Abstract
Purpose of Review
Acute myeloid leukemia (AML) is a hematologic neoplasia consisting of incompletely differentiated hematopoietic cells of the myeloid lineage that proliferate in the bone marrow, blood, and/or other tissues. Clinical implementation of fluorescence in situ hybridization (FISH) in cytogenetic laboratories allows for high-resolution analysis of recurrent structural chromosomal rearrangements specific to AML, especially in AML with normal karyotypes, which comprises approximately 33–50% of AML-positive specimens. Here, we review the use of several FISH probe strategies in the diagnosis of AML. We also review the standards and guidelines currently in place for use by clinical cytogenetic laboratories in the evaluation of AML.
Recent Findings
Updated standards and guidelines from the WHO, ACMG, and NCCN have further defined clinically significant, recurring cytogenetic anomalies in AML that are detectable by FISH.
Summary
FISH continues to be a powerful technique in the diagnosis of AML, with higher resolution than conventional cytogenetic analysis, rapid turnaround time, and a considerable diagnostic and prognostic utility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a hematologic neoplasia consisting of incompletely differentiated hematopoietic cells of the myeloid lineage that proliferate in the bone marrow, blood, and/or other tissues, and is diagnosed by the presence of at least 20% blasts in the bone marrow [1, 2]. AML preponderantly afflicts those over age 60 years, with increasingly dismal prognoses in advanced age, especially with loss of the TP53 tumor suppressor gene [3]. However, AML can present in children and young adults as well, and is more common in infants than acute lymphoblastic leukemia (ALL) [4]. Recent studies showed hematopoietic clones bearing mutations in AML-related genes to be nearly ubiquitous in healthy adults aged 50–70 years, compared to prior literature showing a presence of ~ 5% in this cohort [5].
For decades, the G-banded karyotype was the gold standard method for diagnosis and prognosis of AML in the clinical cytogenetic laboratory [6]. However, the clinical implementation of fluorescence in situ hybridization (FISH) in cytogenetic laboratories allows for higher resolution analysis of structural chromosomal rearrangements specific to AML that are not detectable with routine karyotyping [7,8,9], especially in AML with normal karyotypes, which comprises approximately 33–50% of AML-positive specimens [10, 11].
In this review, we describe the use of several FISH probe strategies in the diagnosis of cancer in general, and AML in particular. We also review the standards and guidelines currently in place for use by clinical cytogenetic laboratories in the evaluation of AML.
FISH Probes and Strategies in Cancer
FISH involves the use of fluorescently labeled DNA probes that hybridize to genomic loci of interest in metaphase spreads from mitotic cells, as well as interphase nuclei from direct harvests [12]. FISH probes can be made to target: (1) repetitive genomic sequences including alpha-satellite DNA in centromeres, (2) entire chromosomes with whole-chromosome paints (WCP), or (3) specific loci using genomic clones made from bacterial artificial chromosome (BAC) DNA [2]. Metaphase FISH is helpful to elucidate submicroscopic losses and gains of genomic loci, cryptic balanced structural chromosomal rearrangements, as well as characterize larger structural chromosomal abnormalities apparent by G-banding [11, 12]. While metaphase FISH requires actively dividing cells, interphase FISH is a very powerful technique because it can detect genomic loci without the need for mitotic cells. For this reason, interphase FISH can be used to analyze hundreds of nuclei without cell culture, or in cultures with low mitotic index [12]. Interphase FISH is extremely helpful in detecting possible mosaicism because of unbiased assessment of abnormal cells without cell-culture variables, and it has robust sensitivity to determine minimal residual disease after chemotherapy [9, 12,13,14].
