Abstract
In the current age of endoscopic and interventional radiologic management of bleeding varices, the paradigm of surgical management for portal hypertension has radically shifted. There remains, however, a less common but important role for the well-trained surgeon who understands and is capable of managing portal hypertension. Patients who may benefit from surgical intervention are those with early cirrhosis or non-cirrhotic portal hypertension and suffer from variceal bleeding due to the consequences of portal, mesenteric, or splenic vein thrombosis. In addition, good surgical candidates who have limited access to care, may not be capable of close follow-up, or who have had failed prior therapy can benefit from more definitive surgical shunting. Liver transplantation has also changed the landscape in managing portal hypertension as the ultimate treatment for patients with advanced cirrhosis. Limited indications and fewer surgeons having been exposed to shunting procedures for portal hypertension have resulted in fewer shunts being performed, though they remain indicated under special circumstances. It is critical that we discern the role of various treatment options in different clinical scenarios and appreciate that under certain circumstances, a surgical intervention is indicated. This article reviews the history and progression of surgery for portal hypertension and highlights the current role of the surgeon in the era of multidisciplinary intervention. Furthermore, an algorithm for current management of variceal bleeding is presented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgery, once a cornerstone in the management of portal hypertension and bleeding varices, has largely been replaced in the current era by endoscopic and radiologic interventions and liver transplantation. Even though surgical procedures for portal hypertension have dramatically declined in the past decades, certain circumstances call for the judgment and technical expertise required to make these operations successful. Though many practitioners believe that surgical procedures for portal hypertension and bleeding varices have only historical value, there continues to be a role for surgical intervention in both cirrhotic and non-cirrhotic patients. In general, surgery for portal hypertension is most applicable in early stage cirrhotic or non-cirrhotic patients, those with total or partial portal or mesenteric vein thrombosis, and good surgical candidates with failed non-surgical interventions.
In North America, surgery for portal hypertension has become anachronistic as few new surgeons have been trained or participated in portal hypertension surgery. More often than not, these are orphan procedures that should be performed at large volume liver transplant centers where multidisciplinary teams are familiar with managing liver disease and have a full understanding of liver transplantation. Careful planning, comprehensive medical support, and expert technical execution are all required for these procedures to be successful. Because so few are performed each year, these operations lend themselves to the center of excellence model with collaborative interdisciplinary teams coordinating care.
Procedures can be divided into three distinct categories—devascularization procedures, non-selective shunts (total or partial), and selective shunts. These generalized groups provide a framework for the evolution of portal hypertension surgery, as they each have their own unique indications and success rates.
Devascularization Procedures
Devascularization procedures are performed to interrupt the blood flow to bleeding varices in the stomach and lower esophagus. Early iterations of this procedure called for interruption and even transection of the lower esophagus. These procedures resulted in severe morbidity and mortality. This is often attributed to poor patient selection and delayed referral in an already compromised cirrhotic patient who often presents in extremis. The Hassab and Sugiura procedures were both purposed to eradicate the varices in the lower esophagus and the stomach [1, 2]. Essentially, the blood supply is interrupted to the high pressure varices. The Hassab procedure called for a splenectomy, devascularization of the distal esophagus, devascularization of the stomach, vagotomy, and pyloroplasty. The Sugiura technique, in comparison, was much more technically demanding. The original Sugiura procedure consisted of esophageal devascularization through a thoracic incision followed by an abdominal operation some weeks later. It also called for, among other steps, complete transection and reanastomosis of the esophagus. These operations were both modified over time into less morbid procedures, making them easier to perform and better tolerated by the patient [3••].
The most successful and widely practiced devascularization operation is the modified Sugiura procedure. Several variations on this operation have been proposed that are known colloquially as the modified, modified Sugiura procedure. They differ in the thoracic versus abdominal approach, extent of gastric devascularization, and the necessity of esophageal transection [4–9]. Regardless of the details, all procedures adequately disrupt the blood supply to the varices in the stomach and esophagus while maintaining collateral flow into the azygos system by preservation of the left gastric or coronary vein. The main indication for this procedure is uncontrolled or recurrent bleeding after failed banding or where a transjugular intrahepatic portosystemic shunt (TIPS) procedure is unavailable or contraindicated. The most common scenario is after a failed endoscopic intervention to control variceal bleeding in a patient with extensive portal venous thrombosis. The modified Sugiura procedure is most successful in non-cirrhotic portal hypertensive patients or carefully selected patients with Child A or B cirrhosis without ascites [9].
