Abstract
Purpose of Review
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare malignancy derived from plasmacyoid dendritic cells whose biology, clinical features, and treatment options are increasingly better understood.
Recent Findings
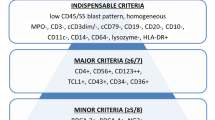
TCF4 is a master regulator that drives donwstream transcriptional programs in BPDCN. In turn, TCF4 activity is dependent on the bromodomain and extra-terminal domain (BET) protein BRD4 whose inhibition provides a promising therapeutic vulnerability. Notably, TCF4 expression is a highly sensitive marker for BPDCN and augments diagnostic specificity alongside CD4, CD56, CD123, and TCL1. The gene expression profile of BPDCN is characterized by aberrant NF-kappaB pathway activation, while its genomic landscape is dominated by structural chromosomal alterations involving ETV6, MYC, and NR3C1, as well as mutations in epigenetic regulators particularly TET2.
Summary
Advances in elucidating the biological characteristics of BPDCN are resulting in a more refined diagnostic approach and are opening novel therapeutic avenues for patients with this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a hematologic malignancy arising from precursors of plasmacytoid dendritic cells (pDCs). The first description of BPDCN is attributed to Kameoka et al., who in 1998 described two cases of cutaneous agranular CD2-/CD4+/CD56+ “lymphoma” and proposed that they represented a distinct entity [1]. Characterization of this rare neoplasm remained elusive until relatively recently, resulting in a nomenclature legacy that includes agranular CD4+ natural killer (NK) cell leukemia, CD56+/TdT+ blastic NK cell tumor, blastic NK cell leukemia/lymphoma, and agranular CD4+/CD56+ hematodermic neoplasm [2,3,4,5]. A similar legacy applies to the identification and characterization of pDCs. Known to occur in focal clusters in some cases of reactive lymphoid hyperplasia, these cells were called lymphoblasts then T-associated plasma cells, plasmacytoid T-cells, and plasmacytoid monocytes, before the current term pDCs was coined in 1997 by Grouard et al. [6]. In a case report, Lucio et al first proposed a possible relationship between pDCs and BPDCN on the basis of shared high-level CD123 expression [7]. The first systematic analysis supporting such a connection was published shortly thereafter by Chaperot et al. [8]
Plasmacytoid dendritic cells are present in blood and tissues where they play important roles in immunity as intermediaries between the innate and adaptive immune systems. [9] This is accomplished primarily through a tightly regulated toll-like receptor (TLR)7/9-MyD88-IRF7 pathway-mediated sensing of nucleic acid sequences and by functioning as antigen presenting cells in concert with other subsets of myeloid dendritic cells. Through the activation of toll-like receptor (TLR) agonists, pDCs secrete a gamut of cytokines dominated by type 1 interferons (mainly interferon alpha) and, to lesser levels, interleukin (IL)-6, IL-8, IL-12, tumor necrosis factor alpha, and other pro-inflammatory chemokines [10, 11]. In turn, pDC activation leads to the activation of T-cells, natural killer cells, and macrophages in physiologic and pathologic adaptive immunity reactions including infections and autoimmune diseases [12, 13]. It should be noted that the term pDC also includes other non-type 1 interferon-producing cells that represent differentiated dendritic cells in blood and tissues [14,15,16]. The latter subsets have been postulated to explain some of the phenotypic diversity of BPDCN [17].
Circulating pDC comprise ≤0.5% of peripheral blood mononuclear cells [18], and in this compartment they are defined as CD11c−/CD123+/CD303+. In tissues, pDC are localized primarily in lymph nodes and tonsils, and to a lesser extent in the bone marrow and spleen.
Etiology and Pathogenesis
The etiology of BPDCN is unknown. Reactive pDC proliferations were first described in 1958 by Lennert and Remmele [19]. Since then, reactive pDC proliferations have been recognized in association with various inflammatory and autoimmune conditions, including Kikuchi-Fujimoto lymphadenopathy (histiocytic necrotizing lymphadenitis), psoriasis, systemic lupus erythematosus, and hyaline-vascular-type Castleman disease [20,21,22]. In addition, nodular pDC proliferations referred to as mature pDC proliferations (MPDCP) have been recognized in association with myeloid neoplasms, most notably chronic myelomonocytic leukemia, myelodysplastic syndrome, and acute myeloid leukemia. [22,23,24] These proliferations typically consist of cytologically bland pDC nodules comprised of cells with moderate amounts of cytoplasm, variably irregular nuclear contours, and inconspicuous nucleoli. While they have been postulated to be clonally related to the associated myeloid neoplasm [25], no data establishes MPDCP as a precursor lesion of BPDCN.