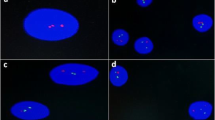
Several probe strategies are available using FISH for chromosomal abnormalities in hematological malignancies, including the use of deletion/duplication (Del/Dup) probes, break-apart probes (BAP), dual-color/dual-fusion (DC/DF) probes, and centromeric (CEP) probes [2, 10, 15] (Fig. 1). Del/Dup probes, typically paired with control probes in contrasting colors on the same chromosome, are designed to target specific genes or disease loci, e.g., the TP53 gene at 17p13.1 in the diagnosis of chronic lymphocytic leukemia (CLL) and multiple myeloma (MM). Loss or gain of fluorescent target signal on one chromosome is confirmed with the remaining control probe that correctly identifies the deleted/duplicated chromosome, as well as the presence of both target and control probes on the other, unaffected homologous chromosome. BAP probes are designed to detect translocations or other rearrangements that rearrange proto-oncogenes, fusing them with other genes or regulatory elements. BAP probes consist of two probes in contrasting colors (green/red) that span opposite ends of the gene, e.g., the KMT2A (MLL) BAP probe at 11q23 with the 5′ end of the gene spanned by a green probe and the 3′ end by a red probe producing two fusion (yellow) signals in normal cells. KMT2A gene rearrangement will result in separated green (5′ KMT2A) and red (3′ KMT2A) signals plus a normal fusion signal at the intact KMT2A allele. DC/DF probes are designed to span genomic loci involved in recurrent balanced translocations or other rearrangements that result in a specific gene fusion, e.g., RUNX1-RUNX1T1 gene fusion as result of the t(8;21)(q22;q22) in AML. The translocation partner genes are spanned by contrasting-colored red and green probes with the translocation resulting in two overlapping red/green (yellow) fusion signals on the two derivative chromosomes, as well as separate red and green signals at the intact gene alleles on the remaining normal homologous chromosomes. Finally, CEP probes are used for chromosome enumeration in interphase nuclei, e.g., chromosome 8 CEP probe in myelodysplastic syndrome (MDS).
Limitations of FISH
FISH only detects abnormalities in genomic regions targeted by the probes used, unlike the whole-genome approach of a full metaphase karyotype via G-bands [2, 10]. The choice of FISH probes is informed by clinical presentation or suspicion of disease. Unlike FISH, chromosomal microarray analysis (CMA), including array comparative genomic hybridization (aCGH) and SNP arrays, is a high-resolution whole-genome approach to genomic copy-number change (CNC) analysis, used for detecting clinically significant submicroscopic gains and losses, and does not require informed choice of probes. CMA resolution is approximately 50–100 kb in the backbone genomic regions, and is higher in targeted gene regions. It can detect CNCs, copy-neutral loss-of-heterozygosity (CN-LOH), and has become a complementary method to chromosome analysis and FISH for the detection of clinically significant chromosomal rearrangements in hematological malignancies. A major limitation of CMA is that it is relatively constrained by poor sensitivity to low-level clonal abnormalities [9, 10]. Both FISH and CMA cannot detect missense/nonsense point mutations (e.g., NPM1 mutations), very small insertions and deletions (indels), and very small intragenic duplications (e.g., internal tandem duplication of FLT3 [FLT3-ITD]). These are typically seen in AML with normal karyotypes and require other molecular techniques for their detection [10, 14].
Use of FISH in AML
In the clinical cytogenetic laboratory, panels of FISH probes are used to detect recurrent abnormalities in AML, utilizing the aforementioned strategies. Del/Dup probes in AML FISH panels cover loci on chromosomes 5 and 7, in order to detect − 5/del(5q) and − 7/del(7q), respectively (Fig. 1a). Deletion of 5q results in loss of red FISH probe, typically spanning the EGR1 (early growth response 1) gene at 5q31. Deletion of 5q31 is often seen in MDS, and concomitant loss of TP53 at 17p13.1 is seen in progression to AML [3]. Monosomy 5 is seen as a recurrent, non-random anomaly in myeloid malignancies, including MDS, myeloproliferative disorders, and AML [10]. Loss of the green FISH probe D7S486 at 7q31 is diagnostic for del(7q), which often includes deletion of the KMT2C (lysine methyltransferase 2C, also known as MLL3, mixed-lineage leukemia 3) gene. Loss of KMT2C is implicated with RAS pathway and TP53 mutations in leukemogenesis [3]. Concomitant loss of CEP 7 indicates monosomy 7 [10]. Although − 7/7q − are often seen in MDS and AML, monosomy 7 is frequently associated with FAB (French-American-British classification) AML types M4-M5 (M4, acute myelomonocytic leukemia; M5, acute monoblastic or monocytic leukemia) [10, 16]. Of note, − 5/5q − and − 7/7q − are indicative of poor disease prognosis in AML (Table 1) [3, 8, 10, 17, 18].