Typical of the modified Sugiura, Selzner et al. reported excellent results with a one-stage operation [10]. The procedure itself consisted of splenectomy and devascularization of the lesser and greater curvature of the stomach extending up to the lower esophagus. The coronary vein was preserved, and the esophagus was transected and reanastomosed with a stapler. Finally, a pyloroplasty was performed to facilitate gastric emptying. At 4 years, they reported a low mortality and rebleed rate. The most prevalent complication was esophageal stricture requiring endoscopic dilation. Subsequently, Orozco omitted the splenectomy from the modified Sugiura-Futagawa procedure resulting in less transfusion requirement and lower risk of postoperative portal vein thrombosis, but there were similar outcomes in terms of rebleeding, encephalopathy, operative times, and postoperative complications [11]. The authors have adopted this approach due to the reduced morbidity with equal success and a focus on achieving adequate portoazygous disconnection. In addition, variceal banding is incorporated as complimentary therapy rather than esophageal transection, as increased esophageal complications are more likely to occur if transection is performed after endoscopic therapy. In carefully selected patients, operative mortality is near 5 % with rebleeding rate of 10–30 % and encephalopathy rate of 5 %. This illustrates that patient selection and fastidious operative technique can result in good outcomes.
Non-Selective Shunts
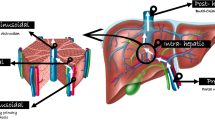
Non-selective shunts divert prehepatic portal flow to the vena cava. These shunts can be total or partial depending on the technique and size of the shunt and whether it allows any prograde flow into the liver. In total shunts, all portal flow is redirected into the vena cava by side-to-side, end-to-side, or interposition graft anastomosis. In general, these shunts are technically less demanding than selective shunts and can be performed rather quickly. The abdomen is entered through a midline incision, and the porta hepatis is dissected, thus preserving the bile duct and hepatic artery. Careful retraction of these structures allows exposure of the portal vein. Next, the vena cava is dissected and controlled. A number of options for anastomosis are available at this time. A side-to-side portocaval anastomosis can be fashioned, which controls gastrointestinal bleeding and ascites (Fig. 1). Alternatively, the portal vein can be divided, and an end-to-side anastomosis can be created to effectively control bleeding. The full shunt is mostly of historical value although in the authors’ experience, this shunt has been helpful in unique situations.
Like the TIPS procedure, non-selective shunts are contraindicated in patients with encephalopathy and the patient’s portal vein must be patent and relatively free from thrombus. The disruption and scarring that occur in the porta hepatis create a hostile hilum and may disadvantage the patient who needs reoperation or transplantation. Despite this, Orloff recently compared portocaval shunting to the TIPS procedure by evaluating over 50 years of data [12•]. In this non-selected, consecutive study, portocaval shunting achieved effective bleeding control (97–100 %), lower rebleeding rates, less shunt occlusion, and better median survival (10 years with shunting vs 2 years in TIPS). Portosystemic encephalopathy with shunting was 15–21 %. In addition, surgical shunting was more cost-effective. Regardless, TIPS remains the initial therapy of choice for most patients with bleeding varices that cannot be controlled with endoscopy in the setting of a patent portal vein. Unfortunately, studies comparing TIPS to non-selective shunts do not adequately address the advantages of minimally invasive approaches, the availability of liver transplantation, and the role of surgical shunts in select populations.