The pathogenesis of BPDCN remains poorly understood. We have identified a high rate of monoallelic and biallelic 12p13/ETV6 deletions in BPDCN tumors as well as in the bone marrows of BPDCN patients without detectable disease, suggesting that such alterations might represent an early pathogenic event [26]. In a subset of patients, BPDCN is identified in a myelodysplastic background (see below) raising the possibility that at least a subset of cases might represent a secondary malignancy [27]. Ceribelli et al. identified a BPDCN-specific transcriptional network regulated by the E-box transcription factor TCF4 (also known as E2-2) that plays a master regulatory role in BPDCN cells and appears to be in turn regulated by the bromodomain and extra-terminal domain (BET) protein BRD4 [28]. Notably, knockdown of TCF4 results in downregulation of CD123 and CD56 expression in BPDCN cells. Indeed, TCF4 had been identified as a key regulator that controls the committed development of pDCs from common dendritic cell progenitors through a regulatory network of secondary transcription factors [29, 30]. In another study, Emadali et al. identified frequent NR3C1 haploinsufficiency in BPDCN linked to aberrant overexpression of a novel long noncoding RNA (lncRNA) gene, lincRNA-3q, whose product is involved in G1/S cell cycle transition through E2F [31]. Notably, BET inhibition abrogated the impact of lincRNA3q overexpression. Gene expression profiling of BPDCN demonstrated a signature that is in keeping with derivation from resting (not activated) myeloid pDCc and demonstrated aberrant NF-kappaB pathway activation [32].
Clinical Characteristics
BPDCN is rare, estimated to represent < 1% of all hematologic malignancies [33]. In a recent analysis based on Surveillance Epidemiology and End Results (SEER) data, the incidence of BPDCN in the USA is estimated to be 0.04 cases per 100,000 individuals, most of whom are Caucasian [34]. Men are affected more commonly than women. Although the disease has been reported in all age groups, the median age of patients at diagnosis is 53 years. Interestingly, the disease appears to exhibit a bimodal incidence pattern in the SEER database, with peaks in individuals < 20 years and those > 60 years [34]. Cutaneous lesions are often the presenting sign for patients with BPDCN, identified in at least 64% of patients [35]. Other common sites of disease involvement include the bone marrow and lymph nodes, and some patients have an overtly leukemic presentation without discernible extramedullary disease at presentation [27, 36, 37]. Overt or occult central nervous system (CNS) involvement is common at diagnosis, and up to one third of patients have CNS involvement at relapse [37,38,39]. A sizeable subset of patients with BPDCN have either synchronous or metachronous myeloid neoplasms that typically include chronic myelomonocytic leukemia, myelodysplastic syndrome, or acute myeloid leukemia [2, 40, 41].
Microscopic Features
Cutaneous lesions consist of a diffuse dermis-based proliferation of neoplastic cells that are small or intermediate in size, often with moderate amounts of cytoplasm and an eccentrically located nucleus with a prominent nucleolus. Mitotic figures are usually present, and necrosis can be present occasionally [2, 42]. The infiltrate is typically extensive and extends deep into subcutaneous tissue, with sparing of the upper dermis, epidermis, and adnexal structures. BPDCN in lymph nodes involves the medullary and interfollicular areas. In the bone marrow, BPDCN often exhibits a diffuse growth pattern with replacement of hematopoietic elements. The cytomorphology of BPDCN on Wright-Giemsa-stained smears is variable, but in many cases the cells are elongated, with a tapered lightly basophilic agranular cytoplasm that ends with a tail-shaped structure. The nucleus has blastoid features with open chromatin and a prominent nucleolus [27]. Less commonly, the neoplastic cells have lymphoid morphology, occasionally with cytoplasmic vacuoles, and less prominent blastoid nuclear features. Sakamoto et al. have proposed recently the term “immunoblastoid” variant to describe BPDCN cases in which the neoplastic cells resemble immunoblasts with their characteristic round nucleus with vesicular chromatin and a prominent nucleolus; 35% of BPDCN cases in their study belonged to this variant category. [43] Several groups have reported myelodysplastic morphologic and cytogenetic (see below) features in the bone marrow of BPDCN patients. [2, 27, 31]
Immunophenotype
The immunophenotype of BPDCN recapitulates that of pDC subsets. In routine practice, immunophenotypic profiling is accomplished using flow cytometry and/or immunohistochemistry. BPDCN is characterized by the expression of the pDC-associated markers CD123, CD303, and TCF4. CD123, the interleukin-3 (IL-3) receptor α-chain, is the primary low-affinity subunit of the IL-3 receptor and promotes high-affinity binding to IL-3 when co-expressed with the β-subunit. It is characteristically expressed at a high level in pDCs, MPDCP, and BPDCN. CD123 is expressed at various levels in other hematologic malignancies, including hairy cell leukemia [44], acute myeloid leukemia [45], and systemic mastocytosis [46], but in most such instances, it is expressed at a relatively lower intensity. CD303 (also known as blood dendritic cell antigen 2; BDCA2) is a pDC-specific type II C-type endocytic lectin that is able to target ligand into antigen-processing and peptide-loading compartments for presentation to T cells [47]. CD303 can also mediate inhibition of interferon α/β, providing a potential negative regulatory pathway for TLR9-induced pDC activation [47, 48]. Although CD303 is a useful specific marker for BPDCN [49], it has limited sensitivity due to its frequent aberrant loss in BPDCN. Indeed, CD303 loss is a useful marker to discern reactive from neoplastic pDC proliferations in some situations. Other pDC-specific antigens, including CD2AP, Spi-B and BCL11A, have been also proposed as useful markers for BPDCN [50]. In addition, BPDCN cells express CD4, CD56, and TCL1, and by definition they are negative for lineage-specific markers including CD3, CD19, and myeloperoxidase [27]. Notwithstanding, various lineage-associated antigens are expressed to varying extents in some BPDCN cases; these include CD2, CD5, CD7, CD33, CD38, CD68, CD117, HLA-DR, and TdT [27]. Expression of BCL2, BCL6, and S100 has also been reported [42, 43, 51, 52]. The Ki-67 proliferation rate is typically high in BPDCN. BPDCN has been shown to consistently lack myeloid cell nuclear differentiation antigen (MNDA) expression, a feature that helps in the distinction between BPDCN and extramedullary myeloid neoplasms, which are often (65%) positive for MNDA expression [53].
