Abstract
Purpose of Review
Chronic kidney disease (CKD) is highly prevalent in patients with heart failure and reduced ejection fraction (HFrEF), representing a major factor of adverse outcomes. In clinical practice, it is one of the main reasons for not initiating, not titrating, and even withdrawing efficient heart failure drug therapies in patients.
Recent Findings
Despite limited data, studies show that HFrEF therapies maintain their benefits on cardiovascular outcomes in patients with CKD. Most HF drugs cause acute renal haemodynamic changes, but with stabilisation or even improvement after the acute phase, thus with no long-term worsening of the renal function.
Summary
In this expert opinion-based paper, we challenge the pathophysiology misunderstandings that impede HF disease-modifying therapy implementation in this setting and propose a strategy for HF drug titration in patients with moderate, severe, and end-stage chronic kidney disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic kidney disease (CKD) represent a large proportion of the heart failure with reduced ejection fraction (HFrEF) population. About half of the patients with HFrEF have an estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2, and up to 20% of HF patients have an eGFR < 30 ml/min/1.73 m2 [1]. Moreover, patients with HF and CKD experience significantly higher rates of adverse outcomes [2–4].
CKD and HF share interrelated pathophysiology pathways. CKD aggravates HF through the increase of pre- and afterload (i.e. increased arterial stiffness, reduced ultrafiltration or high output shunting in dialysis patients) or through load independent factors such as neurohormonal activation, accelerated progression of coronary artery disease, anaemia, increased inflammation or uremic toxin accumulation. On the other hand, HF accelerates CKD progression due to reduced renal blood flow, chronic hypoperfusion, increased renin-angiotensin system exposure, increased central venous pressure and tissue congestion together with frequent haemodynamic variations and significant diuretic stress related to HF therapies during decompensations [5, 6].
The 2021 European HFrEF guidelines recommend the introduction and uptitration to optimal doses of a quadruple therapy including an angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor–neprilysin inhibitors (ARNI) with a betablocker (BB), a mineralocorticoid receptor antagonist (MRA) and a sodium–glucose cotransporter 2 (SGLT2) inhibitor, in order to decrease the mortality and HF hospitalisation rate [7, 8]. However, most of the studies on which these guidelines are based excluded patients with eGFR < 30 ml/min/1.73 m2 [9–13].
The lack of studies including HFrEF patients with advanced CKD translates into the real world by suboptimal utilisation of these therapies in these patients [1, 14–17]. The presence of a low eGFR, a history of hyperkalaemia > 5 mmol/l and an episode of worsening renal function remain the main factors of HF drug withdrawal, downtitration or even absence of initiation by the cardiologist community [18]. In HF patients with CKD, lower rates of treatment initiation are observed, as well as a lower adherence rate, but a higher risk of treatment discontinuation and subsequently lower chances of reintroduction [19]. However, data from clinical studies and registries clearly show that patients with CKD are those who benefit the most from HF therapies, despite worsening renal function or hyperkalaemic episodes [20].
Taking all this into account, this opinion-based paper, written by a group of cardiologists and nephrologists specialised in heart failure, aims to discuss the pathophysiology misunderstandings that impede HF quadritherapy implementation and then proposes a practical pro-active strategy to improve titration of disease-modifying therapies in patients with CKD.
Background Evidence for HF Drug Use in HFrEF
Several reports from international experts in the field of HF have described extensively each individual heart failure drug class level of evidence depending on the eGFR value [21, 22••]. In most HF trials, patients with advanced chronic kidney disease defined by an eGFR < 30 ml/min/1.73 m2 were excluded. Only the recent trials on SGLT2 inhibitors included patients with eGFR down to 20 ml/min/1.73 m2.
In all these trials and in observational cohorts, patients with CKD experience more hyperkalaemia and worsening renal function episodes related to HF drug therapy. However, the beneficial effect of HF drug therapies in these patients remains unchanged or is even increased. In the recent STRONG-HF trial, there was a positive interaction between maximised HF drug therapy and lower eGFR values [23•].
Despite this data from randomised clinical trials and observational registries, the prescription, initiation and adherence to HFrEF GDMT in clinical practice are clearly lower in patients with eGFR < 30 ml/min/1.73 m2. As presented in Fig. 1, renin-angiotensin system inhibitors (RASi) and MRA prescription are significantly reduced when the GFR is < 30 ml/min/1.73 m2. Conversely, in the same patient population, RASI and MRAs are more frequently discontinued and thereafter not re-initiated. In HFrEF, CKD and a history of hyperkalaemia remain the leading causes for disease-modifying therapies under prescription. A pre-existing kidney impairment is a major limiting factor in HFrEF therapy introduction and uptitration and a frequent cause of downtitration or discontinuation. When treatment is stopped because of acute kidney injury or hyperkalaemia, treatment is often never reintroduced. A close monitoring should however allow to re-initiate and uptitrate again.
RASI and MRA prescription/initiation/adherence/discontinuation and re-initiation rates in patients with HFrEF according to eGFR [19] (adapted table inserted here). Globally, RASI (A) and MRA (B) prescription is lower in patients with GFR < 30 ml/min/1.73 m2 compared to patients without CKD. eGFR, estimated glomerular filtration rate; RASI, renin-angiotensin system inhibitors; MRA, mineralocorticoid receptor antagonist
Titration According to CKD Stage—Misunderstandings, Pathophysiology and Evidence
The 2021 European HF guidelines suggest to abandon the long-standing sequential approach for quadritherapy introduction, placing all classes on the same level of evidence and thus recommending for them to be introduced in all HFrEF patients [7]. The “right” way to introduce these drugs and the optimised ordering of treatment is still debatable, ultimately contributing to an ambiguity that impedes the process itself. Recently, the STRONG-HF trial managed to reinforce the idea that rapid up-titration of HFrEF drugs during and early after acute HF admission is safe when associated with frequent monitoring, resulting in a significant reduction of HF readmissions and all-cause mortality [23•].
