Abstract
Purpose of review
Optimal control of HIV can be achieved by early diagnosis followed by the initiation of antiretroviral therapy (ART). Two large randomised trials (TEMPRANO and START) have recently been published documenting the clinical benefits to HIV-positive adults of early ART initiation. Main findings are reviewed with a focus on serious non-AIDS (SNA) conditions.
Recent findings
Data from the two trials demonstrated that initiating ART early in the course of HIV infection resulted in marked reductions in the risk of opportunistic diseases and invasive bacterial infections. This indicates that HIV causes immune impairment in early infection that is remedied by controlling viral replication. Intriguingly, in START, a marked reduction in risk of cancers, both infection-related and unrelated types of cancers, was observed. Like the findings for opportunistic infections, this anti-cancer effect of early ART shows how the immune system influences important pro-oncogenic processes. In START, there was also some evidence suggesting that early ART initiation preserved kidney function, although the clinical consequence of this remains unclear. Conversely, while no adverse effects were evident, the trials did not demonstrate a clear effect on metabolic-related disease outcomes, pulmonary disease, or neurocognitive function.
Summary
HIV causes immune impairment soon after acquisition of infection. ART reverses this harm at least partially. The biological nature of the immune impairment needs further elucidation, as well as mechanisms and clinical impact of innate immune activation. Based on the findings from TEMPRANO and START, and because ART lowers the risk of onward transmission, ART initiation should be offered to all persons following their diagnosis of HIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
By starting antiretroviral therapy (ART) early in the course of HIV infection, severe immune impairment is avoided. However, the evidence base to support use of life-long ART in persons with early HIV infection was only definitively established in 2015. During the 15 years prior to this, when ART initiation was still deferred to substantially lower CD4+ lymphocyte counts, there were substantial and sustained improvements in survival [1•]. Not only was the risk of opportunistic disease declining as CD4 count among treated persons continued to increase, but, intriguingly, the risk of cardiovascular disease and liver disease was also declining. This improvement was explained by better clinical care. This included continuous use of ART, in the aftermath of the completion of the Strategies for Management of Antiretroviral Therapy (SMART) study in 2006 [2].
The SMART study documented that continuous control of viral replication resulting in higher counts of CD4+ lymphocytes (as opposed to using ART intermittently) reduced risk not only of opportunistic infections but also of a composite outcome of non-AIDS-defining end-organ diseases and cancers—collectively labelled serious non-AIDS (SNA) conditions [3]; definitions are available in [4]. In addition to the traditional risk factors for these events, lower CD4+ lymphocyte counts [3, 5,6,7] and a higher state of ongoing inflammation and coagulation system activation (as reflected in elevated interleukin-6 and D-dimer levels) [8••] after achieving virologic suppression with ART were risk factors.
Based on the findings from SMART, it was important to determine whether risk of SNA conditions could be reduced by starting ART in early HIV infection. If early ART did reduce this risk, it would not only have clinical importance but it would also enhance our understanding of HIV pathogenesis and open up new avenues of research (Tables 1 and 2).
Approaches to Define the Benefit to Risk Ratio of Early ART Initiation
Many observational studies have attempted to address this question [9,10,11,12,13]. The latest of these reports (from the HIV Cohorts Analysed Using Structural Approaches to Longitudinal data [HIV-CAUSAL] Collaboration [13•]) which used optimal methods to adjust for baseline and time-dependent confounders predicted the survival benefit from earlier use of ART in the range of 3 to 20% [13•]. Being an observational study, the underlying assumption was that there was no unmeasured confounder that could have influenced the decision to start ART. Deferral of ART was the usual standard of care in the cohorts contributing to the reports [9,10,11,12, 13•].
An informed decision on whether to initiate ART in early HIV infection requires, like when starting any type of medical interventions, that the benefit from starting the treatment outweighs the potential harm from doing so [14, 15]. The observational studies cited above [9,10,11,12, 13•] focused on risk of death and AIDS, as these outcomes are fairly reliably ascertained in cohort studies. Non-fatal SNA outcomes were not considered. However, pathologies contributing to death are diverse, and their relative contribution may be affected differentially by earlier ART initiation. The ratio of AIDS to non-AIDS conditions contributing to death is substantially higher in those dying with low CD4+ lymphocyte count, than would be expected if ART was started earlier in the course of HIV infection. Since non-AIDS causes of death could be adversely influenced by early ART and since non-fatal adverse events that impact quality of life could also be greater with early ART, it was important to expand evaluations of early ART to include these outcomes. Among those with early HIV, event rates were expected to be low and the effects of early ART modest. Therefore, it was critical to assess the risks and benefits of early ART in large randomised trials in which bias due to confounding could be eliminated and risks and benefits could be reliably measured. Results from these two trials were reported in 2015 [16••, 17••]. Given the clear benefit of early ART initiation, it is unlikely that additional trials will be undertaken in the future.
