Abstract
Purpose of Review
Over the past two decades, the introduction of tyrosine kinase inhibitors (TKIs) has transformed the treatment of chronic myeloid leukemia (CML). With four agents currently approved for frontline use in chronic-phase (CP) disease, it follows that treatment decision-making has been rendered more challenging. Here we will review recent advances that help inform the selection of a first-line TKI.
Recent Findings
Extended follow-up of the seminal CML trials has demonstrated the long-term efficacy of TKIs, while also highlighting significant differences in their respective toxicity profiles and potency. Dasatinib and nilotinib generate deeper molecular responses than imatinib, particularly among patients with higher risk disease, but this has not translated into a significant survival advantage. Similar results have been obtained at 1 year with bosutinib; its efficacy and toxicity were well balanced at a dose of 400 mg daily, prompting its recent approval for this indication. Lastly, multiple studies have demonstrated that TKIs can be safely discontinued in select individuals who have maintained deep responses for extended periods, establishing treatment-free remission as a novel goal in CP CML.
Summary
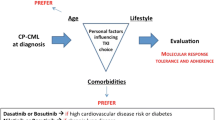
The careful consideration of parameters such as disease risk, the potency, and toxicity profile of each TKI, as well as each patient’s unique comorbidities and preferences, enables truly individualized therapeutic decision-making in CP CML, with the goal of ensuring that a high quality of life accompanies the survival advantage conferred by these agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myeloid leukemia (CML) is a clonal stem cell neoplasm characterized by the universal presence of the Philadelphia chromosome (Ph), the product of a reciprocal translocation that juxtaposes the c-ABL1 oncogene on chromosome 9q34 and the housekeeping gene BCR on chromosome 22q11 [1, 2]. The resulting BCR-ABL fusion protein has dysregulated tyrosine kinase activity which drives uncontrolled proliferation in the granulocytic lineage [3, 4]. In the absence of treatment, CML classically follows a triphasic clinical course as it progresses from an indolent chronic phase (CP), characterized by leukocytosis and splenomegaly, to an accelerated phase (AP), where the disease takes on aggressive features such as increased circulating blasts, difficult to control blood counts, or additional cytogenetic abnormalities, and ultimately onto a terminal blast crisis (BC), where myeloid or lymphoid blasts proliferate uncontrollably, similar to acute leukemia [5].
BCR-ABL is both necessary and sufficient for the development of CML, and appreciation of this unique pathophysiology spurred the development of tyrosine kinase inhibitors (TKIs), small molecules designed to specifically inhibit this fusion protein. The introduction of imatinib, and subsequently the second- and third-generation TKIs, has revolutionized the treatment of CML, with survival in chronic-phase patients now approaching that of age-matched controls. With four agents currently approved for the frontline treatment of CP CML, clinicians are left with an embarrassment of riches, and a challenging decision regarding which drug to start in a given patient. This review will discuss each of the TKIs approved for frontine use in CP CML, highlighting key advances that help inform the clinical decision-making process.
TKIs Studied in the Frontline Setting
Imatinib
Imatinib mesylate (Gleevec, formerly STI571) is a 2-phenylaminopyrimidine molecule which targets the ATP-binding site of the ABL kinase domain, acting as a competitive inhibitor. In addition to c-ABL and BCR-ABL, it also potently inhibits the PDGFR (platelet-derived growth factor receptor), and c-KIT kinases [6]. Imatinib binds to the inactive conformation of the ABL kinase domain, contacting 21 amino acids within a tight pocket [7]. Following demonstration of its activity against CML in pre-clinical studies and early phase clinical trials, imatinib was evaluated in the seminal phase III International Randomized Study of Interferon and STI571 (IRIS) [8]. This trial randomized newly diagnosed CP CML patients to receive either imatinib 400 mg once daily or combination therapy with interferon alpha (IFN-α) and low-dose cytarabine (ara-C), the standard of care at that time. At 18 months, the estimated rate of complete cytogenetic response (CCyR, the absence of the Philadelphia chromosome among 20 evaluable bone marrow metaphases) was markedly different between the two treatment groups—76.2% in imatinib-treated patients versus 14.5% in those receiving IFN-α/ara-C. Additionally, the rate of freedom from progression to AP and BC was 96.7% in the imatinib arm compared to 91.5% with combination therapy [8]. The long-term efficacy of imatinib has been highlighted in the recently published 10-year follow-up of IRIS, where patients randomized to receive TKI had an overall survival of 83% and an estimated rate of freedom from progression of 92% [9••].
While IRIS established imatinib as a new standard of care for the frontline treatment of CP CML, a small proportion of patients do progress on therapy, secondary to either compliance issues or the development of resistance, most often via point mutations in the ABL kinase domain [10, 11]. Given that these mutations act to reduce imatinib’s binding affinity, a mechanism that could potentially be overcome by increased drug concentrations, several clinical trials have compared higher doses of imatinib to the standard dose of 400 mg daily. These showed no consistent differences in remission rates or survival, but high-dose imatinib was invariably associated with increased toxicity [12,13,14,15].
