Abstract
Purpose of Review
In 2018–2019, studies were published assessing the effectiveness of reducing HIV incidence by expanding HIV testing, linkage to HIV treatment, and assistance to persons living with HIV to adhere to their medications (the “90-90-90” strategy). These tests of “treatment as prevention” (TasP) had complex results.
Recent Findings
The TasP/ANRS 12249 study in South Africa, the SEARCH study in Kenya and Uganda, and one comparison (arms A to C) of the HPTN 071 (PopART) study in South Africa and Zambia did not demonstrate a community impact on HIV incidence. In contrast, the Botswana Ya Tsie study and the second comparison (arms B to C) of PopART indicated significant ≈ 30% reductions in HIV incidence in the intervention communities where TasP was expanded.
Summary
We discuss the results of these trials and outline future research and challenges. These include the efficient expansion of widespread HIV testing, better linkage to care, and viral suppression among all persons living with HIV. A top implementation science priority for the next decade is to determine what strategies to use in specific local contexts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The “90-90-90” goals of the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization (WHO) aspire for 90% of all people living with HIV to know their status, 90% of all HIV-infected persons who know their status to take antiretroviral therapy (ART), and 90% of those on ART to be virally suppressed, all by the year 2020 [1]. None of these goals will be reached, though global progress is impressive. The goal for the year 2030 is “95-95-95.” Reflecting definitive evidence from the HIV prevention and treatment fields, global recommendations from the WHO shifted in 2016 to urge universal treatment for all people living with HIV (PLHIV), regardless of their CD4+ cell counts or their clinical status [1,2,3]. These recommendations represented a more aggressive and simplified approach to ART initiation and coverage. They were based on recognition that early treatment yielded better clinical outcomes and would prevent transmissions to others (“Treatment as Prevention” [TasP]). Fiscal support to achieve 90-90-90 has come from the US President’s Emergency Plan for AIDS Relief (PEPFAR), the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), National Ministries of Health, and other funding sources from donor countries and foundations. By far, this is the largest single-focus public health campaign in world history with over US$90 billion invested by PEPFAR alone [4]. While much forecasting has been done to determine the extent to which 90% testing-90% ART linkage-90% viral suppression coverage using universal test and treat (also termed “test and start” or “treat all”) guidelines can control the epidemic, there remain questions as to whether TasP can be properly measured and achieved [5,6,7,8]. We have presented a scientific rationale for TasP elsewhere, and key points are reiterated in this review [9].
As progress towards 90-90-90 goals are assessed and complex findings from large-scale TasP studies are interpreted, we review the successes and continued challenges to TasP as a strategy to reduce HIV incidence. Here, we summarize recent findings from four large-scale community-based randomized trials designed to assess the impact of large-scale deployment of TasP on HIV transmission, and discuss the challenges remaining in implementation of TasP and achieving global goals to end HIV.
Findings from Large-Scale Trials of TasP
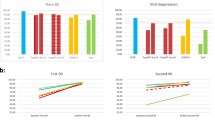
There have been four large-scale clinical trials of TasP with HIV incidence outcomes, all conducted in sub-Saharan Africa: the TasP/ANRS 12249 study in South Africa, the Sustainable East Africa Research in Community Health (SEARCH) study in Kenya and Uganda, the Botswana Combination Prevention Project (BCPP) or Ya Tsie study, and the HIV Prevention Trials Network (HPTN) 071 (PopART) study in South Africa and Zambia [10••, 11••, 12••, 13•]. Each of these studies published primary findings in 2018 or 2019, offering fresh understandings of the facilitators and barriers in reducing HIV incidence in the era of universally recommended testing and treatment. A comparison of the contexts and methods of these trials is available elsewhere [14•]. Figure 1, adapted from [15•], summarizes primary results.
Viral suppression, HIV incidence rates, and overall effectiveness in preventing HIV. Results from community-based cluster-randomized control trials of universal test-and-treat strategies. From New England Journal of Medicine, Abdool Karim SS, HIV-1 Epidemic Control - Insights from Test-and-Treat Trials, 381, 286–288 Copyright © (2019) Massachusetts Medical Society. Reprinted with permission
TasP/ANRS 12249
The first completed trial was the TasP/ANRS 12249 protocol (the TasP study) conducted by the Africa Centre, now part of the African Health Research Institute. The TasP study was a cluster-randomized trial to examine the effectiveness of TasP on HIV incidence in KwaZulu-Natal, South Africa, where adult HIV prevalence has been estimated to be ~ 30% [16]. All 22 population/geographic clusters deployed repeated home-based HIV testing of adults across a population of 34,000 inhabitants 16 years and older. Following an HIV diagnosis, individuals in the 11 intervention clusters were immediately initiated on ART, while those in the 11 control clusters were initiated on ART according to national guidelines at the time (CD4+ < 350 cells/μL, WHO stage 3 or 4 disease, or multi-drug-resistant/extensively drug-resistant tuberculosis). Home-based testing enabled achievement of the first 90 testing target [17]. However, linkage to care and initiation of ART (the second 90) was low in both arms, with 58.5% ART initiation in the intervention arm and 57.5% in the control arm. Viral suppression (the third 90) was higher in the intervention arm (86.6%), but very similar to the control arm (84.1%) [10••]. There was no significant difference in HIV incidence between the intervention (2.11 per 100 person-years; 95% CI 1.84–2.39) and the control (2.27 per 100 person-years; 95% CI 2.00–2.54) groups (adjusted hazard ratio 1.01, 95% CI 0.87–1.17; p = 0.89).