TEMPRANO [16••]
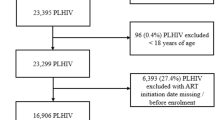
TEMPRANO was a trial, using a two-by-two factorial design, to address whether earlier ART and initiation of isoniazid primary chemoprophylaxis would reduce a composite clinical endpoint that included AIDS events, non-AIDS-defining cancer, non-AIDS-defining invasive bacterial disease, and death from any cause [16••]. TEMPRANO was conducted by the French ANRS (National Agency for AIDS Research) in the Ivory Coast (2056 participants were enrolled). The most frequently occurring primary endpoints were tuberculosis and invasive bacterial infections. In the arm randomised to deferred ART, the CD4+ lymphocyte threshold for initiation changed during the trial, reflecting changes in the WHO recommendations from starting at 200 and later on 350 and 500 cells/μL. Earlier ART was found to reduce the clinical events risk by 44%. As the number of SNA conditions were low, it was not possible to assess possible benefit from earlier ART initiation on these outcomes.
The Strategic Timing of Antiretroviral Treatment (START) Trial [17••]
START was conducted in 35 countries on 5 continents and enrolled 4685 ART naïve participants of whom 54% received care in low- and middle-income countries [17••]. All had a CD4+ lymphocyte count at enrolment above 500 cells/μL (20% above 800) and without prior AIDS. The broad geographical representation was by design to ensure generalizable conclusions [18]. The design was a simple comparison of risk of a major clinical endpoint from immediate versus deferred ART initiation (when CD4+ lymphocyte count had decreased to 350 cells/μL; the observed count just before starting was 440) [19]. The primary endpoint was a composite of fatal and non-fatal AIDS and SNA events. Following from the results of SMART [2], non-fatal SNA events considered major cardiovascular, liver and renal clinical events and non-AIDS-defining cancers. Several secondary outcomes were defined to further understand the potential benefits and risks of early ART. Based on pre-specified monitoring guidelines, the Data and Safety Monitoring Board for START determined that early ART was superior to deferred ART before the planned completion date. Overall, there was 57% reduction in the primary endpoint in favour of earlier ART initiation. In addition, for each of the two major components of the composite primary endpoint, AIDS and non-AIDS, early ART was superior to deferred ART (72 and 39% reductions with early ART, respectively). The benefit was consistent in all subgroups examined (demographics, HIV-related factors, underlying CV risk, i.e. no statistically significant interaction). In models that assumed that all the trial participants adhered to the protocol, the proportion developing the primary endpoint 5 years into the trial was projected to be 3.2% in the immediate arm and 7% in the deferred arm [20•]. The absolute risk reduction (which takes into account varying underlying risk of the various outcomes) in favour of earlier ART initiation was more marked for older persons (primarily driven by higher risk of SNA conditions), and those with more perturbed HIV infection (higher viral load and low CD4:CD8 ratio) [21]. Consistent with the observed clinical benefit, the general health quality of life estimate increased in the arm initiating ART immediately [22].
When ART is initiated in late stages of HIV infection, increasing CD4+ lymphocyte counts is usually projected as a suitable surrogate of benefit. However, preliminary analyses only estimate that 15% of the benefit from earlier ART initiation in the START trial was explained by improvement of this immune marker [23•]. Higher follow-up levels of the CD4:CD8 ratio with early as compared to deferred ART explained more of the benefit.
Opportunistic Infections
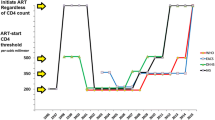
In HIV, the risk of opportunistic infections, also in early HIV infection, can fairly reliably be predicted by the combination of the CD4+ lymphocyte count and the HIV-RNA viral load [24]. Both TEMPRANO and START confirmed these observations. A post hoc analysis in START, expanding on the types of bacterial infections included in the endpoint yielded consistent reduction of invasive bacterial infection risk (61%) [25•] to that observed in the TEMPRANO trial [16••] (Fig. 1). For this particular outcome, increasing CD4+ lymphocyte counts explained most of the benefit from earlier initiation of ART.