However, in patients with CKD, several issues are being raised when considering the implementation of the quadritherapy: whether the introduction is allowed in patients with low eGFR (i.e. < 60 ml/min/1.73 m2 and < 30 ml/min/1.73 m2, respectively), whether it will worsen pre-existing CKD or what is the right attitude when facing kidney side effects?
Proof of Efficacy in CKD and Kidney Safety Profile of HFrEF Drugs
In daily clinical practice, the estimation of kidney function is based on eGFR which further guides treatment options. One must however consider the limitations of the eGFR, notably its high variability. Variations in eGFR occur not only as a consequence of a decline in functional nephron number, but also from haemodynamic alterations. An isolated creatinine value at a moment in time should therefore be interpreted with caution, and changes in creatinine over time are more valuable. Creatinine by itself is an unreliable reflection of kidney function [6, 24]. Furthermore, in HF patients, due to a context of sarcopenia, volume overload or diuretic prescription, plasma creatinine is particularly difficult to analyse and often misleading [25]. Most of the time, eGFR overestimates the true GFR leading to a false sense of security.
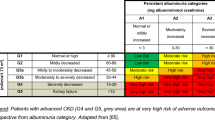
As summarised in Fig. 2, CKD progression in HF patients is equally a major concern as numerous factors already put these patients at a higher risk for faster aggravation. These patients frequently present, on one side, HF-independent risk factors, such as age, associated comorbidities (diabetes, proteinuria or other concomitant kidney diseases), and HFrEF-specific debilitating factors such as RAS hyperactivation, chronic hypoperfusion or congestion [5, 6]. Moreover, CKD patients hospitalised for acute HF have a nearly threefold higher rate of CKD progression and death than patients with no HF hospitalisation [2].
Pathophysiology of long-term irreversible damage to the remaining nephrons in heart failure patients with chronic kidney disease. In CKD patients with heart failure, the principal factors that cause persistent damage to the nephron are either independent from heart failure or directly caused by the neuro-hormonal activation related to heart failure. Of note, permanent damage in the kidneys is usually characterised by the presence of fibrosis with the loss of functional nephron units assessed by pathology on kidney biopsies. As such, kidney fibrosis in heart failure is not always present, and the relationship between estimated glomerular filtration rate and true kidney function is complex. All the GDMT HF classes indicated in heart failure cannot be directly considered as nephrotoxic but, on the contrary, directly block the factors causing persistent nephron damage. As such, RASi, MRAs and SGLT2i really exert a nephroprotective effect. The first deleterious effect related to GDMT is their “nephrodynamic” consequences and the impact on nephron blood flow. The second deleterious effect is related to the changes in pharmacokinetics due to lowered filtration rates and increased risks of hyperkalaemia. CKD, chronic kidney disease; GDMT HF, guideline-directed medical therapy in heart failure
As most HF therapies interfere with kidney haemodynamics, transient alterations of eGFR are frequent after their introduction. Considering these drugs as “nephrotoxic” is a common misconception that limits HFrEF treatment optimisation. Heart failure drugs especially RASI and MRAs are better defined as “nephrodynamic”.
In this section, we aim to address individually the kidney effects of evidence-based HFrEF drugs as well as their efficiency in patients with CKD.
Renin-Angiotensin System Inhibitors (RASi)
ACEI and ARBs both have direct effects on intraglomerular haemodynamics, mainly by reducing intraglomerular hydrostatic pressure through efferent arteriolar vasodilation. This leads to a rise in creatinine levels linked to the decrease of glomerular filtration with glomerular blood flow and pressure reduction. Unless the glomerular blood flow reduction is severe and persistent, RASi do not induce loss of functional nephrons and are on the contrary commonly described as nephroprotectors [26].
Data regarding the RASi effect on eGFR slope are heterogeneous. An early drop in eGFR has been observed with both ACEi and ARB introduction, but with no evidence of persistent reduction after the initial drop [27, 28]. A recent study on advanced CKD patients with eGFR < 30 ml/min/1.73 m2 found no significant difference in a long-term eGFR decrease rate, after RASi discontinuation [29]. It could therefore be deduced that in the absence of kidney harm, RASi should be maintained for their cardiovascular benefits.
ARNi
ARNI provide an additional target in the abnormal HF-associated neurohormonal cascade through neprilysin inhibition. Sacubitril inhibits the breakdown of natriuretic peptides, which are responsible for an increase in diuresis and natriuresis as well as an increase in GFR through afferent arteriolar vasodilating effects and an increase in glomerular capillary ultrafiltration [22••]. ARNi have demonstrated significant reductions in cardiovascular mortality and HF hospitalisations, independently of CKD presence [30]. Their principal deleterious effect is their significant hypotensive effect, which significantly increased compared to ACEi [31]. This hypotensive effect can result in glomerular hypoperfusion (deleterious “nephrodynamic” effect), which in turn can induce permanent kidney damage.
The kidney outcomes have been dissected through post hoc analyses from several trials [32–34]. These analyses suggest a superiority of sacubitril/valsartan compared with enalapril in terms of long-term eGFR preservation and reduction of renal events (sustained 50% reduction in eGFR or onset of end-stage kidney disease) although with an increase in urinary albumin to creatinine ratio. In these trials, all patients with significant hypotension were excluded.
In dialysis patients, limited data from small studies suggest that ARNI treatment is safe and results in an improvement of systolic and diastolic left ventricular function [35, 36].
MRAs
MRAs aim to oppose the abnormal hyperactivation of the mineralocorticoid receptors leading to inflammation and fibrosis in cardiorenal disease [37, 38].