The mesocaval shunt is centered on the superior mesenteric vein rather than the portal vein but is still technically considered a total shunting operation (Fig. 1). Patients who receive a mesocaval shunt mostly have Child A or early B cirrhosis. Some of these patients may become candidates for liver transplantation but are so early in their disease that TIPS is inappropriate because of its limited durability [13]. Furthermore, patients with Budd-Chiari syndrome, non-cirrhotic portal hypertension, or refractory ascites may be suitable for this procedure. Excellent results can be seen with this approach, and unlike the portal caval shunts, it does not require a patent portal vein and does not violate the porta hepatis [14]. The shunt is performed through a midline incision that extends beyond the umbilicus. The transverse mesocolon is reflected superiorly in order to expose the superior mesenteric vein. The vena cava can be exposed either through the right colon mesentery or by medial visceral rotation. Some controversy exists over the choice of conduit, but both non-biologic grafts and autologous vein (often the internal jugular vein) have been used successfully with excellent long-term patency [15, 16]. Care must be taken in the course of the graft to prevent acute angles or kinking that could result in subsequent thrombosis. As with all total shunts and TIPS procedures, patients with preexisting uncontrolled hepatic encephalopathy should be excluded. In well-selected patients, 1-year survival of 92 % can be achieved with shunt patency rate of 90 % and encephalopathy rate of 10–15 %.
Partial Shunts
In essence, partial shunts are anatomically similar to total shunts with one major variation: The diameter of the shunt is reduced to preserve prograde flow to the liver, hence reducing risk of encephalopathy and liver dysfunction. The partial portocaval shunt popularized by Sarfeh creates a partial shunt by interposing a reduced diameter conduit between the portal vein and the vena cava [17]. Usually, the conduit is composed of ringed PTFE, and the critical decision is choosing the size of the graft. A 10-mm graft can maintain prograde portal flow in nearly 50 % of patients, whereas an 8-mm graft secures prograde flow in most cases. The smaller diameter shunt diverts flow to the IVC yet still allows for hepatopetal flow which lessens the risk of subsequent encephalopathy. The Sarfeh shunt, as it is often referred to, requires collateral ligation to secure more flow through the shunt and reduce bleeding risk. The coronary vein, gastroepiploic veins, veins along the lesser curve of the stomach, and in some instances the inferior mesenteric vein are ligated. This procedure is also technically less challenging than the splenorenal shunt, which makes it more applicable to general and vascular surgeons [18, 19]. Long-term results reported by Sarfeh and colleagues show 7-year patency rates of 95 % for grafts at risk with absence of variceal bleeding in 92 %; operative mortality of 7.7 % was reported for Child class A and B patients [20].
A modification used by the authors with great success has been the partial splenorenal shunt with interposition PTFE graft, usually 8 or 10 mm in diameter (Fig. 1). This shunt has been effective in avoiding the porta hepatis and can be paired with partial devascularization as described above. In our experience, this shunt is best used in patients with failed attempts at TIPS, who have patent vasculature or may be potential transplant candidates. The partial splenorenal shunt is advantageous in the setting of orthotopic liver transplant because the splenic contribution to the portal inflow is restored by shunt ligation.
Selective Shunts
The eponymous distal splenorenal shunt (DSRS) is the most well-known selective shunt and was originally proposed by Warren et al. [21]. This shunt is referred to interchangeably as the Warren shunt or the distal splenorenal shunt. The selective nature of this shunt is intended to separate the portal flow system from the gastrosplenic-esophageal venous collaterals. This shunt results in decompression of varices while preserving or possibly raising portal pressure. In this procedure, the gastrocolic ligament is opened, and all the small feeding vessels are ligated. The coronary and right gastroepiploic veins are identified and ligated. Short gastric vessels are preserved to allow for drainage through the splenic vein. The splenic vein is dissected free of the pancreas, divided at its confluence with the superior mesenteric vein, and subsequently anastomosed to the left renal vein. Flow from esophageal and gastric varices is directed into the splenic vein and then into the left renal vein (Fig. 1). Care should be taken in creating a tension free and “loose” lie, or the anastomosis and splenic vein may be prone to thrombosis. If, in attempting a DSRS, full mobilization of the splenic vein proves challenging, an interposition graft can be used as an alternative. Encephalopathy is reported at 5–10 % with rebleeding at 5 %; operative mortality averages at 5 % and long-term shunt patency of 90 % among patients at risk.