Effect of early versus deferred antiretroviral therapy initiation on clinical outcomes. a All-cause deaths. b AIDS-defining events. c Cancer: AIDS and non-AIDS; infection-related and unrelated. d Invasive bacterial infections. *See O’Connor [25•] and TEMPRANO ANRS 12136 Study group [16••] (supplementary material) for the list of events classified as serious/invasive bacterial infections. e Tuberculosis. f Cardiovascular disease. *Cardiovascular disease was defined as myocardial infarction, stroke, or coronary revascularization, in START and as stroke, pulmonary embolism, dilated myocardiopathy, or deep vein thrombosis, in TEMPRANO
Cancer
A number of pro-oncogenic infections, including Epstein-Barr virus (EBV), Kaposi’s sarcoma-associated herpesvirus (human herpes virus 8) and Human Papilloma Virus (HPV), replicate better and thereby exert their oncogenic potential in patients with impaired T-lymphocyte function. Given the findings relating to opportunistic infection cited above, it is therefore not surprising that the risk of infection-related cancers, in particular, non-Hodgkin lymphoma and Kaposi sarcoma, was reduced by earlier ART initiation in START [26•] (Fig. 1). A similar benefit was also observed for infection-unrelated cancers albeit to a smaller extent. These analyses did not show that increasing CD4+ lymphocyte count was readily explaining the clinical benefit, implying a more complex interaction in how immune function affects oncogenesis. Other studies have also found a CD4+ lymphocyte gradient of risk between both types of malignancies [27]. It is plausible that earlier ART only affects de novo oncogenic transformation and not transformations already having occurred prior to initiation of ART. Consistent with this hypothesis, the benefit from earlier initiation of ART on cancer risk only became apparent approximately 12 months into the study, whereas the benefit on opportunistic infections occurred within 2–3 months [17••, 25•, 26•]. With respect to lymphoma, an EBV-related malignancy, other mechanisms by which early ART initiation may have reduced risk include a shift to a less oncogenic EBV latency pattern [28, 29] and interference with HIV-associated lymphomagenesis [29,30,31].
Cardiovascular Disease
Traditional as well as ART-related risk factors affect risk of cardiovascular disease in HIV [32•]. Inflammatory and coagulation markers (such as interleukin-6 and D-dimer) are associated with an increased risk of HIV-related cardiovascular disease [33] and all-cause mortality [34], and these markers were lowered by ART seen in both the SMART [35] and START [36] studies. Also, ART initiation increases levels of HDL cholesterol [37•] and, as a consequence, may lower cardiovascular disease risk. The number of cardiovascular endpoints in START and TEMPRANO were too small to draw any definitive conclusions about whether early ART affects clinical CVD outcomes (Fig. 1). In part, this reflects the young age groups enrolled in these two studied, and, in part, it reflects the short follow-up. Both trials [37•, 38•] have reported changes in traditional risk factors during follow-up, but differences between the treatment groups were small and inconsistent for the risk factors considered. In a substudy embedded in START, Baker and colleagues recently reported comparable changes in arterial elasticity between the early and deferred ART groups [39•]. These data indicate that earlier ART, despite lowering inflammatory markers and increasing HDL-cholesterol, does not differ from deferred ART in measures of small and large artery elasticity over 2–4 years of follow-up. A longer-term follow-up of the START study participants will be informative with regard to risk of cardiovascular disease outcomes.
Kidney Function
Lower kidney function renders HIV+ persons at excess risk of terminal kidney failure [40] and increased risk of cardiovascular disease [41]. HIV directly induces impairment of kidney function, in particular in persons carrying host genetic traits rendering them susceptible (seen more frequently in persons of black race) [42]. Conversely, several antiretroviral drugs adversely affect the organ [43•, 44], in particular if the underlying risk of chronic kidney disease is high [44]. In START, there was a modest improvement in estimated glomerular filtration rate in those starting ART earlier, in particular in persons of black race [45]. Long-term START follow-up will also be informative to better define this.
Pulmonary Function
Studies of longitudinal lung function are sparse in HIV. Given the high prevalence of smoking and potential adverse consequences on bronchial and lung structures from uncontrolled HIV-related inflammation in this body compartment, there is an unmet need to improve this knowledge gap. Kunisaki and colleagues conducted a large substudy (1026 participants) in START assessing lung function at study entry [46] and follow-up [47••]. At entry, there was a 7% prevalence of chronic obstructive pulmonary disease, associated with smoking and older age. Over follow-up, a more marked decline in lung function was seen in smokers as expected (approximately 30 vs 25 mL/year decline in FEV1), but earlier ART did not affect this outcome irrespective of smoking status. Therefore, the timing of ART initiation had no major short-term effect (positive or negative) on rate of lung function decline in HIV-positive individuals who are naive to ART, with CD4 T cell counts of more than 500/μL [47••].
Bone Mineral Density
ART initiation is known to deplete bone mineral density in the first year of treatment [48], likely by reducing bone turnover seen in untreated HIV [48]. This detrimental effect is of unknown clinical significance and is not clearly associated with use of particular antiretroviral drugs. In START, Hoy and colleagues conducted a substudy with serial bone mineral density measurements [49•]. Consistent with findings from other studies, initiation of ART lead to a small (1.9–2.5%) but significant reduction on bone mineral density of the hip and spine. Conversely, recently published observational data suggest that tenofovir DF—but not other antiretroviral drugs—may be associated with excess risk of bone fractures in older persons using the drug for extended periods of time [50]. The possible clinical impact from replacing tenofovir DF with other drugs remains to be clarified.