Dasatinib
Dasatinib (Sprycel) is a second-generation TKI structurally unrelated to imatinib. It is 325-fold more potent at inhibiting BCR-ABL and exhibits activity against a number of ABL kinase domain point mutants. Dasatinib also targets the SRC family kinases, which have been implicated in imatinib resistance, as well as the c-KIT, PDGFR-α/β, and ephrin receptor tyrosine kinases [16,17,18]. Dasatinib was initially shown to have significant clinical activity in CML patients resistant or intolerant to imatinib [19,20,21]. Subsequently, it was evaluated as a first-line agent in the phase III multicenter Dasatinib versus Imatinib Study in Treatment-Naïve CML Patients (DASISION) trial, which compared once daily dosing of dasatinib (100 mg) to imatinib (400 mg) in patients with newly diagnosed CP CML [22]. At 12 months of follow-up, CCyR, the trial’s primary endpoint, was achieved in 77% of dasatinib patients compared to 66% of those receiving imatinib. Moreover, major molecular responses (MMR, a greater than three-log reduction in BCR-ABL1 transcript levels) were achieved more rapidly and at higher rates (46 vs. 28%) with dasatinib compared to imatinib [22]. In the 5-year update of this trial, dasatinib continued to demonstrate superior rates of CCyR and MMR, but this did not result in significantly improved progression-free or overall survival [23••].
Nilotinib
Nilotinib (Tasigna) is a second-generation TKI that was rationally designed from imatinib’s chemical structure in order to optimize drug binding to BCR-ABL. By improving topological fit into ABL’s ATP-binding site, nilotinib has ~ 30-fold greater potency than imatinib, with improved selectivity [24]. Compared to imatinib, it exhibits decreased activity against the KIT and PDGFR tyrosine kinases, but can potently inhibit a number of BCR-ABL kinase domain point mutants [17]. Following demonstration of its clinical activity in imatinib-resistant/imatinib-intolerant patients [24,25,26], nilotinib was evaluated in the phase III ENESTnd (Evaluating Nilotinib Efficacy and Safety in Clinical Trials-newly diagnosed patients) study. CP patients were randomized into three groups: nilotinib 300 mg twice daily (BID), nilotinib 400 mg BID, or imatinib 400 mg once daily. At 12 months, patients receiving either nilotinib dose achieved higher rates of MMR, the trial’s primary endpoint (44% for 300 mg BID, 43% for 400 mg BID, 22% for imatinib), as well as improved time to progression to AP/BC [27]. At 5 years of follow-up, nilotinib continued to show higher rates of MMR; however, similar to dasatinib in DASISION, this did not result in substantially improved progression-free or overall survival [28••].
Of note, in ENESTnd, nilotinib at a dose of 400 mg BID resulted in increased toxicity compared to 300 mg BID. At 5 years of follow-up, serious adverse events arose in 33% of patients at the higher nilotinib dose compared to 26% at the lower dose. Particularly notable were the rates of cardiovascular events, which occurred in 13.4% of patients in the 400 mg BID arm compared to 7.5% in the 300 mg BID arm and 2.1% in the imatinib arm [28••]. In light of this toxicity profile and the aforementioned efficacy findings, 300 mg BID is the recommended starting dose of nilotinib in newly diagnosed CP patients [29••, 30••].
Bosutinib
Bosutinib (Bosulif) is a 4-anilino-3-quinolinecarbonitrile molecule, structurally unrelated to imatinib. It was originally developed as a SRC inhibitor, but was subsequently found to inhibit BCR-ABL with greater potency than imatinib while lacking activity against PDGFR-α/β and c-KIT [31, 32]. Similar to dasatinib, bosutinib can bind to the active and inactive conformations of the ABL kinase domain and inhibit a number of kinase domain mutants [33]. Bosutinib has been studied as a frontline agent in CP CML in two phase III trials. The first, BELA (Bosutinib Efficacy and Safety in Newly Diagnosed Chronic Myeloid Leukemia), compared bosutinib 500 mg once daily to imatinib 400 mg. This trial’s primary endpoint was not met, as bosutinib did not exhibit superior rates of CCyR at 12 months (70% for bosutinib vs. 68% for imatinib), though secondary analyses did show higher rates of MMR at 12 and 24 months, as well as shorter times to these molecular milestones with bosutinib [34, 35]. Of note, early gastrointestinal and hepatic toxicity led to higher rates of treatment discontinuation in the bosutinib arm, which likely impacted efficacy outcomes.
In a follow-up phase III study (BFORE, Bosutinib Trial in First-Line Chronic Myelogenous Leukemia Treatment), a lower dose of bosutinib (400 mg once daily) was compared to imatinib in newly diagnosed CP patients [36••]. In this trial, bosutinib achieved its primary endpoint, a higher rate of MMR at 12 months than imatinib (47 vs. 37%), while also resulting in significantly higher rates of CCyR and shorter times to these milestones. In BFORE, drug discontinuation occurred less frequently with bosutinib than imatinib (22 vs. 27%) [36••]. Thus, with this lower dose, bosutinib provided an effective balance of efficacy and toxicity, and on the strength of the BFORE data, bosutinib 400 mg daily was approved for the frontline treatment of CP CML by the FDA in December 2017 [37].
TKIs Not Approved for Frontline Therapy—Ponatinib
Ponatinib (Iclusig) was designed to overcome the T315I “gatekeeper” mutation, which confers resistance to imatinib, dasatinib, nilotinib, and bosutinib [10, 17]. As a result of its unique structure, ponatinib can form a hydrophobic interaction with the isoleucine-315 side chain, enabling it to bind to and inhibit the kinase activity of T315I BCR-ABL. Ponatinib also inhibits all other documented BCR-ABL kinase domain mutants, as well as SRC, VEGF, FGFR, and PDGFR kinase family members [38].