A key lesson from the ANRS 12249 trial was that the intervention failed to overcome barriers to ART initiation and retention in care; hence, the trial was not a good test of concept for TasP, but rather indicated how difficult linkage to care and HIV suppression to reduce HIV incidence is in a rural African setting. Individuals who had never been in HIV care before referral, students, adults who completed some or all secondary schooling, those who lived closer to TasP clinics, and those who were referred to the clinic after two or more contacts were all unlikely to initiate care. Linkage to care was higher in adults who reported knowledge of a family member living with HIV and among those who said that they would take ART as soon as possible after receiving an HIV diagnosis [18]. More recent secondary analyses have provided insights into individuals’ retention in care trajectories [19]. This work identified four trajectories: group 1 that remained in care (71.3%); group 2 that exited care and then returned after a median of 4 months (5.2%); group 3 that exited care rapidly after 4 months (12.6%); and group 4 that exited care later after 11 months (10.9%). Patients with higher CD4+ cell counts were more likely to exit care, but then return. Men, young people, and those recently diagnosed were more likely to exit care at any point during the study. Despite the success of home-based testing (the first 90), the TasP study results suggest that better strategies are needed to link, retain, and enhance ART adherence in rural South Africa, particularly among men, young adults, and newly diagnosed patients.
The SEARCH Study
The SEARCH cluster-randomized trial was conducted in three regions of rural Uganda and Kenya, and embedded TasP within an integrated multi-disease, patient-centered care model that sought to improve overall community health while suppressing HIV incidence via TasP [20]. The primary outcome was cumulative HIV incidence at 3 years, with secondary outcomes including HIV viral suppression, overall mortality, tuberculosis incidence, and control of hypertension. Thirty-two communities were pair-matched and randomly assigned to either intervention or control arms (total population of 150,395 individuals aged 15 years or older). Communities were matched based on geographic region, population density, number of trading centers, variety of community member occupations, and community member mobility patterns. The intervention communities received a package including the following: (1) community health fairs at baseline and annually where HIV, TB, malaria, and non-communicable disease (NCD; hypertension and diabetes) screening was conducted; (2) home-based (or other location of patient’s choice) testing for those who were not tested at fairs’ (3) facilitated linkage and immediate appointments to clinics for ART initiation among all those testing positive; (4) a patient-centered chronic care model for HIV and NCD care; (5) clinics with trained and sensitized providers and flexible operating hours; and (6) mobile phone triage and appointment reminders. Control communities received the following: health fair for testing and diagnosis at baseline only; home-based testing upon request; ART initiation based on national guidelines (which varied based on location and date from CD4+ < 350 cells/μL, WHO stage 3 or 4 disease, or TB/HBV co-infection to CD4+ < 500 cells/μL, but expanded to universal initiation during the study period); and facilitated access to the national standard of care for HIV and NCDs [11••, 21].
As in the TasP/ANRS 12249 study, the first 90 was achieved at baseline in both the intervention (90%) and control (91%) communities. The testing approach was highly successful, achieving an estimated 98% testing coverage of residents in the intervention communities and 96% coverage of residents in the control communities by the end of the study. Testing coverage before the trial started was only 57%. In the intervention communities, testing of residents who had migrated into the communities was made possible by the annual screening approaches [11••]. In the intervention communities, 92% of PLHIV knew their status, 95% of these individuals had initiated ART, and 90% of those on ART achieved viral suppression at the end of the study period. In the control communities, 91% of HIV-positive individuals knew their status, 86% of these individuals had received ART, and 87% on ART were virally suppressed. Overall, population-level viral suppression (calculated as virally suppressed/all HIV+) in the intervention communities (79%) was higher than in the control communities (68%). The secondary community health outcomes were significantly better in the intervention communities with lower rates of tuberculosis in HIV-positive patients (1.19 vs. 1.50 events per 100 person-years; relative risk, 0.79; 95% CI, 0.67 to 0.94) and higher rates of hypertension control in HIV-positive patients (relative prevalence, 1.26; 95% CI, 1.15 to 1.39). Despite these positive outcomes, there was only a small benefit in the 3-year cumulative incidence of HIV infection between the intervention (0.77%) and the control (0.81%) communities that was not statistically significant (relative risk, 0.95; 95% CI, 0.77 to 1.17).
The SEARCH team has offered a few theories that may explain why there was no significant reduction in HIV incidence despite improvements in viral suppression. They note that their control communities were “active” with provision of health fairs and home-based testing at baseline. This active control, combined with guideline changes recommending universal ART eligibility, may have reduced the differences between the intervention and control groups [11••]. However, without baseline HIV rates from the control communities, it is difficult to assess this theory. The authors also suggest possible routes through which new infections could have arisen in the intervention group: infections from non-trial communities, unrecognized outbreaks of acute HIV, and/or infections from unsuppressed individuals. These hypotheses might be tested in future phylogenetic studies. Other possible explanations could be that a subset of individuals was never exposed to the full intervention, including more mobile populations, youth, or individuals during the early stages of new infection and with a high level of infectiousness [22, 23]. The authors state that the in-migration data will be investigated in future analyses, which will allow these hypotheses to be tested. Newly infected individuals may not yet have had an opportunity to be diagnosed, may have tested negative on an antibody test despite having been recently infected, and/or may be those involved with higher numbers of concurrent partnerships. If a high proportion of all new infections arise in these situations, it may be that additional outreach for testing is needed.
The Botswana Combination Prevention Project or Ya Tsie Study
The Ya Tsie study in Botswana also employed a pair-matched community-randomized trial of 30 communities (total n = 12,610). Intervention communities (n = 15) received the following: (1) community mobilization to encourage HIV testing and counseling and male circumcision; (2) home-based and other mobile HIV testing campaigns; (3) linkage to care support; (4) scaled-up linkage to male circumcision services; and (5) expanded ART at government clinics to cover HIV-positive individuals with either CD4+ cell counts of > 350–500 cells/μL or CD4+ > 500 cells/μL and HIV-1 RNA ≥ 10,000 copies/mL. The Ya Tsie study had a focus on combination HIV prevention (through enhanced access to voluntary medical male circumcision in addition to TasP), as was also implemented in the HPTN 071 (PopART) study discussed below. The 15 standard of care communities initiated ART according to national guidelines, i.e., CD4+ ≤ 350, WHO III/IV disease, or pregnancy. As with SEARCH and the PopART study, midway through the study period, Botswana revised their guidelines and the Ya Tsie study began offering immediate ART initiation regardless of CD4 count or clinical status to both study arms [24]. The Ya Tsie study intervention was highly successful, with 88% of all PLHIV in the intervention group achieving viral suppression by the end of the trial (RR, 1.12; 95% CI, 1.09–1.16) [12••]. Rates of circumcision were higher in the intervention communities (30% at baseline and 40% at the end of the trial) compared with the standard of care communities (33% at baseline and 35% at the end of the trial) (RR, 1.26; 95% CI, 1.17–1.35), but were lower than the investigators had expected. The study authors were unable to identify which specific intervention components had the greatest impact, but point to improved linkage-to-care in intervention communities (69 days from diagnosis to ART initiation) compared with control communities (367 days) as a key factor. Recent qualitative data have further elucidated some of the specific barriers and facilitators to ART initiation, suggesting how to further improve the intervention components [25].