Neurocognitive Function
Prior studies suggest improvement of neurocognitive function after initiation of ART [51], also in early HIV disease. Wright, Price and colleagues conducted a substudy among 600 participants in START [52] to test whether indeed earlier as opposed to later initiation of ART led to such effect. Consistent with earlier studies, preliminary data from this substudy did show that neurocognitive function improved in the group randomised to immediate initiation of ART. However, an improvement of similar magnitude was also observed in the group randomised to deferred ART and while most remained of ART in that group. The improvement, hence, is derived from the methodology of assessing neurocognitive function (learning effect) and not from early ART use per se.
HIV Transmission Benefit
Suppression of HIV replication—by use of ART—reduces the risk of perinatal and sexual [53••, 54••] transmission. If HIV RNA levels are durably suppressed, the risk of transmission appears negligible. This societal benefit requires that the person on ART also benefit from using this intervention—this precondition is met for all HIV+ persons irrespective of stage of their HIV infection, as per data reviewed above. TEMPRANO researchers modelled data from that trial to assess which level of risk compensation would off-set using ART in all HIV+ persons to limit transmission, and found that only extreme scenarios would do so [55]. To fully exploit this, it is however required that all HIV+ persons are diagnosed and placed and maintained on ART for life. Otherwise, those with ongoing HIV replication will continue to be source of new infections. In 2017, UNAIDS estimates that one in ten on average of the 20 million HIV+ persons still not on ART transmitted HIV in 2015. Additional preventive tools, including pre-exposure prophylaxis, are likely needed to further contain HIV transmission.
Conclusions
The question of when to start ART in the course of HIV infection has been resolved. This effective intervention should be initiated as soon as possible after the diagnosis of HIV, as it reduces the risk of opportunistic infections, cancers and onward transmission of HIV. By combining these benefits (some of them of benefit to the individual and others to public health), the numbers needed to treat for one of these events to be avoided is less than 10. This is mainly driven by reduced transmission risk. As for the clinical benefit to the individual HIV+ persons, risk for disease progression is small without ART, while the CD4+ lymphocyte count remains high. The numbers needed to treat for one to benefit clinically is therefore larger, and mainly affected by older age, higher HIV-RNA viral load and lower CD4:CD8 ratio. A compelling argument for earlier initiation of ART is that the ART-preventable diseases are severe in nature and develop in an unpredictable way.
There are areas of HIV infection where the evidence base for earlier ART initiation is less clear, in particular during acute infection and in chronically infected persons with low HIV replication [56•]. This conundrum is mainly due to the fact, that the randomised controlled trials were unable to specifically address the potential clinical benefit from using ART in these scenarios, as the number of patients from these subgroups enrolled was low. Other trials are also not conclusive [57, 58]. In TEMPRANO and START, there was no evidence that benefit varied by duration of infection or levels of HIV viral load at entry [16••, 17••]. As such, the available data do not suggest that benefit (in relative terms) would be different irrespective of HIV stage. In support of this, cellular and soluble biomarkers suggest benefit across these subgroups. Despite this, the uncertainty—especially in relation to those with low untreated HIV RNA levels—calls for individualising the decision on when to commence ART for these individuals.
Given the clarification on when to start ART provided by the evidence summarised here, there remain several challenges for the HIV medicine community to resolve. HIV contributes to the inflammatory state of HIV+ persons which predicts clinical outcome, and ART reduces this state to some extent and has broad clinical benefit. However, it remains unsolved whether adjunctive therapy with other anti-inflammatory medical intervention is of additional clinical benefit among those on ART with ongoing inflammation. ART reduces the risk of opportunistic infections and cancers; with a system biology characterisation (including microbiota and host genetics) of large cohorts [59, 60], it may be possible to further delineate the mechanisms by which ART prevents these conditions from emerging. Finally, organ-specific SNA conditions develop as part of a complex pathological process and involves multiple risk factors (both demographic, behavioural, host genetic and HIV-specific). Of the potentially modifiable processes, it would be of interest to understand which are most influential and hence should be the targets for prevention.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, Reiss P, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014;384(9939):241–8. International cohort collaboration demonstrating marked reduction in last 15 years in fatal AIDS and SNA-related events incl those caused by cardiovascular and liver pathologies but not non-AIDS cancers. Whereas reduction in AIDS conditions were associated with gradually increasing CD4+ lymphocyte count, this was not the case for the SNA conditions, but perhaps better quality of care .
The Strategies for Management of Antiretroviral Therapy (SMART) Study Group, El-Sadr WM, Lundgren J, Neaton JD, Gordin F, Abrams D, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–96.
Phillips AN, Neaton J, Lundgren JD. The role of HIV in serious diseases other than AIDS. AIDS. 2008;22(18):2409–18.
Lifson AR, Belloso WH, Davey RT, Duprez D, Gatell JM, Hoy JF, et al. Development of diagnostic criteria for serious non-AIDS events in HIV clinical trials. HIV Clin Trials. 2010;11(4):205–19.