Post hoc analyses of EPHESUS, RALES and EMPHASIS HF trials emphasised their efficiency on cardiovascular outcomes in HFrEF patients with an eGFR < 60 ml/min/1.73 m2. A small decline in eGFR can also be observed during MRA initiation, but this effect fades in long-term assessment. Nevertheless, they induce a higher risk of hyperkalaemia and thus require a more frequent monitoring of potassium and creatinine levels [39–42].
A large meta-analysis highlighted that in dialysis patients, MRA use was associated with a significant improvement in cardiovascular outcomes [43]. A recent retrospective cohort similarly demonstrated significantly lower cardiovascular death risk in dialysis patients on MRA [44], yet this result was not confirmed by a small randomised trial conducted by Charytan et al. [45].
Finerenone, a novel nonsteroidal selective MRA, demonstrated in preclinical studies a more balanced distribution between the heart and kidney compared with spironolactone (which is predominantly concentrated in the kidneys) with more potent anti-inflammatory and antifibrotic renal effects [46]. In patients with mild and moderate CKD, finerenone was associated with a smaller increase in potassium levels than spironolactone and with a lower rate of hyperkalaemia [47], while significantly reducing the risk of CKD progression and cardiovascular events in type 2 diabetic patients with CKD [48, 49]. Despite these data suggesting a safer kidney profile than steroidal MRA, the efficacy in HFrEF patients remains to be addressed.
Betablockers
Betablockers are the only class that does not have direct effects on kidney haemodynamics. Yet, chronic sympathetic hyperactivation promotes renin release and leads to increase levels of angiotensin II [50].
Regarding BB use in CKD, a meta-analysis including more than 16,000 patients from 10 betablocker trials found that for patients in sinus rhythm, BB improve cardiovascular outcomes across all CKD stages (as low as an eGFR of 30 to 44 ml/min/1.73 m2). Moreover, BB do not lead to any kidney function deterioration in patients with pre-existing kidney impairment [51]. In dialysis CKD patients, a small randomised study equally showed a reduction in mortality in the carvedilol group compared to placebo, as well as a reduction in the HF hospitalisation number [52].
SGLT2 Inhibitors
SGLT2 inhibitors safely and significantly improve cardiovascular outcomes in all major trials conducted, including in patients with CKD with an eGFR as low as 30 ml/min/1.73 m2 in DAPA-HF and as low as 20 ml/min/1.73 m2 in EMPEROR-REDUCED trial [9–12].
Differential analysis according to the CKD stage has subsequently been realised and confirmed the cardiovascular outcome improvements across the spectrum of kidney function. Studies suggest a renal protective profile of SGLT2 inhibitors with a reduction in renal events in patients with and without CKD, despite an initial slight decrease in eGFR after initiation [53, 54]. Two dedicated randomised trials, the DAPA-CKD and the EMPA-KIDNEY trial, showed that regardless of CKD aetiology, gliflozins significantly reduce the risk of a long-term decline in eGFR, end-stage kidney disease or death from kidney causes [55, 56].
Managing HF Drug Prescription and Side Effects in Patients with CKD
Side effects following guideline-directed medical therapy (GDMT) introduction can decrease or even halt further uptitration. In this section, the most common ones will be stressed out and the evidence-based recommended management will be summarised (Fig. 3).
Worsening Renal Function
Worsening of renal function (WRF), defined as a change in serum creatinine ≥ 0.3 mg/mL [57], is frequent in HFrEF patients [4]. Several expert reviews have addressed treatment algorithms of WRF in HF patients [7, 58]. WRF entails however different prognosis values according to the context, and it should be interpreted as such, with the three main causes being treatment-induced modifications, haemodynamic changes and intrinsic disease progression in the kidneys.
Treatment-Induced WRF
As previously described, most HF drugs have an impact on kidney function. RASI, ARNi and SGLT2 inhibitors reduce intraglomerular pressures, leading to acute drops in eGFR. These alterations however are to be interpreted as haemodynamic changes and not linked to a reduction in functional nephrons. On the contrary, the slope of eGFR tends to get stabilised after the acute phase, with an inversion of the curve in favour of a slower progression of CKD associated with treatment vs placebo [33, 53, 54, 59, 60]. Consequently, HF drugs should not be considered as intrinsic nephrotoxic drugs but rather as modifiers of kidney haemodynamics. However, any brutal and steep increase in creatine levels early after RASi introduction should lead to a doppler ultrasound evaluation of the renal arteries in order to exclude bilateral renal artery stenosis.
In contrast, a meta-analysis studying the kidney effects following BB introduction showed that a WRF of 20% or greater was associated with a 28% increase in mortality [51]. This data suggests that WRF occurring in relation to BB introduction is due to a profound decrease in cardiac output and therefore associated with a worse prognosis.
Consequently, a moderate WRF in the context of the recent introduction or uptitration of RASi, ARNI or SGLT2i without no other coexisting triggers needs no further action besides regular monitoring. On the other hand, a WRF after BB introduction or uptitration should prompt a more complete re-evaluation of the cardiac output, other signs of clinical deterioration or other causes for the renal dysfunction.
WRF in Congestive HF Patient
Congestion status must be assessed at each time, especially since CKD patients are at higher risk of HF decompensations. In the context of decompensated HF, the main determinant of WRF is increased kidney venous pressure due to venous congestion, followed in a smaller proportion by renal hypoperfusion due to low cardiac output or increased intraabdominal pressure [61].
The increase in serum creatinine in the presence of congestion should be managed with adapted diuretic protocols to insure efficient decongestion [62, 63•]. In this setting, HF drugs should not be reduced or withdrawn except in case of hypotension or severe hyperkalaemia or secondarily if WRF persists despite effective correction of venous congestion.
Unprovoked WRF
When no triggering factor can be attributed to the change in GFR, WRF is strongly associated to worse outcomes, as it reflects a true decrease in residual nephrons. In these patients, no therapeutic options exist to reverse the damage, and attention should be paid to reducing risk factors of progression, such as the use of nephrotoxic agents and strict cardiovascular risk factors monitoring [61]. The interaction between the cardiologist and the nephrologist is then highly recommended.