Several studies have compared the DSRS shunt to other procedures to control variceal bleeding [22, 23, 24•]. Although the splenorenal shunt prevented recurrent bleeding in patients more effectively than other therapies, there was no difference in overall patient survival when compared to TIPS. Furthermore, there appeared to be no cost difference between TIPS and the DSRS shunt, though TIPS is associated with increase in cost later in years, probably related to need for monitoring and reinterventions. One major advantage with TIPS is restoration of portal flow dynamics after liver transplantation [25]. Most studies, however, fail to identify disease-specific, metabolic, and physiologic parameters that would help the clinician tailor the most suitable shunt for the most appropriate patient and circumstances. This is a concern especially with indiscriminate use of TIPS.
In addition, for patients with Child A cirrhosis and no indication or prospects for liver transplantation, the DSRS achieves very good long-term control while preserving liver prograde flow. The latter is of concern as some patients show progressive, potentially precipitous deterioration in liver function or septic events as a result of TIPS. Unlike the portocaval total shunts, the DSRS shunt is well outside the operative field for subsequent liver transplantation, thus making it the preferred therapy in some patients awaiting liver transplant and when other methods of variceal bleeding control have failed [26]. The distal splenorenal shunt should be in every portal hypertension surgeon’s armamentarium. In patients that are early in their disease process, have failed TIPS, or are either unwilling or incapable of the close follow-up required with other modalities, the splenorenal shunt is a long proven and durable therapy. For these patients awaiting liver transplantation, the use of fully reversible shunts is preferred.
The Rex Shunt
Extrahepatic portal hypertension secondary to portal vein occlusion in children presents a unique problem. This can occur de novo or after liver transplantation. When the occlusion is chronic, these patients develop portal hypertension and bleeding in the setting of a normally functioning liver. In these situations, liver transplantation is usually not the solution and conservative treatment with a non-selective beta blocker is appropriate. Initial bleeding episodes are controlled with banding of esophageal varices. However, gastric varices frequently become problematic, and esophageal varices can extend further proximally along the esophagus. Any episode of bleeding should lead to cross-sectional imaging. If the left intrahepatic portal vein is patent, a Rex shunt can be performed. In this procedure, the Rex recess is approached, and dissection reveals the left portal vein. Next, an autologous vein, often the left internal jugular vein or femoral vein, is harvested and a bridge is created between the superior mesenteric vein and left portal vein, utilizing the vein as a conduit (Fig. 2). This essentially bypasses the affected portal vein. This elegant solution creates a purely prehepatic bypass and prevents the incidence of subsequent encephalopathy [27••]. This is an anatomically restorative shunt and is associated with improved liver function as well. Several studies have shown this technique to be superior to traditional shunts in children with this condition [28, 29, 30••]. A unique application of this type of shunt that has been feasible is in left-lobe, living-donor liver transplant recipients with portal vein thrombosis [31].
Unconventional shunts to alleviate portal hypertensive bleeding. a Coronary caval shunt with PTFE (arrow). b Mesogonadal shunt showing gonadal to mesenteric vein branch anastomotic site (arrow) with enlargement of the gonadal vein. c Inferior mesenteric vein-renal shunt. d Rex mesoportal shunt showing proximal anastomosis (solid arrow) and left portal vein (hashed arrow)
The current authors have used the Rex shunt in selected adults with segmental portal occlusion [32]. The challenge is identifying the native left portal vein which may not be well visualized on cross-sectional imaging. Additionally, the shunt pressure is initially elevated but subsequently improves with gradual dilatation of the portal venous system beyond the anastomosis (Fig. 2). This elevated pressure may be associated with early shunt thrombosis; therefore, early monitoring with frequent ultrasounds and early intervention are crucial to salvage the shunt.
