Abstract
Purpose of Review
Adherence to antiretroviral treatment (ART) is crucial for the successful treatment of HIV. Unfortunately, it is estimated that 45% of persons living with HIV (PLWH) have poor adherence to ART. To provide health care professionals and PLWH with effective tools for supporting adherence, researchers have investigated the effectiveness of psychosocial interventions to enhance adherence to ART. In this paper, interventional studies, systematic reviews, and meta-analyses that examine ART adherence interventions for PLWH are reviewed.
Recent Findings
There is great variability among interventions in terms of quality, sample, measures, and outcome characteristics. Despite a diverse and wide-ranging assortment of ART adherence interventions, consistent lessons have been learned. Interventions that focus on individual and interpersonal factors have been effective for improving ART adherence; however, the improvement in adherence tends to be short-lived. Additionally, interventions are most successful when tailored to those at risk for poor adherence. Finally, theory-based interventions are more likely to be effective than non-theory-based interventions.
Summary
A variety of individual-level psychological interventions have been shown to be effective in improving ART adherence in the short term. Digital and mobile interventions have the potential to improve dissemination and implementation of these evidence-based interventions and could be used to extend intervention effects. Future interventions that address issues of accessibility, inequality, structural and institutional barriers to ART adherence should also be tested and prioritized. Implementation science frameworks can be used to assess and address issues of accessibility and systematic barriers to care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soon after the introduction of highly active antiretroviral therapy (HAART) in 1996, HIV infection transformed from a life-threatening disease to a chronic illness. However, it was quickly discovered that for HAART to suppress viral replication and remain effective over time, high levels of patient adherence are needed [1,2,3,4]. Although improvements in adherence have been evident with newer and simpler regimens of antiretroviral therapy (ART) [5], a recent study found that 45% of individuals living with HIV had poor adherence to ART [6]. Similarly, only half of the people living with HIV (PLWH) in the USA are virologically suppressed [7]. In low- and middle-income countries (LMIC) where clinical resources are more limited, the rates of retention in care and virologic suppression are even lower [8]. Consequences of poor adherence include the emergence of drug-resistant strains of HIV, increased incidence of opportunistic infections, increased morbidity and mortality, and increased rates of hospitalization. Long-term optimal adherence (i.e., consistent uptake of over 80% of ART doses) [7, 9, 10] not only yields improved individual health outcomes, but is also a form of prevention as suppressing HIV viral replication inhibits transmission to others [7]. In addition, adherence to HIV-related medical appointments allows for other important interventions to occur such as risk reduction counseling, mental health and substance use referrals, and healthcare maintenance [11, 12].
The reasons for poor adherence to ART and HIV-related care are diverse and span individual, interpersonal, and structural factors [9]. A meta-analysis of 207 studies found that adherence in PLWH was significantly improved by greater self-efficacy, social support, and a belief that ART was necessary. In contrast, adherence was reduced by the presence of substance use, financial constraints, depressive symptoms, and HIV-related stigma [5]. Additionally, remarkable health disparities exist for racial and ethnic minorities regarding adherence to ART and HIV care. Several studies have demonstrated poorer adherence among African Americans, men who have sex with men (MSM), transgender persons, and youth [4, 13,14,15,16,17,18]. Thus, a clear need exists for efficacious interventions to improve adherence among diverse populations as well as those facing economic hardship.
To provide healthcare professionals and PLWH with effective tools for supporting adherence, researchers have investigated the effectiveness of psychosocial interventions to enhance adherence to ART. Broadly, psychosocial interventions involve providing participants with knowledge, skills, and techniques in order to enact behavioral change [19, 20]. Ideally, they are also tailored towards a specific population and rooted in an established theory that addresses the complex biopsychosocial and environmental factors that interfere with healthy behaviors.
A multitude of models and theories have been applied to ART adherence interventions. They generally emphasize the importance of addressing patients’ motivation, self-efficacy, beliefs, and the larger social context in order to enhance adherence [21]. For example, according to the Information, Motivation, Behavioral Skills model (IMB), gaining relevant HIV and HIV treatment information is a prerequisite for optimal ART adherence. Personal motivation and social motivation (perceived social and cultural support for performing these acts) related to ART adherence, as well as the behavioral skills and perceived self-efficacy to engage in appropriate adherence behaviors, are also critical components [22, 23]. Social cognitive theory (SCT) developed by Albert Bandura, has also been utilized in adherence interventions [24,25,26,27,28,29]. This theory posits that health-promoting behaviors are governed by several core determinants, including an individual’s perceived (1) self-efficacy regarding their ability to make a positive change, (2) knowledge about how their behavior impacts their health, (3) outcomes that may result from their actions, (4) overall goals for their health, (5) facilitators for making a change, and (6) impediments to this change [30]. In addition, the stress and coping theory proposed by Lazarus and Folkman (1984) has been used in adherence interventions [31,32,33]. This theory maintains that an individual’s effective response to a stressor depends on their cognitive appraisal and the behaviorally derived coping mechanisms they choose to utilize as a result. Another example of a theory used in ART adherence interventions is the theory of empowerment education. This theory suggests that individuals who are disenfranchised or disempowered can best gain knowledge and change behavior when they take control over their own learning and actions. This change occurs through the development of a deeper understanding of their position within a community and through active participation and engagement [34]. Additionally, cognitive behavioral therapy (CBT) and motivational interviewing (MI) are also psychotherapeutic models utilized widely in the literature to enact positive behavioral change in individuals with chronic illnesses [35,36,37,38,39,40,41,42,43,44,45,46,47]. CBT addresses the relationship between cognitive distortions and maladaptive behaviors in order to improve self-confidence, coping skills, and problem-solving abilities (APA, 2017). MI seeks to tap an individual’s inner motivation to change by reducing their resistance to change, exploring their ambivalence about it, and enhancing their readiness for it [48].
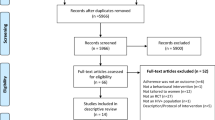
These various theories and models have been used in ART adherence interventions in multiple settings, for a wide range of participants. In recent years, technological advances have also been employed. In this paper, interventions, systematic reviews, and meta-analyses that examine ART adherence interventions for PLWH are reviewed. Because of the broad range of adherence interventions and outcomes in PLWH, we used broad search terms and phrases (antiretroviral/ART adherence, HIV adherence, psychosocial intervention to improve antiretroviral adherence) to identify pertinent published studies in PubMed, CINAHL, Web of Science, and PsycINFO. We also searched the National Institutes of Health Research Portfolio Online Reporting Tools (NIH-RePORT) for interventions still underway.
In-person Interventions
There are numerous in-person adherence interventions for PLWH with various sample sizes, locations, theories or models, and modalities (e.g., individual or group sessions, peer or professional facilitator). Studies examining the effectiveness of in-person CBT and MI interventions have yielded very promising, although not always significant, results. For example, Wagner et al. (2006) compared the effectiveness of a five-session CBT intervention to treatment as usual (TAU) in 230 PLWH. CBT participants were more likely to take at least 90% of their ART doses (82% vs. 65%; p < 0.01) at week 4, but the change was not sustained at weeks 12 and 24 [35]. Also, Golin et al. (2006) compared individual MI versus general education in a randomized controlled trial (RCT) of 140 adult PLWH. While group differences were not statistically significant, adherence in the MI group increased by 4.5% (p = 0.10) and optimal adherence was greater as well (29% vs. 17%, p = 0.13) [24]. These and other studies suggest that CBT and MI are promising interventions for ART adherence.
Some interventions have focused on skills training and education. In a RCT, Johnson and colleagues (2010) enrolled PLWH (n = 249; 226 males) who were concerned about ART side effects [33]. The intervention, based on stress and coping theory, consisted of five individual counseling and training sessions focused on coping with medication side effects. Odds of non-adherence in the intervention group decreased 6% per month (OR = 0.94; p = 0.02), compared to the control group. Similar efficacy has been shown with group sessions. For example, In The Mix was a skills-based intervention grounded in conflict theory of decision making that was designed to reduce HIV transmission risk by targeting sexual risk behaviors and suboptimal medication adherence via 7 facilitator-led sessions (2 individual, 5 group). In a RCT among PLWH (n =436), the intervention was effective for improving medication adherence (β = 0.07, p < 0.05) and reducing unprotected sex (β = 0.43, p < 0.05) at 4.5 months post-intervention.
Considering that greater social support has been associated with better medication adherence [5], utilizing peers as intervention facilitators would seem to be a logical strategy. However, recent reviews find that peer-led interventions are either of unclear benefit [49] or are ineffective [50]. However, Mark et al. (2019) argue that the high degree of heterogeneity among such studies, such as how peer services are employed and operationalized, may be the reason behind inconsistent results [51]. They suggest that peer-based interventions may be particularly useful for specific groups, such as adolescents and young people (youth) living with HIV (YLWH). For example, the Red Carpet Program intervention, which included peer counseling and education, resulted in a statistically significant improvement in linkage to and retention in ART care (ps < 0.001) for up to 6 months among YLWH (n =559) in Kenya [52]. Of note, no theoretical basis or model was explicitly mentioned in this program. Similarly, Link LA, a peer navigation intervention, was based in SCT and designed for HIV-infected men and transgender women scheduled to be released from jail (n =356). It demonstrated significant improvements in viral suppression at 12 months (p = 0.03), but not in medication adherence as compared to a case management control [25]. Consequently, there may be benefits to peer support interventions, but the effectiveness may vary based on location, outcomes, population, and services provided.