Multicolor multiparameter flow cytometry plays an important role in the immunophenotyping of BPDCN, particularly in the evaluation of bone marrow samples. Besides its diagnostic utility in distinguishing BPDCN from acute myeloid leukemia, flow cytometry is useful for assessment of measurable residual disease (MRD) in patients who achieve clinical remission following induction chemotherapy. Furthermore, flow cytometry allows differential analysis of the BPDCN population as well as background hematopoietic elements (myeloblasts and maturing elements), particularly in cases where BPDCN is present in association with another hematologic malignancy. The BPDCN flow cytometry panel employed presently at MD Anderson for baseline evaluation and residual disease assessment includes the following markers: CD4, CD33, CD45, CD56, CD64, CD123, CD303, and HLA-DR. Analysis of BPDCN cells is typically achived by gating on CD123+ events. This approach is also applicable in patients receiving CD123-targeted therapy, as most agents available to date do not cause significant alteration of CD123 expression levels.
The immunophenotype of MPDCP is similar to that of pDCs, although on occasion aberrant expression patterns may be seen. The clinical and prognostic significance of the latter remains unclear. Aberrantly expressed antigens reported have included CD2, CD5, CD7, CD10, CD13, CD14, CD15, and CD33. CD56 is usually negative, but we have seen rare cases with weak focal CD56 expression. TdT is negative and, in contrast to BPDCN, the Ki-67 proliferation rate is typically low in MPDCP [23, 50, 54, 55].
Chromosomal Abnormalities and Mutations
Although BPDCN cases exhibit heterogeneous karyotypic features, salient patterns have been recognized. The majority of BPDCN cases have chromosomal abnormalities detectable by conventional karyotyping, and up to 75% have a complex karyotype (≥ 3 abnormalities, including at least one structural abnormality) [56]. Abnormalities involving the short arm of chromosome 12 and, more specifically, the 12p13 locus containing ETV6 are the most frequent findings in BPDCN. Other frequently abnormal chromosomes include 6 and 13.
Rearrangements involving the MYC locus on 8q24 and resulting in MYC protein overexpression have been reported in 38% of BPDCN cases and correlated with so-called immunoblastoid morphology [43]. A subset of patients with MYC rearrangement have a recurrent balanced translocation t(6;8)(p21;q24) [57]. In a report of a single case of BPDCN with t(6;8)(p21;q24), SUPT3H, a TATA-binding protein-associated factors (TAF)-associated protein, was identified as a partner gene [58].
Chromosomal abnormalities associated with myelodysplastic syndrome or acute myeloid leukemia with myelodysplasia-related changes are identified often in BPDCN. These include − 5 or del(5q), − 7 or del(7q), del(9q), del(11q), del(12p) and del(13q). [27, 56, 59] Similarly, array comparative genomic hybridization has demonstrated frequent deletions involving chromosomes 4q34.1-4q34.2, 9p13.2-9p11.2, 9q12-9q34.3, and 13q12.11-13q31.1 [60].
Mutation profiling of BPDCN using next-generation sequencing techniques has demonstrated mutations involving TET2, ASXL1, NRAS, and ATM [27, 39, 61, 62]. Additional mutations identified less commonly involve APC, BRAF, IDH2, KIT, KRAS, MET, MLH1, RB1, RET, TP53, and VHL. NPM1 mutations have been reported rarely in BPDCN [61, 63], but other series have reported no cases with NPM1 mutations [62, 64]. An unpublished BPDCN series from The University of Texas MD Anderson Cancer Center had no cases with NPM1 mutations [39].