Splenopneumopexy
Splenopneumopexy, a procedure developed and popularized in Japan, has been shown to be an effective surgical procedure for Budd-Chiari syndrome [33]. The technique preserves some portal hypertension, and collaterals are expected to develop over time with minimal to no risk of encephalopathy. The procedure involves ligation of the splenic artery and left gastric vein. The lower portion of the esophagus is devascularized from venous collaterals, and the short gastric veins are left intact. A small incision is made in the diaphragm, and the spleen is fixed to the cut edge of the diaphragm. The splenic capsule is peeled away and spleen sutured to the lower surface of left lower lung lobe after abrading its surface. In experienced hands, this technique has proven very effective in control of variceal bleeding and alleviating symptoms in patients with Budd-Chiari syndrome. In addition, better diversion of portal blood is expected over time.
Sinistral Portal Hypertension
A comprehensive review of portal hypertension surgery in the non-cirrhotic patient is not complete without mentioning left-sided or sinistral portal hypertension. Left-sided portal hypertension occurs when the pancreatic vein is occluded and the venous return is detoured through the short gastric, gastroepiploic, or right gastric (coronary) veins. This results in high pressure venous return in these usually low pressure and thin-walled veins [34]. Esophageal varices, commonly attributed to portal venous hypertension, can also occur from redirection of the pancreatic venous flow through retroperitoneal collateral channels or along the lower esophagus. These varices can lead to bleeding in the stomach and occasionally in the esophagus. The etiology of the splenic vein thrombosis is classically caused by chronic pancreatitis, especially in the setting of pseusocyst. [35] One solution to this problem is splenectomy, but thoughtful treatment of sinistral hypertension may be more complex.
Diagnosis of splenic vein thrombosis is usually suspected within the workup of pain from chronic pancreatitis or gastrointestinal bleeding. Diagnosis should include visualization of the mesenteric and portal venous system with an imaging test such as CT venogram, MRI, or ultrasound with Doppler and endoscopic evaluation to reveal the extent and location of esophageal and/or gastric varices. These modalities can also evaluate simultaneously for splenomegaly.
If thrombosis or occlusion extends beyond the splenic vein into the portal or superior mesenteric vein or if EGD shows portal hypertensive gastropathy, one should consider portal hypertension. In this event, underlying liver disease should be evaluated with laboratory data, liver morphology, and possibly liver biopsy. Surgery can then be considered in light of the severity of liver disease or cirrhosis, if present.
Endoscopy can be used for diagnosis and therapy. Sclerotherapy, injection, or banding may relieve bleeding from the varices. As this does not alleviate the underlying etiology, however, bleeding may recur leading to further intervention. Operative intervention for bleeding is splenectomy, and if indicated, it can be combined with pancreatic surgery such as a pseudocyst drainage or lateral pancreaticojejunostomy if deemed necessary.
The Authors’ Approach
Given the interdisciplinary nature of portal hypertension management, we have developed treatment algorithms for patients with bleeding secondary to portal hypertension (Fig. 3). Such alogrithms incorporate the available resources and expertise, account for changes in practice and new techniques, and are modified based on perceived efficacy and outcomes. Furthermore, it has become evident that TIPS has resulted in reduced need for surgical interventions. However, there is still an important role for shunting procedures, if expertise is available and a data-driven approach is utilized to achieve optimal and cost-effective outcomes.
Management of variceal bleeding with failed medical therapies. a Initial workflow leading to surgical algorithm. b Options for surgical interventions. Asterisk denotes review of Child stage and suitable anatomy for shunt feasibility. Double asterisks highlights surgeon preference and transplant candidacy issues; please refer to text for more discussion
In patients being considered for liver transplantation, if bleeding recurs in the absence of hepatic encephalopathy, consideration is given for the TIPS procedure. We have found that, with the judicious use of available medical therapies, most patients can be brought to liver transplant, as this is the ultimate therapy for portal hypertension secondary to cirrhosis. In the rare instances where these methods are unsuccessful at stopping or preventing further bleeding, we have considered several surgical approaches (Fig. 3) and more recently more radical interventions including balloon-occluded retrograde transvenous obliteration (BRTO) [36]. In such patients, we prefer the H graft partial shunts (splenorenal, mesocaval) which can be fully reversed during transplant. Alternatively, devascularization may be considered especially in the setting of encephalopathy. The DSRS is kept as a last resort given the permanent diversion of splenic flow; though this is an excellent shunt for Child A and select Child B patients. In non-transplant candidates, the DSRS is favored with suitable anatomy in Child A and early B patients. The small diameter H graft shunt can also be an option depending on surgeon preference or comfort. In this setting, we reserve devascularization when a shunt is not feasible such as portomesenteric thrombosis, small vessels, or in the presence of encephalopathy. Limited access to care and poor compliance should favor surgical shunts, being more definitive and requiring less reinterventions.