Hyperkalaemia
CKD patients are at higher risk of hyperkalaemia, especially when they are treated with RASi or MRA. One can easily understand that hyperkalaemia is the leading cause of RASi and MRA down-titration or discontinuation. However, there are several alternatives to manage hyperkalaemia allowing the prescription of RASi and MRAs.
First, drug dosage should be adapted to CKD level. This accounts for the reduction in drug epuration by the kidneys but also reduces the risk of hyperkalaemia. For instance, lowering the drug dosage of spironolactone to the lowest level possible and spacing the prescription to 2 or 3 times per week (one day out of two or three) while monitoring serum potassium levels allows their prescription. The recent results from the STRONG HF trial demonstrate that applying a proactive prescription protocol with frequent medical follow-up enables the prescription of MRAs in more than 80% of patients [23•].
Second, potassium binders such as patiromer, sodium zirconium cyclosilicate (SZC) or sodium polystyrene sulfonate and calcium polystyrene sulfonate [64] should be used in combination with RASi and MRAs in case of hyperkalaemia. Several randomised clinical trials have shown the safety and the benefit of patiromer and sodium zirconium cyclosilicate to allow RASi and/or MRAs prescription and maintenance [65, 66•, 67]. Recently, the DIAMOND trial demonstrated significantly lower kalaemia and fewer hyperkalaemic episodes with patiromer use when compared with the placebo group (hazard ratio [HR] 0.63; P = 0.006) [66•]. In the OPAL-HK trial that included strictly CKD patients (with eGFR down to 15 ml/min/1.73 m2) with RASi treatment, a significant difference in hyperkalaemia recurrence was observed with patiromer compared with the placebo group (60% in the placebo group vs 15% in the patiromer group, P < 0.001) [67].
Third, the complementary use of SGLT2i significantly reduces hyperkalaemia episodes. A large meta-analysis including nearly 50,000 participants treated with SGLT2 inhibitors, showed a significant reduction of hyperkalaemia rates (16%), with no increased risk of hypokalaemia in patients treated with SGLT2i versus placebo (HR 0.84 [95% CI, 0.76–0.93], P heterogeneity = 0.71) [68]. The same was shown in patients with HF [69].
Finally, the education of patients and reduction in potassium-rich alimentary sources toward a lower-potassium regimen is another way to reduce the risk of hyperkalaemia.
In summary, in CKD patients who develop moderate hyperkalaemia (K + levels > 5.5 mEq/l but < 6.0 mEq/l), in parallel with searching and correcting for reversible causes (such as recent diet modification with intake of potassium-rich food), a potassium chelator could be initiated. After 48 to 72 h of therapy, if the kalaemia remains > 5.5 mEq/l, MRA and RASi dose reduction should be considered with close monitoring. If potassium levels remain > 5.5 mEq/l, withdrawal of MRA and/or RASi should be considered. In case of severe hyperkalaemia (> 6 mEq/l), all RASi should be stopped and specific treatment for hyperkalaemia should be started during a dedicated hospitalisation.
Hypotension
Hypotension is common in HF patients representing a barrier in uptitration or even introduction of HF therapy, especially RASi [70]. Low blood pressure (BP) in HF patients can be multifactorial, with the main actors being altered systolic function, hypovolemia or treatment-induced vasodilation.
Studies suggest that low BP in the setting of acute HF is correlated with a worse prognosis, as it reflects the lack of contractile reserve of the left ventricle [70, 71, 73]. However, the prognostic value of hypotension in ambulatory chronic HF patients is less clear, and efforts should be pursued in maintaining evidence-based HF drugs despite an associated low BP. Moreover, lowering LV afterload by decreasing BP allows to improve ventriculo-arterial coupling to decrease myocardial strain.
Amongst HF treatment, ARNI have the most pronounced hypotensive effect, followed by ACEi and ARBs, then MRA and lastly SGLT2 inhibitors [72].
In case of hypotension following GDMT introduction or uptitration, we suggest to first assess its clinical relevance, through the presence of associated symptoms (e.g. dizziness, light-headedness or confusion) as well as the recent context (e.g. dehydration by diuretics dose augmentation or by recent diarrhoea or fever). In line with the current guidelines, no further action is needed in the absence of symptoms [7]. In the presence of symptomatic hypotension with a reversible cause, the latter should be addressed (i.e., optimising the intravascular volume status), with no change in HFrEF treatment. When no other triggering factors are found, the doses of ARNI or ACEi/ARB should be decreased, or in the case of an already minimal ARNI dose, a switch for an ACEi should be performed.
Pro-active Strategy to Initiate, Uptitrate and Monitor HFrEF Quadritherapy in CKD Patients
Considering these aforementioned issues, we suggest a more pro-active approach for HFrEF quadritherapy introduction in CKD patients. This strategy is summarised in Fig. 4.
The main principles of prescription and management of heart failure therapies according to chronic kidney disease severity. GFR, glomerular filtration rate; GDMT, guideline-directed medical therapy; HF, heart failure; SGLT2i, sodium-glucose receptor type 2 inhibitors; RAS, renin-angiotensin system; ARNI, angiotensin receptor and neprilysin inhibitors; SBP, systolic blood pressure
The eGFR level when nephrologist referral should be advised is a matter of debate, and multidisciplinary discussions should be promoted. According to a Cochrane meta-analysis, late referral to a nephrologist (defined as the first nephrology consultation being less than one to six months prior to the initiation of dialysis) was associated with higher mortality and hospitalisation in CKD patients [74]. Nonetheless, a series of general nephroprotective measures should equally be considered in parallel with treatment optimisation. As in every patient, but more particularly with CKD, tobacco discontinuation, minimal physical activity, salt restriction and vaccination update should be strongly promoted. To avoid acute kidney injury, nephrotoxic drugs must be avoided (iodine contrast should be used with caution when eGFR is low and non-steroidal anti-inflammatory drugs are contraindicated), and drugs, particularly antibiotics, must be adapted to the eGFR and to serum concentration.