Despite promising results for in-person ART adherence interventions, further research is needed, including cost-effectiveness analyses and how to best sustain improvements in adherence post-intervention. A meta-analysis involving 5479 HIV-infected adults, with a median time between baseline and final adherence assessments of 9 months, found that while psychosocial interventions do enhance ART adherence when compared to TAU (SMD = 0.30, 95% CI 0.20–0.40), the significance of this effect was not sustained long-term [53]. The majority of the interventions in the analyses were in-person and only 3 of the 27 primarily utilized computers or phones. In-person psychosocial interventions may require multiple sessions and trained facilitators, making them time and cost-intensive. Therefore, using computer or mobile health (mHealth) interventions may more affordably deliver content or provide booster sessions to sustain intervention effects.
Technology-Based Interventions
The need for more readily disseminatable, affordable interventions has generated interest in the development of computerized, electronic, and mobile technologies to promote ART adherence [54]. A myriad of programs and devices have been developed and tested, including electronic pill monitoring devices, text messaging, and mobile gaming interventions [4]. These technologies have the potential to improve dissemination and implementation of evidence-based treatments, both domestically and abroad. Technology can also assist in the delivery of intervention content to highly stigmatized or vulnerable populations (e.g., youth, those who have financial constraints, are homeless, have substance use disorders, or exchange sex for money). Vulnerable and stigmatized person groups more frequently fall out of care and could be less likely to engage in in-person interventions [54, 55].
Computerized Interventions
The first computerized interventions to improve ART adherence were offline software programs delivered in clinical settings. A comprehensive review examined seven computerized ART adherence interventions for PLWH. Of these, four showed significant improvement in adherence using various measures, and another two-approached significance [56]. The interventions varied in theoretical orientation, utilizing CBT principles, the IMB model [57,58,59], MI/motivational enhancement framework [42, 43], and SCT [56] and social action theory [60].
LifeWindows was one of the first examples of a comprehensive computer-delivered intervention for promoting ART adherence. It was grounded in the IMB model and was delivered at regularly scheduled HIV care visits at five clinical settings with nearly 600 PLWH in the USA. When looking at the intent to treat sample, the intervention did not significantly improve adherence to care compared to the control. However, of those who remained in care (n=398), the intervention’s impact was significant, resulting in significantly higher levels of perfect three-day adherence at 18 months. This study also demonstrated the feasibility of integrating a computerized intervention into clinical care settings among a large number of patients [57].
Electronic Adherence Monitoring Devices
Electronic interventions have also evolved to include technologies that can be easily utilized by patients outside of clinical settings. One of the first well-known health technologies to monitor adherence in this manner was an electronic adherence monitoring device (EAM) known as the Medication Event Monitoring System (MEMS). The MEMS device records pill cap opening and closing events; adherence data can then be downloaded using a USB cable [61]. A meta-analysis examining the utility of MEMS (or MEMS-like devices) in a variety of medical conditions, showed that feedback or counseling sessions informed by MEMS-recorded dosing patterns positively influenced adherence behaviors [62, 63]. An example of an effective in-person intervention enhanced with MEMS is the AIMS intervention in which patients examined differences between their desired and actual adherence recorded by MEMS during a MI-informed counseling session. A RCT (n=133) found that the intervention increased the number of patients with an undetectable viral load at 4 months (OR = 2.96, p < 0.05) [37].
More recently, real-time EAMs such as Clever Cap, Wisepill, Wisebag, evriMED 500/1000, AdhereTech, GlowCaps, MedMinder, MedSignals, Sensemedic Smart, and Tell-Me-Box have been developed. These devices function similarly to standard EAMs but transmit adherence data via cellular networks in real-time. Many of these devices can deliver adherence reminders through text messaging, audiovisual reminders, and alarms at the time of a missed dose. Challenges to EAMs’ real-world utility include the need to keep EAMs charged and gaps in network coverage [64, 65]. Additionally, concerns remain about unintended disclosure of HIV status among PLWH as device alarms can draw attention and the devices themselves can be bulky [39, 66].
The most important limitation of real-time EAMs is that they only target missed doses due to forgetfulness. Although forgetfulness is commonly cited as a reason for non-adherence, patients’ actual reasons for “forgetting” doses can be more complex than they appear. Forgetfulness is a product of motivational issues and cognitive processes. This complexity explains why EAMS that are coupled with theory-driven behavioral interventions have been more effective in improving adherence in PLWH than EAMS alone [67]. In addition to reminders, interventions need to target individuals’ poor information about HIV and its consequences, inconsistent motivation, and a lack of skills needed for ideal adherence behaviors.
Short Messaging Service Interventions (SMS)
Text messages that contain motivational and skill-building content have been used in combination with real-time monitoring devices to improve ART adherence. For example, Sabin and colleagues performed a RCT with 120 HIV patients in China who were provided personalized, triggered, and real-time SMS reminders, coupled with counseling sessions, when missed doses were detected by Wisepill [39]. At 9 months, mean adherence for the intervention arm was 96.2% versus 89.1% in the control (p = 0.003). These significant changes in mean adherence between the groups were also appreciated among those with suboptimal (p = 0.039) and optimal (p = 0.028) pre-intervention adherence [39].
A meta-analysis of 34 studies by Mayer et al. found impressive effects of text messaging interventions on HIV-related treatment adherence in a variety of care outcomes. The analyses showed that text message reminders significantly (1) reduced the rates of non-attendance (n = 7; OR, 0.66; p= 0.01; I2 = 52%), (2) increased ART adherence (n = 20; SMD, 0.87; p = 0.04; I2 = 99%), and (3) improved physiologic measures (CD4 count or viral load) (n = 11; SMD, 1.53; p=0.003; I2=99%). Most of the SMS interventions were of short duration (6 months or less) and used messaging only once or twice weekly to reduce message fatigue [68].
Recent reviews have also shown that SMS interventions are more successful when interactive and guided by theory. It is believed that interactive text messages allow for emotional support and more opportunities to provide tailored information to build knowledge, motivation, and skills. Garofalo et al. conducted a randomized trial of a two-way, interactive, personalized daily text messaging intervention with 105 YLWH who were non-adherent. The intervention was informed by SCT and optimal adherence was assessed by self-report. At 6 months, those in the intervention period were more likely to be optimally adherent (OR = 2.12, p < 0.05), and the effect was maintained at 12 months [28].
SMS allows for the provision of intervention content to patients living in remote areas without access to smartphones and with limited ability to interact with clinic staff. For these reasons, there have been more international trials testing HIV-related SMS interventions in LMICs than in developed countries [69] Two recently published RCTs from sub-Saharan Africa demonstrate the potential for text messages to improve adherence outcomes among young people, who spend large amounts of time on their phones. An RCT from Nigeria of 209 adolescents (aged 15–19) with suboptimal ART adherence found that those in the daily two-way text message ART reminder group, compared to the control group, had lower log10 viral loads (1.97 vs. 2.63; p = 0.001) and higher rates of viral suppression (63% vs. 46%; p = 0.022) [70]. Another RCT in Uganda with YLWH (n = 155), informed by behavioral economics, tested two SMS interventions compared to a standard of a care control group. Of the intervention conditions, one group received weekly SMS feedback on their actual ART adherence level as measured by Wisepill; the second group received similar feedback as well as a report on the adherence levels of their peers. The addition of the peer adherence report improved ART adherence compared to the control group (2.4% difference controlling for baseline adherence levels) but was not statistically significant.
Social Media
Social media has been increasingly used to deliver HIV-related interventions. Unlike SMS interventions, the majority of social media interventions have been tested in developed countries in which patients are more likely to have smartphones with connectivity to online media. Popular social media platforms, such as Facebook, Instagram, and YouTube, are interactive, allowing users to generate content [71, 72]. Social media also provides convenient access to information, services, and social communities for stigmatized populations.
A recent systematic review by Cao et al. (2016) examined the effectiveness of social media interventions to promote HIV testing, linkage to care, adherence, and retention. Many HIV testing and linkage to care campaigns have been successfully tested on social and sexual networking sites such as Facebook, Grindr, YouTube, Twitter, QQ, Gaydar, Jack’d, Scruff, A4A, and Radar. However, this review found a dearth of effective social media interventions to promote adherence to ART [71, 73]. The only ART adherence study cited in the Cao et al. (2016) review was “Thrive with Me” (TWM), an intervention for HIV-positive men who identify as gay or bisexual. TWM has three components: (1) a social networking feature; (2) tailored ART adherence information and medication reminders; and (3) and reflection. Men reporting imperfect ART adherence in the past month were randomized to receive usual care (n = 57) or the 8-week TWM intervention (n = 67). The TWM intervention appeared feasible to implement, acceptable to users, and showed modest effects for the overall sample. Furthermore, among current drug-using participants, the TWM (vs. control) group reported significantly higher overall ART adherence (90.1 vs. 57.5% at follow-up; difference = 31.1, p = 0.02) [72]. A larger trial of TWM is currently being conducted among 400 MSM living with HIV [74].
There are more social media interventions to promote ART adherence in development and testing. One such study, entitled weCare, is designed to increase linkage and retention to HIV care among racially and ethnically diverse young MSM ages 13 to 34. Based on SCT and theory of empowerment education, this intervention utilizes participants’ existing social media preferences (e.g., Facebook’s in-app instant messenger), SMS, and an assigned health educator. The adherence-focused components include feedback about ART refills and daily medication reminders, problem-solving for ART prescription and adherence barriers, and positive reinforcement of desired behaviors. At the time of this review, the results of this trial are unavailable [27].