The most satisfying and technically demanding operations we perform for portal hypertensive bleeding involve patients with extensive portal venous thrombosis in the absence of cirrhosis. These patients are referred for a variety of reasons. Some examples are idiopathic portal vein thrombosis with recurrent episodes of bleeding that cannot be controlled by conservative methods and patients with episodes of bleeding that have been controlled but need to be anti-coagulated. In these patients, we obtain a triple phase contrast computed tomography study of the abdomen and pelvis. More often than not, a prominent varix can be seen. At this point, we take what some would consider an “a la carte” approach. At surgery, we will bypass from the varix to the systemic circulation using a native or synthetic conduit (8–10 mm PTFE graft) (Fig. 2). We will simultaneously perform a partial devascularization along the greater and lesser curvatures if the patient has prominent gastric varices. In some instances, we ligate the splenic artery as well to modulate collateral flow. This combination of devascularization and bypass has proven quite successful [37•].
The Rex shunt is reserved for patients with isolated portal vein thrombosis and patent mesenteric veins in the absence of liver disease or cirrhosis. We have successfully performed this shunt in two adults, though most applications are in children. While the algorithms outlined (Fig. 3) serve as a good starting point, the surgeon is often faced with navigating various options in diverse clinical settings. In addition, local expertise should be taken into consideration to safely achieve the most effective result. Being well versed with portal hypertension and surgical maneuvers is critical to achieve the best outcomes in these patients.
Conclusion
In conclusion, the role of surgery for portal hypertension and the control of variceal bleeding has changed significantly over the past decade. Medical therapies (including endoscopic variceal ligation) and radiologic interventions (TIPS, BRTO) achieve control in the majority of instances. However, surgery remains an important option in certain circumstances. These include patients with failed prior interventions and non-cirrhotic patients with thrombosis in the portal venous system. Patients with early cirrhosis and poor access to follow-up or non-candidates for liver transplantation also benefit from definitive surgical shunting. Principles of portal hypertension treatment should govern the chosen operation as outlined above (Fig. 3). These patients should be treated by a multidisciplinary team at a tertiary care center with expertise in all facets of liver disease including liver transplantation. It is especially important to frame therapy within the context of the overall care plan, including liver transplantation if deemed suitable. This would allow for proper sequencing and anticipation of future therapies. Given that surgical shunts and devascularization procedures are becoming less frequent, referral to a qualified surgeon when indicated is not top of mind for the referring physician. In addition, with change in referral patterns, non-transplant surgeons are rarely exposed to portal hypertension surgery. Hence, it behooves us to work in collaborative teams to continue refining the roles of various therapies for different disease states and develop processes for timely referral for surgical therapy when indicated. It is also critical for surgeons to be able to maintain surgical skills and competency in managing portal hypertension, medically and surgically, to best serve this unique patient population.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hassab MA. Gastroesophageal decongestion and splenectomy in the treatment of esophageal varices in bilharzial cirrhosis: further studies with a report on 355 operations. Surgery. 1967;61:169–76.
Sugiura M, Futagawa S. A new technique for treating esophageal varices. J Thorac Cardiovasc Surg. 1973;66:677–85.
Liu Y, Li Y, Ma J, Lu L, Zhang L. A modified Hassab's operation for portal hypertension: experience with 562 cases. J Surg Res. 2013;185:463–8. The largest published experience with the modified Hassab operation. Worth noting that with proper selection, better outcomes can be achieved. In the United States, this operation has been used as a last resort and hence the checkered experience.
Pierce GE, Thomas JH, Estes NC. A transthoracic devascularization procedure for control of bleeding esophageal varices: preliminary report. Am J Surg. 1977;134:794–8.