BAP probes in AML FISH panels cover the KMT2A (lysine methyltransferase 2A, also known as MLL, mixed-lineage leukemia) gene at 11q23 and the CBFB (core-binding factor beta subunit) gene at 16q22, as these genes are frequently disrupted by translocation or inversion in AML. KMT2A has a promiscuous multitude of translocation partners in hematological malignancies, with nearly 80 direct fusion partners, and 120 reciprocal fusion variants [19]. KMT2A functions as a lysine methyltransferase whose function is to epigenetically activate gene promoter regions and maintain cell-type-specific gene transcription [19]. Fusion proteins resulting from KMT2A translocations disrupt proper gene expression in roles of transcription initiation and elongation [19]. The most common rearrangements of KMT2A in AML include t(9;11)(p21;q23) and t(11;19)(q23;p13.1). The World Health Organization (WHO) has given special focus to t(9;11)(p21;q23) (KMT2A-MLLT3) as a recurrent anomaly in AML with prognostic value (Table 1) [7, 8]. When observed in AML, KMT2A translocations are associated with AML FAB types M4-M5, like monosomy 7, and are also consistent with an intermediate-to-poor prognosis (Table 1) [10]. While KMT2A rearrangements are common in AML, KMT2A rearrangements present in up to 34–50% of infant AML cases [20].
Structural rearrangements involving CBFB (16q22) can lead to juxtaposition with the MYH11 (myosin heavy chain 11) gene at 16p13.1 via inv(16)(p13.1q22) (Fig. 1b) or t(16;16)(p13.1;q22), generating a novel CBFB-MYH11 chimeric fusion protein that affects RUNX1 protein function and potentiates leukemogenesis in AML [13, 21]. The CBFB FISH BAP probes include 5′ red and 3′ green probes, which are normally present as red/green (yellow) fusion signals spanning the intact CBFB gene on each chromosome 16q22. Inversion or translocation of CBFB results in a split of the signal into separate red and green FISH probe signals on the der(16) (Fig. 1b). CBFB, along with RUNX1, are part of the “core-binding factor” group of genes, which comprise a family of heterodimeric transcription factors that regulate a number of genes in hematopoiesis [3, 22]. AML with inv(16) or t(16;16) is often classified as FAB M4Eo with myelomonocytic blasts and atypical eosinophils [2]. AML with “core-binding factor” abnormalities, including inv(16), t(16;16), and t(8;21) are consistent with favorable prognoses (Table 1) [2, 13].
Dual-color/dual-fusion (DC/DF) FISH probes span genes that are involved in recurrent translocations and concomitant fusions that contribute to pathogenesis in AML, including RUNX1-RUNX1T1 fusion via t(8;21)(q22;q22) in AML, and PML-RARA fusion via t(15;17)(q24;q21) in acute promyelocytic leukemia (APL) (Fig. 1). A red fluorescent probe spans the RUNX1T1 (RUNX1 translocation partner 1, also known as ETO, eight-twenty-one) gene at 8q22 while a contrasting green probe spans RUNX1 at 21q22. The recurrent translocation t(8;21)(q22;q22) results in breakage of one red and one green signal on each translocation chromosome, resulting in a red/green (yellow) fusion signal from the RUNX1-RUNX1T1 fusion on the derivative chromosome 8 and another fusion signal from the reciprocal fusion on the derivative chromosome 21. In addition, separate red and green signals remain at the intact gene alleles on the remaining normal homologous chromosomes (Fig. 1c). Like CBFB, RUNX1 encodes a component of the “core-binding factor” transcription factors [3, 22]. The novel RUNX1-RUNX1T1 chimeric fusion protein acts to suppress normal RUNX1 function in hematopoiesis and results in AML FAB M2 [10, 21]. Similarly to inv(16), t(8;21) in AML has a favorable prognosis (Table 1) [2, 13].
