern Med J. 2013;43(2):137–43.
Basile J, Neutel J. Overcoming clinical inertia to achieve blood pressure goals: the role of fixed-dose combination therapy. Ther Adv Cardiovasc Dis. 2010;4(2):119–27.
Lanier G, Sankholkar K, Aronow WS. Azilsartan, aliskiren, and combination antihypertensives utilizing renin-angiotensin-aldosterone system antagonists. Am J Ther. 2014;21(5):419–35.
Oparil S, Melino M, Lee J, Fernandez V, Heyrman R. Triple therapy with olmesartan medoxomil, amlodipine besylate, and hydrochlorothiazide in adult patients with hypertension: the trinity multicenter, randomized, double-blind, 12-week, parallel-group study. Clin Ther. 2010;32(7):1252–69.
Lacourciere Y, Taddei S, Konis G, Fang H, Severin T, Zhang J. Clinic and ambulatory blood pressure lowering effect of aliskiren/amlodipine/hydrochlorothiazide combination in patients with moderate-to-severe hypertension: a randomized active-controlled trial. J Hypertens. 2012;30(10):2047–55.
Toth K, Investigators P. Antihypertensive efficacy of triple combination perindopril/indapamide plus amlodipine in high-risk hypertensives: results of the pianist study (perindopril-indapamide plus amlodipine in high risk hypertensive patients). Am J Cardiovasc Drugs. 2014;14(2):137–45.
Weir MR, Hsueh WA, Nesbitt SD, Littlejohn 3rd TJ, Graff A, Shojaee A, et al. A titrate-to-goal study of switching patients uncontrolled on antihypertensive monotherapy to fixed-dose combinations of amlodipine and olmesartan medoxomil +/− hydrochlorothiazide. J Clin Hypertens. 2011;13(6):404–12.
Taddei S. Fixed-dose combination therapy in hypertension: pros. High Blood Press Cardiovasc Prev Off J Ital Soc Hypertens. 2012;19(2):55–7. An intersting debate on the pros and cons of using fixed-dose combinations in the, anagement of hypertension. Assocaited with the paper of ANgeli et al. below.
Angeli F, Reboldi G, Mazzotta G, Garofoli M, Ramundo E, Poltronieri C, et al. Fixed-dose combination therapy in hypertension: cons. High Blood Press Cardiovasc Prev Off J Ital Soc Hypertens. 2012;19(2):51–4.
Burnier M. Fixed combinations in the pragmatic management of hypertension: focus on aliskiren and hydrochlorothiazide as a single pill. Integr Blood Press Control. 2010;3:57–62.
Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62(2):218–25. A careful review of the different techniques of measuring and analysing adherence data with a description of all the pitfalls and limits of the various available techniques.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336(7653):1114–7.
Kizilirmak P, Berktas M, Uresin Y, Yildiz OB. The efficacy and safety of triple vs dual combination of angiotensin ii receptor blocker and calcium channel blocker and diuretic: a systematic review and meta-analysis. J Clin Hypertens. 2013;15(3):193–200.
Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713–9.
Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension. 2010;55(2):399–407.
Halpern MT, Khan ZM, Schmier JK, Burnier M, Caro JJ, Cramer J, et al. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension. 2006;47(6):1039–48.
Burnier M, Brede Y, Lowy A. Impact of prolonged antihypertensive duration of action on predicted clinical outcomes in imperfectly adherent patients: comparison of aliskiren, irbesartan and ramipril. Int J Clin Pract. 2011;65(2):127–33.
Tung YC, Lin YS, Wu LS, Chang CJ, Chu PH. Clinical outcomes and healthcare costs in hypertensive patients treated with a fixed-dose combination of amlodipine/valsartan. J Clin Hypertens. 2015;17(1):51–8.
Corrao G, Parodi A, Nicotra F, Zambon A, Merlino L, Cesana G, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29(3):610–8.
Compliance with Ethics Guidelines
Conflict of Interest
M Burnier declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Novel Treatments for Hypertension
Rights and permissions
About this article
Cite this article
Burnier, M. Antihypertensive Combination Treatment: State of the Art. Curr Hypertens Rep 17, 51 (2015). https://doi.org/10.1007/s11906-015-0562-0
Published:
DOI: https://doi.org/10.1007/s11906-015-0562-0