Therapeutic Approaches and Prognosis
Although the initial presentation of cutaneous lesions may appear to be indolent, BPDCN is a highly aggressive malignancy with rapid systemic dissemination for which no consensus therapy guidelines are yet available. Accordingly, patients who are diagnosed with BPDCN should be referred for treatement under a clinical trial if feasible. At present, there is no standard therapy for BPDCN, and most published studies are based on retrospective data. Pagano et al. [37] reported that lymphoma regimens including CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) and CHEOP (CHOP plus etoposide) as well as acute lymphoblastic leukemia/lymphoma (ALL) regimens such as hyper-CVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone, and methotrexate and cytarabine) and GIMEMA ALL trial therapy (doxorubicin, vincristine, prednisone, asparaginase), with intrathecal therapy, were associated with significantly better overall survival results compared to acute myeloid leukemia regimens such as MICE (mitoxantrone, cytarabine, etoposide) or ICE (idarubicin, cytarabine, etoposide) for patients with BPDCN. Nonetheless, without stem cell transplant therapy (SCT) the median overall survival is generally dismal [37, 38]. Stem cell transplant therapy, particularly allogeneic SCT, administered during first remission remains the only therapeutic modality that results in durable remissions [65,66,67]. It should be noted that Aoki et al. [66] have reported better outcomes with autologous SCT compared with allogeneic SCT, but those results have not been reproduced by other groups [67].
A number of novel therapies for BPDCN are being investigated. SL-401 (Stemline Therapeutics) is a recombinant protein composed of the catalytic and translocation domains of diptheria toxin (DT) fused via a Met-His linker to IL-3. The payload is delivered in a targeted fashion to CD123-positive cells via IL-3 binding, achieving cytotoxicity through DT-mediated inhibition of protein synthesis [68]. Early results showed promising response rates in BPDCN [69]. The pivotal phase 2 trial of SL-401 in BPDCN has met its primary endpoint (Pemmaraju N. et al.; presented at the Annual Meeting of the European Hematology Association, June 15, 2018).
Other agents targeting CD123 are also being evaluated in phase 1 clinical trials. These include IMGN632 (Immunogen), a conjugate of CD123-targeting antibody with a novel DNA-alkylating payload [70] and a bispecific antibody, XmAb14045 (Xencor), targeting CD123 and CD3. In addition, anti-CD123 chimeric antigen receptor T cell (CAR-T) therapy phase 1 trials for patients with BPDCN are underway.
Other therapeutic approaches have involved agents such as venetoclax, lenalidomide, and bortezomib. BPDCN cells are highly dependent on BCL2 for survival, and they demonstrate in vitro and in vivo sensitivity to BCL2 inhibition with venetoclax [71]. Anecdotal reports of venetoclax therapy for BPDCN patients seems to support its potential effectiveness [71, 72]. Similarly, preclinical data on the activity of lenalidomide [73] and bortezomib [74] in BPDCN are promising, but these agents have yet to be tested clinically. And, although BET inhibition has been shown to be a promising treatment option in preclinical studies [28, 31], this area also remains to be explored in clinical trials.
Conclusions and Future Directions
Recent advances, particularly the identification of the critical role of TCF4 in orchestrating the expression profile and much of the phenotype of BPDCN, have permitted a clearer disctinction between BPDCN and other hematolymphoid malignancies, particularly acute myeloid leukemia. Indeed, TCF4 offers a novel marker that is useful for the diagnosis of BPDCN alongside other more-or-less specific markers such as CD123 and TCL1. Notwithstanding, some patients with BPDCN, particularly those who present with a mostly leukemic disease, still get mislabeled as having acute myeloid leukemia in some community-based settings. The main reason is that commercial reference labs have not all fully embraced including some of the markers of BPDCN, particulary CD123, in their acute leukemia flow cytometry panels.
Patients diagnosed with BPDCN have more treatment options today than they did just a few years ago. Chemotherapy induction with ALL-type regimens remains a mainstay for eligible patients, while allogeneic SCT offers the best chance for durable remission. The results of clinical trials evaluating targeted therapies such as SL-401 offer hope that CD123 offers a therapeutic vulnearability that could augment other therapeutic approaches. As treatment approaches for BPDCN become clearer and more standardized, prognostic modeling to better risk-stratify patients for optimal therapy choices would be warranted. At present our best prognostic markers such as MYC rearrangement status remain incompletely developed and their impact on therapy selection is largely limited.
In view of its rarity and features that overlap with myeloid and lymphoid malignancies, it took until relatively recently to recognize the unique nature of BPDCN and begin to understand its enigmatic characteristics. However, the unprecedented tools for research discovery and drug development available presently have permitted an unprecedented fast-paced unraveling of the biology of BPDCN and are offering promising therapy options for patients with this disease. The collective efforts to fight this aggressive malignancy offer hope and a real-life model of the way forward in the fight against cancer.
References
Kameoka J, Ichinohasama R, Tanaka M, Miura I, Tomiya Y, Takahashi S, et al. A cutaneous agranular CD2- CD4+ CD56+ “lymphoma”: report of two cases and review of the literature. Am J Clin Pathol. 1998;110(4):478–88.
Khoury JD, Medeiros LJ, Manning JT, Sulak LE, Bueso-Ramos C, Jones D. CD56(+) TdT(+) blastic natural killer cell tumor of the skin: a primitive systemic malignancy related to myelomonocytic leukemia. Cancer. 2002;94(9):2401–8.