Merdad A, Sibiany A. Modified Sugiura procedure for nonalcoholic bleeding esophageal varices. Ann Saudi Med. 1995;15:407–9.
Shah SR, Nagral SS, Mathur SK. Results of a modified sugiura's devascularisation in the management of "unshuntable" portal hypertension. HPB Surg. 1999;11:235–9.
Sharma D, Agrawal S, Saxena A, Raina VK. A modified technique of devascularization for surgical management of portal hypertension in children. Trop Dr. 2001;31:93–5.
Soonawalla ZF, Shah SR, Mathur SK. Modified Sugiura procedure. J Am Coll Surg. 2002;194:247.
Feng AC, Liao CY, Fan HL, Chen TW, Hsieh CB. The modified Sugiura procedure as bridge surgery for liver transplantation: a case report. J Med Case Rep. 2015;9:50.
Selzner M, Tuttle-Newhall JE, Dahm F, Suhocki P, Clavien PA. Current indication of a modified Sugiura procedure in the management of variceal bleeding. J Am Coll Surg. 2001;193:166–73.
Orozco H, Mercado MA, Martinez R, Tielve M, Chan C, Vasquez M, et al. Is splenectomy necessary in devascularization procedures for treatment of bleeding portal hypertension? Arch Surg. 1998;133:36–8.
Orloff MJ. Fifty-three years' experience with randomized clinical trials of emergency portacaval shunt for bleeding esophageal varices in Cirrhosis: 1958-2011. JAMA Surg. 2014;149:155–69. This is a unique paper outlining a large experience by a single author. This is a rare experience worth reading to better understand that under proper selection and set of circumstances shunts may still have a role in managin variceal bleeding.
Maleux G, Nevens F, Wilmer A, et al. Early and long-term clinical and radiological follow-up results of expanded-polytetrafluoroethylene-covered stent-grafts for transjugular intrahepatic portosystemic shunt procedures. Eur Radiol. 2004;14:1842–50.
Henderson JM, Nagle A, Curtas S, Geisinger M, Barnes D. Surgical shunts and TIPS for variceal decompression in the 1990s. Surgery. 2000;128:540–7.
Stipa S, Thau A, Schillaci A, Ziparo V, Rossi P, Passariello R. Mesentericocaval shunt with the internal jugular vein. Surg Gynecol Obstet. 1978;146:391–9.
Descottes B, Lachachi F, Maisonnette F, et al. Long-term results of mesocaval shunts with polytetrafluoroethylene grafts. Int Surg. 2008;93:268–73.
Sarfeh IJ, Rypins EB. The emergency portacaval H graft in alcoholic cirrhotic patients: influence of shunt diameter on clinical outcome. Am J Surg. 1986;152:290–3.
Hillebrand DJ, Kojouri K, Cao S, Runyon BA, Ojogho O, Concepcion W. Small-diameter portacaval H-graft shunt: a paradigm shift back to surgical shunting in the management of variceal bleeding in patients with preserved liver function. Liver Transpl. 2000;6:459–65.
Sriussadaporn S, Pak-art R, Sriussadaporn S. Small-diameter H-graft portacaval shunt for variceal hemorrhage: experience at King Chulalongkorn Memorial Hospital. J Med Assoc Thail. 2004;87:427–31.
Collins JC, Ong MJ, Rypins EB, Sarfeh IJ. Partial portacaval shunt for variceal hemorrhage: longitudinal analysis of effectiveness. Arch Surg. 1998;133:590–2. discussion 2-4.
Warren WD, Zeppa R, Fomon JJ. Selective trans-splenic decompression of gastroesophageal varices by distal splenorenal shunt. Ann Surg. 1967;166:437–55.
Santambrogio R, Opocher E, Costa M, Bruno S, Ceretti AP, Spina GP. Natural history of a randomized trial comparing distal spleno-renal shunt with endoscopic sclerotherapy in the prevention of variceal rebleeding: a lesson from the past. World J Gastroenterol. 2006;12:6331–8.