May MT, Vehreschild J, Trickey A, Obel N, Reiss P, Bonnet F, et al. Mortality according to CD4 count at start of combination antiretroviral therapy among HIV-infected patient followed for up to 15 years after start of treatment: collaborative cohort study. Clin Infect Dis. 2016;62:1571–7.
Baker JV, Peng G, Rapkin J, Krason D, Reilly C, Cavert WP, et al. Poor initial CD4+ recovery with antiretroviral therapy prolongs immune depletion and increases risk for AIDS and non-AIDS diseases. J Acquir Immune Defic Syndr. 2008;48:541–6.
Achhra AC, Amin J, Law MG, Emery S, Gerstoft J, Gordin FM, et al. Immunodeficiency and the risk of serious clinical endpoints in a well studied cohort of treated HIV-infected patients. AIDS. 2010;24(12):1877–86.
•• Grund B, Baker JV, Deeks SG, et al. Relevance of interleukin-6 and D-dimer for serious non-AIDS morbidity and death among HIV-positive adults on suppressive antiretroviral therapy. PLoS One. 2016;11:e0155100. Combined cohort analysis demonstrating persisting prognostic impact from initial levels of interleukin-& and D-dimer. These observations were confirmed in the START cohort (Baker JV, Sharma S, Grund B, et al. Association of inflammation and coagulation with clinical risk in the START Trial. Abstract, Conference on Retroviruses and Opportunistic Infections (CROI), Seattle, Washington, 2017) .
Kitahata MM, Gange SJ, Abraham AG, Merriman B, Saag MS, Justice AC, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–26.
Sterne JA, May M, Costagliola D, de Wolf F, Phillips AN, Harris R, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1 infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373:1352–63.
CASCADE Collaboration, Jonsson M, Fusco JS, Cole SR, Thomas JC, Porter K, et al. Timing of HAART initiation and clinical outcomes in human immunodeficiency virus type 1 seroconverters. Arch Intern Med. 2011;171:1560–9.
Cain LE, Logan R, Robins JM, Sterne JA, Sabin C, Bansi L, et al. When to initiate combined antiretroviral therapy to reduce mortality and AIDS-defining illness in HIV-infected persons in developed countries: an observational study. Ann Intern Med. 2011;154:509–15.
• The HIV-Causal Collaboration, Lodi S, Phillips A, Logan R, Olson A, Costagliola D, et al. Comparative effectiveness of immediate antiretroviral therapy versus CD4-based initiation in HIV-positive individuals in high-income countries: observational cohort study. Lancet HIV. 2015;2:e335-e-345. Most recent report to address whether statistical analysis of observational studies can predict the benefit from earlier initiation of ART. The predicted benefit (3–20%) was smaller than what was observed in the START study .
Lane HC, Neaton JD. When to start therapy for HIV infection: a swinging pendulum in search of data. Ann Intern Med. 2003;138(8):680–1.
Lundgren JD, Babiker AG, Gordin FM, et al. When to start antiretroviral therapy: the need for an evidence base during early HIV infection. BMC Med. 2013;11:148.
•• TEMPRANO ANRS 12136 Study Group, Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–22. Single country (Ivory Coast) randomised controlled trial demonstrating clinical benefit from starting ART earlier rather than later in course of early HIV infection. Benefit was due to reduced risk of tuberculosis and invasive bacterial infections (44% reduction) .
•• The INSIGHT START Study Group, Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373:795–807. Large, geographical diverse randomised controlled trial demonstrating clinical benefit from starting ART earlier rather than later in course of early HIV infection. Benefit was due to reduced risk of opportunistic infections and cancer (57%) .
INSIGHT Strategic Timing of AntiRetroviral Treatment (START) Study Group, Lundgren J, Babiker A, Gordin F, Emery S, Fätkenheuer G, et al. Why START? Reflections that led to the conduct of this large long-term strategic HIV trial. HIV Med. 2015;16(Suppl 1):1–9. https://doi.org/10.1111/hiv.12227.
Babiker AG, Emery S, Fätkenheuer G, et al. Considerations in the rationale, design and methods of the Strategic Timing of AntiRetroviral Treatment (START) study. Clin Trials. 2013;10(1 Suppl):S5–S36.
• Lodi S, Sharma S, Lundgren JD, Phillips AN, Cole SR, Logan R, et al. The per-protocol effect of immediate versus deferred antiretroviral therapy initiation. AIDS. 2016;30(17):2659–63. Analysis of the START cohort with aim to assess the benefit from earlier ART if all had all the trial participants adhered to the protocol. The ITT effect estimate (as reported in the N Engl J Med main article) may underestimate the benefit of immediate ART initiation by 23%.
Molina JM, Grund B, Gordin F, et al. Who benefited most from immediate treatment in START? A subgroup analysis. Abstract THAB0201, AIDS 2016, Durban, South Africa; 2016.