Gamification
Serious games—designed to influence learning or health behavior change—are increasingly being used to address factors that inhibit adherence to medical treatment regimens [75,76,77,78]. These games are designed to be goal-oriented, motivating, immersive, and enjoyable [79]. Serious games have been shown to influence health attitudes and self-efficacy in other chronic diseases such as asthma, diabetes, and cancer [80,81,82].
A review of gaming interventions for PLWH identified five digital ART adherence games from NIH reporters, and the majority target YLWH and are in development or testing [77]. A small number of RCTs utilizing mobile gaming interventions to improve adherence to ART have reported outcome data. BattleViro, a 16-week iPhone gaming adherence intervention grounded in the IMB model, was tested in a RCT with 61 YLWH. While playing BattleViro, participants travel through multiple organs in the body, fight off HIV, collect strength by taking pills and solve HIV-related puzzles. Participants in the intervention arm received the BattleViro gaming app, an electronic pill monitoring device, and twice-weekly game-related text messages guided by monitoring device data. Participants with perfect adherence were sent texts of congratulations (e.g., “Great job in Battle. You are winning!”) and others were sent motivational texts (e.g., “Get back in battle! Take your dose!). BattleViro demonstrated promising, but nonsignificant, improvements in HIV knowledge (ESD = 0.50), ART knowledge (ESD = 0.42) and social support (ESD = 0.62). Exploratory moderation analyses revealed significant interactions between BattleViro and newly starting ART. Those newly starting ART in the BattleViro condition, compared to those in the control, experienced a 0.96 log greater decrease in viral load (ESD = −2.21, p = 0.04), better adherence (71% vs 48%; ESD = 1.15, p = 0.05), more HIV knowledge (ESD = 0.90), and more ART knowledge (ESD = 0.72) [23].
Another gaming app, AllyQuest, combines social networking, game mechanics, such as challenges, points, and rewards, and a medication tracker to improve ART adherence. Participants also utilized an app-based calendar for reflection on adherence over time. Development was guided by health behavior change theories including SCT, narrative communication (e.g., storytelling), and the Fogg Behavioral Model of persuasive technology [83]. A 28-day pilot trial was conducted with 20 HIV-positive YMSM, ages 19 to 24 years. Participants found the app easy to use and navigate, not intrusive, and experienced few technical issues. Higher levels of app usage were positively correlated with HIV self-management outcomes. There was a statistically significant (p < 0.05) positive association between the number of days logged into the app and knowledge and confidence in ability to reliably take HIV medications [29].
Multilevel Apps/Multilevel Interventions
The weCare intervention, described above, is an excellent example of a multilevel intervention, as it includes in-person, SMS, Facebook, and app-based instant messaging [27]. More multilevel interventions for PLWH exist; however, many have not been tested in an RCT. The Health Resources and Services Administration (HRSA) funded an initiative entitled “Using Social Media to Improve Engagement, Retention, and Health Outcomes along the HIV Care Continuum Initiative for Youth and Young Adults Living with HIV.” Ten clinical demonstration sites examined the feasibility and acceptability of various combinations of bi- and/or unidirectional messaging services, SMS/text messaging, original or adapted mobile applications, and social media to improve adherence [84]. Two promising projects from the initiative are OPT-In for Life and PositiveLinks. OPT-In for Life is a multifaceted, mobile app-based intervention with integrated user-friendly features including a two-way secure SMS, viewable HIV-related laboratory results, and appointment and medication reminders. It was tested among 92 YLWH (18 to 34 years old) who had a history of falling out of care or had detectable HIV viral loads. Retention rates among study participants increased from 41.3% at baseline to 78.6% at 6-month follow-up. This rate was maintained at 12-month follow-up (79.8%), and slightly decreased to 73.4% at 18-month follow-up but it was still significantly higher than the baseline retention rate (p < 0.0001). The rate of viral suppression (HIV RNA <200 copies/mL) increased from 64.1% at baseline to about 85% at 6-month and at 12-month follow-up and reached 91.4% at 18-month (p = 0.0002) among the participants who were retained in care [85]. Although these demonstration projects intervened on multiple technological levels (e.g., social media, SMS, apps), the utilization of familiar smartphone technology likely contributed to their success.
There has been an impressive evolution in mHealth adherence interventions for PLWH. However, significant gaps in our knowledge remain. The vast majority of newer mHealth interventions have been tailored to adolescents and young adults [77]. Although youth are early adopters and widespread utilizers of technologies, mobile phone use is ubiquitous, and people of all ages have access to mobile technology. mHealth interventions for older adults and other special groups are needed. Additionally, there is a great need in moving mHealth pilot studies to larger-scale clinical trials. Finally, future mHealth or eHealth adherence trials for PLWH should address issues of implementation in clinical settings and measure cost-effectiveness. The recently funded UNC/Emory Center for Innovative Technology (iTech) Across the Prevention and Care Continuum is developing standardized cost collection analytic strategies to be used across their current research portfolio of ten technology-based HIV-related interventions. Proving the cost-effectiveness of mHealth interventions will aid in their widespread clinical use [86].
Targeted and Tailored Interventions
In the USA and around the world, some populations are disproportionately impacted by HIV/AIDS and are at higher risk for suboptimal ART adherence. In addition to youth, other vulnerable populations include racial minorities, women (both cis- and transgender), MSM, and older adults. Also, depression and substance use disorders are the most common noncommunicable comorbidities among PLWH [87, 88] and have been consistently shown to be associated with reduced ART adherence. Psychosocial interventions that address the needs of these groups have the potential to improve overall health outcomes and reduce illness burden. While promising examples of such interventions exist, some clear and pressing gaps remain.
Adolescents and Youth
There is a great need for adherence-promoting interventions for YLWH as this population has an increased HIV-related mortality rate, and poorer retention in care compared to older individuals [89]. As of 2018, youth (ages 13 to 24 years) accounted for 21% of new HIV diagnoses in the USA [90]. Furthermore, among PLWH, youth have low rates of viral suppression. The Centers for Disease Control and Prevention (CDC) estimate that only 30% of YLWH are virally suppressed, 43% receive some HIV care, and 31% are retained in care [90]. Surveillance data indicates that YLWH (ages 18 to 24) are more likely to identify as racial and sexual minorities, engage in sexual activity without a condom, and have psychosocial stressors, including poverty, incarceration, substance abuse, and homelessness, as compared to older PLWH (all p < 0.01) [91]. In addition to these stressors, YLWH face transitions in care from their pediatric healthcare providers to adult care settings during young adulthood. This transition often results in rupture in care. A recent review found highly variable rates of retention (37% to 94.7%) after this transition with worsening rates over time [92]. In an effort to reach youth with an appealing intervention format, many of the promising ART adherence interventions for YLWH utilize technology (as reviewed above) [28, 52, 93].
Older Individuals
Because antiretroviral medications have enabled individuals to live longer with HIV, over half of all PLWH in the USA are over the age of 50 [94]. Studies have found that older age is associated with reduced ART adherence [94, 95]. Unfortunately, there is a dearth of ART adherence interventions tailored to older adults. Older PLWH face many unique challenges, including increased comorbidities, physical and cognitive impairments, and adverse drug interactions [94]. Non-adherence among older individuals is of particular concern as it can hasten disease progression and mortality [94]. To identify possible intervention strategies, Johnson et al. assessed 244 PLWH over age 50 using the cognitive-affective model based on social support theory and the stress and coping model. Neuropsychological functioning was not associated with ART adherence, and consistent with the stress and coping model, social support and maladaptive coping were mediators. Therefore, future interventions for older adults should address negative affect and provide adaptive coping strategies and social support [95]. An open pilot trial by Pagan-Ortiz et al. tested a text-based mobile phone intervention to improve ART adherence among 21 older (ages 50–68) African Americans living with HIV. The intervention, informed by the Health Beliefs Model and SCT, incorporated pill reminders, and motivational/informational messages. At the 8-week follow-up, ART adherence was significantly improved by self-report. This suggests that text-based interventions are a feasible and effective method to improve adherence in older PLWH [26]. Telephone-delivered ART adherence interventions are another option and are currently being explored in the ongoing PRIME study among a sample of 426 PLWH over age 50 in the USA [96].
Women
In 2018, women comprised 19% of new HIV diagnoses in the USA and, of these women, 57% identified as Black or African American [97]. Furthermore, AIDS is the leading cause of death globally for females between the ages of 15 and 49 [98]. Suboptimal ART adherence has been associated with female gender and minority status [99, 100]. However, existing interventions for women living with HIV (WLWH) show mixed results and there are few existing interventions specifically tailored to African American WLWH [100]. The Keeping Health and Active with Risk Reduction and Medication Adherence (KHARMA) Project is an ART adherence trial [36]. It was tested in a sample of primarily African American WLWH on ART (n = 203) who were randomized into nurse-led MI intervention or control health promotion program [40]. Adherence rates significantly declined in both groups (p < 0.0005), but at 3 months, intervention participants who attended seven or more sessions took more doses and took them more on time than controls (p = 0.04). On a larger scale, Pellowski et al. (2019) conducted a systematic review (n = 14) and meta-analysis (n =13) of ART adherence interventions that included 1806 cisgender WLWH. Analyses initially demonstrated that the interventions were effective at increasing medication adherence, but they lost significance when two studies with larger effect sizes were excluded. Moderators of larger effect sizes included employing group-based interventions (β= 0.47; p =0.049), being located in an LMIC (β = 0.50; p = 0.043), and utilizing nurses and peer counselors (β= 0.53; p = 0.02). As noted by the authors, only three of the studies explicitly stated that the intervention had a gender-specific focus, despite specifically recruiting and targeting ART adherence in WLWH [101].