Early phase clinical trials, most notably the phase II Ponatinib Ph+ ALL and CML Evaluation (PACE) study, clearly established ponatinib’s clinical activity in CML patients with resistance/intolerance to earlier generation TKIs or T315I mutations [39, 40]. Subsequently, it was evaluated as a frontline agent in EPIC (Evaluation of Ponatinib versus Imatinib in CML) trial, a phase III study that randomized newly diagnosed CP CML patients to receive ponatinib 45 mg once daily or imatinib 400 mg once daily [41]. However, EPIC was terminated prematurely due to reports of high rates of myocardial infarction, stroke, and peripheral vascular disease during the extended follow-up of the early phase clinical trials involving ponatinib. Particularly notable were results from PACE, where by 5 years, 29% of patients had experienced arterial occlusion events [42•]. When EPIC was halted, only 23 patients had completed 12 months of follow-up; consequently, the superiority of ponatinib with respect to the trial’s primary endpoint, MMR at 12 months, could not be established [41]. As such, ponatinib is currently not approved as a first-line agent for CP CML, but plays an important role as a second-line agent for T315I-mutant disease, albeit with careful evaluation of cardiovascular risk prior to drug initiation. Several studies evaluating the efficacy and risk profile of lower doses of ponatinib in TKI-resistant patients are currently underway. These include OPTIC, a phase II trial comparing three different starting doses of ponatinib (15 mg/day, 30 mg/day, and 45 mg/day); OPUS, a phase II trial where ponatinib is initiated at 30 mg/day, then reduced to 15 mg/day upon achievement of MMR; and OPTIC-2L, a phase III trial comparing nilotinib 400 mg twice daily to ponatinib 15 mg/day and 30 mg/day.
Choice of TKI in the Frontline Setting
At present, based on data from the aforementioned phase III clinical trials, four TKIs are approved for the frontline therapy of chronic-phase CML: imatinib, dasatinib, nilotinib, and most recently, bosutinib (Table 1). When selecting an agent for upfront therapy, several factors must be taken into consideration including disease risk, the toxicity profiles of each TKI, and their interaction with patient comorbidities, as well as drug availability, cost, and ease of administration.
Disease Risk
The Sokal and Hasford (Euro) prognostic scoring systems have historically been used to stratify CP CML patients into low-, intermediate-, and high-risk groups by integrating clinical parameters from the time of presentation, including patient age, spleen size, and CBC indices [43, 44]. Though developed prior to the introduction of TKIs, they do predict outcome in imatinib-treated patients; for example, in IRIS, patients with a high Sokal score had lower overall survival at 10 years (69%) compared to those with intermediate (80%) or low scores (90%) [9••]. Notably, in the ENESTnd and DASISION trials, individuals with intermediate- or high-risk disease had higher rates of MMR and less progression to AP/BC when treated with second-generation TKIs compared to imatinib [23••, 28••]. While this has not translated into statistically significant survival improvements in these studies, dasatinib and nilotinib are generally considered to be preferable alternatives to imatinib as first-line therapy in these populations [30••]. While the clinical data for bosutinib is less mature at this time, 1-year follow-up of the BFORE trial has similarly shown higher rates of MMR with bosutinib treatment, an effect that was most pronounced among high-risk Sokal patients (34% with bosutinib vs. 17% with imatinib) [36••]. Based on this preliminary data, recent clinical guidelines have included it alongside the other second-generation agents as a preferable alternative to imatinib as frontline therapy in intermediate- and high-risk patients [30••].
Moving forward, our understanding of disease risk in CP CML will continue to evolve as novel biological and molecular features that predict patient outcome on TKI therapy are identified. For example, BCR-ABL1 transcript type has been suggested as a factor that can influence patient outcomes, as individuals with the e13a2 (b2a2) transcript have been shown to have lower and slower MMR rates and inferior survival compared to those with the e14a2 (b3a2) transcript [45, 46]. However, this association has not been consistently replicated across studies [47, 48]. As such, it has not been integrated into prognostic scoring systems in routine clinical practice at this time, and the the Sokal and Hasford systems remain the recommended tools to inform frontline TKI selection [30••].
Interplay Between TKI Toxicity Profiles and Patient Comorbidities
The first- and second-generation TKIs share numerous class-wide side effects, including myelosuppression, rash, myalgia/arthralgia, fluid retention, and liver toxicity. However, there are notable differences in their toxicity profiles (Table 1), which, depending on their interaction with pre-existing comorbidities, can influence suitability for a given patient.
Clinical trial data has established a clear association between dasatinib and pulmonary toxicity. In DASISION, pleural effusion was reported in 28% of patients receiving dasatinib versus 0.8% of those receiving imatinib after 5 years of follow-up. Moreover, pulmonary arterial hypertension was identified as a serious late complication, as it was diagnosed in 5% of dasatinib-treated patients compared to 0.4% of imatinib-treated patients [23••]. While all the frontline TKIs have been associated with bleeding, this risk is most profound with dasatinib, thought to be attributable to drug-induced platelet dysfunction. Bleeding has been reported in up to 20–25% of patients receiving dasatinib and typically involves the GI tract or mucosal surfaces and occurs in the setting of concomitant thrombocytopenia [49, 50].
Nilotinib also has a set of toxicities distinct from the other TKIs approved for frontline use, including several related to an increased risk of cardiovascular disease. In ENESTnd, new or worsening elevations of total cholesterol and blood glucose occurred in 27 and 51% of nilotinib-treated patients, respectively [28••]. Cardiovascular events occurred in 10.4% of patients receiving nilotinib versus 2.1% of those receiving imatinib, and peripheral artery occlusion was exclusively seen with nilotinib, affecting 2.5% of individuals [28••]. Nilotinib can also cause QT prolongation with rare reports of sudden cardiac death. Hence, ECGs should be obtained at baseline and periodically thereafter, the concomitant usage of medications that likewise prolong the QT should be avoided, and careful monitoring is required if a drug capable of inhibiting CYP3A4 is initiated, as this can increase nilotinib levels. Lastly, nilotinib can lead to elevations in serum lipase and on occasion cause overt pancreatitis, particularly among patients with a prior history.