Lifson AR, Grund B, Gardner EM, Kaplan R, Denning E, Engen N, et al. Improved quality of life with immediate versus deferred initiation of antiretroviral therapy in early asymptomatic HIV infection. AIDS. 2017;31(7):953–63.
• Babiker A, Grund B, Sharma S, et al. The role of HIV RNA and T cell counts, percent and ratio in explaining the benefit of immediate ART initiation in HIV+ individuals with high CD4+ counts. Abstract, AIDS 2016, Durban, South Africa; 2016. Analysis of the START study focusing on which immunological parameters could explain benefit from earlier ART initiation. Whereas changes in absolute CD4 count over follow-up only explained a small fraction of benefit (15%), changes in the CD4:CD8 ratio was a better predictor (45%).
Mocroft A, Furrer HJ, Miro JM, Reiss P, Mussini C, Kirk O, et al. The incidence of AIDS-defining illnesses at a current CD4 count ≥ 200 cells/μL in the post-combination antiretroviral therapy era. Clin Infect Dis. 2013;57(7):1038–47.
• O'Connor J, Vjecha MJ, Phillips AN, Angus B, Cooper D, Grinsztejn B, et al. Effect of immediate initiation of antiretroviral therapy on risk of severe bacterial infections in HIV-positive people with CD4 cell counts of more than 500 cells per μL: secondary outcome results from a randomised controlled trial. Lancet HIV. 2017;4(3):e105–12. Analysis in START cohort of how earlier ART reduced substantially (61%) the risk of contracting a composite endpoint of severe bacterial infection (including bacterial pneumonia, pulmonary or extrapulmonary tuberculosis, or any bacterial infectious disorder of grade 4 severity, that required unscheduled hospital admissions, or caused death). This benefit was partially explained by how earlier ART increased CD4+ lymphocyte count.
• Borges AH, Neuhaus J, Babiker AG, et al. Immediate antiretroviral therapy reduces risk of infection-related cancer during early HIV infection. Clin Infect Dis. 2016;63:1668–76. Detailed analysis of cancer emerging in the START cohort, and how earlier initiation of ART reduced risk of both infectious-related and un-related types of cancers. Intriguingly, adjusted for time-updated HIV-RNA levels (but not CD4+ count) attenuated the observed benefit from earlier initiation of ART, but this effect was not observed for infectious-related, suggesting that the anti-cancer benefit from earlier ART initiation is not solely attributable to suppression of HIV replication.
Reekie J, Kosa C, Engsig F, Monforte AD, Wiercinska-Drapalo A, Domingo P, et al. Relationship between current level of immunodeficiency and non-acquired immunodeficiency syndrome-defining malignancies. Cancer. 2010;116(22):5306–15.
Kersten MJ, Van Gorp J, Pals ST, Boon F, Van Oers MH. Expression of Epstein-Barr virus latent genes and adhesion molecules in AIDS-related non-Hodgkin’s lymphomas: correlation with histology and CD4-cell number. Leuk Lymphoma. 1998;30(5–6):515–24.
Arvey A, Ojesina AI, Pedamallu CS, Ballon G, Jung J, Duke F, et al. The tumor virus landscape of AIDS-related lymphomas. Blood. 2015;125(20):e14–22.
Mazzuca P, Marsico S, Schulze K, Mitola S, Pils MC, Giagulli C, Guzman CA, Caruso A, Caccuri F. Role of Autophagy in HIV-1 Matrix Protein p17-Driven Lymphangiogenesis. J Virol. 2017;91(16). https://doi.org/10.1128/JVI.00801-17.
Borges ÁH. Combination antiretroviral therapy and cancer risk. Curr Opin HIV AIDS. 2017;12(1):12–9.
• Friis-Møller N, Ryom L, Smith C, Weber R, Reiss P, Dabis F, et al. An updated prediction model of the global risk of cardiovascular disease in HIV-positive persons: the dData-collection on Adverse Effects of Anti-HIV Drugs (D:A:D) study. Eur J Prev Cardiol. 2016;23(2):214–23. Updated version of the D:A:D study predictor of absolute underlying risk of cardiovascular disease in HIV+ populations. This and risk prediction tools for chronic kidney disease are available for online use at http://www.chip.dk/Tools .
Duprez DA, Neuhaus J, Kuller LH, Tracy R, Belloso W, De Wit S, et al. Inflammation, coagulation and cardiovascular disease in HIV-infected individuals. PLoS One. 2012;7(9):e44454. https://doi.org/10.1371/journal.pone.0044454.
Kuller LH, Tracy R, Belloso W, Wit SD, Drummond F, Lane HC, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203.
Baker JV, Neuhaus J, Duprez D, et al. Changes in inflammatory and coagulation biomarkers: a randomized comparison of immediate versus deferred antiretroviral therapy in patients with HIV infection. J Acquir Immune Defic Syndr. 2011;56:36–43.