Pregnancy also poses a unique challenge to ART adherence for WLWH. Barriers to medication initiation and adherence in pregnancy include lack of knowledge, younger age, unknown HIV status, lack of self-efficacy and social support, stigma, and concerns about cost and side effects [102]. Also, there is a significant risk of WLWH dropping out of care during the postpartum period. One retrospective cohort study of 561 WLWH in the USA demonstrated that in the 2 years post-delivery, only 25% of the participants were retained in care and 34% were virally suppressed [103]. Psychosocial interventions have attempted to address these issues. The use of peer support in improving postpartum care retention has shown promise in WLWH in African countries, particularly interventions that include home visits, counseling, medication reminders, education, and cognitive behavioral skills [104]. Furthermore, a meta-analysis of pregnant WLWH in sub-Saharan Africa (n = 27,974) found that ART adherence was reported by 59.3% of intervention participants versus 22.5% of control participants [105]. Although a variety of interventions were analyzed and there was heterogeneity among outcome variables, ones that addressed a range of psychosocial factors showed a significant effect on adherence: (1) social support and structural support (RR = 1.58; p < 0.00001), (2) education, social support, and structural support (RR = 2.60; 95%; p < 0.00001), and (3) device reminders (RR = 1.13; p = 0.0004).
Transgender women living with HIV are also at risk for suboptimal medication adherence. Of the 2351 transgender individuals who were diagnosed with HIV in the USA between 2009 and 2014, 84% were transgender women and half of them identified as Black or African American [106]. In a study of 2200 YLWH Dowshen et al. (2016) found that transgender women had worse adherence rates than to matched behaviorally infected youth (51.5% versus 30.0%, p = 0.020). Transgender youth were also more likely to report psychosocial stressors, including low educational achievement (p < 0.001) and unemployment (p < 0.001). Furthermore, lack of social support for appointments, unstable housing, and depression increased the predicted probability of having a detectable viral load in these individuals (p < 0.001) [107]. Similar findings have been seen in adults. In a sample of HIV-infected adults, Baguso et al. found that in comparison to men (n =201) and cisgender women (n =72), transgender women (n = 22) had lower adherence to medications (p = 0.028) and were less likely to achieve viral suppression (p = 0.039) [108]. Despite the high incidence of HIV and low rates of ART adherence in transgender women, ART interventions are lacking. These findings illustrate that need for tailored and culturally appropriate interventions for cis- and transgender women living with HIV.
Men Who Have Sex with Men (MSM)
Gay and bisexual men accounted for 69% of new HIV infections in the USA in 2018 [109] and the majority of those men identify as Black or African American [110]. Gay and bisexual men living with HIV face numerous barriers to achieving optimal ART adherence, including stigma, substance use, violence, trauma, limited economic resources, and mental illness [111,112,113]. Furthermore, younger and racial minority men are at an increased risk of not being virally unsuppressed, which increases their risk of poor health outcomes and transmission to their partners [112,113,114]. A variety of ART adherence interventions have been developed and tested, many of which included a substantial proportion of racial minority MSM; however, fewer interventions have been tailored specifically for this group. In addition to the technology-based interventions mentioned above [29, 41], Blashill et al. examined the efficacy of an individual, 12-session CBT intervention for body image and self-care (CBT-BISC) in sexual minority males LWH (n = 44). In this study, compared to participants in TAU, those in CBT-BISC had significantly greater on-time ART adherence during the treatment phase (β = 8.8, p = 0.01) and total adherence at 3 months after the intervention (β = 8.6, p = 0.039) [44]. Combining in-person and technology-based modalities, Project nGage, an intervention designed for young Black MSM (n = 98) using the IMB model, CBT, and MI, employed one 90-min in-person session followed by four mobile phone booster sessions. Those in the intervention, compared to TAU) were 2.91 times more likely to report ≥ 90% medication adherence (p = 0.031) at 12 months [41].
Living with HIV and Depression
Compared to the general population, PLWH are twice as likely to suffer from depression, with 20–30% being affected in the USA [87, 88, 115, 116]. Grief regarding diagnosis, the stress of managing a chronic illness, lack of social support, and internalized stigma are among the factors attributed to this increased prevalence [88]. Untreated depression in PLWH has been associated with cognitive impairment [88], sexual risk behaviors [115, 116], lower CD4 counts, higher viral load, and higher mortality rates [87, 115, 116]. Notably, a meta-analysis of 95 studies revealed that depression was significantly associated with lower ART adherence (p < 0.0001) [87]. Turan and colleagues’ study among women with HIV (n=862) found depressive symptoms mediated the effect of baseline internalized stigma on ART adherence at follow-up (β = −0.05, 95% CI [−0.11, −0.006]), which helps illuminate the mechanism behind these effects on adherence [117].
Treatments for depression (i.e., antidepressants and psychotherapy) have been shown to be effective and safe for use in PLWH [116] and may improve ART adherence. A meta-analysis of 29 studies, from around the world, by Sin et al., demonstrated that, overall, the treatment of depression and psychological distress improved ART adherence (p < 0.001). On average, participants were 83% more likely to adhere to ART if they were treated for depression. This benefit was magnified among samples with lower CD4 counts and more severe depression at baseline [118]. Within this meta-analysis, four well-powered, observational studies examined the effects of antidepressants on adherence, while two additionally compared the effects of antidepressants with psychotherapy on ART adherence [119]. However, neither study reported the types of therapy provided [119, 120]. These four studies all found that those receiving depression treatment had significantly better ART adherence than control PLWH with untreated depression, with all p-values < 0.002 [119,120,121,122]. Furthermore, Turner et al. found that compared to those receiving no depression treatment, the likelihood of adhering to ART was greater for both those receiving solely psychotherapy alone (AOR 1.52; 95% CI, 1.03–2.26) or combined both psychotherapy and antidepressants (AOR 1.49; 95% CI, 1.04–2.15) [119]. Similarly, Akinicigil et al. found that receiving either antidepressants or psychotherapy alone was associated with better adherence than no depression treatment (AOR 2.52; 95% CI, 1.40–4.53) [120].
In another meta-analysis of 14 studies from sub-Saharan Africa, depression interventions were also associated with large improvements in depression (p < 0.01). Pharmacological interventions yielded stronger depression benefits compared to psychological interventions. However, no significant improvement was found on ART adherence, based on CD4 count (p = 0.08) [123]. The bulk of studies have compared depression treatments to no treatment. In contrast, two studies evaluated the impact of a manualized, measured-guided, depression treatment among YLWH at HIV clinical care sites in the USA [124, 125]. Both studies were cluster randomized trials of a medication management algorithm and tailored CBT, which was compared to standard access to medication and psychotherapy at control sites. The larger study enrolled 156 YLWH at thirteen sites and found that the patients at intervention sites, compared to TAU, reported fewer depressive symptoms (p < 0.01) and were more likely to have responded to treatment (62.3% vs. 17.9%, p < 0.001). These studies suggest that tailoring interventions and measured-guided care can improve the efficacy of the treatment of depression.
Despite the high prevalence of depression and the clear benefits of treatment, less than 20% of PLWH with depression receive effective treatment [116]. Low treatment rates in LMICs have been frequently attributed to healthcare provider shortages [87]. To address this issue, healthcare workers could be trained to provide evidence-based, CBT treatments [116]. Another possible solution could be that all practitioners receive standardized depression treatment recommendations through pamphlets and workshops. Findings also suggest the benefit of providing depression-specific health education (opposed to general mental health information) and peer support to PLWH to help them identify signs of depression and seek resources [126].
Living with HIV and Substance Use Disorders
As with depression, studies show elevated prevalence of substance use among PLWH. PLWH consume twice the amount of alcohol as the general population, and roughly 25% meet diagnostic criteria for substance use disorder [45, 127]. Substance use by PLWH is particularly concerning as it is associated with sexual risk behavior and poorer adherence to ART, which can propagate HIV transmission and increase morbidity and mortality [45, 127]. It is imperative that interventions target the unique barriers to ART adherence experienced by those using drugs and/or alcohol.
One US study of 180 heavy drinking, MSM with HIV compared the effects of MI and TAU on reducing problematic alcohol use. The MI group consumed fewer drinks per week at both 6-month (8.0 vs 14.5 drinks; p < 0.001) and 12-month follow-up (7.2 vs 11.6 drinks; p < 0.04) periods compared to the TAU group [15]. However, there were no significant differences in viral load and CD4 count [46]. Another RCT to reduce problematic alcohol use in PLWH (n=40), compared MI/CBT to an equal attention control, the World Health Organization Mental Health Gap Action Programme (WHO mhGAP), in Zimbabwe. In this case, both treatment groups experienced reduction in alcohol use (p < 0.001), and there were no significant differences between groups (p = 0.70) [47]. In contrast to the prior study, both treatment groups also had improved CD4 counts at 3 months. However, it is important to note that the earlier study’s intervention consisted of only one in-person session and two short phone calls, in contrast to sixteen sessions in mhGAP [46, 47].