Monitoring of HFrEF in CKD includes the usual standards of care: evaluating serum sodium, potassium, creatinine (eGFR) and urine albumin-to-creatinine ratio. A urine albumin-to-creatinine ratio under 0.5 g/g should be targeted, mainly through ACEi/ARB use. Correction of metabolic acidaemia (serum bicarbonate < 22 mEq/l) is often addressed with sodium bicarbonate oral supplementation, and it will also participate in the prevention of hyperkalaemia. However, the associated increased sodium intake should warrant a closer monitoring of the risk of hypervolemia following its introduction with an adaptation of diuretics when necessary. A low-protein diet, ideally adapted with a personalised nutritional assessment, is also part of the nephroprotective strategy to avoid hyperphosphatemia. Similarly, vitamin D and calcium deficiency should be corrected with oral intake, as appropriate, to prevent secondary hyperparathyroidism and CKD-mineral and bone disorder. CKD is often associated with anaemia. Although erythropoiesis-stimulating agents have no effect on the prevention or treatment of HF in patients with CKD, trials on HFrEF patients show that the treatment of iron deficiency was associated with improvements in functional capacity and of symptoms, as well as with a significant reduction of HF hospitalisation rate [75, 76].
HF Patients with Moderate Renal Insufficiency
HFrEF patients with moderate CKD (eGFR 30–60 ml/min/1.73 m2) have no strict contraindication for any of the HF drugs. Thus, in de novo HF patients, low doses of all four classes should be initiated from the beginning, with the decision between an ACEi and ARNI to be made according to baseline blood pressure. Known hypertensive patients could rather benefit directly from ARNi, whereas patients with a SBP < 100 mmHg are at higher risk of adverse events (i.e., hypotension) with ARNi rather than with ACEi. Similarly, in chronic HF patients already treated by a sub-optimal treatment, treatment should be revised and optimised whenever feasible to include all four classes in line with the recommendations. In these patients, regular monitoring of potassium and creatinine levels is mandatory as they are more prone to WRF and hyperkalaemia. We suggest assessing kalaemia and creatinine 1 to 2 weeks after each initiation or uptitration. In the absence of adverse events, titration should be pursued until the maximum-tolerated dose is achieved.
HF Patients with Severe Renal Insufficiency
For patients with severe CKD with an eGFR < 30 ml/min/1.73 m2 but already on GDMT, attempts should be made to maintain the quadritherapy with close monitoring of the possible adverse events and therapeutic adaption if necessary. Progression of CKD in itself however should not be the sole reason for treatment discontinuation, as long as GDMT are well tolerated otherwise and adverse events are under control.
In de novo HF in already severe CKD, we still suggest GDMT initiation but with a slightly different strategy since these patients are at a higher risk of WRF and drug overaccumulation due to reduced eGFR. Therefore, a sequential initiation should be considered instead of a concomitant quadritherapy initiation in this situation. Considering their kidney safety profile, we suggest the immediate introduction of a standard dose of BB and SGLT2 inhibitor with no limitation at the first stage of the strategy, and with a rapid uptitration to the maximal tolerated dose. BB and SGLT2 inhibitor introduction and uptitration should not lead to mandatory additional biological controls, unless guided by modification of the clinical status of the patient (i.e. unusual fatigue, oedema). It should be kept in mind that these patients are likely to be already treated with a RASi, as part of their nephroprotective strategy (i.e. to control hypertension and proteinuria to prevent CKD progression), unless HF and CKD were both previously unknown and unfollowed, requiring in parallel a fast nephrology referral. If not, a small dose of an ACEI or an ARNi can also be initiated concomitantly.
The choice between an ACEI or an ARNi can be based on the same considerations as previously discussed, depending on the patient’s baseline SBP, in regard to the expected hypotensive effect of the ARNi. ACEI or ARNi introduction however require monitoring of serum creatinine and potassium levels, as well as their further needed uptitration. Uptitration of ACEI or ARNi should indeed be delayed in this population, guided by clinical and biological tolerance. Once stability under BB, SGLT2i and ACEI/ARNi is ensured, only then should MRA be introduced as the last of the quadritherapy, and its initiation should be considered with a spaced administration (i.e. every 2 to 3 days instead of daily), in order to prevent hyperkalaemia and to allow successful management of it without treatment discontinuation. A closer surveillance of patients with advanced CKD should equally be organised in concertation with their nephrologist, with monthly creatinine and potassium levels controls as well as 7 to 10 days after ACEI, ARNi or MRA treatment uptitration.
Patient with End-Stage Renal Failure or Replacement Therapy
In end-stage renal disease with renal replacement therapy, i.e. maintenance haemodialysis or peritoneal dialysis, very limited data is available to guide the optimal management, which should be guided ideally with close communication to the nephrology referral team of the patient to ensure good adherence. These patients already benefit from close clinical monitoring, with congestion and volo-dependant hypertension being controlled mainly through ultrafiltration in dialysis (and ideally maintained at their targeted “dry weight”) along with a strict sodium and fluid restriction, and partly with their residual renal function (which should be preserved as much as possible if still present, and usually maintained with high doses of loop diuretics). They also undergo close biological monitoring, including potassium levels, which are most of the times kept under control with dialysis, and if needed with potassium chelators. In this very specific population where further degradation of the renal function is no longer possible or futile, we could only assume that any benefit on cardiovascular mortality related to HF therapy is superior to none, especially since these patients experience a very high cardiovascular risk, with cardiovascular events being the leading cause of death [20]. The expected adverse effects of GMDT such as hyperkalaemia or WRF in dialysis patients would be more limited, and downtitration or withdrawal of therapies should be guided mostly by symptomatic hypotension. GDMT quadritherapy should be maintained as much as possible, to their maximal tolerated dose. Down-titration is often required once the optimal “dry weight” is reached and volo-dependant hypertension is corrected. If the lowest doses are still not tolerated, a spaced administration should also be considered in this population and guided by the symptoms: for example, if the patient experiences intra-dialytic hypotension, taking the medication only on dialysis-free days could be proposed to avoid these events and ensure adherence. If withdrawal is mandatory, we suggest following the opposite order of the proposed introduction (i.e. MRA, then ACEI or ARNi, and then only if necessary BB). Regarding SGLT2i, there is no experience or real-world data in dialysis patients, especially since their mechanisms are not currently fully understood beyond the glycosuric and natriuretic effects that are reduced in end-stage kidney failure.