In the BFORE trial, where bosutinib was initiated at a dose of 400 mg daily, its major side effects were gastrointestinal, in particular diarrhea (70% of bosutinib-treated patients vs. 34% with imatinib), which was typically mild and short-lived. Bosutinib also caused notable hepatotoxicity, with more frequent elevations in ALT (31 vs. 6%) and AST (23 vs. 6%). Conversely, it was associated with less neutropenia, myalgia/arthralgia, and peripheral edema than imatinib and displayed no signal for increased rates of pleural effusion, pulmonary hypertension, or peripheral artery occlusion [36••].
Given the unique toxicity profiles of each of the TKIs approved for frontline treatment, a thorough assessment of relevant comorbidities is crucial for guiding drug selection [30••, 51]. In practice, imatinib is generally considered to have the mildest side effect profile of the TKIs approved for frontline use. Dasatinib should be used with caution in patients with pre-existing lung disease or pleural effusion, as well as in individuals on antiplatelet/anticoagulant medications or with a history of bleeding. For nilotinib, a careful evaluation of cardiovascular risk is required prior to its initiation, and alternative agents should be strongly considered in patients with a history of cardiovascular disease or pancreatitis. Hepatotoxicity is a class-wide TKI toxicity, but among the second-generation agents, this is least pronounced with dasatinib; consequently, it may be preferable to nilotinib and bosutinib in patients with a history of liver disease. Given that these comorbidities are common among the CML patient population, they require careful attention during frontline TKI selection in an effort to reduce the occurrence of serious adverse events [52].
Additional Considerations
In addition to efficacy and toxicity, several practical factors require consideration during the selection of a first-line TKI, including ease of administration and drug availability/cost. Regarding the former, compared to the other approved agents, nilotinib has notable differences in its pharmacokinetics. Not only is it dosed twice daily, but concurrent food intake variably influences its absorption [53]. Consequently, it is recommended that nilotinib be taken on an empty stomach, with no food for 2 h before and 1 h after each dose, a schedule that can prove challenging to patients [54].
While the introduction of imatinib and other TKIs has been transformative with respect to patient outcomes in CML, this comes at a significant financial burden, as branded imatinib, dasatinib, and nilotinib have average wholesale prices in the range of $150,000 USD per year [55]. Given the emerging evidence supporting a relationship between higher out-of-pocket costs and decreased patient adherence [56, 57], addressing the affordability of CML care is a priority moving forward. The approval of generic versions of imatinib is one potential solution. Observational studies have demonstrated comparable efficacy to the branded drug [58,59,60]; thus, this may emerge as a cost-effective strategy, contingent upon the expected drop in drug price upon their introduction to the market [55, 61].
Response Monitoring and Milestones
Following TKI initiation, patient response is monitored by periodic complete blood counts and quantification of BCR-ABL1 transcript levels every 3 months, preferably in a laboratory that utilizes the International Scale (IS), enabling standardization of results [29••, 30••, 62]. Historically, bone marrow examination has formed a key component of evaluating response in CP CML and has been performed until achievement of a CCyR. However, given that a two-log reduction in BCR-ABL1 transcript levels roughly equates to a CCyR, many centers have moved towards only performing bone marrow cytogenetics after initial diagnosis in the setting of suspected treatment failure [30••, 63, 64].
The National Comprehensive Cancer Network (NCCN) and European LeukemiaNet (ELN) have outlined molecular response milestones at various timepoints after the initiation of therapy [29••, 30••]. Central to both is the prognostic value of achieving a CCyR (or alternatively a BCR-ABL1 transcript level of < 1%) by 12 months, with the inability to reach this milestone considered overt treatment failure. However, they differ slightly in the emphasis placed on early molecular responses (EMR), defined as a 3-month BCR-ABL1 transcript level < 10%. EMR has been shown to independently predict survival in numerous trials, including DASISION and ENESTnd [65,66,67]; however, other studies have suggested that re-assessing response at 6 months in individuals not achieving EMR may provide a better prediction of patient outcome [68, 69]. As such, the ELN guidelines consider the inability to reach EMR as a “warning” which warrants close monitoring. Conversely, the NCCN states that failure to reach EMR can be considered as impetus for treatment modification at 3 months. However, in keeping with recent studies suggesting that the rate of BCR-ABL1 transcript decline may in fact carry greater prognostic significance than an EMR [70, 71], they comment that prior to making significant changes to treatment strategy based on a 3-month measurement, the kinetics of transcript decline should be considered [30••].
The common elements used to define treatment failure in the ELN and NCCN guidelines are outlined in Table 2. In these instances, prompt clinical evaluation is warranted, including an assessment of patient compliance, potential drug interactions and bone marrow cytogenetics, as well as molecular testing for BCR-ABL1 kinase domain mutations. A detailed discussion of TKI therapy beyond the first-line is beyond the scope of this review, but has been covered elsewhere [72]. Briefly, dasatinib, nilotinib, bosutinib, ponatinib, and high-dose imatinib can all be utilized for second-line treatment and beyond, though the latter is not recommended after failure of a second-generation TKI. In the setting of drug intolerance, an agent with a potentially more favorable side effect profile should be selected; for example, in individuals with significant edema and/or gastrointestinal discomfort on imatinib, nilotinib may prove more tolerable. As discussed above, disease resistance frequently develops due to the acquisition of tyrosine kinase domain mutations; as such, in this setting, second-line agents should be selected based on a balance between their activity against the mutation in question and alignment with patient comorbidities. Importantly, T315I mutations confer resistance to all TKIs except ponatinib, restricting treatment options to this agent, the protein synthesis inhibitor omacetaxine, or allogeneic stem cell transplant [30••].