PML-RARA fusion via t(15;17)(q24;q21) is diagnostic in APL FAB M3 [2, 8, 9, 16] (Fig. 1d). Similarly to DC/DF probes for t(8;21), a red fluorescent probe spans PML, while a contrasting green probe spans RARA. The t(15;17) translocation is detected by breakage and fusion of the respective red and green FISH signals spanning the PML and RARA genes. The PML (promyelocytic leukemia) gene at 15q24 encodes a tripartite zinc finger and RING-domain-binding protein, which acts as a transcription factor and tumor suppressor to promote terminal granulocyte differentiation [11]. The RARA (retinoic acid receptor alpha) gene at 17q21 encodes the receptor for retinoic acid ligand, which regulates growth factor expression and hematopoietic progenitor cell differentiation [11]. The PML-RARA chimeric fusion protein results in recruitment of nuclear co-repressors, and blocks the transcription of genes that are fundamental to the hematopoietic differentiation process [23]. The resultant APL was formerly seen as one of the most aggressive leukemias, presenting with disseminated intravascular coagulation (DIC) [2, 10]. However, with the implementation of ATRA (All-trans retinoic acid), APL is now considered a model of targeted therapy. Because of the high risk for early death, and available treatment, rapid identification of APL using FISH or other methods is critical [2].
While conventional G-banded chromosome analysis with unstimulated cultures is indicated for all hematological malignancies to determine baseline karyotype [7,8,9], recent findings continue to bolster the enhanced utility of FISH to detect cryptic cytogenetic rearrangements of clinical significance. Tirado et al. (2016) recently characterized a cryptic three-way rearrangement in AML involving chromosomes 3, 9, and 12, using FISH to determine a possible ETV6-ABL1 rearrangement with an unknown partner on 3p25 [24]. The ambiguous nature of the cryptic rearrangements between distal 9q and 12q highlight the utility of FISH in this case. Barrett et al. (2017) also determined a cryptic insertional translocation t(8;16)(p11.2;p13.3) with KAT6A-CREBBP fusion in a newborn with spontaneously remitting AML in a normal karyotype [4]. Such findings are remarkable and showcase the utility of FISH in putatively normal karyotypes [10, 11].
Even though FISH brings increased yield and ability to detect clinically significant cryptic abnormalities in AML with “normal” karyotypes, the importance of a full 20-cell G-banded chromosome analysis is clear [17]. In a prospective study of 433 clinically suspected cases of MDS or AML, Coleman et al. (2011) detected only six abnormal cases by FISH within 222 full 20-cell chromosome analyses, which were normal by G-bands (2.7%), of which three were 5q- and only one of the three being diagnosed as unclassifiable MDS; none were classified as AML [25]. They suggested that little additional diagnostic or prognostic information is gained by FISH in normal G-banded studies of MDS/AML with full 20-cell chromosome analyses, but may prove beneficial when metaphase yields are poor or structural abnormalities are discovered but require further characterization by FISH. Also, a recent group’s work on comprehensive cytogenetic scoring systems for MDS and MDS-to-AML evolution suggests that abnormalities should be visible by G-bands to be included in the scoring criteria [26, 27].
Current Clinical Guidelines for AML Diagnosis
The “2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia” continued the move away from primary use of the established FAB system for characterizing AML (using morphology, cytochemistry, immunophenotype, genetics, and clinical features) in favor of a more standardized molecular genetic basis, especially in the context of cytogenetically normal AML [7]. While the FAB system sets the formal classification of AML at 30% bone marrow blasts, the WHO sets cutoffs for bone marrow blasts in defining AML at 20% [17, 28]. However, the presence of a recurrent cytogenetic abnormality detectable by FISH obviates the 20% blast cutoff, including t(15;17), t(8;21), and inv(16) or t(16;16) regardless of the percentage of marrow blasts [17].
In addition to the general AML guidelines presented by the WHO [7, 8] and the National Comprehensive Cancer Network (NCCN) [17], practice standards and guidelines for AML evaluation are provided by the American College of Medical Genetics and Genomics (ACMG), within “Section E6.1–6.4 of the ACMG technical standards and guidelines: chromosome studies of neoplastic blood and bone marrow–acquired chromosomal abnormalities” [9]. Within these guidelines, ACMG strongly recommends the G-banded chromosome analysis of 20 metaphase cells from unstimulated, short-term or overnight cultures whenever possible. All normal analyses are to be documented with two karyotypes. Additional cells may be analyzed to characterize any abnormality with positive pathology results with G-banding or FISH. Abnormal G-banded analyses are to be documented with at least one karyotype per abnormal clone, for a minimum total of two karyotypes. In addition to G-banding, interphase FISH is also indicated as a primary testing methodology for hematological malignancies including AML [9]. The benefits of interphase FISH in AML diagnosis include (a) rapid results for differential diagnosis or treatment planning, (b) detection of cryptic submicroscopic anomalies in context of normal G-banded results, (c) detection of clinically significant gene amplification, (d) alternative diagnostic method in the absence of metaphase cells in culture failure or low mitotic index, (e) detection of abnormalities in samples not appropriate for or amenable to G-banded chromosome analysis [9]. However, metaphase FISH is useful to characterize abnormal signal patterns detected with interphase FISH, when such mitotic cells are available [9].