One limitation of this trial was a failure to fully engage all household members, such that 20% of age- and residency-eligible members of enumerated households were not enrolled. The most common reasons for non-participation were absenteeism and refusal; it is possible that people not found or not consenting in a household will differ in key characteristics from enrolled participants [24]. In addition, the Ya Tsie study investigators identified remaining vectors of HIV transmission not necessarily reached by the intervention, such as non-community residents, community residents not linked to ART, non-Botswana citizens who do not receive free ART, and persons with acute HIV infection. Women remained at unacceptably high risk for HIV infection even in the intervention communities [12••]. Just as random imbalances of characteristics at baseline could have led to a null result in SEARCH, random imbalances at baseline could have resulted in a positive result in Ya Tsie, e.g., if the intervention group included participants with higher baseline viral suppression, circumcision, and/or ART coverage. However, a sensitivity analysis to examine the effect of non-participation did not suggest this to be the case as findings were robust in the sensitivity models. Furthermore, their estimates of population viral suppression incorporated population mobility [12••]. The Ya Tsie study finding was remarkable since Botswana programs had been close to achieving 90-90-90 goals even at study baseline, reducing power to detect an intervention effect [26]. It may be that the persons reached in the intervention who would not have been reached in the control group (national standard of care) were contributing to HIV incidence such that their engagement was vital to the overall study result. The findings from Botswana suggest that it is possible to increase ART coverage and reduce HIV incidence in a high (29%) prevalence context, even with high baseline testing, linkage, and ART coverage.
In subgroup analyses, the intervention had a greater, though non-significant, effect compared with the standard of care on HIV incidence among men, individuals < 35 years of age, and in communities in more remote northern Botswana. The Ya Tsie study seemed to have had success in reaching men and youth who are typically more marginalized and/or difficult to reach. Qualitative work is in progress to understand how this was accomplished. Botswana’s programmatic successes have been summarized elsewhere [27] and include rapid point-of-care testing, free and decentralized access to ART, and routine access to viral load monitoring. A recent costing analysis of Ya Tsie’s testing component found that the costs of intensive home-based and mobile testing to identify HIV-positive individuals who might otherwise not be found were comparable with such costs in other settings. However, untargeted home-based testing was more expensive given the efforts needed to assess testing eligibility in a setting with high prior testing coverage and ART initiation [28]. Further understanding of costs and cost-effectiveness of the individual intervention components of the Ya Tsie study will help determine the feasibility for analogous interventions to be delivered at scale in Botswana or elsewhere.
The HPTN 071 (PopART) Study
The HPTN 071 (PopART) study was a cluster-randomized trial with 21 communities (n = 50,873) in South Africa and Zambia conducted from 2014 to 2018, with a primary outcome of HIV incidence at 36 months [29]. PopART is an acronym standing for “Population Effects of Antiretroviral Therapy to Reduce HIV Transmission” (https://www.hptn.org/research/studies/hptn071). There were three study arms and seven groups of three clustered communities grouped by similar characteristics, and HIV prevalence levels were randomized. Arm A provided the full PopART combination prevention intervention package and immediate ART initiation for PLHIV. Arm B provided the same package, except that ART initiation followed national guidelines, initially, ART when CD4 count < 350 cells/μL. Guidelines changed to universal ART in 2016, at which time, arm B was identical to arm A. Arm C served as the control, providing standard of care including ART initiation consistent with national guidelines and treatment support from the respective Ministries of Health aided by resources from PEPFAR and other sources. ART initiation in arm C became the same as arms A and B in 2016. The full PopART intervention package included the following elements: (1) annual rounds of home-based HIV testing by community HIV-care providers (CHiPs); (2) active referral and/or retention in care support by CHiPs; (3) referrals/enhanced linkage to voluntary male circumcision for HIV-negative men; (4) community support for antenatal care (ANC)/prevention of mother-to-child transmission (PMTCT), adolescent and male engagement, use of community engagement boards, and community dialog processes; and (5) screening/referral for tuberculosis and sexually transmitted infections (STIs). While CHiPs home-based visits sought to offer testing to persons who did not know their current HIV status, the linking and treatment elements targeted all PLHIV whether newly diagnosed, in care but not receiving ART, or seropositive, but lost to follow-up. In all of the study communities, ART was provided at local government clinics [13•]. PopART findings underscored the need to enhance quality assurance measures for community-based point-of-care testing [30], testing scale-up [31, 32], and linkage to care [31, 33, 34].
The study was powered to detect differences in arm A vs. arm C, and in arm A vs. B, but not arm B vs. arm C, which could therefore be regarded as a secondary comparison [29]. At the end of the study period, there was no difference between the A and C arms, but there was a significant 30% decrease in new HIV infections between the B and C arms [13•]. The HPTN 071 (PopART) trial included 48,301 participants in the population cohort used to estimate incidence rates. Baseline HIV prevalence was 21–22% across study arms, and from months 12–36 of the study, 553 new HIV infections within 39,702 person-years (py) were observed (incidence 1.4/100 py), about twice as high in women than men. The adjusted rate-ratio for arm A vs. C was 0.93 (95% CI 0.74–1.18, p = 0.51) and arm B vs. C was 0.70 (95% CI 0.55–0.88, p = 0.006). Viral suppression at 24 months was 71.9% in arm A, compared with 67.5% in arm B, and 60.2% in arm C. The adjusted prevalence ratio for viral suppression in arm A compared with Arm C was 1.16 (95% CI, 0.99 to 1.36, p = 0.07). The prevalence ratio in arm B compared with arm C was 1.08 (95% CI, 0.92 to 1.27, p = 0.30). For both arms A and B, the prevalence of viral suppression was higher among women compared with men and higher among older participants (aged 25+) compared with younger participants (aged 18–24). ART coverage at 36 months did not differ in arm A (81%) vs. arm B (80%) [13•].