Boyer TD, Henderson JM, Heerey AM, et al. Cost of preventing variceal rebleeding with transjugular intrahepatic portal systemic shunt and distal splenorenal shunt. J Hepatol. 2008;48:407–14.
Kokudo T, Bonard E, Gillet M, Kokudo N, Halkic N. Reappraisal of shunt surgery for extrahepatic portal vein obstruction in adults: report of a single-center case series. Hepatol Res. 2015. A small but meaningful report illustrating role of various surgical shunts for extrahepatic portal vein obstruction also showing excellent survival.
Abouljoud MS, Levy MF, Rees CR, et al. A comparison of treatment with transjugular intrahepatic portosystemic shunt or distal splenorenal shunt in the management of variceal bleeding prior to liver transplantation. Transplantation. 1995;59:226–9.
Elwood DR, Pomposelli JJ, Pomfret EA, Lewis WD, Jenkins RL. Distal splenorenal shunt: preferred treatment for recurrent variceal hemorrhage in the patient with well-compensated cirrhosis. Arch Surg. 2006;141:385–8. discussion 8.
Alberti D, Colusso M, Cheli M, et al. Results of a stepwise approach to extrahepatic portal vein obstruction in children. J Pediatr Gastroenterol Nutr. 2013;57:619–26. Excellent series of pediatric patients with extrahepatic portal vein obstruction with a systematic approach to surgical options inclusive of the Rex shunt.
Bhat R, Lautz TB, Superina RA, Liem R. Perioperative strategies and thrombophilia in children with extrahepatic portal vein obstruction undergoing the meso-Rex bypass. J Gastrointest Surg. 2013;17:949–55.
Guerin F, Bidault V, Gonzales E, Franchi-Abella S, De Lambert G, Branchereau S. Meso-Rex bypass for extrahepatic portal vein obstruction in children. Br J Surg. 2013;100:1606–13.
Lautz TB, Keys LA, Melvin JC, Ito J, Superina RA. Advantages of the meso-Rex bypass compared with portosystemic shunts in the management of extrahepatic portal vein obstruction in children. J Am Coll Surg. 2013;216:83–9. One of the largest series of Rex shunt showing significant metabolic advantages with Rex shunt compared to portosystemic shunts.
Soejima Y, Shirabe K, Yoshizumi T, et al. Rex shunt for portal vein thrombosis after adult living donor liver transplantation. Fukuoka Igaku Zasshi. 2013;104:464–8.
Vanderlan WB M, Bansal A MD, Abouljoud MS MD. Adult portal hypertension secondary to posttraumatic extrahepatic portal vein thrombosis treated with Rex Shunt. J Trauma. 2009;66:260–3.
Akita H, Sakoda K. Portopulmonary shunt by splenopneumopexy as a surgical treatment of Budd-Chiari syndrome. Surgery. 1980;87:85–94.
Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179:129–33.
Agarwal AK, Raj Kumar K, Agarwal S, Singh S. Significance of splenic vein thrombosis in chronic pancreatitis. Am J Surg. 2008;196:149–54.
Park JK, Saab S, Kee ST, et al. Balloon-occluded retrograde transvenous obliteration (BRTO) for treatment of gastric varices: review and meta-analysis. Dig Dis Sci. 2014.
Nagai S, Abouljoud MS, Kazimi M, Yoshida A. Emergent nonconventional mesosystemic shunt for diffuse portomesenteric thrombosis: sparing patients from liver/multivisceral transplantation. Liver Transpl. 2013;19:661–3. A unique approach used by the authors to create a surgical shunt in a patient with portomesenteric thrombosis to treat varicela bleeding and avoid multivisceral transplantation.
Compliance with Ethics Guidelines
Conflict of Interest
Marwan Abouljoud, MD, Lauren Malinzak, MD, and David Bruno MD declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Portal Hypertension
Rights and permissions
About this article
Cite this article
Abouljoud, M., Malinzak, L. & Bruno, D. Surgical Options for the Management of Portal Hypertension. Curr Hepatology Rep 14, 225–233 (2015). https://doi.org/10.1007/s11901-015-0276-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-015-0276-4