Baker JV, Sharma S, Grund B, Rupert A, Metcalf JA, Schechter M, et al.Systemic Inflammation, Coagulation, and Clinical Risk in the START Trial. Open Forum Infect Dis. 2017;4(4):ofx262. http://www.ncbi.nlm.nih.gov/pubmed/29308409
• Baker JV, Sharma S, Achhra AC, Bernardino JI, Bogner JR, Duprez D, et al. Changes in cardiovascular disease risk factors with immediate versus deferred antiretroviral therapy initiation among HIV-positive participants in the START (Strategic Timing of Antiretroviral Treatment) Trial. J Am Heart Assoc. 2017;6(5). Analysis in START cohort of how earlier ART initiation impact traditional cardiovascular risk factors, iincluding worsening dyslipidaemia (in part depending on type of antiretroviral drug used), but decreased use of blood pressure medications, leading to an overall projected clinically insignificant impact on cardiovascular risk. Risk of new onset diabetes was not affected.
• Ghehi C, Gabillard D, Moh R, Badje A, Kouamé GM, Oouttara E, et al. High correlation between Framingham equations with BMI and with lipids to estimate cardiovascular risks score at baseline in HIV-infected adults in the Temprano trial, ANRS 12136 in Côte d’Ivoire. PLoS One. 2017;12(6):e0177440. Analysis of the TEMPRANO study using the Framingham equation, assessing temporal trends during follow-up and between the two randomised arms of the trial. No effect of earlier ART initiation affected this outcome.
• Baker JV, Hullsiek KH, Engen NW, Nelson R, Chetchotisakd P, Gerstoft J, et al. Early antiretroviral therapy at high CD4 counts does not improve arterial elasticity: a substudy of the Strategic Timing of AntiRetroviral Treatment (START) Trial. Open Forum Infect Dis. 2016;3(4):ofw213. Substudy in START assessing whether earlier ART affects changes in arterial elasticity (a marker of arterial wall disease which in general population studies are closely linked with risk of cardiovascular disease). No benefit from earlier ART was observed in this study.
Trullas JC, Mocroft A, Cofan F, Tourret J, Moreno A, Bagnis CI, et al. Dialysis and renal transplantation in HIV-infected patients: a European survey. J Acquir Immune Defic Syndr. 2010;55(5):582–9.
Ryom L, Lundgren JD, Ross M, Kirk O, Law M, Morlat P, et al. Renal impairment and cardiovascular disease in HIV-positive individuals: the D:A:D study. J Infect Dis. 2016;214(8):1212–20.
Parsa A, Kao L, Xie D, et al. APOL1 risk variants, race, and progression of chronic kidney disease. N Engl J Med. 2013;369:2183–96.
• Mocroft A, Lundgren JD, Ross M, Fux CA, Reiss P, Moranne O, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3(1):e23–32. International cohort study demonstrating dose-response association between duration of tenofovir disoproxil fumarate, ritonavir-boosted atazanavir, or ritonavir-boosted lopinavir usage and gradually increasing risk of developing chronic kidney disease. This finding did in relative terms not interact with patients underlying risk of contracting this outcome, implying that this complication is relatively common in those with elevated predicted underlying risk (i.e. a low number needed to harm).
Mocroft A, Lundgren J, Ross M, Law M, Reiss P, Kirk O, et al. Development and validation of a risk score for chronic kidney disease in HIV infection using prospective cohort data from the D:A:D study. PLoS Med. 2015;12:e1001809.
Achhra AC, Mocroft A, Ross M, Ryom-Nielson L, Avihingsanon A, Bakowska E, et al. Impact of early versus deferred antiretroviral therapy on estimated glomerular filtration rate in HIV-positive individuals in the START trial. Int J Antimicrob Agents. 2017.
Kunisaki KM, Niewoehner DE, Collins G, Nixon DE, Tedaldi E, Akolo C, et al. Pulmonary function in an international sample of HIV-positive, treatment-naïve adults with CD4 counts > 500 cells/μL: a substudy of the INSIGHT Strategic Timing of AntiRetroviral Treatment (START) trial. HIV Med. 2015;16(Suppl 1):119–28.
•• Kunisaki KM, Niewoehner DE, Collins G, Aagaard B, Atako NB, Bakowska E, et al. Pulmonary effects of immediate versus deferred antiretroviral therapy in HIV-positive individuals: a nested substudy within the multicentre, international, randomised, controlled Strategic Timing of Antiretroviral Treatment (START) trial. Lancet Respir Med. 2016;4(12):980–9. Substudy from START study, assessing whether earlier ART affects longitudinal pulmonary function over a 2 year period. No such effect was found, irrespective of smoking status, which by itself markedly affected the course of pulmonary function.