Brody JP, Allen S, Schulman P, Sun T, Chan WC, Friedman HD, et al. Acute agranular CD4-positive natural killer cell leukemia. Comprehensive clinicopathologic studies including virologic and in vitro culture with inducing agents. Cancer. 1995;75(10):2474–83.
DiGiuseppe JA, Louie DC, Williams JE, Miller DT, Griffin CA, Mann RB, et al. Blastic natural killer cell leukemia/lymphoma: a clinicopathologic study. Am J Surg Pathol. 1997;21(10):1223–30.
Petrella T, Comeau MR, Maynadie M, Couillault G, De Muret A, Maliszewski CR, et al. ‘Agranular CD4+ CD56+ hematodermic neoplasm’ (blastic NK-cell lymphoma) originates from a population of CD56+ precursor cells related to plasmacytoid monocytes. Am J Surg Pathol. 2002;26(7):852–62.
Grouard G, Rissoan MC, Filgueira L, Durand I, Banchereau J, Liu YJ. The enigmatic plasmacytoid T cells develop into dendritic cells with interleukin (IL)-3 and CD40-ligand. J Exp Med. 1997;185(6):1101–11.
Lucio P, Parreira A, Orfao A. CD123hi dendritic cell lymphoma: an unusual case of non-Hodgkin lymphoma. Ann Intern Med. 1999;131(7):549–50.
Chaperot L, Bendriss N, Manches O, Gressin R, Maynadie M, Trimoreau F, et al. Identification of a leukemic counterpart of the plasmacytoid dendritic cells. Blood. 2001;97(10):3210–7.
Collin M, Bigley V. Human dendritic cell subsets: an update. Immunology. 2018;154(1):3–20.
Cella M, Jarrossay D, Facchetti F, Alebardi O, Nakajima H, Lanzavecchia A, et al. Plasmacytoid monocytes migrate to inflamed lymph nodes and produce large amounts of type I interferon. Nat Med. 1999;5(8):919–23.
Sozzani S, Vermi W, Del Prete A, Facchetti F. Trafficking properties of plasmacytoid dendritic cells in health and disease. Trends Immunol. 2010;31(7):270–7.
Swiecki M, Colonna M. Unraveling the functions of plasmacytoid dendritic cells during viral infections, autoimmunity, and tolerance. Immunol Rev. 2010;234(1):142–62.
Takagi H, Arimura K, Uto T, Fukaya T, Nakamura T, Choijookhuu N, et al. Plasmacytoid dendritic cells orchestrate TLR7-mediated innate and adaptive immunity for the initiation of autoimmune inflammation. Sci Rep. 2016;6:24477.
Bjorck P, Leong HX, Engleman EG. Plasmacytoid dendritic cell dichotomy: identification of IFN-alpha producing cells as a phenotypically and functionally distinct subset. J Immunol. 2011;186(3):1477–85.
Soumelis V, Liu YJ. From plasmacytoid to dendritic cell: morphological and functional switches during plasmacytoid pre-dendritic cell differentiation. Eur J Immunol. 2006;36(9):2286–92.
Zhang H, Gregorio JD, Iwahori T, Zhang X, Choi O, Tolentino LL, et al. A distinct subset of plasmacytoid dendritic cells induces activation and differentiation of B and T lymphocytes. Proc Natl Acad Sci U S A. 2017;114(8):1988–93.
Facchetti F, Cigognetti M, Fisogni S, Rossi G, Lonardi S, Vermi W. Neoplasms derived from plasmacytoid dendritic cells. Mod Pathol. 2016;29(2):98–111.
Jing Y, Shaheen E, Drake RR, Chen N, Gravenstein S, Deng Y. Aging is associated with a numerical and functional decline in plasmacytoid dendritic cells, whereas myeloid dendritic cells are relatively unaltered in human peripheral blood. Hum Immunol. 2009;70(10):777–84.
Lennert K, Remmele W. Karyometrische Untersuchungen an Lymphknotenzellen des Menschen: I. Mitt. Germinoblasten, Lymphoblasten und Lymphozyten. Acta Haematol (Basel). 1958;19:99–113.
Nestle FO, Conrad C, Tun-Kyi A, Homey B, Gombert M, Boyman O, et al. Plasmacytoid predendritic cells initiate psoriasis through interferon-alpha production. J Exp Med. 2005;202(1):135–43.
Rollins-Raval MA, Marafioti T, Swerdlow SH, Roth CG. The number and growth pattern of plasmacytoid dendritic cells vary in different types of reactive lymph nodes: an immunohistochemical study. Hum Pathol. 2013;44(6):1003–10.
Vermi W, Lonardi S, Morassi M, Rossini C, Tardanico R, Venturini M, et al. Cutaneous distribution of plasmacytoid dendritic cells in lupus erythematosus. Selective tropism at the site of epithelial apoptotic damage. Immunobiology. 2009;214(9–10):877–86.