Altice et al. targeted cocaine and heroin using populations in an individual-level intervention, directly administered ART (DAART) for drug users. Intervention participants were reminded daily via pager to report to a community healthcare van for their medications where adherence could be observed, and social support provided. After 6 months, a significantly greater proportion of the intervention group had a reduction in HIV RNA levels compared to the self-administered therapy group (70.5% vs. 54.7; p = 0.02) [128]. In addition, Turner et al. found that among men living with HIV and a substance use disorder, regular drug treatment was significantly associated with improved ART adherence (AOR= 1.26; 95% CI, 1.02–1.56). Regular drug treatment was also associated with improved ART adherence in men with HIV, depression, and substance use disorder (AOR= 1.65; 95% CI, 1.19–2.28) [119]. One systematic review in the USA assessed the effect of medications for opioid use disorder (OUD) on ART adherence among PLWH. Overall, both methadone and buprenorphine were correlated with improved adherence, when measured by viral load and CD4 counts, and reduced mortality among PWLH with OUD [129]. Similar to Altice et al., Lucas and colleagues utilized DAART for a 12-month intervention among opioid users in a methadone clinic with daily direct observation of patients using ART. At 6 months, the intervention group, compared to the control, had a significantly larger decrease in viral load (2.5 vs. 1.3 log10 copies/mL, p = 0.001) and larger proportion who achieved an undetectable viral load (74% vs. 41%, p < 0.001) [130].
These studies highlight the importance of addressing substance use among PLWH. To do this, clinicians should screen patients for alcohol and drug use, monitor their adherence and refer them to targeted treatment [131]. One such example is the adaptation of the intervention Life Steps by Claborn et al., to include educational, motivational, and behavioral skills components that target both ART adherence and substance use among PLWH [127]. Furthermore, those with OUD would likely benefit from medications for OUD, such as buprenorphine and naloxone, and from needle exchange programs [129, 132].
Conclusions
When reviewing the literature on psychosocial interventions to improve ART adherence in PLWH, it can be a challenge to draw sweeping conclusions. There is great variability among interventions in terms of quality, intervention, sample, measures, and outcome characteristics. However, even with this variability, systematic reviews and meta-analyses have demonstrated that psychosocial interventions improve ART adherence. A recent meta-analysis by Spaan, van Luenen, Garnefski, and Kraaj (2020) examined 43 high-quality RCTs (n = 5095) that specifically examined psychosocial interventions to improve ART adherence. Overall, the analyses demonstrated that psychosocial interventions have a moderately positive effect on ART adherence (Hedges’ g = 0.37; p < 0.001). Study location, duration, and type of intervention, provider, and control used did not significantly impact effect sizes [133]. Therefore, it can be concluded from these analyses that a wide range of psychosocial interventions can be effective for improving ART adherence across a variety of settings.
Our review also demonstrates that interventions informed and guided by models and theories are often more successful than interventions lacking theoretical underpinnings [133]. In the presence of numerous health behavior models and theories, it is impossible to determine which are most useful in improving health behavior. Instead, it is clear that models and theories are useful in identifying the most salient of factors related to ART adherence in a specific population. The list of potential influences is long and includes an individual’s knowledge, attitudes, emotions, and risk perception, power dynamics between partners, accessibility of services, economic inequalities, and stigma. Examination of these factors with models and theories can suggest the most relevant intervention targets to improve health. The majority of ART adherence interventions focus on individual and interpersonal factors, while few address structural, community, and institutional or health system barriers to ART adherence [53]. A recent meta-analysis of psychological interventions to improve ART adherence found that individual-level psychological interventions are effective strategies to improve ART adherence in the short term [53]. However, there is a lack of evidence for interventions demonstrating longer-term improvements in ART adherence. Interventions that address issues of accessibility, inequality, and structural and institutional barriers to care should be prioritized and could demonstrate longer-term improvements in adherence.
It is important to note the lack of ART adherence interventions tailored to African American women, African American MSM, and transgender individuals. These groups are at risk for poor adherence due to stigma as well as structural and systemic barriers to care. Of the 19 interventions listed on the CDC’s Compendium of Evidence-Based Interventions for ART Adherence (DEBI), there are no interventions tailored to African American women, only one tailored to African American MSM, and just one tailored to transgender persons. Despite the large number of interventions for youth in development or pilot stages, there is only one DEBI listed for youth. Future research should examine how to tailor evidence-based approaches to populations that are at risk for suboptimal adherence. Interventions should also assess and intervene upon structural and system-level barriers to adherence in addition to individual-level factors [134].
Implementation science (IS) frameworks can be used to assess and address issues of accessibility, inequality, structural and institutional barriers to care and could be helpful in tailoring interventions to marginalized groups. Incorporation of evolving clinical, cultural, and community context into intervention delivery is critical for addressing inequity. IS frameworks can also be used to examine both individual and system-level factors influencing the sustainment of intervention effects [135].
Future research should examine intervention cost-effectiveness in clinical settings, outside the context of the RCT. Technology-based interventions hold great potential for cost-effective intervention delivery. However, even easily scalable technologies require receptive healthcare delivery systems and human and financial investment. IS frameworks can also be used for understanding and harnessing community and system-level resources for long-term sustainability [136, 137].
Another future area of research is the identification of flexible interventions that address a “continuum” of ART adherence needs. It is unlikely that the needs of a person newly starting ART are similar to those of a patient who has been in long-term care. Nor is it reasonable to assume that the needs of patients with poor ART adherence are similar to those who are working to maintain optimal or perfect adherence. Sequential, multiple assignments, randomized trials (SMART) trials can intervene with groups of patients scattered across a continuum of adherence needs using a variety of intervention components in order to determine the optimal intervention components.
This review adds to the existing literature by establishing the positive effect of a wide range of psychosocial interventions on medication adherence in PLWH. Better medical adherence improves the health of individuals living with HIV and decreases transmission risk. Achieving optimal ART adherence can be challenging, especially in the long term. It is important for clinicians and researchers to understand both the evolution of ART adherence interventions and the most recent developments in the field.
Data Availability
Not applicable.
Change history
15 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11904-021-00573-y
References
Howard AA, Arnsten JH, Lo Y, Vlahov D, Rich JD, Schuman P, et al. A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS England. 2002;16:2175–82.
Knobel H, Alonso J, Casado JL, Collazos J, González J, Ruiz I, et al. Validation of a simplified medication adherence questionnaire in a large cohort of HIV-infected patients: the GEEMA Study. AIDS England. 2002;16:605–13.
Knobel H, Guelar A, Carmona A, Espona M, González A, López-Colomés JL, et al. Virologic outcome and predictors of virologic failure of highly active antiretroviral therapy containing protease inhibitors. AIDS Patient Care STDS United States. 2001;15:193–9.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med United States. 2000;133:21–30.
Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdóttir TB, Richter C, et al. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med. 2014. https://doi.org/10.1186/s12916-014-0142-1.
Benson C, Wang X, Dunn KJ, Li N, Mesana L, Lai J, et al. Antiretroviral adherence, drug resistance, and the impact of social determinants of health in HIV-1 patients in the US. AIDS Behav. 2020;24:3562–73. https://doi.org/10.1007/s10461-020-02937-8.
Centers for Disease Control and Prevention (CDC). Vital signs: HIV prevention through care and treatment--United States. [Internet]. MMWR. Morb. Mortal. Wkly. Rep. 2011. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22129997
World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. WHO Guidel. 2014;
Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis an Off Publ Infect Dis Soc Am. United States. 2013;57:1164–71.
Byrd KK, Hou JG, Hazen R, Kirkham H, Suzuki S, Clay PG, et al. antiretroviral adherence level necessary for HIV viral suppression using real-world data. J Acquir Immune Defic Syndr. 2019;82:245–51.
Cavaleri MA, Kalogerogiannis K, Mckay MM, Vitale L, Levi E, Jones S, et al. Barriers to HIV care: an exploration of the complexities that influence engagement in and utilization of treatment. Soc Work Health Care. 2010;49:934–45. https://doi.org/10.1080/00981389.2010.514563.
Metsch LR, Pereyra M, Messinger S, Del Rio C, Strathdee SA, Anderson-Mahoney P, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis an Off Publ Infect Dis Soc Am. United States. 2008;47:577–84.
Mannheimer S, Friedland G, Matts J, Child C, Chesney M. The consistency of adherence to antiretroviral therapy predicts biologic outcomes for human immunodeficiency virus-infected persons in clinical trials. Clin Infect Dis an Off Publ Infect Dis Soc Am. United States. 2002;34:1115–21.
Golin CE, Liu H, Hays RD, Miller LG, Beck CK, Ickovics J, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17:756–65.
Moss AR, Hahn JA, Perry S, Charlebois ED, Guzman D, Clark RA, et al. Adherence to highly active antiretroviral therapy in the homeless population in San Francisco: a prospective study. Clin Infect Dis an Off Publ Infect Dis Soc Am. United States. 2004;39:1190–8.
Thrasher AD, Earp JAL, Golin CE, Zimmer CR. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. J Acquir Immune Defic Syndr. United States. 2008;49:84–93.
Simoni JM, Huh D, Wilson IB, Shen J, Goggin K, Reynolds NR, et al. Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60:466–72.
Kyser M, Buchacz K, Bush TJ, Conley LJ, Hammer J, Henry K, et al. Factors associated with non-adherence to antiretroviral therapy in the SUN study. AIDS Care England. 2011;23:601–11.
England MJ, Butler AS, Gonzalez ML, editors. Psychosocial interventions for mental and substance use disorders: a framework for establishing evidence-based standards. Washington (DC); 2015.
World Health Organization. Withdrawal Management. Clin guidel withdrawal manag treat drug depend closed settings. 2009.