Conclusion
In chronic heart failure with reduced ejection fraction and CKD patients, the use of the four GDMT classes is associated with significant improvement in clinical outcomes, symptoms and quality of life. This improvement seems to be inversely correlated to the level of CKD severity despite the concomitant increase in side effects. Therefore, further investigations through randomised controlled trials are mandatory to confirm the efficacy and safety of HF drugs in patients with severe and end-stage renal disease. Meanwhile, these drugs should be used with appropriate care and monitoring in these patients and nothing should prevent their use because of renal dysfunction.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance. • Of importance
Löfman I, Szummer K, Hagerman I, Dahlström U, Lund LH, Jernberg T. Prevalence and prognostic impact of kidney disease on heart failure patients. Open Hear. 2016;3:e000324.
Bansal N, Zelnick L, Bhat Z, Dobre M, He J, Lash J, Jaar B, Mehta R, Raj D, Rincon-Choles H. Burden and outcomes of heart failure hospitalizations in adults with chronic kidney disease. J Am Coll Cardiol. 2019;73:2691–700.
Löfman I, Szummer K, Dahlström U, Jernberg T, Lund LH. Associations with and prognostic impact of chronic kidney disease in heart failure with preserved, mid-range, and reduced ejection fraction. Eur J Heart Fail. 2017;19:1606–14.
Damman K, Valente MAE, Voors AA, O’Connor CM, van Veldhuisen DJ, Hillege HL. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35:455–69.
Ter Maaten JM, Damman K, Verhaar MC, Paulus WJ, Duncker DJ, Cheng C, Van Heerebeek L, Hillege HL, Lam CSP, Navis G. Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail. 2016;18:588–98.
House AA, Wanner C, Sarnak MJ, et al. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95:1304–17.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution. Eur Heart J. 2021;42:3599–726.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e263–421.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022;387:1089–98.
Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–93.
Patel RB, Fonarow GC, Greene SJ, Zhang S, Alhanti B, DeVore AD, Butler J, Heidenreich PA, Huang JC, Kittleson MM. Kidney function and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol. 2021;78:330–43.
Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. J Card Fail. 2007;13:422–30.
Savarese G, Vasko P, Jonsson Å, Edner M, Dahlström U, Lund LH. The Swedish Heart Failure Registry: a living, ongoing quality assurance and research in heart failure. Ups J Med Sci. 2019;124:65–9.
Patel UD, Hernandez AF, Liang L, Peterson ED, LaBresh KA, Yancy CW, Albert NM, Ellrodt G, Fonarow GC. Quality of care and outcomes among patients with heart failure and chronic kidney disease: a Get With the Guidelines – Heart Failure Program study. Am Heart J. 2008;156:674–81.
Fauvel C, Bonnet G, Mullens W, et al. Sequencing and titrating approach of therapy in heart failure with reduced ejection fraction following the 2021 European Society of Cardiology guidelines: an international cardiology survey. Eur J Heart Fail. 2022. https://doi.org/10.1002/ejhf.2743.
Janse RJ, Fu EL, Dahlström U, Benson L, Lindholm B, van Diepen M, Dekker FW, Lund LH, Carrero J, Savarese G. Use of guideline‐recommended medical therapy in patients with heart failure and chronic kidney disease: from physician’s prescriptions to patient’s dispensations, medication adherence and persistence. Eur. J. Heart Fail. 2022;24:2185–2195.
Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular disease in chronic kidney disease. Circulation. 2021;143:1157–72.
Beldhuis IE, Lam CSP, Testani JM, Voors AA, Van Spall HGC, Ter Maaten JM, Damman K. Evidence-based medical therapy in patients with heart failure with reduced ejection fraction and chronic kidney disease. Circulation. 2022;145:693–712.
Mullens W, Martens P, Testani JM, et al (2022) Renal effects of guideline-directed medical therapies in heart failure: a consensus document from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 24:603–619. Detailed, systematic review describing the renal effects of HF therapies with their level of evidence according to the eGFR value.
Mebazaa A, Davison B, Chioncel O, et al (2022) Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet. https://doi.org/10.1016/S0140-6736(22)02076-1. Randomised trial that demonstrates the safety and the tolerability in the setting of a close follow up of an intensive treatment strategy of rapid up-titration of HF GDMT after a HF hospitalisation.
Inker L, Levey AS: Assessment of glomerular filtration rate. In: Feehally J, Floege J, Tonelli M, Johnson RJ, editors. Comprehensive Clinical Nephrology, 6th ed. Elsevier; 2019;29–39.
Kervella D, Lemoine S, Sens F, Dubourg L, Sebbag L, Guebre-Egziabher F, Bonnefoy E, Juillard L. Cystatin C versus creatinine for GFR estimation in CKD due to heart failure. Am J Kidney Dis. 2017;69:321–3.
Navis G, Faber HJ, de Zeeuw D, de Jong PE. ACE inhibitors and the kidney. Drug Saf. 1996;15:200–11.