Vitte F, Fabiani B, Benet C, Dalac S, Balme B, Delattre C, et al. Specific skin lesions in chronic myelomonocytic leukemia: a spectrum of myelomonocytic and dendritic cell proliferations: a study of 42 cases. Am J Surg Pathol. 2012;36(9):1302–16.
Benet C, Gomez A, Aguilar C, Delattre C, Vergier B, Beylot-Barry M, et al. Histologic and immunohistologic characterization of skin localization of myeloid disorders: a study of 173 cases. Am J Clin Pathol. 2011;135(2):278–90.
Mongkonsritragoon W, Letendre L, Li CY. Multiple lymphoid nodules in bone marrow have the same clonality as underlying myelodysplastic syndrome recognized with fluorescent in situ hybridization technique. Am J Hematol. 1998;59(3):252–7.
Tang Z, Li Y, Wang W, Yin CC, Tang G, Aung PP, et al. Genomic aberrations involving 12p/ETV6 are highly prevalent in blastic plasmacytoid dendritic cell neoplasms and might represent early clonal events. Leuk Res 2018 73:86-94.
Alayed K, Patel KP, Konoplev S, Singh RR, Routbort MJ, Reddy N, et al. TET2 mutations, myelodysplastic features, and a distinct immunoprofile characterize blastic plasmacytoid dendritic cell neoplasm in the bone marrow. Am J Hematol. 2013;88(12):1055–61.
Ceribelli M, Hou ZE, Kelly PN, Huang DW, Wright G, Ganapathi K, et al. A Druggable TCF4- and BRD4-dependent transcriptional network sustains malignancy in blastic plasmacytoid dendritic cell neoplasm. Cancer Cell. 2016;30(5):764–78.
Cisse B, Caton ML, Lehner M, Maeda T, Scheu S, Locksley R, et al. Transcription factor E2-2 is an essential and specific regulator of plasmacytoid dendritic cell development. Cell. 2008;135(1):37–48.
Swiecki M, Colonna M. The multifaceted biology of plasmacytoid dendritic cells. Nat Rev Immunol. 2015;15(8):471–85.
Emadali A, Hoghoughi N, Duley S, Hajmirza A, Verhoeyen E, Cosset FL, et al. Haploinsufficiency for NR3C1, the gene encoding the glucocorticoid receptor, in blastic plasmacytoid dendritic cell neoplasms. Blood. 2016;127(24):3040–53.
Sapienza MR, Fuligni F, Agostinelli C, Tripodo C, Righi S, Laginestra MA, et al. Molecular profiling of blastic plasmacytoid dendritic cell neoplasm reveals a unique pattern and suggests selective sensitivity to NF-kB pathway inhibition. Leukemia. 2014;28(8):1606–16.
Bueno C, Almeida J, Lucio P, Marco J, Garcia R, de Pablos JM, et al. Incidence and characteristics of CD4(+)/HLA DRhi dendritic cell malignancies. Haematologica. 2004;89(1):58–69.
Guru Murthy GS, Pemmaraju N, Atallah E. Epidemiology and survival of blastic plasmacytoid dendritic cell neoplasm. Leuk Res. 2018;73:21–3.
Martin-Martin L, Lopez A, Vidriales B, Caballero MD, Rodrigues AS, Ferreira SI, et al. Classification and clinical behavior of blastic plasmacytoid dendritic cell neoplasms according to their maturation-associated immunophenotypic profile. Oncotarget. 2015;6(22):19204–16.
Loghavi S, Khoury JD. Disseminated blastic plasmacytoid dendritic cell neoplasm. Blood. 2015;126(4):558.
Pagano L, Valentini CG, Pulsoni A, Fisogni S, Carluccio P, Mannelli F, et al. Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study. Haematologica. 2013;98(2):239–46.
Martin-Martin L, Almeida J, Pomares H, Gonzalez-Barca E, Bravo P, Gimenez T, et al. Blastic plasmacytoid dendritic cell neoplasm frequently shows occult central nervous system involvement at diagnosis and benefits from intrathecal therapy. Oncotarget. 2016;7(9):10174–81.
Pemmaraju N, Kantarjian HM, Cortes JE, Duvic M, Khoury JD, Patel K, et al. Blastic plasmacytoid dendritic cell neoplasm (BPDCN): a large single-center experience: analysis of clinical and molecular characteristics and patient outcomes. Blood. 2015;126(23):3746.
Feuillard J, Jacob MC, Valensi F, Maynadie M, Gressin R, Chaperot L, et al. Clinical and biologic features of CD4(+)CD56(+) malignancies. Blood. 2002;99(5):1556–63.
Loghavi S, Khoury JD. Recent updates on chronic myelomonocytic leukemia (2018). Current Hematologic Malignancy Reports 2018.
Julia F, Dalle S, Duru G, Balme B, Vergier B, Ortonne N, et al. Blastic plasmacytoid dendritic cell neoplasms: clinico-immunohistochemical correlations in a series of 91 patients. Am J Surg Pathol. 2014;38(5):673–80.