Adefolalu AO. Cognitive-behavioural theories and adherence: application and relevance in antiretroviral therapy. South Afr J HIV Med. 2018;19.
Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, et al. The information-motivation-behavioral skills model of ART adherence in a deep south HIV+ clinic sample. AIDS Behav. 2009;
Whiteley L, Brown LK, Mena L, Craker L, Arnold T. Enhancing health among youth living with HIV using an iPhone game. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2018;30.
Golin CE, Earp J, Tien H-C, Stewart P, Porter C, Howie L. A 2-arm, randomized, controlled trial of a motivational interviewing-based intervention to improve adherence to antiretroviral therapy (ART) among patients failing or initiating ART. JAIDS J Acquir Immune Defic Syndr [Internet]. 2006;42. Available from: https://journals.lww.com/jaids/Fulltext/2006/05000/A_2_Arm,_Randomized,_Controlled_Trial_of_a.6.aspx
Cunningham WE, Weiss RE, Nakazono T, Malek MA, Shoptaw SJ, Ettner SL, et al. Effectiveness of a peer navigation intervention to sustain viral suppression among HIV-positive men and transgender women released from jail: the LINK LA randomized clinical trial. JAMA Intern Med. 2018;178:542–53.
Pagan-Ortiz ME, Goulet P, Kogelman L, Levkoff SE, Weitzman PF. Feasibility of a texting intervention to improve medication adherence among older HIV+ African Americans: A mixed-method pilot study. Gerontol Geriatr Med. 2019;5:2333721419855662.
Tanner AE, Mann L, Song E, Alonzo J, Schafer K, Arellano E, et al. Wecare: A social media–based intervention designed to increase HIV care linkage, retention, and health outcomes for racially and ethnically diverse young MSM. AIDS Educ Prev. 2016;
Garofalo R, Kuhns LM, Hotton A, Johnson A, Muldoon A, Rice D. A randomized controlled trial of personalized text message reminders to promote medication adherence among HIV-positive adolescents and young adults. AIDS Behav. 2016;
Hightow-Weidman L, Muessig K, Knudtson K, Srivatsa M, Lawrence E, LeGrand S, et al. A gamified smartphone app to support engagement in care and medication adherence for HIV-positive young men who have sex with men (AllyQuest): development and pilot study. J Med Internet Res. 2018.
Bandura A. Health promotion by social cognitive means. Heal Educ Behav Off Publ Soc Public Heal Educ. United States. 2004;31:143–64.
Folkman S. Personal control and stress and coping processes: a theoretical analysis. J Pers Soc Psychol. 1984;46:839–52.
Bova C, Burwick TN, Quinones M. Improving women’s adjustment to HIV infection: results of the Positive Life Skills Workshop Project. J Assoc Nurses AIDS Care. United States. 2008;19:58–65.
Johnson MO, Dilworth SE, Taylor JM, Neilands TB. Improving Coping Skills for Self-management of treatment side effects can reduce antiretroviral medication nonadherence among people living with HIV. Ann Behav Med. 2011;41:83–91. https://doi.org/10.1007/s12160-010-9230-4.
Cummins J. Negotiating identities: education for empowerment in a diverse society. Ontario, Canada: California Association of Bilingual Education; 2001.
Wagner GJ, Kanouse DE, Golinelli D, Miller LG, Daar ES, Witt MD, et al. Cognitive-behavioral intervention to enhance adherence to antiretroviral therapy: a randomized controlled trial (CCTG 578). AIDS [Internet]. 2006;20. Available from: https://journals.lww.com/aidsonline/Fulltext/2006/06120/Cognitive_behavioral_intervention_to_enhance.11.aspx
Holstad MMD, DiIorio C, Magowe MKM. Motivating HIV positive women to adhere to antiretroviral therapy and risk reduction behavior: The KHARMA Project. Online J Issues Nurs. 2006.
de Bruin M, Hospers HJ, van Breukelen GJP, Kok G, Koevoets WM, Prins JM. Electronic monitoring-based counseling to enhance adherence among HIV-infected patients: a randomized controlled trial. Health Psychol. 2010.
Linde DS, Korsholm M, Katanga J, Rasch V, Lundh A, Andersen MS. One-way SMS and healthcare outcomes in Africa: systematic review of randomised trials with meta-analysis. PLoS One. 2019;14:e0217485. https://doi.org/10.1371/journal.pone.0217485.
Sabin LL, Bachman DeSilva M, Gill CJ, Zhong L, Vian T, Xie W, et al. Improving adherence to antiretroviral therapy with triggered real-time text message reminders: the China adherence through technology study. J Acquir Immune Defic Syndr. 2015;69:551–9.
Holstad MM, DiIorio C, Kelley ME, Resnicow K, Sharma S. Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS Behav. 2011;15:885–96. https://doi.org/10.1007/s10461-010-9865-y.
Bouris A, Jaffe K, Eavou R, Liao C, Kuhns L, Voisin D, et al. Project nGage: results of a randomized controlled trial of a dyadic network support intervention to retain young black men who have sex with men in HIV care. AIDS Behav [Internet]. 2017;21:3618–29. Available from: https://pubmed.ncbi.nlm.nih.gov/29079949
Naar-King S, Outlaw AY, Sarr M, Parsons JT, Belzer M, Macdonell K, et al. Motivational Enhancement System for Adherence (MESA): pilot randomized trial of a brief computer-delivered prevention intervention for youth initiating antiretroviral treatment. J Pediatr Psychol. 2013;38:638–48.
Shegog R, Markham CM, Leonard AD, Bui TC, Paul ME. “+CLICK”: pilot of a web-based training program to enhance ART adherence among HIV-positive youth. AIDS Care. Taylor & Francis. 2012;24:310–8. https://doi.org/10.1080/09540121.2011.608788.
Blashill AJ, Safren SA, Wilhelm S, Jampel J, Taylor SW, O’Cleirigh C, et al. Cognitive behavioral therapy for body image and self-care (CBT-BISC) in sexual minority men living with HIV: A randomized controlled trial. Heal Psychol Off J Div Heal Psychol Am Psychol Assoc. 2017;36:937–46.
Madhombiro M, Dube B, Dube M, Zunza M, Chibanda D, Rusakaniko S, et al. Intervention for alcohol use disorders at an HIV care clinic in Harare: a pilot and feasibility study. Addict Sci Clin Pract. 2019;14:16.
Kahler CW, Pantalone DW, Mastroleo NR, Liu T, Bove G, Ramratnam B, et al. Motivational interviewing with personalized feedback to reduce alcohol use in HIV-infected men who have sex with men: a randomized controlled trial. J Consult Clin Psychol. 2018;86:645–56.
Madhombiro M, Dube-Marimbe B, Dube M, Chibanda D, Zunza M, Rusakaniko S, et al. A cluster randomised controlled trial protocol of an adapted intervention for alcohol use disorders in people living with HIV and AIDS: impact on alcohol use, general functional ability, quality of life and adherence to HAART. BMC Psychiatry. 2017;17:44.
Rollnick S, Allison J. The Essential Handbook of Treatment and prevention of alcohol problems. Essent Handb Treat Prev Alcohol Probl. 2004.
Boucher LM, Liddy C, Mihan A, Kendall C. Peer-led self-management interventions and adherence to antiretroviral therapy among people living with HIV: a systematic review. AIDS Behav. 2020;24:998–1022. https://doi.org/10.1007/s10461-019-02690-7.
Areri HA, Marshall A, Harvey G. Interventions to improve self-management of adults living with HIV on antiretroviral therapy: a systematic review. PLoS One. Public Library of Science. 2020;15:e0232709. https://doi.org/10.1371/journal.pone.0232709.
Mark D, Hrapcak S, Ameyan W, Lovich R, Ronan A, Schmitz K, et al. Peer support for adolescents and young people living with HIV in sub-Saharan Africa: emerging insights and a methodological agenda. Curr HIV/AIDS Rep. 2019;16:467–74. https://doi.org/10.1007/s11904-019-00470-5.
Ruria EC, Masaba R, Kose J, Woelk G, Mwangi E, Matu L, et al. Optimizing linkage to care and initiation and retention on treatment of adolescents with newly diagnosed HIV infection. AIDS [Internet]. Lippincott Williams & Wilkins; 2017;31 Suppl 3:S253–60. Available from: https://pubmed.ncbi.nlm.nih.gov/28665883
Locher C, Messerli M, Gaab J, Gerger H. Long-term effects of psychological interventions to improve adherence to antiretroviral treatment in HIV-infected persons: a systematic review and meta-analysis. AIDS Patient Care STDs Mary Ann Liebert, Inc. 2019;33:131–44. https://doi.org/10.1089/apc.2018.0164.
Pellowski JA, Kalichman SC. Recent advances (2011-2012) in technology-delivered interventions for people living with HIV. Curr HIV/AIDS Rep. 2012;9:326–34. https://doi.org/10.1007/s11904-012-0133-9.
Swendeman D, Rotheram-Borus MJ. Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Curr. Opin. Psychiatry. Swendeman, Dallas: Center for Community Health, University of California, Los Angeles, 10920 Wilshire Boulevard, Suite 350, Los Angeles, CA, US, 90024, dswendeman@mednet.ucla.edu: Lippincott Williams & Wilkins; 2010. p. 139–44.
Claborn KR, Fernandez A, Wray T, Ramsey S. Computer-based HIV adherence promotion interventions: a systematic review: Translation Behavioral Medicine. Transl Behav Med. 2015;5:294–306.