McCallum W, Tighiouart H, Ku E, Salem D, Sarnak MJ. Acute declines in estimated glomerular filtration rate on enalapril and mortality and cardiovascular outcomes in patients with heart failure with reduced ejection fraction. Kidney Int. 2019;96:1185–94.
Kiernan MS, Gregory D, Sarnak MJ, Rossignol P, Massaro J, Kociol R, Zannad F, Konstam MA. Early and late effects of high- versus low-dose angiotensin receptor blockade on renal function and outcomes in patients with chronic heart failure. JACC Heart Fail. 2015;3:214–23.
Bhandari S, Mehta S, Khwaja A, Cleland JGF, Ives N, Brettell E, Chadburn M, Cockwell P. Renin-angiotensin system inhibition in advanced chronic kidney disease. N Engl J Med. 2022. https://doi.org/10.1056/NEJMoa2210639.
McMurray JJV, Packer M, Desai AS, et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Vardeny O, Claggett B, Packer M, Zile MR, Rouleau J, Swedberg K, Teerlink JR, Desai AS, Lefkowitz M, Shi V. Efficacy of sacubitril/valsartan vs. enalapril at lower than target doses in heart failure with reduced ejection fraction: the PARADIGM-HF trial. Eur J Heart Fail. 2016;18:1228–34.
Voors AA, Gori M, Liu LCY, et al. Renal effects of the angiotensin receptor neprilysin inhibitor LCZ696 in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2015;17:510–7.
Damman K, Gori M, Claggett B, et al. Renal effects and associated outcomes during angiotensin-neprilysin inhibition in heart failure. JACC Hear Fail. 2018;6:489–98.
Mc Causland FR, Lefkowitz MP, Claggett B, et al. Angiotensin-neprilysin inhibition and renal outcomes in heart failure with preserved ejection fraction. Circulation. 2020;142:1236–45.
Lee S, Oh J, Kim H, Ha J, Chun K, Lee CJ, Park S, Lee S-H, Kang S-M. Sacubitril/valsartan in patients with heart failure with reduced ejection fraction with end-stage of renal disease. ESC Hear Fail. 2020;7:1125–9.
Niu C, Yang S, Ou S, Wu C, Huang P, Hung C, Lin C, Li S. Sacubitril/valsartan in patients with heart failure and concomitant end-stage kidney disease. J Am Heart Assoc. 2022;11:e026407.
Buonafine M, Bonnard B, Jaisser F. Mineralocorticoid receptor and cardiovascular disease. Am J Hypertens. 2018;31:1165–74.
Barrera-Chimal J, Girerd S, Jaisser F. Mineralocorticoid receptor antagonists and kidney diseases: pathophysiological basis. Kidney Int. 2019;96:302–19.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709–17.
Eschalier R, McMurray JJV, Swedberg K, van Veldhuisen DJ, Krum H, Pocock SJ, Shi H, Vincent J, Rossignol P, Zannad F. Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure). J Am Coll Cardiol. 2013;62:1585–93.
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–21.
Rossignol P, Cleland JGF, Bhandari S, Tala S, Gustafsson F, Fay R, Lamiral Z, Dobre D, Pitt B, Zannad F. Determinants and consequences of renal function variations with aldosterone blocker therapy in heart failure patients after myocardial infarction: insights from the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study. Circulation. 2012;125:271–9.
Quach K, Lvtvyn L, Baigent C, Bueti J, Garg AX, Hawley C, Haynes R, Manns B, Perkovic V, Rabbat CG. The safety and efficacy of mineralocorticoid receptor antagonists in patients who require dialysis: a systematic review and meta-analysis. Am J Kidney Dis. 2016;68:591–8.
Lin DS-H, Lin F-J, Lin Y-S, Lee J-K, Lin Y-H. The effects of mineralocorticoid receptor antagonists on cardiovascular outcomes in patients with end-stage renal disease and heart failure. Eur J Heart Fail. 2022. https://doi.org/10.1002/ejhf.2740.
Charytan DM, Himmelfarb J, Ikizler TA, et al. Safety and cardiovascular efficacy of spironolactone in dialysis-dependent ESRD (SPin-D): a randomized, placebo-controlled, multiple dosage trial. Kidney Int. 2019;95:973–82.
Agarwal R, Kolkhof P, Bakris G, Bauersachs J, Haller H, Wada T, Zannad F. Steroidal and non-steroidal mineralocorticoid receptor antagonists in cardiorenal medicine. Eur Heart J. 2021;42:152–61.
Pitt B, Kober L, Ponikowski P, Gheorghiade M, Filippatos G, Krum H, Nowack C, Kolkhof P, Kim S-Y, Zannad F. Safety and tolerability of the novel non-steroidal mineralocorticoid receptor antagonist BAY 94–8862 in patients with chronic heart failure and mild or moderate chronic kidney disease: a randomized, double-blind trial. Eur Heart J. 2013;34:2453–63.
Bakris GL, Agarwal R, Anker SD, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383:2219–29.
Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021;385:2252–63.
Schrier RW, Berl T. Mechanism of effect of alpha adrenergic stimulation with norepinephrine on renal water excretion. J Clin Invest. 1973;52:502–11.
Kotecha D, Gill SK, Flather MD, Holmes J, Packer M, Rosano G, Böhm M, McMurray JJV, Wikstrand J, Anker SD. Impact of renal impairment on beta-blocker efficacy in patients with heart failure. J Am Coll Cardiol. 2019;74:2893–904.
Cice G, Ferrara L, D’Andrea A, D’Isa S, Di Benedetto A, Cittadini A, Russo PE, Golino P, Calabrò R. Carvedilol increases two-year survivalin dialysis patients with dilated cardiomyopathy: a prospective, placebo-controlled trial. J Am Coll Cardiol. 2003;41:1438–44.
Zannad F, Ferreira JP, Pocock SJ, et al. Cardiac and kidney benefits of empagliflozin in heart failure across the spectrum of kidney function. Circulation. 2021;143:310–21.