Sakamoto K, Katayama R, Asaka R, Sakata S, Baba S, Nakasone H, Koike S, Tsuyama N, Dobashi A, Sasaki M, Ichinohasama R, Takakuwa E, Yamazaki R, Takizawa J, Maeda T, Narita M, Izutsu K, Kanda Y, Ohshima K, Takeuchi K Recurrent 8q24 rearrangement in blastic plasmacytoid dendritic cell neoplasm: association with immunoblastoid cytomorphology, MYC expression, and drug response. Leukemia 2018.
Del Giudice I, Matutes E, Morilla R, Morilla A, Owusu-Ankomah K, Rafiq F, et al. The diagnostic value of CD123 in B-cell disorders with hairy or villous lymphocytes. Haematologica. 2004;89(3):303–8.
Munoz L, Nomdedeu JF, Lopez O, Carnicer MJ, Bellido M, Aventin A, et al. Interleukin-3 receptor alpha chain (CD123) is widely expressed in hematologic malignancies. Haematologica. 2001;86(12):1261–9.
Pardanani A, Reichard KK, Zblewski D, Abdelrahman RA, Wassie EA, Morice Ii WG, et al. CD123 immunostaining patterns in systemic mastocytosis: differential expression in disease subgroups and potential prognostic value. Leukemia. 2016;30(4):914–8.
Dzionek A, Sohma Y, Nagafune J, Cella M, Colonna M, Facchetti F, et al. BDCA-2, a novel plasmacytoid dendritic cell-specific type II C-type lectin, mediates antigen capture and is a potent inhibitor of interferon alpha/beta induction. J Exp Med. 2001;194(12):1823–34.
Pellerin A, Otero K, Czerkowicz JM, Kerns HM, Shapiro RI, Ranger AM, et al. Anti-BDCA2 monoclonal antibody inhibits plasmacytoid dendritic cell activation through Fc-dependent and Fc-independent mechanisms. EMBO Mol Med. 2015;7(4):464–76.
Boiocchi L, Lonardi S, Vermi W, Fisogni S, Facchetti F. BDCA-2 (CD303): a highly specific marker for normal and neoplastic plasmacytoid dendritic cells. Blood. 2013;122(2):296–7.
Marafioti T, Paterson JC, Ballabio E, Reichard KK, Tedoldi S, Hollowood K, et al. Novel markers of normal and neoplastic human plasmacytoid dendritic cells. Blood. 2008;111(7):3778–92.
Jegalian AG, Buxbaum NP, Facchetti F, Raffeld M, Pittaluga S, Wayne AS, et al. Blastic plasmacytoid dendritic cell neoplasm in children: diagnostic features and clinical implications. Haematologica. 2010;95(11):1873–9.
Cota C, Vale E, Viana I, Requena L, Ferrara G, Anemona L, et al. Cutaneous manifestations of blastic plasmacytoid dendritic cell neoplasm-morphologic and phenotypic variability in a series of 33 patients. Am J Surg Pathol. 2010;34(1):75–87.
Johnson RC, Kim J, Natkunam Y, Sundram U, Freud AG, Gammon B, et al. Myeloid cell nuclear differentiation antigen (MNDA) expression distinguishes extramedullary presentations of myeloid leukemia from Blastic Plasmacytoid dendritic cell neoplasm. Am J Surg Pathol. 2016;40(4):502–9.
Facchetti F, Vermi W, Santoro A, Vergoni F, Chilosi M, Doglioni C. Neoplasms derived from plasmacytoid monocytes/interferon-producing cells: variability of CD56 and granzyme B expression. Am J Surg Pathol. 2003;27(11):1489–92 author reply 92-3.
Dargent JL, Delannoy A, Pieron P, Husson B, Debecker C, Petrella T. Cutaneous accumulation of plasmacytoid dendritic cells associated with acute myeloid leukemia: a rare condition distinct from blastic plasmacytoid dendritic cell neoplasm. J Cutan Pathol. 2011;38(11):893–8.
Tang Z, Tang G, Wang SA, Lu X, Young KH, Bueso-Ramos CE, et al. Simultaneous deletion of 3’ETV6 and 5’EWSR1 genes in blastic plasmacytoid dendritic cell neoplasm: case report and literature review. Mol Cytogenet. 2016;9:23.
Sumarriva Lezama L, Chisholm KM, Carneal E, Nagy A, Cascio MJ, Yan J, Chang CC, Cherry A, George TI, Ohgami RS An analysis of blastic plasmacytoid dendritic cell neoplasm with translocations involving the MYC locus identifies t(6;8)(p21;q24) as a recurrent cytogenetic abnormality. Histopathology 2018.
Nakamura Y, Kayano H, Kakegawa E, Miyazaki H, Nagai T, Uchida Y, et al. Identification of SUPT3H as a novel 8q24/MYC partner in blastic plasmacytoid dendritic cell neoplasm with t(6;8)(p21;q24) translocation. Blood Cancer J. 2015;5:e301.