Hoy J, Grund B, Roediger M, Ensrud KE, Brar I, Colebunders R, et al. Interruption or deferral of antiretroviral therapy reduces markers of bone turnover compared with continuous therapy: The SMART body composition substudy. J Bone Miner Res. 2013;28(6):1264–74.
• Hoy JF, Grund B, Roediger M, Schwartz AV, Shepherd J, Avihingsanon A, et al. Immediate initiation of antiretroviral therapy for HIV infection accelerates bone loss relative to deferring therapy: findings from the START bone mineral density substudy, a randomized trial. J Bone Miner Res. 2017;32:1945–55. https://doi.org/10.1002/jbmr.3183. Substudy from START study, assessing whether earlier ART affects changes in bone mineral density over a 2 year period. Earlier ART reduced density more so in the first but not the second year, and this initial decline was not linked to type of ART used.
Borges ÁH, Hoy J, Florence E, Sedlacek D, Stellbrink HJ, Uzdaviniene V, et al. Antiretrovirals, fractures, and osteonecrosis in a large international HIV cohort. Clin Infect Dis. 2017;64(10):1413–21.
Cysique LA, Vaida F, Letendre S, Gibson S, Cherner M, Woods SP, et al. Dynamics of cognitive change in impaired HIV-positive patients initiating antiretroviral therapy. Neurology. 2009;73(5):342–8.
Wright E, Grund B, Robertson K, Cysique L, Collins G, Brew B et al. No difference between the effects of immediate versus deferred ART on neuropsychological test performance in HIV-positive adults with CD4+ cell counts > 500 cells/μL. 15th European AIDS Conference (EACS), Barcelona, October 2015.
•• Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–9. Follow-up report to original HPTN 052 report documenting substantial reduction (93%) in risk of linked HIV transmission from placing HIV+ person on ART. Whereas no linked transmission was observed while index HIV+ person was on fully suppressive ART, a total of 8 linked transmissions were observed after initiation of ART stressing that full adherence is required.
•• Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using supportive antiretroviral therapy. JAMA. 2016;316:171–81. International study assessing the risk of HIV transmission in serodiscordant relationships having condom-less sex, and where the initial HIV+ person was on fully suppressive ART. No linked transmissions were observed after 40,000+ sexual intercourses. Supports claim that fully suppressive ART renders the person no longer able to transmit HIV.
Jean K, Boily MC, Danel C, Moh R, Badjé A, Desgrées-du-Loû A, et al. What level of risk compensation would offset the preventive effect of early antiretroviral therapy? Simulations from the TEMPRANO trial. Am J Epidemiol. 2016;184:755–60.
• Sereti I, Gulick RM, Krishnan S, et al. ART in HIV persons with pre-treatment viremia ≤ 3000 c/mL: the START study. Abstract 984, Conference on Retroviruses and Opportunistic Infections (CROI), Seattle, Washington, 2017. Subgroup analysis of START cohort, focused on those entering the study with low HIV RNA viral load. Earlier ART raised CD4+ lymphocyte count and reduced risk of HIV viral rebound . No power was available to assess impact on clinical events from earlier initiation of ART.
The SPARTAC Trial Investigators, Fidler S, Porter K, Ewings F, Frater J, Ramjee G, et al. Short-course antiretroviral therapy in primary HIV infection. N Engl J Med. 2013;368:207–17.
Crowell TA, Hatano H. Clinical outcomes and antiretroviral therapy in ‘elite’ controllers: a review of the literature. J Virus Erad. 2015;1:72–7.
Borges AH, Neuhaus J, Sharma S, et al. Benefit of continuous/immediate ART on disease risk: SMART & START combined analysis. Abstract 793, Conference on Retroviruses and Opportunistic Infections (CROI), Seattle, Washington; 2017.
Mocroft A, Phillips AN, Gatell J, Ledergerber B, Fisher M, Clumeck N, et al. Normalization of CD4 counts in patients with HIV-1 infection and maximum virological suppression who are taking combination antiretroviral therapy: an observational study. Lancet. 2007;370:407–13.
Acknowledgements
The authors would like to thank the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials), its leadership including Drs. F Gordin, A Babiker, A Phillips, J Baker and B Grund, and main funder division of AIDS, National Institutes of Allergy and Infectious Diseases, USA.
Funding
This work was supported by the Danish National Research Foundation [grant 126].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alvaro H Borges is supported by Lundbeckfonden (grant R219-2016-762). James D. Neaton reports grants from NIH and NIAID. Jens D. Lundgren declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Co-infections and Comorbidity
Rights and permissions
About this article
Cite this article
Lundgren, J.D., Borges, A.H. & Neaton, J.D. Serious Non-AIDS Conditions in HIV: Benefit of Early ART. Curr HIV/AIDS Rep 15, 162–171 (2018). https://doi.org/10.1007/s11904-018-0387-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-018-0387-y