The inclusion of FISH probes targeting specific recurrent abnormalities in AML is based on diagnostic and prognostic value. Interphase FISH analysis of rearrangements of the KMT2A (MLL) gene at 11q23 is of primary importance due to their often cryptic nature and prognostic implications [9], especially AML with t(9;11)(p21;q23) resulting in KMT2A-MLLT3 fusion [7, 8]. Inclusion of t(8;21)(q22;q22) (RUNX1-RUNX1T1) in AML panels is based on the prediction of response to chemotherapy and increased liability to AML relapse in patients with t(8;21) [17]. The use of FISH probes at CBFB (16q22) to diagnose inv(16) or t(16;16) arose to address often poor chromosome morphology to detect inv(16), as well as to determine the fusion of CBFB-MYH11, as “core-binding factor” AML has favorable prognosis [9, 17]. Inclusion of t(15;17)(q24;q21) with PML-RARA fusion is notable for its extremely high value for diagnosis of APL, a formerly feared, aggressive leukemia with highly effective chemotherapy using ATRA [9, 10, 17]. Deletion/duplication probes on chromosomes 5 and 7 are included in the AML FISH panels as they are diagnostic for AML with monosomy 5 and 7, and for del(5q) and del(7q). These are adverse cytogenetic anomalies with poor prognoses [9, 10, 17].
Each laboratory that uses FISH for clinical applications must establish quality control/quality assurance metrics via validation of each FISH probe used for testing. Validation of FISH probes used for clinical testing must be recorded per CLIA ‘88 regulations as well as the ACMG standards and guidelines, including factors such as correct probe localization, sensitivity, and specificity [12]. Also of critical importance in use of FISH for AML and other hematological malignancies is determination of cutoff values, as these chromosomal abnormalities are clonal in nature, and detection of minimal residual disease burden requires very high sensitivity and specificity. Each laboratory is to determine its own cutoff values for FISH probes in a consistent manner, whether it is via usage of the confidence interval around the mean, the inverse beta function, maximum likelihood, or some other statistical method [12].
Conclusions
Clinically significant recurrent chromosomal abnormalities in AML are successfully analyzed using FISH. While G-banded chromosome analysis is indicated as a first-pass test to determine a baseline karyotype in AML and other hematological malignancies, FISH continues to be a powerful technique in the diagnosis of AML, with higher resolution than conventional cytogenetic analysis, rapid turnaround time, and a considerable diagnostic and prognostic utility.
References
Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373:1136–52.
Gersen SL, Keagle MB, editors. The principles of clinical cytogenetics. 3rd ed. New York City: Springer; 2013.
Sperling AS, Gibson CJ, Ebert BL. The genetics of myelodysplastic syndrome: from clonal hematopoiesis to secondary leukemia. Nat Rev Cancer. 2017;17:5–19.
Barrett R, Morash B, Roback D, Pambrun C, Marfleet L, Ketterling RP, et al. FISH identifies a KAT6A/CREBBP fusion caused by a cryptic insertional t(8;16) in a case of spontaneously remitting congenital acute myeloid leukemia with a normal karyotype. Pediatr Blood Cancer. 2017:1–4.
Young AL, Challen GA, Birmann BM, Druley TE. Clonal haematopoiesis harbouring AML-associated mutations is ubiquitous in healthy adults. Nat Commun. 2016;7:1–7.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med. 2009;361:1058–66.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–51.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Mikhail FM, Heerema NA, Rao KW, Burnside RD, Cherry AM, Cooley LD, et al. Section E6.1–6.4 of the ACMG technical standards and guidelines: chromosome studies of neoplastic blood and bone marrow–acquired chromosomal abnormalities. Genet Med. 2016;18:635-42.