TKI Discontinuation
Traditionally, TKIs are taken indefinitely by CML patients following their initiation, but much recent investigation has focused upon assessing the safety of their discontinuation in patients who have maintained deep molecular responses over extended periods of time. This was first evaluated in the Stop Imatinib (STIM-1) trial, where 100 patients with undetectable molecular residual disease (UMRD) for at least 2 years discontinued drug with close molecular monitoring [73]. One year after imatinib discontinuation, 41% of patients remained in molecular remission. In a recent update of this trial, where patients were followed for a median of greater than 6 years, there was no evidence of late recurrences, with the majority occurring within 6 months of discontinuation. Importantly, resumption of imatinib post-relapse resulted the re-establishment of UMRD in 55 of 57 patients [74••]. Several other prospective studies studying the discontinuation of imatinib or second-generation TKIs in comparable patient populations have generated similar results [75,76,77,78]. Across all of these, the length of exposure to TKI therapy and the duration of deep molecular response prior to treatment discontinuation have emerged as consistent predictors of the ability to achieve an extended treatment-free remission (TFR). Interestingly, there is emerging evidence supporting a role for the immune system in maintaining TFRs, as both increased numbers of natural killer and low numbers of CD86+ plasmacytoid dendritic cells have been found to correlate with the likelihood of successful TKI discontinuation [79,80,81].
Thus, recent clinical trial data has established that with close monitoring, TKIs can be safely discontinued in select CP CML patients, with the hope of obtaining extended TFRs. According to recent NCCN guidelines, CP CML patients with a four-log reduction in BCR-ABL1 transcript levels for greater than 2 years are eligible to attempt TKI discontinuation, with a strict schedule of molecular monitoring during follow-up [30••]. In addition to ameliorating quality of life by allowing for drug holidays, TFRs will also prove particularly useful in CML patients considering pregnancy, where the use of TKIs is contraindicated.
Conclusions
The introduction of imatinib and the later generation TKIs has revolutionized the treatment of CML, rendering the survival of CP patients comparable to that of age-matched controls. Four agents are currently approved for the frontline treatment of CP CML, enabling physicians to make highly individualized treatment decisions which balance disease risk, drug side effects, and patient comorbidities. However, despite these successes, challenges do remain, including how best to manage the acute and chronic toxicities associated with these agents. TFR has emerged as a novel goal of CML therapy in the TKI era, bringing renewed focus upon how best to achieve deep, sustained molecular responses. In the hope of reaching this objective, we excitedly await results from studies evaluating ABL001, a novel allosteric inhibitor of BCR-ABL, as well as combination therapies, where TKIs are partnered with a second agent such as IFN-α or the JAK1/2 inhibitor ruxolitinib. Moving forward, we aspire to build upon the incredible progress of the past two decades by continuing to redefine treatment approaches and patient outcomes in CML.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Rowley JD. Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973;243:290–3.
Konopka JB, Watanabe SM, Witte ON. An alteration of the human c-abl protein in K562 leukemia cells unmasks associated tyrosine kinase activity. Cell. 1984;37:1035–42.
Pear WS, Miller JP, Xu L, Pui JC, Soffer B, Quackenbush RC, et al. Efficient and rapid induction of a chronic myelogenous leukemia-like myeloproliferative disease in mice receiving P210 bcr/abl-transduced bone marrow. Blood. 1998;92:3780–92.
Faderl S, Talpaz M, Estrov Z, O’Brien S, Kurzrock R, Kantarjian HM. The biology of chronic myeloid leukemia. N Engl J Med. 1999;341:164–72.
Buchdunger E, Zimmermann J, Mett H, Meyer T, Müller M, Druker BJ, et al. Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo by a 2-phenylaminopyrimidine derivative. Cancer Res. 1996;56:100–4.
Nagar B, Bornmann WG, Pellicena P, Schindler T, Veach DR, Miller WT, et al. Crystal structures of the kinase domain of c-Abl in complex with the small molecule inhibitors PD173955 and imatinib (STI-571). Cancer Res. 2002;62:4236–43.
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348:994–1004.
•• Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP, et al. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376:917–27. Ten-year update of the seminal IRIS clinical trial—reinforces the long-term efficacy and safety of imatinib in the frontline treatment of CP CML.
Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN, et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 2001;293:876–80.
von Bubnoff N, Schneller F, Peschel C, Duyster J. BCR-ABL gene mutations in relation to clinical resistance of Philadelphia-chromosome-positive leukaemia to STI571: a prospective study. Lancet. 2002;359:487–91.
Baccarani M, Rosti G, Castagnetti F, Haznedaroglu I, Porkka K, Abruzzese E, et al. Comparison of imatinib 400 mg and 800 mg daily in the front-line treatment of high-risk, Philadelphia-positive chronic myeloid leukemia: a European LeukemiaNet Study. Blood. 2009;113:4497–504.