Jhund PS, Solomon SD, Docherty KF, et al. Efficacy of dapagliflozin on renal function and outcomes in patients with heart failure with reduced ejection fraction. Circulation. 2021;143:298–309.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
The EMPA-KIDNEY Collaborative Group, Staplin N, Wanner C, Green JB, Hauske SJ, Emberson JR, Preiss D, Judge P, Mayne KJ, et al. Empagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 2023 Jan 12;388(2):117–127.
Shirakabe A, Hata N, Kobayashi N, Okazaki H, Matsushita M, Shibata Y, Nishigoori S, Uchiyama S, Asai K, Shimizu W. Worsening renal function definition is insufficient for evaluating acute renal failure in acute heart failure. ESC Hear Fail. 2018;5:322–31.
Mewton N, Girerd N, Boffa J-J, et al. Practical management of worsening renal function in outpatients with heart failure and reduced ejection fraction: statement from a panel of multidisciplinary experts and the Heart Failure Working Group of the French Society of Cardiology. Arch Cardiovasc Dis. 2020;113:660–70.
Holtkamp FA, de Zeeuw D, Thomas MC, Cooper ME, de Graeff PA, Hillege HJL, Parving H-H, Brenner BM, Shahinfar S, LambersHeerspink HJ. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 2011;80:282–7.
Clark H, Krum H, Hopper I. Worsening renal function during renin–angiotensin–aldosterone system inhibitor initiation and long-term outcomes in patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2014;16:41–8.
Mullens W, Damman K, Testani JM, et al. Evaluation of kidney function throughout the heart failure trajectory – a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22:584–603.
Mullens W, Damman K, Harjola V-P, et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:137–55.
Girerd N, Mewton N, Tartière J-M, et al (2022) Practical outpatient management of worsening chronic heart failure. Eur J Heart Fail 24:750–761. Extensive review of pathophysiological aspects of diuretic therapy, the suitable profile of worsening HF that may be managed in an ambulatory setting and the pharmacological IV diuretic protocols that can be used.
Harel Z, Harel S, Shah PS, Wald R, Perl J, Bell CM. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126:264-e9.
Pitt B, Anker SD, Bushinsky DA, Kitzman DW, Zannad F, Huang I-Z, Investigators on behalf of the P-H. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32:820–8.
• Butler J, Anker SD, Lund LH, Coats AJS, Filippatos G, Siddiqi TJ, Friede T, Fabien V, Kosiborod M, Metra M (2022) Patiromer for the management of hyperkalemia in heart failure with reduced ejection fraction: the DIAMOND trial. Eur. Heart J. A randomised trial that demonstrates that use of patiromer reduces the risk of recurrent hyperkalemia and allows the pursuit of MRA treatment.
Weir MR, Bakris GL, Bushinsky DA, Mayo MR, Garza D, Stasiv Y, Wittes J, Christ-Schmidt H, Berman L, Pitt B. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med. 2015;372:211–21.
Neuen BL, Oshima M, Agarwal R, et al. Sodium-glucose cotransporter 2 inhibitors and risk of hyperkalemia in people with type 2 diabetes: a meta-analysis of individual participant data from randomized, controlled trials. Circulation. 2022;145:1460–70.
Shen L, Kristensen SL, Bengtsson O, Böhm M, de Boer RA, Docherty KF, Inzucchi SE, Katova T, Køber L, Kosiborod MN. Dapagliflozin in HFrEF patients treated with mineralocorticoid receptor antagonists: an analysis of DAPA-HF. Heart Fail. 2021;9:254–64.
Cautela J, Tartiere J-M, Cohen-Solal A, Bellemain-Appaix A, Theron A, Tibi T, Januzzi JL Jr, Roubille F, Girerd N. Management of low blood pressure in ambulatory heart failure with reduced ejection fraction patients. Eur J Heart Fail. 2020;22:1357–65.
Adams KF, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149:209–16.
Gheorghiade M, Abraham WT, Albert NM, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–26.
Ambrosy AP, Vaduganathan M, Mentz RJ, Greene SJ, Subačius H, Konstam MA, Maggioni AP, Swedberg K, Gheorghiade M. Clinical profile and prognostic value of low systolic blood pressure in patients hospitalized for heart failure with reduced ejection fraction: insights from the Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study with Tolvaptan (EVEREST) t. Am Heart J. 2013;165:216–25.
Smart NA, Dieberg G, Ladhani M, Titus T (2014) Early referral to specialist nephrology services for preventing the progression to end-stage kidney disease. Cochrane database Syst Rev CD007333
Ponikowski P, van Veldhuisen DJ, Comin-Colet J, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency†. Eur Heart J. 2015 Mar 14;36(11):657–68.
Ponikowski P, Kirwan B-A, Anker SD, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet (London, England). 2020;396:1895–904.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Stefana Enachi, Chahreddine Hadjseyd, Lucie Daniel and Sandrine Lemoine declare no competing interests. Maxime Schleef reports grants from Hospices Civils de Lyon, outside the submitted work. Charles Fauvel reports personal fees from Janssen and grants from Pfizer, outside the submitted work. Nathan Mewton and Laurent Sebbag report personal fees from Bayer, Novartis, Astra Zeneca, Boehringer Ingelheim and Vifor Pharma outside of the submitted work. Antoine Jobbe Duval reports personal fees from Amicus, Bohringer Ingelheim, Novartis and Astra Zeneca and personal fees and non-financial support from Pfizer and Sanofi, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Enachi, S., Schleef, M., Hadjseyd, CE. et al. Challenges and Opportunities in Titrating Disease-Modifying Therapies in Heart Failure with Reduced Ejection Fraction and Chronic Kidney Disease. Curr Heart Fail Rep 20, 101–112 (2023). https://doi.org/10.1007/s11897-023-00594-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-023-00594-1