The HPTN 071 (PopART) results require additional work to better understand why there was no significant effect of the intervention on HIV incidence for arm A. The investigators offered some possible explanations. Written informed consent was required for initiation of ART outside local guidelines until the guidelines were changed in 2016. This could have prevented some participants from initiating ART; however, the similarities in coverage and viral suppression across the arms argue against this explanation. The authors also suggest that universal ART in arm A may have changed or decreased actions towards primary prevention. Although the participant-reported data do not support this explanation, the investigators are conducting additional analyses to further examine the possibility. In addition, it is possible that there was imbalance post-randomization of the communities assigned to each arm sufficiently different to confound the results. For example, 38% of arm B participants living with HIV were already on ART at baseline, while only 31–32% of those in the other two arms were. Multivariate adjusted analysis is in progress to address potential confounders, along with further analysis of qualitative and quantitative data as well as phylogenetic data to further understand the unexpected Arms A to C results compared with arms B to C. In addition, given the similarity between the interventions delivered in arm A and B, it is possible that the differences between these two arms was a chance finding, and that their combined difference with arm C (approximately a 20% reduction in incidence) reflects the key, albeit post hoc, finding of the trial. This effect was statistically significant, but smaller than hypothesized (adjusted rate ratio, 0.81; 95% CI, 0.66–0.99) [13•].
Although there were challenges in reaching some key populations, particularly young adults [31], the distribution of young people was similar across the three arms. Although it is possible that in-migration might reduce 90-90-90 coverage, the HPTN 071 (PopART) investigators did not report any differential migration across study arms. As suggested in the other TasP trials, the “last unreached 25%” may be those most responsible for a disproportionately high number of transmissions, such that 90-90-90 coverage may not be adequate to fully reduce the population viral load. We have previously speculated that the 3-year study duration was not long enough to fully observe the effect of the intervention, given suboptimal linkage-to-care rates in the first half of the study [9].
Studies of the Implementation of 90-90-90 in Sub-Saharan Africa
In addition to the large-scale clinical trials of TasP described above, there have been several studies examining the process of implementing the 90-90-90 goals [35,36,37,38,39,40]. Such studies are an anchor of HIV implementation science efforts, and we highlight three of the larger such studies—MaxART in eSwatini (formerly Swaziland) [41], Project Shikamana in Tanzania [42, 43••], and the SAPPH-IRe intervention in Zimbabwe [44••]. None had HIV seroincidence endpoints.
The MaxART (early access to ART for all in Swaziland) study was a stepped-wedge randomized trial with open enrollment of all adults aged 18 years and older across 14 public-sector clinical sites in eSwatini’s HhoHho Region (n = 3405). The goal was to assess the impact of TasP compared with standard of care on patient retention and viral suppression, specifically, the impact of TasP on patients who initiated ART early, rather than on HIV incidence among others. Sites transitioned two at a time from the standard of care to the intervention (early ART initiation) [41]. This study employed mixed methods to determine the feasibility, acceptability, clinical outcomes, affordability, and scalability of offering early ART to all HIV-positive individuals in a public-sector health system. Qualitative findings have provided further context for the role of the community advisory board in supporting study implementation [45], reasons for “false starts” in ART initiation [46], challenges associated with treatment retention for mobile populations [47], and the challenges associated with increasing numbers of patients and task-shifting in public clinics [48]. Interim results of MaxART found that TasP modestly improved retention, improved client perceptions of care quality, and increased retention and viral suppression rates combined fivefold. These findings support the hypothesis that early ART initiation is beneficial, not only for population health, but also for individual patients [49]. Final results reporting the impacts of early initiation, and other key lessons from MaxART are likely to be published in 2020.
Project Shikamana was a prospective community-randomized trial of a community-based model of combination HIV prevention to improve TasP among high-risk female sex workers (FSWs) in the Iringa region of Tanzania [42]. Participants were recruited from entertainment venues, and time-location sampling was used to enroll a cohort of 203 HIV-positive and 293 HIV-negative women. Time-location sampling entailed identifying times when the target population gathered at venues, constructing sampling frames of venues and daytime units, randomly selecting and visiting venues and daytime units, and systematically collecting information from eligible women. Recruitment venues were in two communities, matched in size and overall HIV prevalence. The intervention package included community-led peer education, condom distribution, and HIV testing in entertainment venues; peer navigation to facilitate ART uptake and retention in care; sensitivity training for HIV clinical providers; short message services (SMS) to promote awareness, solidarity, and adherence; and a community-led center with activities to promote social cohesion and community mobilization to address challenges specific to FSWs. As in the other large TasP studies, pre-exposure prophylaxis (PrEP) was not part of the intervention. The control community received standard of care HIV services through government clinics, and HIV health education, condom promotion, and HIV testing initiatives delivered by non-governmental organizations. The study assessed feasibility and acceptance of the package as well as preliminary effectiveness.
Baseline data described participants’ characteristics and progress towards the 90-90-90 goals in this setting, as well as the links between mobility and gender-based violence [42, 50]. The final results indicated that the community-based intervention was highly successful. HIV-negative participants in the intervention community were less likely to have become infected with HIV (OR 0.38, p = 0.047) by the end of the study, and less likely to report inconsistent condom use with a client (RR 0.81, p = 0.042). HIV-positive participants in the intervention community also had better outcomes. A total of 79.1% of HIV-positive participants were linked to care compared with 55% in the control arm (RR 1.44, p = 0.002), and 81.3% of intervention participants were on ART at the study endpoint, compared with 63.8% in the control arm (RR 1.27, p = 0.013). There were positive, but non-significant, improvements in viral suppression as well (from 40 to 50.6% in the intervention vs. 35.9 to 47.4% in the control; RR 1.05, p = 0.7) [43••]. Most of these positive outcomes were also associated with higher levels of exposure to the intervention components. Recent qualitative findings provide insights into how meaningful community engagement was achieved in the intervention [51], and the authors describe plans for future quantitative analyses to examine the relative impact of different intervention components.