Cortes JE, Baccarani M, Guilhot F, Druker BJ, Branford S, Kim D-W, et al. Phase III, randomized, open-label study of daily imatinib mesylate 400 mg versus 800 mg in patients with newly diagnosed, previously untreated chronic myeloid leukemia in chronic phase using molecular end points: tyrosine kinase inhibitor optimization and selectivity study. J Clin Oncol Off J Am Soc Clin Oncol. 2010;28:424–30.
Deininger MW, Kopecky KJ, Radich JP, Kamel-Reid S, Stock W, Paietta E, et al. Imatinib 800 mg daily induces deeper molecular responses than imatinib 400 mg daily: results of SWOG S0325, an intergroup randomized PHASE II trial in newly diagnosed chronic phase chronic myeloid leukaemia. Br J Haematol. 2014;164:223–32.
Kalmanti L, Saussele S, Lauseker M, Müller MC, Dietz CT, Heinrich L, et al. Safety and efficacy of imatinib in CML over a period of 10 years: data from the randomized CML-study IV. Leukemia. 2015;29:1123–32.
Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL. Overriding imatinib resistance with a novel ABL kinase inhibitor. Science. 2004;305:399–401.
O’Hare T, Walters DK, Stoffregen EP, Jia T, Manley PW, Mestan J, et al. In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res. 2005;65:4500–5.
Donato NJ, Wu JY, Stapley J, Gallick G, Lin H, Arlinghaus R, et al. BCR-ABL independence and LYN kinase overexpression in chronic myelogenous leukemia cells selected for resistance to STI571. Blood. 2003;101:690–8.
Hochhaus A, Baccarani M, Deininger M, Apperley JF, Lipton JH, Goldberg SL, et al. Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia. 2008;22:1200–6.
Apperley JF, Cortes JE, Kim D-W, Roy L, Roboz GJ, Rosti G, et al. Dasatinib in the treatment of chronic myeloid leukemia in accelerated phase after imatinib failure: the START a trial. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27:3472–9.
Cortes J, Rousselot P, Kim D-W, Ritchie E, Hamerschlak N, Coutre S, et al. Dasatinib induces complete hematologic and cytogenetic responses in patients with imatinib-resistant or -intolerant chronic myeloid leukemia in blast crisis. Blood. 2007;109:3207–13.
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2010;362:2260–70.
•• Cortes JE, Saglio G, Kantarjian HM, Baccarani M, Mayer J, Boqué C, et al. Final 5-year study results of DASISION: the dasatinib versus imatinib study in treatment-naïve chronic myeloid leukemia patients trial. J Clin Oncol Off J Am Soc Clin Oncol. 2016;34:2333–40. Five-year follow-up of the DASISION trial showing that dasatinib results in deeper molecular responses than imatinib, without conferring a significant survival advantage.
Weisberg E, Manley PW, Breitenstein W, Brüggen J, Cowan-Jacob SW, Ray A, et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. Cancer Cell. 2005;7:129–41.
Kantarjian H, Giles F, Wunderle L, Bhalla K, O’Brien S, Wassmann B, et al. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med. 2006;354:2542–51.
Kantarjian HM, Giles F, Gattermann N, Bhalla K, Alimena G, Palandri F, et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood. 2007;110:3540–6.
Saglio G, Kim D-W, Issaragrisil S, le Coutre P, Etienne G, Lobo C, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362:2251–9.
•• Hochhaus A, Saglio G, Hughes TP, Larson RA, Kim D-W, Issaragrisil S, et al. Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia. 2016;30:1044–54. Five-year update of the ENESTnd trial showing that nilotinib results in deeper molecular responses than imatinib, without substantial differences in survival.
•• Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122:872–84. ELN guidelines for the management of CML.
•• National Comprehensive Cancer Network. Chronic myeloid leukemia (Version 4.2018) [Internet]. [cited 2018 Jan 25]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cml.pdf. Updated 2018 NCCN guidelines for the management of CML. Include bosutinib as an approved agent for the frontline treatment of CP CML, as well as recommendations regarding patient populations where TKI discontinuation can be safely trialed.
Boschelli DH, Ye F, Wang YD, Dutia M, Johnson SL, Wu B, et al. Optimization of 4-phenylamino-3-quinolinecarbonitriles as potent inhibitors of Src kinase activity. J Med Chem. 2001;44:3965–77.
Manley PW, Cowan-Jacob SW, Mestan J. Advances in the structural biology, design and clinical development of Bcr-Abl kinase inhibitors for the treatment of chronic myeloid leukaemia. Biochim Biophys Acta. 2005;1754:3–13.
Puttini M, Coluccia AML, Boschelli F, Cleris L, Marchesi E, Donella-Deana A, et al. In vitro and in vivo activity of SKI-606, a novel Src-Abl inhibitor, against imatinib-resistant Bcr-Abl+ neoplastic cells. Cancer Res. 2006;66:11314–22.
Cortes JE, Kim D-W, Kantarjian HM, Brümmendorf TH, Dyagil I, Griskevicius L, et al. Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:3486–92.
Brümmendorf TH, Cortes JE, de Souza CA, Guilhot F, Duvillié L, Pavlov D, et al. Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukaemia: results from the 24-month follow-up of the BELA trial. Br J Haematol. 2015;168:69–81.
•• Cortes JE, Gambacorti-Passerini C, Deininger MW, Mauro MJ, Chuah C, Kim D-W, et al. Bosutinib versus imatinib for newly diagnosed chronic myeloid leukemia: results from the randomized BFORE trial. J Clin Oncol Off J Am Soc Clin Oncol. 2018;36:231–7. Phase III trial evaluating bosutinib (400 mg daily) as a first-line agent in CP CML. Similar to the other second-generation TKIs, bosutinib results in deeper molecular responses, but confers no survival advantage.