Fisher JD, Amico KR, Fisher WA, Cornman DH, Shuper PA, Trayling C, et al. Computer-based intervention in HIV clinical care setting improves antiretroviral adherence: the LifeWindows Project. AIDS Behav United States. 2011;15:1635–46.
Hersch RK, Cook RF, Billings DW, Kaplan S, Murray D, Safren S, et al. Test of a web-based program to improve adherence to HIV medications. AIDS Behav. 2013;17:2963–76.
Ownby RL, Waldrop-Valverde D, Caballero J, Jacobs RJ. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav HIV Med. 2012;4:113–21.
Remien RH, Hirky AE, Johnson MO, Weinhardt LS, Whittier D, Le GM. Adherence to medication treatment: a qualitative study of facilitators and barriers among a diverse sample of HIV+ men and women in four U.S. cities. AIDS Behav. 2003;7:61–72. https://doi.org/10.1023/A:1022513507669.
Encyclopedia of Behavioral Medicine. Encycl. Behav. Med. Springer Science+Business Media; 2013
Demonceau J, Ruppar T, Kristanto P, Hughes DA, Fargher E, Kardas P, et al. Identification and assessment of adherence-enhancing interventions in studies assessing medication adherence through electronically compiled drug dosing histories: a systematic literature review and meta-analysis. Drugs. 2013;73:545–62.
Vrijens B, Urquhart J, White D. Electronically monitored dosing histories can be used to develop a medication-taking habit and manage patient adherence. Expert Rev Clin Pharmacol England. 2014;7:633–44.
Mbuagbaw L, Hajizadeh A, Wang A, Mertz D, Lawson DO, Smieja M, et al. Overview of systematic reviews on strategies to improve treatment initiation, adherence to antiretroviral therapy and retention in care for people living with HIV: part 1. BMJ Open. 2020;10:e034793.
Craker L, Tarantino N, Whiteley L, Brown L. Measuring antiretroviral adherence among young people living with HIV: observations from a real-time monitoring device versus self-report. AIDS Behav [Internet]. 2019;23:2138–45 Available from: https://pubmed.ncbi.nlm.nih.gov/30888573.
Van der Elst EM, Mbogua J, Operario D, Mutua G, Kuo C, Mugo P, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013;17:2162–72.
van Heuckelum M, van den Ende CHM, Houterman AEJ, Heemskerk CPM, van Dulmen S, van den Bemt BJF. The effect of electronic monitoring feedback on medication adherence and clinical outcomes: a systematic review. PLoS One Public Library of Science. 2017;12:e0185453. https://doi.org/10.1371/journal.pone.0185453.
Mayer JE, Fontelo P. Meta-analysis on the effect of text message reminders for HIV-related compliance. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2017;29:409–17.
Taylor D, Lunny C, Lolić P, Warje O, Geldman J, Wong T, et al. Effectiveness of text messaging interventions on prevention, detection, treatment, and knowledge outcomes for sexually transmitted infections (STIs)/HIV: a systematic review and meta-analysis. Syst Rev. 2019;8:12.
Abiodun O, Ladi-Akinyemi B, Olu-Abiodun O, Sotunsa J, Bamidele F, Adepoju A, et al. A single-blind, parallel design RCT to assess the effectiveness of SMS Reminders in Improving ART adherence among adolescents living with HIV (STARTA Trial). United States: J Adolesc Heal Off Publ Soc Adolesc Med; 2020.
Cao B, Gupta S, Wang J, Hightow-Weidman LB, Muessig KE, Tang W, et al. Social media interventions to promote HIV testing, linkage, adherence, and retention: systematic review and meta-analysis. J Med Internet Res. 2017;19:e394.
Horvath KJ, Oakes JM, Rosser BRS, Danilenko G, Vezina H, Amico KR, et al. Feasibility, acceptability and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. AIDS Behav. 2013;17:2031–44.
Dulli L, Ridgeway K, Packer C, Murray KR, Mumuni T, Plourde KF, et al. A social media-based support group for youth living with HIV in Nigeria (SMART Connections): randomized controlled trial. J Med Internet Res. 2020;22:e18343.
Horvath KJ, Amico KR, Erickson D, Ecklund AM, Martinka A, DeWitt J, et al. Thrive With Me: protocol for a randomized controlled trial to test a peer support intervention to improve antiretroviral therapy adherence among men who have sex with men. JMIR Res Protoc. 2018;7:e10182.
LeGrand S, Muessig KE, McNulty T, Soni K, Knudtson K, Lemann A, et al. Epic allies: development of a gaming app to improve antiretroviral therapy adherence among young HIV-positive men who have sex with men. JMIR Serious Games. 2016;4:e6.
Kato PM. Video games in health care: closing the gap. Rev Gen Psychol SAGE Publications Inc. 2010;14:113–21. https://doi.org/10.1037/a0019441.
Hightow-Weidman LB, Muessig KE, Bauermeister JA, LeGrand S, Fiellin LE. The future of digital games for HIV prevention and care. Curr. Opin. HIV AIDS. 2017.
Ritterfeld U, Cody M, Vorderer P. Serious games: mechanisms and effects. Serious Games Mech. Eff. 2009.
LeGrand S, Muessig KE, Platt A, Soni K, Egger JR, Nwoko N, et al. Epic allies, a gamified mobile phone app to improve engagement in care, antiretroviral uptake, and adherence among young men who have sex with men and young transgender women who have sex with men: protocol for a randomized controlled trial. JMIR Res Protoc. 2018;7:e94.
Baranowski T, Baranowski J, Cullen KW, Marsh T, Islam N, Zakeri I, et al. Squire’s Quest! Dietary outcome evaluation of a multimedia game. Am J Prev Med Netherlands. 2003;24:52–61.
Brown SJ, Lieberman DA, Germeny BA, Fan YC, Wilson DM, Pasta DJ. Educational video game for juvenile diabetes: results of a controlled trial. Med Inform (Lond). England. 1997;22:77–89.
Kato PM, Cole SW, Bradlyn AS, Pollock BH. A video game improves behavioral outcomes in adolescents and young adults with cancer: a randomized trial. Pediatrics United States. 2008;122:e305–17.
Fogg B. A behavior model for persuasive design. ACM Int Conf Proceeding Ser. 2009.
Medich M, Swendeman DT, Comulada WS, Kao UH, Myers JJ, Brooks RA, et al. Promising approaches for engaging youth and young adults living with hiv in hiv primary care using social media and mobile technology interventions: protocol for the spns social media initiative. JMIR Res Protoc. 2019.
Dillingham R, Ingersoll K, Flickinger TE, Waldman AL, Grabowski M, Laurence C, et al. PositiveLinks: a mobile health intervention for retention in HIV care and clinical outcomes with 12-month follow-up. AIDS Patient Care STDS. Dillingham, Rebecca: UVA School of Medicine, P.O. Box 801379, Charlottesville, VA, US, 22908, rd8v@virginia.edu: Mary Ann Liebert, Inc.; 2018. p. 241–50.
UNC Behavior and Technology Lab. The UNC/EMORY Center For Innovative Technology [Internet]. Available from: https://batlab.web.unc.edu/itech/
Chibanda D. Depression and HIV: integrated care towards 90-90-90. Int Health. 2017.
Rubin LH, Maki PM. HIV, depression, and cognitive impairment in the era of effective antiretroviral therapy. Curr HIV/AIDS Rep. 2019;16:82–95.
Enane LA, Vreeman RC, Foster C. Retention and adherence: global challenges for the long-term care of adolescents and young adults living with HIV. Curr Opin HIV AIDS United States. 2018;13:212–9.
Centers for Disease Control and Prevention (CDC). HIV and Youth. 2020.
Beer L, Mattson CL, Shouse RL, Prejean J. Receipt of clinical and prevention services, clinical outcomes, and sexual risk behaviors among HIV-infected young adults in care in the United States. AIDS Care Taylor & Francis. 2016;28:1166–70. https://doi.org/10.1080/09540121.2016.1160028.
Ritchwood TD, Malo V, Jones C, Metzger IW, Atujuna M, Marcus R, et al. Healthcare retention and clinical outcomes among adolescents living with HIV after transition from pediatric to adult care: a systematic review. BMC Public Health. 2020;20:1195. https://doi.org/10.1186/s12889-020-09312-1.
Whiteley L, Brown LK, Mena L, Craker L, Arnold T. Enhancing health among youth living with HIV using an iPhone game. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2018;30:21–33.
Ghidei L, Simone MJ, Salow MJ, Zimmerman KM, Paquin AM, Skarf LM, et al. Aging, antiretrovirals, and adherence: a meta analysis of adherence among older HIV-infected individuals. Drugs Aging. 2013;30:809–19.
Johnson CJ, Heckman TG, Hansen NB, Kochman A, Sikkema KJ. Adherence to antiretroviral medication in older adults living with HIV/AIDS: a comparison of alternative models. AIDS Care. 2009;21:541–51.
McCoy K, Waldrop-Valverde D, Balderson BH, Mahoney C, Catz S. Correlates of antiretroviral therapy adherence among HIV-infected older adults. J Int Assoc Provid AIDS Care. 2016;15:248–55.
Centers for Disease Control and Prevention (CDC). HIV and Women. 2020.