The SAPPH-IRe (Sisters Antiretroviral Prevention Programme—an Integrated Response) trial was a pair-matched, parallel, cluster-randomized study nested within the Sisters with a Voice national sex work program in Zimbabwe [44••]. The primary outcome was the proportion of FSWs with HIV viral loads of > 1000 copies/mL. An additional nine secondary outcomes related to aspects of treatment and prevention were also assessed. Similar to Project Shikamana, peer and community engagement was emphasized. In the seven clusters receiving the standard of care, the Sisters program provided FSWs with free condoms and contraception, free HIV testing and counseling, STI treatment, health education, community mobilization, and legal advice. These services were provided at drop-in centers in primary care clinics and supported by peer educators. Women testing HIV-positive were referred to government clinical services. In the seven intervention clusters, an enhanced version of the Sisters program was implemented. This enhanced version provided additional community mobilization activities aimed at raising awareness of the benefits of ART and PrEP, strengthened support networks to encourage health-promoting behaviors and developing leadership skills. In addition, ART and PrEP users were encouraged to join a community-based Adherence Sisters program, which allowed them to nominate a trusted “sister” to serve as their adherence supporter and to attend Adherence Sisters training together. The program also included activities to encourage HIV testing every 6 months among HIV-negative women, including mobile phone messaging reminders. Clinical services were also improved to enable initiation of ART or PrEP on site, in compliance with local and international guidelines. Patient support services were delivered by clinic staff, with text messages and follow-up phone calls used to support clinic attendance. A representative sample for outcome surveys was sought through respondent-driven sampling.
Between study baseline and the end of the assessment period, the proportions of women with viral loads of > 1000 copies/mL dropped in both the control (35.1% reduction) and intervention (45.6% reduction) clusters. However, the weighted percentage risk difference of − 2.8% suggested little difference between the groups (95% CI − 8.1 to 2.5, p = 0.23). Among the secondary outcomes, the proportions of HIV-positive women who reported being aware of their status, taking ART, and being virally suppressed all increased, but to similar degrees between control and intervention groups. The intervention did strengthen engagement of FSWs with services but did not lower overall viral loads in the intervention group relative to the control. Study authors believed their results supported a conclusion that FSWs, if supported, will access services in the public sector. They also identified improvements that could be made in testing and ART uptake. Since the Sisters approach did not specifically seek to identify highly vulnerable sex workers including those who are younger, new to sex work and/or with mental illness, or substance use issues, they may not have reached these individuals, reducing the impact of the intervention. A recently published process evaluation of the trial indicated some challenges with maintaining program fidelity although these challenges were not specific to one arm. The evaluation also found that the overall policy and health system environment in Zimbabwe became more supportive such that HIV testing and care for FSW was prioritized beyond the intervention. The authors feel that increased national emphasis on reaching FSWs may have contributed to the limited difference between the control and intervention clusters [52].
Conclusions and Future Directions
The results from the randomized trials seeking to assess the impact of TasP have been mixed. Each of these studies had to contend with logistical and measurement challenges, which may explain some of the inconsistent findings. Despite what many might consider large budgets, it is nevertheless possible that each of these studies was not adequately funded, and consequently supervised, managed, and conducted, to ensure reliable results concerning the efficacy of these combination interventions. National treatment guidelines in all TasP trial countries changed during the study, which meant that immediate ART initiation became available in the control arms, which would have reduced the power of these studies to detect an effect [15•]. Another challenge faced by all four TasP trials was with adequately identifying and testing difficult-to-reach populations that are simultaneously harder to access for interventions due to mobility or marginalization, and more likely to be the sources for new infections. Although home-based testing, or testing at venues preferred by patients, can help achieve wider testing coverage, the TasP trials reveal that these costly approaches may need to be scaled-up, including expanded testing with lower yield groups and increased self-testing [15•, 53]. The TasP/ANRS 12249 trial had notable difficulties with linkage and retention in care, and may not have been a fair test of concept for TasP. Given that acute and recent infections are more efficiently transmitted, it is important to develop strategies to ensure rapid linkage to care, such as home-based initiation and delivery of ART [54].
Stigma also continues to be a challenge, and was investigated in the PopART study, both in terms of general stigma characteristics of study communities [55] and as a possible explanation for variation in linkage to and retention in care [56, 57]. Some of the trials are still seeking to learn whether reproductive tract infections such as bacterial vaginosis and sexually transmitted infections might have facilitated HIV transmission in selected populations, thereby diluting TasP effects [58]. Finally, it is important to note that the costs and complexities of the four TasP trials demonstrate the difficulties inherent in assessing the feasibility and scalability of TasP in real-world settings [59].
Given that global guidelines urge TasP for the benefit of PLHIV, we believe that the Ya Tsie study and PopART indicate that community transmission can be suppressed with expanded testing and successful treatment of PLHIV, though it may not be as robust as predictive models had hoped, given mathematical HIV transmission models [60, 61]. The greatest challenge now is the deployment of implementation science studies that can identify the best strategies to facilitate efficient and effective program expansion that will be critical to achieve the 95-95-95 goals for 2030, including identifying the components of the complex trials discussed in this article that are most effective and cost-effective for programmatic dissemination and scale-up. Despite the inconsistent findings of the four TasP trials, PEPFAR has been documented as a resounding success, responsible for saving hundreds of thousands of lives and bringing the HIV epidemic down to its relatively lower levels of prevalence and incidence, as compared with the emergency situations in many sub-Saharan countries in the 1980s and 1990s [62,63,64,65,66]. It is thus vital that PEPFAR be continued to achieve the 2030 goals, given the need to scale-up PrEP, and sustain and expand successes in testing, linkage-to-care, and ART-driven viral suppression around the world.
Change history
30 June 2020
The original version of this review article unfortunately contained a mistake in the category section. The Section Editor was inadvertently captured as ���E Geng��� instead of ���SH Vermund���.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Granich R, Williams B, Montaner J, Zuniga JM. 90-90-90 and ending AIDS: necessary and feasible. Lancet. 2017;390(10092):341–3.
Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009;301(22):2380–2.
World Health Organization (WHO). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. World Health Organization. 2016.
The Kaiser Family Foundation (KFF). The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR): Kaiser Family Foundation. 2019 [cited 2019 December]. Available from: https://www.kff.org/global-health-policy/fact-sheet/the-u-s-presidents-emergency-plan-for/. Accessed Nov 2019.
Galvani AP, Pandey A, Fitzpatrick MC, Medlock J, Gray GE. Defining control of HIV epidemics. Lancet HIV. 2018;5(11):e667–e70.
Ghys PD, Williams BG, Over M, Hallett TB, Godfrey-Faussett P. Epidemiological metrics and benchmarks for a transition in the HIV epidemic. PLoS Med. 2018;15(10):e1002678.
Sabapathy K, Hensen B, Varsaneux O, Floyd S, Fidler S, Hayes R. The cascade of care following community-based detection of HIV in sub-Saharan Africa–a systematic review with 90-90-90 targets in sight. PLoS One. 2018;13(7):e0200737.
Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57.
Brault MA, Spiegelman D, Hargreaves J, Nash D, Vermund SH. Treatment as prevention: concepts and challenges for reducing HIV incidence. J Acquir Immune Defic Syndr. 2019;82(2):S104.
•• Iwuji CC, Orne-Gliemann J, Larmarange J, Balestre E, Thiebaut R, Tanser F, et al. Universal test and treat and the HIV epidemic in rural South Africa: a phase 4, open-label, community cluster randomised trial. Lancet HIV. 2018;5(3):e116–e25 This paper presents the primary results and progress towards 90-90-90 of the TasP/ANRS 12249 trial in Kwa-Zulu Natal, South Africa.
•• Havlir DV, Balzer LB, Charlebois ED, Clark TD, Kwarisiima D, Ayieko J, et al. HIV testing and treatment with the use of a community health approach in rural Africa. N Engl J Med. 2019;381(3):219–29 This paper presents the primary HIV and NCD findings from the SEARCH TasP trial conducted in rural Kenya and Uganda.
•• Makhema J, Wirth KE, Pretorius Holme M, Gaolathe T, Mmalane M, Kadima E, et al. Universal testing, expanded treatment, and incidence of HIV infection in Botswana. N Engl J Med. 2019;381(3):230–42 This paper presents the primary findings related to achievement of 90–90-90 in the BotswanaYa TsieTasP trial.
•• Hayes RJ, Donnell D, Floyd S, Mandla N, Bwalya J, Sabapathy K, et al. Effect of universal testing and treatment on HIV incidence - HPTN 071 (PopART). N Engl J Med. 2019;381(3):207–18 This study presents the primary findings from the 3 arms of the PopART TasP trial conducted in South Africa and Zambia.
• Perriat D, Balzer L, Hayes R, Lockman S, Walsh F, Ayles H, et al. Comparative assessment of five trials of universal HIV testing and treatment in sub-Saharan Africa. J Int AIDS Soc. 2018;21(1):e25048. This paper provides a comparative assessment of the trial designs for the key TasP studies discussed in this review.
• Abdool Karim SS. HIV-1 epidemic control - insights from test-and-treat trials. N Engl J Med. 2019;381(3):286–8 This piece serves as a companion to the three TasP studies published in theNew England Journal of Medicine(SEARCH,Ya Tsie, and PopART), and discusses hypotheses for the mixed findings.
Iwuji CC, Orne-Gliemann J, Tanser F, Boyer S, Lessells RJ, Lert F, et al. Evaluation of the impact of immediate versus WHO recommendations-guided antiretroviral therapy initiation on HIV incidence: the ANRS 12249 TasP (treatment as prevention) trial in Hlabisa sub-district, KwaZulu-Natal, South Africa: study protocol for a cluster randomised controlled trial. Trials. 2013;14:230.
Iwuji CC, Orne-Gliemann J, Larmarange J, Okesola N, Tanser F, Thiebaut R, et al. Uptake of home-based HIV testing, linkage to care, and community attitudes about ART in rural KwaZulu-Natal, South Africa: descriptive results from the first phase of the ANRS 12249 TasP cluster-randomised trial. PLoS Med. 2016;13(8):e1002107.
Plazy M, Farouki KE, Iwuji C, Okesola N, Orne-Gliemann J, Larmarange J, et al. Access to HIV care in the context of universal test and treat: challenges within the ANRS 12249 TasP cluster-randomized trial in rural South Africa. J Int AIDS Soc. 2016;19(1):20913.
Gosset A, Protopopescu C, Larmarange J, Orne-Gliemann J, McGrath N, Pillay D, et al. Retention in care trajectories of HIV-positive individuals participating in a universal test-and-treat program in rural South Africa (ANRS 12249 TasP trial). J Acquir Immune Defic Syndr. 2019;80(4):375–85.
Chamie G, Clark TD, Kabami J, Kadede K, Ssemmondo E, Steinfeld R, et al. A hybrid mobile approach for population-wide HIV testing in rural east Africa: an observational study. Lancet HIV. 2016;3(3):e111–9.
Kwarisiima D, Kamya MR, Owaraganise A, Mwangwa F, Byonanebye DM, Ayieko J, et al. High rates of viral suppression in adults and children with high CD4+ counts using a streamlined ART delivery model in the SEARCH trial in rural Uganda and Kenya. J Int AIDS Soc. 2017;20(Suppl 4):21673.
Camlin CS, Akullian A, Neilands TB, Getahun M, Eyul P, Maeri I, et al. Population mobility associated with higher risk sexual behaviour in eastern African communities participating in a Universal Testing and Treatment trial. J Int AIDS Soc. 2018;21(Suppl 4):e25115.
Jain V, Petersen ML, Liegler T, Byonanebye DM, Kwarisiima D, Chamie G, et al. Population levels and geographical distribution of HIV RNA in rural Ugandan and Kenyan communities, including serodiscordant couples: a cross-sectional analysis. Lancet HIV. 2017;4(3):e122–e33.