FDA grants accelerated approval to bosutinib for treatment of newly-diagnosed PH+ CML [Internet]. [cited 2018 Jan 25]. Available from: https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm589856.htm
O’Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F, et al. AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell. 2009;16:401–12.
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I, et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med. 2012;367:2075–88.
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C, et al. A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med. 2013;369:1783–96.
Lipton JH, Chuah C, Guerci-Bresler A, Rosti G, Simpson D, Assouline S, et al. Ponatinib versus imatinib for newly diagnosed chronic myeloid leukaemia: an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2016;17:612–21.
• Kantarjian HM, Pinilla-Ibarz J, Le Coutre PD, Paquette R, Chuah C, Nicolini FE, et al. Five-year results of the ponatinib phase II PACE trial in heavily pretreated CP-CML patients (pts). J Clin Oncol. 2017;35:7012. Extended follow-up of the PACE trial showing high rates of arterial occlusion events in ponatinib-treated patients.
Sokal JE, Cox EB, Baccarani M, Tura S, Gomez GA, Robertson JE, et al. Prognostic discrimination in “good-risk” chronic granulocytic leukemia. Blood. 1984;63:789–99.
Hasford J, Pfirrmann M, Hehlmann R, Allan NC, Baccarani M, Kluin-Nelemans JC, et al. A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon alfa. Writing Committee for the Collaborative CML Prognostic Factors Project Group. J Natl Cancer Inst. 1998;90:850–8.
Jain P, Kantarjian H, Patel KP, Gonzalez GN, Luthra R, Kanagal Shamanna R, et al. Impact of BCR-ABL transcript type on outcome in patients with chronic-phase CML treated with tyrosine kinase inhibitors. Blood. 2016;127:1269–75.
Castagnetti F, Gugliotta G, Breccia M, Iurlo A, Levato L, Albano F, et al. The BCR-ABL1 transcript type influences response and outcome in Philadelphia chromosome-positive chronic myeloid leukemia patients treated frontline with imatinib. Am J Hematol. 2017;92:797–805.
Hanfstein B, Lauseker M, Hehlmann R, Saussele S, Erben P, Dietz C, et al. Distinct characteristics of e13a2 versus e14a2 BCR-ABL1 driven chronic myeloid leukemia under first-line therapy with imatinib. Haematologica. 2014;99:1441–7.
Pfirrmann M, Evtimova D, Saussele S, Castagnetti F, Cervantes F, Janssen J, et al. No influence of BCR-ABL1 transcript types e13a2 and e14a2 on long-term survival: results in 1494 patients with chronic myeloid leukemia treated with imatinib. J Cancer Res Clin Oncol. 2017;143:843–50.
Quintás-Cardama A, Han X, Kantarjian H, Cortes J. Tyrosine kinase inhibitor-induced platelet dysfunction in patients with chronic myeloid leukemia. Blood. 2009;114:261–3.
Quintás-Cardama A, Kantarjian H, Ravandi F, O’Brien S, Thomas D, Vidal-Senmache G, et al. Bleeding diathesis in patients with chronic myelogenous leukemia receiving dasatinib therapy. Cancer. 2009;115:2482–90.
Steegmann JL, Baccarani M, Breccia M, Casado LF, García-Gutiérrez V, Hochhaus A, et al. European LeukemiaNet recommendations for the management and avoidance of adverse events of treatment in chronic myeloid leukaemia. Leukemia. 2016;30:1648–71.
Jabbour E, Makenbaeva D, Lingohr-Smith M, Lin J. Use of real-world claim databases to assess prevalence of comorbid conditions relevant to the treatment of chronic myelogenous leukemia based on National Comprehensive Network Treatment Guidelines. Clin Lymphoma Myeloma Leuk. 2015;15:797–802.
Tanaka C, Yin OQP, Sethuraman V, Smith T, Wang X, Grouss K, et al. Clinical pharmacokinetics of the BCR-ABL tyrosine kinase inhibitor nilotinib. Clin Pharmacol Ther. 2010;87:197–203.
Nilotinib [package insert]. Novartis Pharmaceuticals Corporation. 2017.
Gorkin L, Kantarjian H. Targeted therapy: generic imatinib—impact on frontline and salvage therapy for CML. Nat Rev Clin Oncol. 2016;13:270–2.
Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32:306–11.
Winn AN, Keating NL, Dusetzina SB. Factors associated with tyrosine kinase inhibitor initiation and adherence among Medicare beneficiaries with chronic myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol. 2016;34:4323–8.
de Lemos ML, Kyritsis V. Clinical efficacy of generic imatinib. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract. 2015;21:76–9.
Danthala M, Gundeti S, Kuruva SP, Puligundla KC, Adusumilli P, Karnam AP, et al. Generic imatinib in chronic myeloid leukemia: survival of the cheapest. Clin Lymphoma Myeloma Leuk. 2017;17:457–62.
Sacha T, Góra-Tybor J, Szarejko M, Bober G, Grzybowska-Izydorczyk O, Niesiobędzka-Krężel J, et al. A multicenter prospective study on efficacy and safety of imatinib generics: a report from Polish Adult Leukemia Group imatinib generics registry. Am J Hematol. 2017;92:E125–8.
Padula WV, Larson RA, Dusetzina SB, Apperley JF, Hehlmann R, Baccarani M, et al. Cost-effectiveness of tyrosine kinase inhibitor treatment strategies for chronic myeloid leukemia in chronic phase after generic entry of imatinib in the United States. J Natl Cancer Inst. 2016;108:djw003.