Joint United Nations Programme on HIV/AIDS (UNAIDS). We’ve got the power — women, adolescent girls and the HIV response [Internet]. 2020. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_women-adolescent-girls-and-hiv_en.pdf
Brown JL, Littlewood RA, Vanable PA. Social-cognitive correlates of antiretroviral therapy adherence among HIV-infected individuals receiving infectious disease care in a medium-sized northeastern US city. AIDS Care [Internet]. 2013/01/11. 2013;25:1149–58. Available from: https://pubmed.ncbi.nlm.nih.gov/23311323
Lambert CC, Mugavero MJ, Najjar YS, Enah C, Guthrie BJ. The state of adherence to HIV care in Black women. J Assoc Nurses AIDS Care. 2018;29:487–503.
Pellowski JA, Price DM, Harrison AD, Tuthill EL, Myer L, Operario D, et al. A systematic review and meta-analysis of antiretroviral therapy (ART) adherence interventions for women living with HIV. AIDS Behav [Internet]. 2019;23:1998–2013. Available from. 2019. https://doi.org/10.1007/s10461-018-2341-9.
Bailey H, Zash R, Rasi V, Thorne C. HIV treatment in pregnancy. Lancet HIV. Elsevier. 2018;5:e457–67. https://doi.org/10.1016/S2352-3018(18)30059-6.
Adams JW, Brady KA, Michael YL, Yehia BR, Momplaisir FM. Postpartum engagement in HIV care: an important predictor of long-term retention in care and viral suppression. Clin Infect Dis. 2015;61:1880–7. https://doi.org/10.1093/cid/civ678.
Momplaisir FM, Storm DS, Nkwihoreze H, Jayeola O, Jemmott JB. Improving postpartum retention in care for women living with HIV in the United States. AIDS [Internet]. 2018;32. Available from: https://journals.lww.com/aidsonline/Fulltext/2018/01140/Improving_postpartum_retention_in_care_for_women.1.aspx
Omonaiye O, Nicholson P, Kusljic S, Manias E. A meta-analysis of effectiveness of interventions to improve adherence in pregnant women receiving antiretroviral therapy in sub-Saharan Africa. Int J Infect Dis Elsevier. 2018;74:71–82. https://doi.org/10.1016/j.ijid.2018.07.004.
Centers for Disease Control and Prevention (CDC). HIV and Transgender People [Internet]. 2019. Available from: https://www.cdc.gov/hiv/pdf/group/gender/transgender/cdc-hiv-transgender-factsheet.pdf
Dowshen N, Matone M, Luan X, Lee S, Belzer M, Fernandez MI, et al. Behavioral and health outcomes for HIV+ young transgender women (YTW) linked to and engaged in medical care. LGBT Heal. 2016;3:162–7.
Baguso GN, Gay CL, Lee KA. Medication adherence among transgender women living with HIV. AIDS Care Taylor & Francis. 2016;28:976–81. https://doi.org/10.1080/09540121.2016.1146401.
U.S. Department of Health & Human Services. HIV Basics: U.S. Statistics [Internet]. 2020. Available from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
Centers for Disease Control and Prevention (CDC). HIV basics: basic statistics. Div. HIV/AIDS Prev. Natl. Cent. HIV/AIDS, Viral Hepatitis, STD, TB Prev. 2021.
Safren SA, Perry NS, Blashill AJ, O’Cleirigh C, Mayer KH. The cost and intensity of behavioral interventions to promote HIV treatment for prevention among HIV-positive men who have sex with men. Arch Sex Behav. 2015;44:1833–41. https://doi.org/10.1007/s10508-014-0455-3.
Quinn KG, Voisin DR. ART adherence among men who have sex with men living with HIV: key challenges and opportunities. Curr HIV/AIDS Rep. 2020;17:290–300.
Mutchler MG, Bogart LM, Klein DJ, Wagner GJ, Klinger IA, Tyagi K, et al. Age matters: differences in correlates of self-reported HIV antiretroviral treatment adherence between older and younger Black men who have sex with men living with HIV. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2019;31:965–72.
Crepaz N, Dong X, Wang X, Hernandez AL, Hall HI. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care - United States, 2014. MMWR Morb Mortal Wkly Rep. 2018;67:113–8.
Pence BW, Gaynes BN, Williams Q, Modi R, Adams J, Quinlivan EB, et al. Assessing the effect of Measurement-Based Care depression treatment on HIV medication adherence and health outcomes: rationale and design of the SLAM DUNC Study. Contemp Clin Trials. 2012;33:828–38.
Pence BW, Gaynes BN, Adams JL, Thielman NM, Heine AD, Mugavero MJ, et al. The effect of antidepressant treatment on HIV and depression outcomes: Results from a randomized trial. AIDS. 2015;29:1975–86.
Turan B, Rice WS, Crockett KB, Johnson M, Neilands TB, Ross SN, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. AIDS. 2019;33:571–6.
Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: a meta-analysis. Ann Behav Med. 2014;47:259–69.
Turner BJ, Laine C, Cosler L, Hauck WW. Relationship of gender, depression, and health care delivery with antiretroviral adherence in HIV-infected drug users. J Gen Intern Med. 2003;18:248–57.
Akincigil A, Wilson IB, Walkup JT, Siegel MJ, Huang C, Crystal S. Antidepressant treatment and adherence to antiretroviral medications among privately insured persons with HIV/AIDS. AIDS Behav. 2011;
Horberg MA, Silverberg MJ, Hurley LB, Towner WJ, Klein DB, Bersoff-Matcha S, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;
Kong MC, Nahata MC, Lacombe VA, Seiber EE, Balkrishnan R. Association between race, depression, and antiretroviral therapy adherence in a low-income population with HIV infection. J Gen Intern Med. 2012;
Passchier RV, Abas MA, Ebuenyi ID, Pariante CM. Effectiveness of depression interventions for people living with HIV in sub-Saharan Africa: a systematic review & meta-analysis of psychological & immunological outcomes. Brain Behav Immun. 2018;73:261–73.
Brown LK, Kennard BD, Emslie GJ, Mayes TL, Whiteley LB, Bethel J, et al. Effective treatment of depressive disorders in medical clinics for adolescents and young adults living with HIV: a controlled trial. J Acquir Immune Defic Syndr. 2016;71:38–46.
Brown L, Chernoff M, Kennard B, Emslie G, Shapiro D, Lypen K, AW SBuisson, Whiteley L, Traite S, Krotje C, Harriff L and ET for the I 2020 team. Site-randomized controlled trial of a combined cognitive behavioral therapy and a medication management algorithm for treatment of depression among youth living with HIV in the United States. 23rd Int AIDS Conf (AIDS 2020).
Graves JC, Elyanu P, Schellack CJ, Asire B, Prust ML, Prescott MR, et al. Impact of a family clinic day intervention on paediatric and adolescent appointment adherence and retention in antiretroviral therapy: a cluster randomized controlled trial in Uganda. PLoS One. 2018;13:e0192068.
Claborn K, Becker S, Operario D, Safren S, Rich JD, Ramsey S. Adherence intervention for HIV-infected persons who use drugs: adaptation, open trial, and pilot randomized hybrid type 1 trial protocol. Addict Sci Clin Pract. 2018;13:12.
Altice FL, Maru DSR, Bruce RD, Springer SA, Friedland GH. Superiority of directly administered antiretroviral therapy over self-administered therapy among HIV-infected drug users: A prospective, randomized, controlled trial. Clin Infect Dis. 2007;45:770–8.
Fanucchi L, Springer SA, Korthuis PT. Medications for treatment of opioid use disorder among persons living with HIV. Curr HIV/AIDS Rep. 2019;16:1–6.
Lucas GM, Mullen BA, Weidle PJ, Hader S, McCaul ME, Moore RD. Directly administered antiretroviral therapy in methadone clinics is associated with improved HIV treatment outcomes, compared with outcomes among concurrent comparison groups. Clin Infect Dis an Off Publ Infect Dis Soc Am. United States. 2006;42:1628–35.
González-Álvarez S, Madoz-Gúrpide A, Parro-Torres C, Hernández-Huerta D, Mangado EO. Relationship between alcohol consumption, whether linked to other substance use or not, and antiretroviral treatment adherence in HIV+ patients. Adicciones. 2019.
Perlman DC, Jordan AE. The Syndemic of Opioid Misuse, Overdose, HCV, and HIV: structural-level causes and interventions. Curr HIV/AIDS Rep. 2018;15:96–112.
van Luenen S, Garnefski N, Spinhoven P, Spaan P, Dusseldorp E, Kraaij V. The benefits of psychosocial interventions for mental health in people living with HIV: a systematic review and meta-analysis. AIDS Behav. 2018.
Centers for Disease Control and Prevention (CDC). Complete listing of medication adherence evidence-based behavioral interventions. 2020.
Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;
Eisman AB, Kilbourne AM, Dopp AR, Saldana L, Eisenberg D. Economic evaluation in implementation science: making the business case for implementation strategies. Psychiatry Res. 2020;283:112433.
Roberts SLE, Healey A, Sevdalis N. Use of health economic evaluation in the implementation and improvement science fields - a systematic literature review. Implement. Sci. 2019
Code availability
Not applicable.
Funding
This work was facilitated by the Providence/Boston Center for AIDS Research (P30AI042853).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Behavioral-Bio-Medical Interface
The original online version of this article was revised: Modifications have been made to the Abstract. Full information regarding the corrections made can be found in the erratum/correction for this article.
Rights and permissions
About this article
Cite this article
Whiteley, L.B., Olsen, E.M., Haubrick, K.K. et al. A Review of Interventions to Enhance HIV Medication Adherence. Curr HIV/AIDS Rep 18, 443–457 (2021). https://doi.org/10.1007/s11904-021-00568-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-021-00568-9