Gaolathe T, Wirth KE, Holme MP, Makhema J, Moyo S, Chakalisa U, et al. Botswana’s progress toward achieving the 2020 UNAIDS 90-90-90 antiretroviral therapy and virological suppression goals: a population-based survey. Lancet HIV. 2016;3(5):e221–30.
Kebaabetswe P, Manyake K, Kadima E, Auletta-Young C, Chakalisa U, Sekoto T, et al. Barriers and facilitators to linkage to care and ART initiation in the setting of high ART coverage in Botswana. AIDS Care. 2019. https://doi.org/10.1080/09540121.2019.1640843.
Moyo S, Gaseitsiwe S, Mohammed T, Pretorius Holme M, Wang R, Kotokwe KP, et al. Cross-sectional estimates revealed high HIV incidence in Botswana rural communities in the era of successful ART scale-up in 2013-2015. PLoS One. 2018;13(10):e0204840.
Marukutira T, Stoove M, Lockman S, Mills LA, Gaolathe T, Lebelonyane R, et al. A tale of two countries: progress towards UNAIDS 90-90-90 targets in Botswana and Australia. J Int AIDS Soc. 2018;21(3):e25090.
Lasry A, Bachanas P, Suraratdecha C, Alwano MG, Behel S, Pals S, et al. Cost of community-based HIV testing activities to reach saturation in Botswana. AIDS Behav. 2019;23(4):875–82.
Hayes R, Ayles H, Beyers N, Sabapathy K, Floyd S, Shanaube K, et al. HPTN 071 (PopART): rationale and design of a cluster-randomised trial of the population impact of an HIV combination prevention intervention including universal testing and treatment - a study protocol for a cluster randomised trial. Trials. 2014;15:57.
Bock P, Phiri C, Piwowar-Manning E, Kosloff B, Mandla N, Young A, et al. Understanding low sensitivity of community-based HIV rapid testing: experiences from the HPTN 071 (PopART) trial in Zambia and South Africa. J Int AIDS Soc. 2017;20(Suppl 6):21780.
Hayes R, Floyd S, Schaap A, Shanaube K, Bock P, Sabapathy K, et al. A universal testing and treatment intervention to improve HIV control: one-year results from intervention communities in Zambia in the HPTN 071 (PopART) cluster-randomised trial. PLoS Med. 2017;14(5):e1002292.
Shanaube K, Schaap A, Floyd S, Phiri M, Griffith S, Chaila J, et al. What works - reaching universal HIV testing: lessons from HPTN 071 (PopART) trial in Zambia. AIDS. 2017;31(11):1555–64.
Sabapathy K, Mubekapi-Musadaidzwa C, Mulubwa C, Schaap A, Hoddinott G, Stangl A, et al. Predictors of timely linkage-to-ART within universal test and treat in the HPTN 071 (PopART) trial in Zambia and South Africa: findings from a nested case-control study. J Int AIDS Soc. 2017;20(4):e25037.
Iwuji C, Newell ML. Towards control of the global HIV epidemic: addressing the middle-90 challenge in the UNAIDS 90-90-90 target. PLoS Med. 2017;14(5):e1002293.
Bowman AS, Mehta M, Lerebours Nadal L, Halpern M, Nicholas SW, Amesty S. Strengthening the HIV care continuum in the Dominican Republic: application of a triadic implementation framework to meet the UNAIDS 90-90-90 treatment goal. AIDS Patient Care STDs. 2017;31(10):407–12.
Wechsberg WM, Ndirangu JW, Speizer IS, Zule WA, Gumula W, Peasant C, et al. An implementation science protocol of the Women’s Health CoOp in healthcare settings in Cape Town, South Africa: a stepped-wedge design. BMC Womens Health. 2017;17(1):85.
Dorward J, Garrett N, Quame-Amaglo J, Samsunder N, Ngobese H, Ngomane N, et al. Protocol for a randomised controlled implementation trial of point-of-care viral load testing and task shifting: the Simplifying HIV TREAtment and Monitoring (STREAM) study. BMJ Open. 2017;7(9):e017507.
Gamble T, Branson B, Donnell D, Hall HI, King G, Cutler B, et al. Design of the HPTN 065 (TLC-Plus) study: a study to evaluate the feasibility of an enhanced test, link-to-care, plus treat approach for HIV prevention in the United States. Clin Trials. 2017;14(4):322–32.
Jia Z, Mao Y, Zhang F, Ruan Y, Ma Y, Li J, et al. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003-11): a national observational cohort study. Lancet. 2013;382(9899):1195–203.
Meloni ST, Agbaji O, Chang CA, Agaba P, Imade G, Oguche S, et al. The role of point-of-care viral load monitoring in achieving the target of 90% suppression in HIV-infected patients in Nigeria: study protocol for a randomized controlled trial. BMC Infect Dis. 2019;19(1):368.
Walsh FJ, Barnighausen T, Delva W, Fleming Y, Khumalo G, Lejeune CL, et al. Impact of early initiation versus national standard of care of antiretroviral therapy in Swaziland’s public sector health system: study protocol for a stepped-wedge randomized trial. Trials. 2017;18(1):383.
Kerrigan D, Mbwambo J, Likindikoki S, Beckham S, Mwampashi A, Shembilu C, et al. Project Shikamana: baseline findings from a community empowerment–based combination HIV prevention trial among female sex workers in Iringa, Tanzania. J Acquir Immune Defic Syndr. 2017;74:S60–S8.
•• Kerrigan DL, Mbwambo JK, Likindikoki S, et al. Project Shikamana: a community empowerment model of combination prevention significantly impacts HIV incidence and care continuum outcomes among female sex workers in Iringa, Tanzania. J Acquir Immune Defic Syndr. 2019;18(2):141–8 This paper presents the primary findings from the Project Shikamana study implementing TasP with female sex workers in Tanzania.
•• Cowan FM, Davey C, Fearon E, Mushati P, Dirawo J, Chabata S, et al. Targeted combination prevention to support female sex workers in Zimbabwe accessing and adhering to antiretrovirals for treatment and prevention of HIV (SAPPH-IRe): a cluster-randomised trial. Lancet HIV. 2018;5(8):e417–e26 This paper presents the primary findings from the SAPPH-Ire study implementing TasP with female sex workers in Zimbabwe.