Leroux D, Mugneret F, Callanan M, Radford-Weiss I, Dastugue N, Feuillard J, et al. CD4(+), CD56(+) DC2 acute leukemia is characterized by recurrent clonal chromosomal changes affecting 6 major targets: a study of 21 cases by the Groupe Francais de Cytogenetique Hematologique. Blood. 2002;99(11):4154–9.
Dijkman R, van Doorn R, Szuhai K, Willemze R, Vermeer MH, Tensen CP. Gene-expression profiling and array-based CGH classify CD4+CD56+ hematodermic neoplasm and cutaneous myelomonocytic leukemia as distinct disease entities. Blood. 2007;109(4):1720–7.
Menezes J, Acquadro F, Wiseman M, Gomez-Lopez G, Salgado RN, Talavera-Casanas JG, et al. Exome sequencing reveals novel and recurrent mutations with clinical impact in blastic plasmacytoid dendritic cell neoplasm. Leukemia. 2014;28(4):823–9.
Stenzinger A, Endris V, Pfarr N, Andrulis M, Johrens K, Klauschen F, et al. Targeted ultra-deep sequencing reveals recurrent and mutually exclusive mutations of cancer genes in blastic plasmacytoid dendritic cell neoplasm. Oncotarget. 2014;5(15):6404–13.
Suma S, Sakata-Yanagimoto M, Nguyen TB, Hattori K, Sato T, Noguchi M, et al. Blastic plasmacytoid dendritic cell neoplasm arising from clonal hematopoiesis. Int J Hematol. 2018;108:447–51.
Facchetti F, Pileri SA, Agostinelli C, Martelli MP, Paulli M, Venditti A, et al. Cytoplasmic nucleophosmin is not detected in blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2009;94(2):285–8.
Roos-Weil D, Dietrich S, Boumendil A, Polge E, Bron D, Carreras E, et al. Stem cell transplantation can provide durable disease control in blastic plasmacytoid dendritic cell neoplasm: a retrospective study from the European Group for Blood and Marrow Transplantation. Blood. 2013;121(3):440–6.
Aoki T, Suzuki R, Kuwatsuka Y, Kako S, Fujimoto K, Taguchi J, et al. Long-term survival following autologous and allogeneic stem cell transplantation for blastic plasmacytoid dendritic cell neoplasm. Blood. 2015;125(23):3559–62.
Kharfan-Dabaja MA, Al Malki MM, Deotare U, Raj RV, El-Jurdi N, Majhail N, et al. Haematopoietic cell transplantation for blastic plasmacytoid dendritic cell neoplasm: a north American multicentre collaborative study. Br J Haematol. 2017;179(5):781–9.
Angelot-Delettre F, Roggy A, Frankel AE, Lamarthee B, Seilles E, Biichle S, et al. In vivo and in vitro sensitivity of blastic plasmacytoid dendritic cell neoplasm to SL-401, an interleukin-3 receptor targeted biologic agent. Haematologica. 2015;100(2):223–30.
Frankel AE, Woo JH, Ahn C, Pemmaraju N, Medeiros BC, Carraway HE, et al. Activity of SL-401, a targeted therapy directed to interleukin-3 receptor, in blastic plasmacytoid dendritic cell neoplasm patients. Blood. 2014;124(3):385–92.
Kovtun Y, Jones GE, Adams S, Harvey L, Audette CA, Wilhelm A, et al. A CD123-targeting antibody-drug conjugate, IMGN632, designed to eradicate AML while sparing normal bone marrow cells. Blood Adv. 2018;2(8):848–58.
Montero J, Stephansky J, Cai T, Griffin GK, Cabal-Hierro L, Togami K, et al. Blastic plasmacytoid dendritic cell neoplasm is dependent on BCL2 and sensitive to venetoclax. Cancer Discov. 2017;7(2):156–64.
Grushchak S, Joy C, Gray A, Opel D, Speiser J, Reserva J, et al. Novel treatment of blastic plasmacytoid dendritic cell neoplasm: a case report. Medicine (Baltimore). 2017;96(51):e9452.
Agliano A, Martin-Padura I, Marighetti P, Gregato G, Calleri A, Prior C, et al. Therapeutic effect of lenalidomide in a novel xenograft mouse model of human blastic NK cell lymphoma/blastic plasmacytoid dendritic cell neoplasm. Clin Cancer Res. 2011;17(19):6163–73.
Philippe L, Ceroi A, Bole-Richard E, Jenvrin A, Biichle S, Perrin S, et al. Bortezomib as a new therapeutic approach for blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2017;102(11):1861–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joseph D. Khoury has received research funding from Stemline Therapeutics.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Molecular Testing and Diagnostics
Rights and permissions
About this article
Cite this article
Khoury, J.D. Blastic Plasmacytoid Dendritic Cell Neoplasm. Curr Hematol Malig Rep 13, 477–483 (2018). https://doi.org/10.1007/s11899-018-0489-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-018-0489-z