Zneimer SM. Cytogenetic abnormalities: chromosomal, FISH and microarray-based clinical reporting. Hoboken: John Wiley & Sons, Inc.; 2014.
Sholl LM, Longtine J, Kuo FC. Molecular analysis of gene rearrangements and mutations in acute leukemias and myeloid neoplasms. Curr Protoc Hum Genet. 2017;92:10.4.1–10.4.49.
Mascarello JT, Hirsch B, Kearney HM, Ketterling RP, Olson SB, Quigley DI, et al. Section E9 of the American College of Medical Genetics technical standards and guidelines: fluorescence in situ hybridization. Genet Med. 2011;13:667–75.
Hourigan CS, Karp JE. Minimal residual disease evaluation in acute myeloid leukaemia. Nat Rev Clin Oncol. 2013;10:460–71.
Sasine JP, Schiller GJ. Acute myeloid leukemia: how do we measure success? Curr Hematol Malig Rep. 2016;11:528–36.
Gowan-Jordan J, Simons A, Schmid M, editors. ISCN 2016 an international system for human Cytogenomic nomenclature (2016). Basel: S. Karger AG; 2016.
Ley TJ. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368:2059–74.
National Comprehensive Cancer Network. Acute myeloid leukemia (Version 3.2017) [Internet]. NCCN Clin. Pract. Guidel. Oncol. (NCCN Guidel. 2017 [cited 2017 Jul 13]. p. MS1-MS77. Available from: https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf
Bochtler T, Granzow M, Stölzel F, Kunz C, Mohr B, Kartal-Kaess M, et al. Marker chromosomes can arise from chromothripsis and predict adverse prognosis in acute myeloid leukemia. Blood. 2017;129:1333–42.
Ney Garcia DR, De Souza MT, De Figueiredo AF, Othman MAK, Rittscher K, Abdelhay E, et al. Molecular characterization of KMT2A fusion partner genes in 13 cases of pediatric leukemia with complex or cryptic karyotypes. Hematol Oncol. 2016:1–9.
Valentine M, Linabery A, Chasnoff S, Hughes A, Mallaney C, Sanchez N, et al. Excess congenital non-synonymous variation in leukemia-associated genes in MLL-infant leukemia: a Children’s Oncology Group report. Leukemia. 2014;28:1235–41.
Shigesada K, van de Sluis B, Liu PP. Mechanism of leukemogenesis by the inv(16) chimeric gene CBFB/PEBP2B-MYH11. Oncogene. 2004;23:4297–307.
Coleman WB, Tsongalis GJ, editors. Molecular diagnostics: for the clinical laboratorian. 2nd ed. Totowa: Humana Press; 2006.
Zahedipour F, Ranjbaran R, Behbahani AB, Afshari KT, Okhovat MA, Tamadon G, et al. Development of flow cytometry-fluorescent in situ hybridization (flow-FISH) method for detection of PML/RARa chromosomal translocation in acute promyelocytic leukemia cell line. Avicenna J Med Biotech. 2017;9:104–8.
Tirado CA, Siangchin K, Shabsovich DS, Sharifian M, Schiller G. A novel three-way rearrangement involving ETV6 (12p13) and ABL1 (9q34) with an unknown partner on 3p25 resulting in a possible ETV6-ABL1 fusion in a patient with acute myeloid leukemia: a case report and a review of the literature. Biomark Res. 2016;4:1–8.
Coleman JF, Theil KS, Tubbs RR, Cook JR. Diagnostic yield of bone marrow and peripheral blood FISH panel testing in clinically suspected myelodysplastic syndromes and/or acute myeloid leukemia: a prospective analysis of 433 cases. Am J Clin Pathol. 2011;135:915–20.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Schanz J, Tüchler H, Solé F, Mallo M, Luño E, Cervera J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30:820–9.
Verstovsek S, Tefferi A, editors. Myeloproliferative neoplasms. New York City: Humana Press; 2011.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Acute Myeloid Leukemias
Rights and permissions
About this article
Cite this article
Gonzales, P.R., Mikhail, F.M. Diagnostic and Prognostic Utility of Fluorescence In situ Hybridization (FISH) Analysis in Acute Myeloid Leukemia. Curr Hematol Malig Rep 12, 568–573 (2017). https://doi.org/10.1007/s11899-017-0426-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-017-0426-6