Mlambo CK, Vernooij E, Geut R, Vrolings E, Shongwe B, Jiwan S, et al. Experiences from a community advisory Board in the Implementation of early access to ART for all in Eswatini: a qualitative study. BMC Med Ethics. 2019;20(1):50.
Pell C, Vernooij E, Masilela N, Simelane N, Shabalala F, Reis R. False starts in ‘test and start’: a qualitative study of reasons for delayed antiretroviral therapy in Swaziland. Int Health. 2018;10(2):78–83.
Shabalala FS, Vernooij E, Pell C, Simelane N, Masilela N, Spiegelman D, et al. Understanding reasons for discontinued antiretroviral treatment among clients in test and treat: a qualitative study in Swaziland. J Int AIDS Soc. 2018;21(S4):e25120.
Dlamini-Simelane T, Moyer E. Task shifting or shifting care practices? The impact of task shifting on patients’ experiences and health care arrangements in Swaziland. BMC Health Serv Res. 2017;17(1):20.
Khan S, Spiegelman D, Walsh F, et al. Universal test and treat (UTT) versus standard of care for access to antiretroviral therapy in HIV clients: the MaxART stepped-wedge randomized controlled health systems trial in Swaziland. Paper presented at: The International AIDS Society. 2018; Amsterdam, Netherlands.
Hendrickson ZM, Leddy AM, Galai N, Mbwambo JK, Likindikoki S, Kerrigan DL. Work-related mobility and experiences of gender-based violence among female sex workers in Iringa, Tanzania: a cross-sectional analysis of baseline data from Project Shikamana. BMJ Open. 2018;8(9):e022621.
Leddy AM, Mantsios A, Davis W, Muraleetharan O, Shembilu C, Mwampashi A, et al. Essential elements of a community empowerment approach to HIV prevention among female sex workers engaged in project Shikamana in Iringa, Tanzania. Cult Health Sex. 2019. https://doi.org/10.1080/13691058.2019.1659999.
Busza J, Chiyaka T, Musemburi S, Fearon E, Davey C, Chabata S, et al. Enhancing national prevention and treatment services for sex workers in Zimbabwe: a process evaluation of the SAPPH-IRe trial. Health Policy Plan. 2019;34(5):337–45.
Larmarange J. The edges of key populations: how to think, desribe and reach these hidden groups? AIDS impact; 07/30/2019; London, England.
Labhardt ND, Ringera I, Lejone TI, Klimkait T, Muhairwe J, Amstutz A, et al. Effect of offering same-day ART vs usual health facility referral during home-based HIV testing on linkage to care and viral suppression among adults with HIV in Lesotho: the CASCADE randomized clinical trial. JAMA. 2018;319(11):1103–12.
Hargreaves JR, Krishnaratne S, Mathema H, Lilleston PS, Sievwright K, Mandla N, et al. Individual and community-level risk factors for HIV stigma in 21 Zambian and south African communities: analysis of data from the HPTN071 (PopART) study. AIDS. 2018;32(6):783–93.
Seeley J, Bond V, Yang B, Floyd S, MacLeod D, Viljoen L, et al. Understanding the time needed to link to care and start ART in seven HPTN 071 (PopART) study communities in Zambia and South Africa. AIDS Behav. 2019;23(4):929–46.
Bond V, Nomsenge S, Mwamba M, Ziba D, Birch A, Mubekapi-Musadaidzwa C, et al. “Being seen” at the clinic: Zambian and South African health worker reflections on the relationship between health facility spatial organisation and items and HIV stigma in 21 health facilities, the HPTN 071 (PopART) study. Health Place. 2019;55:87–99.
McKinnon LR, Liebenberg LJ, Yende-Zuma N, Archary D, Ngcapu S, Sivro A, et al. Genital inflammation undermines the effectiveness of tenofovir gel in preventing HIV acquisition in women. Nat Med. 2018;24(4):491–6.
Granich R, Williams BG. Treatment as prevention trials and ending AIDS: what do we know, when did we know it, and what do we do now? Curr Opin HIV AIDS. 2019;14(6):514–20.
Cori A, Ayles H, Beyers N, Schaap A, Floyd S, Sabapathy K, et al. HPTN 071 (PopART): a cluster-randomized trial of the population impact of an HIV combination prevention intervention including universal testing and treatment: mathematical model. PLoS One. 2014;9(1):e84511.
Estill J, Marsh K, Autenrieth C, Ford N. How to achieve the global 90-90-90 target by 2020 in sub-Saharan Africa? A mathematical modelling study. Tropical Med Int Health. 2018;23(11):1223–30.
Fauci AS, Eisinger RW. PEPFAR - 15 years and counting the lives saved. N Engl J Med. 2018;378(4):314–6.
Goosby E, Von Zinkernagel D, Holmes C, Haroz D, Walsh T. Raising the bar: PEPFAR and new paradigms for global health. J Acquir Immune Defic Syndr. 2012;60(Suppl 3):S158–62.
Heaton LM, Bouey PD, Fu J, Stover J, Fowler TB, Lyerla R, et al. Estimating the impact of the US President’s emergency plan for AIDS relief on HIV treatment and prevention programmes in Africa. Sex Transm Infect. 2015;91(8):615–20.
Sturchio JL, Cohen GM. How PEPFAR’s public-private partnerships achieved ambitious goals, from improving labs to strengthening supply chains. Health Aff (Millwood). 2012;31(7):1450–8.
Webster P. PEPFAR at 15 years. Lancet. 2018;392(10143):200.
Funding
The authors of this study are supported by National Institutes of Health grants K12HS023000 (MAB), R01AI112339 (DS, SHV), P30MH062294 (MAB, SHV), and UM1AI068619 (SHV).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Treatment as Prevention
Rights and permissions
About this article
Cite this article
Brault, M.A., Spiegelman, D., Abdool Karim, S.S. et al. Integrating and Interpreting Findings from the Latest Treatment as Prevention Trials. Curr HIV/AIDS Rep 17, 249–258 (2020). https://doi.org/10.1007/s11904-020-00492-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-020-00492-4