Hughes T, Deininger M, Hochhaus A, Branford S, Radich J, Kaeda J, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37.
Ross DM, Branford S, Moore S, Hughes TP. Limited clinical value of regular bone marrow cytogenetic analysis in imatinib-treated chronic phase CML patients monitored by RQ-PCR for BCR-ABL. Leukemia. 2006;20:664–70.
Geelen IGP, Thielen N, Janssen JJWM, Hoogendoorn M, Roosma TJA, Valk PJM, et al. Omitting cytogenetic assessment from routine treatment response monitoring in CML is safe. Eur J Haematol. 2018;100:367–71.
Marin D, Ibrahim AR, Lucas C, Gerrard G, Wang L, Szydlo RM, et al. Assessment of BCR-ABL1 transcript levels at 3 months is the only requirement for predicting outcome for patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:232–8.
Jabbour E, Kantarjian HM, Saglio G, Steegmann JL, Shah NP, Boqué C, et al. Early response with dasatinib or imatinib in chronic myeloid leukemia: 3-year follow-up from a randomized phase 3 trial (DASISION). Blood. 2014;123:494–500.
Hughes TP, Saglio G, Kantarjian HM, Guilhot F, Niederwieser D, Rosti G, et al. Early molecular response predicts outcomes in patients with chronic myeloid leukemia in chronic phase treated with frontline nilotinib or imatinib. Blood. 2014;123:1353–60.
Nazha A, Kantarjian H, Jain P, Romo C, Jabbour E, Quintas-Cardama A, et al. Assessment at 6 months may be warranted for patients with chronic myeloid leukemia with no major cytogenetic response at 3 months. Haematologica. 2013;98:1686–8.
Kim DDH, Hamad N, Lee HG, Kamel-Reid S, Lipton JH. BCR/ABL level at 6 months identifies good risk CML subgroup after failing early molecular response at 3 months following imatinib therapy for CML in chronic phase. Am J Hematol. 2014;89:626–32.
Branford S, Yeung DT, Parker WT, Roberts ND, Purins L, Braley JA, et al. Prognosis for patients with CML and >10% BCR-ABL1 after 3 months of imatinib depends on the rate of BCR-ABL1 decline. Blood. 2014;124:511–8.
Hanfstein B, Shlyakhto V, Lauseker M, Hehlmann R, Saussele S, Dietz C, et al. Velocity of early BCR-ABL transcript elimination as an optimized predictor of outcome in chronic myeloid leukemia (CML) patients in chronic phase on treatment with imatinib. Leukemia. 2014;28:1988–92.
Patel AB, Wilds BW, Deininger MW. Treating the chronic-phase chronic myeloid leukemia patient: which TKI, when to switch and when to stop? Expert Rev Hematol. 2017;10:659–74.
Mahon F-X, Réa D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–35.
•• Etienne G, Guilhot J, Rea D, Rigal-Huguet F, Nicolini F, Charbonnier A, et al. Long-term follow-up of the French Stop Imatinib (STIM1) study in patients with chronic myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:298–305. Update of the STIM-1 trial, which first established the feasibility of TKI discontinuation. There was no evidence of late recurrences during 6 years of follow-up.
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood. 2013;122:515–22.
Rea D, Nicolini FE, Tulliez M, Guilhot F, Guilhot J, Guerci-Bresler A, et al. Discontinuation of dasatinib or nilotinib in chronic myeloid leukemia: interim analysis of the STOP 2G-TKI study. Blood. 2017;129:846–54.
Hochhaus A, Masszi T, Giles FJ, Radich JP, Ross DM, Gómez Casares MT, et al. Treatment-free remission following frontline nilotinib in patients with chronic myeloid leukemia in chronic phase: results from the ENESTfreedom study. Leukemia. 2017;31:1525–31.
Imagawa J, Tanaka H, Okada M, Nakamae H, Hino M, Murai K, et al. Discontinuation of dasatinib in patients with chronic myeloid leukaemia who have maintained deep molecular response for longer than 1 year (DADI trial): a multicentre phase 2 trial. Lancet Haematol. 2015;2:e528–35.
Schütz C, Inselmann S, Sausslele S, Dietz CT, Mu Ller MC, Eigendorff E, et al. Expression of the CTLA-4 ligand CD86 on plasmacytoid dendritic cells (pDC) predicts risk of disease recurrence after treatment discontinuation in CML. Leukemia. 2017;31:829–36.
Ilander M, Olsson-Strömberg U, Schlums H, Guilhot J, Brück O, Lähteenmäki H, et al. Increased proportion of mature NK cells is associated with successful imatinib discontinuation in chronic myeloid leukemia. Leukemia. 2017;31:1108–16.
Hughes A, Clarson J, Tang C, Vidovic L, White DL, Hughes TP, et al. CML patients with deep molecular responses to TKI have restored immune effectors and decreased PD-1 and immune suppressors. Blood. 2017;129:1166–76.
Acknowledgments
The authors apologize to those researchers whose work could not be cited due to limitations in the length of the review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myeloproliferative Neoplasms
Rights and permissions
About this article
Cite this article
Kennedy, J.A., Hobbs, G. Tyrosine Kinase Inhibitors in the Treatment of Chronic-Phase CML: Strategies for Frontline Decision-making. Curr Hematol Malig Rep 13, 202–211 (2018). https://doi.org/10.1007/s11899-018-0449-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-018-0449-7